The Associations Between Physical Activity, Body Perception, and Self-Rated Health in Korean Adults: An Analysis of the 2023 Korean Community Health Survey
Abstract
1. Introduction
2. Materials and Methods
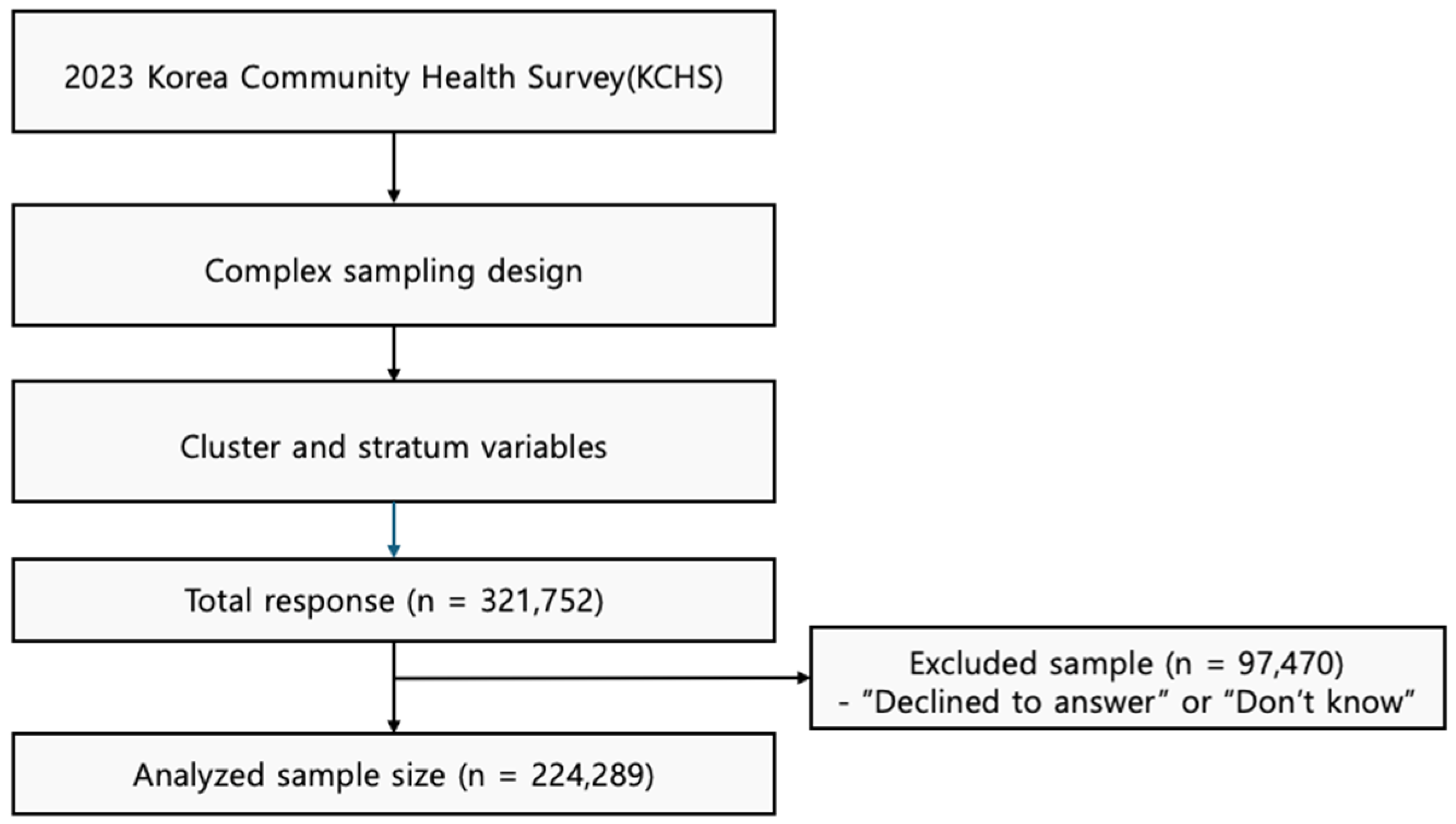
2.1. Data Source and Study Subjects
2.2. Study Participants
2.3. Measure Variables
2.3.1. Physical Activity
2.3.2. BMI
2.3.3. Body Perception
2.3.4. Self-Rated Health (SRH)
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joo, H.; Hong, J.; Jung, J. Projection of future medical expenses based on medical needs and physician availability. J. Korean Med. Sci. 2025, 40, e121. [Google Scholar] [CrossRef]
- Kang, H.; Kim, D.H. Socioeconomic, health, and social connectedness factors associated with self-rated health of octogenarians and nonagenarians in South Korea: Metropolitan and rural comparison. BMC Public Health 2024, 24, 3477. [Google Scholar] [CrossRef]
- Jun, J.; Park, D. Factors associated with self-rated health among Korean elderly. Iran. J. Public Health 2023, 52, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Repkine, A. Determinants of health status and life satisfaction among older south koreans. Healthcare 2024, 12, 1124. [Google Scholar] [CrossRef]
- Tanaka, S.; Muraki, S.; Inoue, Y.; Miura, K.; Imai, E. The association between self-rated health perception and lifestyle factors in Shiga Prefecture, Japan: A cross-sectional study. BMC Public Health 2020, 20, 1786. [Google Scholar] [CrossRef]
- Ryou, I.; Cho, Y.; Yoon, H.J.; Park, M. Gender differences in the effect of self-rated health (SRH) on all-cause mortality and specific causes of mortality among individuals aged 50 years and older. PLoS ONE 2019, 14, e0225732. [Google Scholar] [CrossRef] [PubMed]
- Zarini, G.G.; Vaccaro, J.A.; Canossa Terris, M.A.; Exebio, J.C.; Tokayer, L.; Antwi, J.; Ajabshir, S.; Cheema, A.; Huffman, F.G. Lifestyle behaviors and self-rated health: The living for health program. J. Environ. Public Health 2014, 2014, 315042. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- WHO Guidelines on Physical Activity and Sedentary Behaviour. Recommendations; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 10 October 2025).
- Johnson, N.F.; Hutchinson, C.; Hargett, K.; Kosik, K.; Gribble, P.; Don, B. Bend don’t break: Stretching improves scores on a battery of fall assessment tools in older adults. J. Sport Rehabil. 2020, 30, 78–84. [Google Scholar] [CrossRef]
- Silva, D.A.S. Longer leisure walking time is associated with positive self-rated health among adults and older adults: A Brazilian nationwide study. PeerJ 2021, 9, e11471. [Google Scholar] [CrossRef]
- Neufeld, S.; Machacova, K.; Mossey, J.; Luborsky, M. Walking ability and its relationship to self-rated health in later life. Clin. Gerontol. 2013, 36, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.B.; Oh, Y.H.; Yang, Y.J. Current Status of Physical Activity in South Korea. Korean J. Fam. Med. 2022, 43, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Chudasama, Y.V.; Khunti, K.K.; Zaccardi, F.; Rowlands, A.V.; Yates, T.; Gillies, C.L.; Davies, M.J.; Dhalwani, N.N. Physical activity, multimorbidity, and life expectancy: A UK Biobank longitudinal study. BMC Med. 2019, 17, 108. [Google Scholar] [CrossRef]
- Lee, S.; Ma, X.; Choi, Y.; Kim, Y.S. Association of physical activity and socio-economic status on mortality in older adults: A retro-spective cohort study of KNHANES-mortality linked data. Sci Rep. 2024, 14, 14447. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.K.; Park, S.W.; Lee, S.M. Differences in Physical Activity and Self-Rated Health Levels Based on Satisfaction with Physical Environment of Local Communities: From School to Lifelong Physical Education. Healthcare 2024, 12, 2244. [Google Scholar] [CrossRef]
- Ibsen, B.; Elmose-Østerlund, K.; Høyer-Kruse, J. Associations of types of physical activity with self-rated physical and mental health in Denmark. Prev. Med. Rep. 2024, 37, 102557. [Google Scholar] [CrossRef]
- Cesari, M.; Onder, G.; Zamboni, V.; Manini, T.; Shorr, R.I.; Russo, A.; Bernabei, R.; Pahor, M.; Landi, F. Physical function and self-rated health status as predictors of mortality: Results from longitudinal analysis in the ilSIRENTE study. BMC Geriatr. 2008, 8, 34. [Google Scholar] [CrossRef]
- Yoon, S.J.; Jung, J.G.; Ahn, S.K.; Kim, J.S.; Hong, J.H. Non-linear relationship between body mass index and self-rated health in older Korean adults: Body image and sex considerations. Epidemiol. Health 2023, 45, e2023061. [Google Scholar] [CrossRef]
- Kang, Y.W.; Ko, Y.S.; Kim, Y.J.; Sung, K.M.; Kim, H.J.; Choi, H.Y.; Sung, C.; Jeong, E. Korea community health survey data profiles. Osong Public Health Res. Perspect. 2015, 6, 211–217. [Google Scholar] [CrossRef]
- Brown, N.I.; Henderson, J.; Stern, M.; Carson, T.L. Health-Related Benefits and Adherence for Multiple Short Bouts of Aerobic Physical Activity Among Adults. Am. J. Lifestyle Med. 2024, 19, 58–72. [Google Scholar] [CrossRef]
- Page, P. Current concepts in muscle stretching for exercise and rehabilitation. Int. J. Sports Phys. Ther. 2012, 7, 109–119. [Google Scholar]
- Thomas, S.L.; Heck, R.H. Analysis of large-scale secondary data in higher education research: Potential perils associated with complex sampling designs. Res. High Educ. 2001, 42, 517–540. [Google Scholar] [CrossRef]
- Chen, T.; Xu, M.; Tu, J.; Wang, H.; Niu, X. Relationship between Omnibus and Post-hoc Tests: An Investigation of performance of the F test in ANOVA. Shanghai Arch. Psychiatry 2018, 30, 60–64. [Google Scholar] [CrossRef] [PubMed]
- JafariNasabian, P.; Inglis, J.E.; Reilly, W.; Kelly, O.J.; Ilich, J.Z. Aging human body: Changes in bone, muscle and body fat with consequent changes in nutrient intake. J. Endocrinol. 2017, 234, R37–R51. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Gallagher, D. Body composition changes with aging: The cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition 2010, 26, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Kye, S.Y.; Park, K. Gender differences in factors associated with body weight misperception. Public Health Nutr. 2021, 24, 2483–2495. [Google Scholar] [CrossRef]
- Swami, V.; Todd, J. Rural-metropolitan differences in body appreciation and associations with life satisfaction in adults from Sabah, Malaysia. Body Image 2022, 43, 385–392. [Google Scholar] [CrossRef] [PubMed]
- White, H.J.; Sharpe, H.; Plateau, C.R. Family body culture, disordered eating and mental health among young adult females during COVID-19. Eat. Behav. 2023, 51, 101792. [Google Scholar] [CrossRef]
- Hanna, K.L.; Collins, P.F. Relationship between living alone and food and nutrient intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef]
- Chae, W.; Ju, Y.J.; Shin, J.; Jang, S.I.; Park, E.C. Association between eating behaviour and diet quality: Eating alone vs. eating with others. Nutr. J. 2018, 17, 117. [Google Scholar] [CrossRef]
- Kim, M.G.; Choi, S. Associations of type and intensity of social participation with depression, self-rated health, and life satisfaction among community-dwelling older adults in the Republic of Korea: A nationwide cross-sectional study. Osong Public Health Res. Perspect. 2024, 15, 451–460. [Google Scholar] [CrossRef]
- Kim, B.; Hyun, H.S. Associations between Social and Physical Environments, and Physical Activity in Adults from metropolitan and Rural Regions. Osong Public Health Res. Perspect. 2018, 9, 16–24. [Google Scholar] [CrossRef]
- Sirotiak, Z.; Brellenthin, A.G.; Hariharan, A.; Welch, A.S.; Meyer, J.D.; Franke, W.D. Psychological correlates of physical activity among adults living in rural and metropolitan settings. Front. Psychol. 2024, 15, 1389078. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lee, S.H. Comparative Analysis of Health Behaviors, Health Status, and Medical Needs among One-Person and Multi-Person Household Groups: Focused on the Ageing Population of 60 or More. Korean J. Fam. Med. 2021, 42, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Ho, Y.L.; Mahirah, D.; Ho, C.Z.; Thumboo, J. The role of the family in health promotion: A scoping review of models and mechanisms. Health Promot. Int. 2022, 37, daac119. [Google Scholar] [CrossRef]
- Golaszewski, N.M.; LaCroix, A.Z.; Hooker, S.P.; Bartholomew, J.B. Group exercise membership is associated with forms of social support, exercise identity, and amount of physical activity. Int. J. Sport Exer. Psychol. 2022, 20, 630–643. [Google Scholar] [CrossRef]
- Jeong, S.M.; Cho, S.I. Effects of living alone versus with others and of housemate type on smoking, drinking, dietary habits, and physical activity among elderly people. Epidemiol. Health 2017, 39, e2017034. [Google Scholar] [CrossRef]
- Lindsay Smith, G.; Banting, L.; Eime, R.; O’Sullivan, G.; van Uffelen, J.G.Z. The association between social support and physical activity in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 56. [Google Scholar] [CrossRef]
- Ferrucci, L.; Cooper, R.; Shardell, M.; Simonsick, E.M.; Schrack, J.A.; Kuh, D. Age-related change in mobility: Perspectives from life course epidemiology and geroscience. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1184–1194. [Google Scholar] [CrossRef]
- Dixon, B.N.; Ugwoaba, U.A.; Brockmann, A.N.; Ross, K.M. Associations between the built environment and dietary intake, physical activity, and obesity: A scoping review of reviews. Obes. Rev. 2021, 22, e13171. [Google Scholar] [CrossRef] [PubMed]
- Alley, S.J.; Schoeppe, S.; Rebar, A.L.; Hayman, M.; Vandelanotte, C. Age differences in physical activity intentions and implementation intention preferences. J. Behav. Med. 2018, 41, 406–415. [Google Scholar] [CrossRef]
- Södergren, M.; Sundquist, J.; Johansson, S.E.; Sundquist, K. Physical activity, exercise and self-rated health: A population-based study from Sweden. BMC Public Health 2008, 8, 352. [Google Scholar] [CrossRef]
- Weinberger, N.A.; Kersting, A.; Riedel-Heller, S.G.; Luck-Sikorski, C. Body dissatisfaction in individuals with obesity compared to normal-weight individuals: A systematic review and meta-analysis. Obes. Facts 2016, 9, 424–441. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Tse, M.M.Y.; Wong, B.Y.M. Exercise habits and preferences of community-dwelling older adults with chronic pain: An exploratory study. Healthcare 2025, 13, 384. [Google Scholar] [CrossRef] [PubMed]
- Hyun, K.R.; Kang, S.; Lee, S. Population aging and healthcare expenditure in Korea. Health Econ. 2016, 25, 1239–1251. [Google Scholar] [CrossRef] [PubMed]
| Variables | N (%) | ||
|---|---|---|---|
| Sex | Male | 104,995 (46.0%) | |
| Female | 123,254 (54.0%) | ||
| Age (years) | 20–29 | 21,446 (9.5%) | |
| 30–39 | 24,240 (10.6%) | ||
| 40–49 | 33,659 (14.8%) | ||
| 50–59 | 42,516 (18.6%) | ||
| 60–69 | 51,449 (22.5%) | ||
| 70–79 | 34,756 (15.2%) | ||
| 80 over | 20,183 (8.8%) | ||
| Location | Metropolitan | 75,016 (32.9%) | |
| Non-metropolitan | 153,233 (67.1%) | ||
| Household (person) | Single | 40,471 (17.7%) | |
| 2–3 | 79,222 (34.7%) | ||
| 4–6 | 96,734 (42.4%) | ||
| 7 over | 11,822 (5.2%) | ||
| Physical Activity | Leisure | Yes | 71,824 (31.5%) |
| No | 156,425 (68.5%) | ||
| Walking | Yes | 38,819 (17.0%) | |
| No | 189,430 (83.0%) | ||
| Stretching | Yes | 100,633 (44.1%) | |
| No | 127,616 (55.9%) | ||
| Total | 228,249 (100.0%) | ||
| Variables | BMI (kg/m2) | Body Perception | Self-Rated Health | ||
|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | |||
| Sex | Male | 24.44 ± 3.27 | 3.20 ± 0.88 | 3.08 ± 0.93 | |
| Female | 23.04 ± 3.36 | 3.31 ± 0.87 | 3.06 ± 0.89 | ||
| t | 100.500 *** | −30.721 *** | 4.804 *** | ||
| r2 | 0.042 | 0.004 | 0.000 | ||
| Age (years) | 20–29 (a) | 22.27 ± 4.15 | 3.28 ± 0.91 | 2.21 ± 0.78 | |
| 30–39 (b) | 24.07 ± 4.10 | 3.47 ± 0.89 | 2.40 ± 0.75 | ||
| 40–49 (c) | 23.95 ± 3.61 | 3.45 ± 0.84 | 2.58 ± 0.72 | ||
| 50–59 (d) | 23.82 ± 3.12 | 3.35 ± 0.81 | 2.69 ± 0.77 | ||
| 60–69 (e) | 23.87 ± 2.91 | 3.27 ± 0.82 | 2.86 ± 0.85 | ||
| 70–79 (f) | 23.65 ± 3.02 | 3.08 ± 0.85 | 3.17 ± 0.92 | ||
| 80 over (g) | 22.53 ± 3.19 | 2.73 ± 0.92 | 3.51 ± 0.94 | ||
| F | 573.432 *** | 2168.954 *** | 7071.262 *** | ||
| Post hoc | g < a < f < d,e < c < b | g < f < a,e < b,c,d | a < b < c < d < e < f < g | ||
| η2 | 0.015 | 0.054 | 0.157 | ||
| GivemnLocation | Metropolitan | 23.69 ± 3.48 | 3.31 ± 0.86 | 2.97 ± 0.87 | |
| Non-metropolitan | 23.68 ± 3.35 | 3.23 ± 0.88 | 3.12 ± 0.92 | ||
| t | 0.110 | 18.414 *** | −36.591 *** | ||
| r2 | 0.000 | 0.001 | 0.006 | ||
| Household (person) | Single (a) | 23.53 ± 3.47 | 3.15 ± 0.91 | 3.01 ± 0.98 | |
| 2–3 (b) | 23.70 ± 3.10 | 3.21 ± 0.85 | 2.88 ± 0.89 | ||
| 4–6 (c) | 23.72 ± 3.56 | 3.34 ± 0.87 | 2.62 ± 0.83 | ||
| 7 over (d) | 23.78 ± 3.58 | 3.28 ± 0.87 | 2.71 ± 0.87 | ||
| F | 35.700 *** | 537.727 *** | 2397.381 *** | ||
| Post hoc | a < b,c,d | a < b < d < c | c < d < b < a | ||
| η2 | 0.000 | 0.007 | 0.031 | ||
| Physical Activity | Leisure | Yes | 23.81 ± 3.24 | 3.33 ± 0.81 | 2.86 ± 0.86 |
| No | 23.63 ± 3.46 | 3.23 ± 0.90 | 3.17 ± 0.91 | ||
| t | 12.383 *** | 26.209 *** | −77.996 *** | ||
| r2 | 0.001 | 0.003 | 0.015 | ||
| Walking | Yes | 23.72 ± 3.55 | 3.17 ± 0.95 | 3.05 ± 1.00 | |
| No | 23.68 ± 3.36 | 3.28 ± 0.86 | 2.73 ± 0.86 | ||
| t | 2.382 * | −20.340 *** | 59.482 *** | ||
| r2 | 0.000 | 0.002 | 0.015 | ||
| Stretching | Yes | 23.77 ± 3.53 | 3.22 ± 0.93 | 2.94 ± 0.92 | |
| No | 23.62 ± 3.28 | 3.29 ± 0.83 | 2.66 ± 0.85 | ||
| t | 10.212 *** | −16.805 *** | 73.972 *** | ||
| r2 | 0.000 | 0.001 | 0.023 | ||
| Variables | Walking (Days/Week) | Stretching (Days/Week) | |
|---|---|---|---|
| M ± SD | M ± SD | ||
| Sex | Male | 4.27 ± 2.68 | 3.07 ± 2.19 |
| Female | 4.20 ± 2.57 | 3.15 ± 2.11 | |
| t | 6.424 *** | −8.847 *** | |
| r2 | 0.000 | 0.000 | |
| Age (years) | 20–29 (a) | 4.72 ± 2.36 | 3.06 ± 2.05 |
| 30–39 (b) | 4.39 ± 2.48 | 3.05 ± 2.03 | |
| 40–49 (c) | 4.17 ± 2.52 | 3.11 ± 2.06 | |
| 50–59 (d) | 4.18 ± 2.57 | 3.37 ± 2.14 | |
| 60–69 (e) | 4.29 ± 2.64 | 3.32 ± 2.22 | |
| 70–79 (f) | 4.27 ± 2.72 | 3.00 ± 2.22 | |
| 80 over (g) | 3.56 ± 2.94 | 2.33 ± 2.02 | |
| F | 378.718 *** | 669.146 *** | |
| Post hoc | g < c,d < e,f < b < a | g < a,b,f < c < d,e | |
| η2 | 0.009 | 0.017 | |
| Location | Metropolitan | 4.70 ± 2.38 | 3.24 ± 2.11 |
| Non-metropolitan | 4.01 ± 2.70 | 3.05 ± 2.16 | |
| t | 62.734 *** | 19.674 *** | |
| r2 | 0.017 | 0.001 | |
| Household (person) | Single (a) | 4.19 ± 2.68 | 3.03 ± 2.17 |
| 2–3 (b) | 4.21 ± 2.69 | 3.15 ± 2.19 | |
| 4–6 (c) | 4.28 ± 2.54 | 3.12 ± 2.10 | |
| 7 over (d) | 4.20 ± 2.62 | 3.02 ± 2.13 | |
| F | 17.299 *** | 32.896 *** | |
| Post hoc | a,b,d < c | a,d < b,c | |
| η2 | 0.000 | 0.000 | |
| Leisure activity | Yes | 4.63 ± 2.42 | 3.75 ± 2.06 |
| No | 4.06 ± 2.69 | 2.82 ± 2.12 | |
| t | 50.794 *** | 98.790 *** | |
| r2 | 0.011 | 0.040 | |
| Variables | BMI (kg/m2) | Body Perception | Self-Rated Health | |
|---|---|---|---|---|
| Physical activity | Frequency (days/week) | M ± SD | M ± SD | M ± SD |
| Walking | 0 (a) | 23.62 ± 3.43 | 3.17 ± 0.95 | 3.05 ± 1.00 |
| 1–2 (b) | 23.73 ± 3.39 | 3.33 ± 0.89 | 2.78 ± 0.84 | |
| 3–4 (c) | 23.75 ± 3.30 | 3.31 ± 0.86 | 3.80 ± 0.85 | |
| 5–7 (d) | 23.87 ± 3.28 | 3.25 ± 0.85 | 2.70 ± 0.87 | |
| F | 53.767 *** | 233.635 *** | 1600.172 *** | |
| Post hoc | a < b,c < d | a < d < b,c | d < b, c < a | |
| η2 | 0.000 | 0.003 | 0.021 | |
| Stretching | 0 (a) | 23.77 ± 3.53 | 3.22 ± 0.93 | 2.94 ± 0.92 |
| 1–2 (b) | 23.60 ± 3.43 | 3.34 ± 0.86 | 2.69 ± 0.82 | |
| 3–4 (c) | 23.58 ± 3.27 | 3.30 ± 0.83 | 2.64 ± 0.82 | |
| 5–7 (d) | 23.65 ± 3.22 | 3.25 ± 0.82 | 2.66 ± 0.88 | |
| F | 39.548 | 162.301 *** | 1877.435 *** | |
| Post hoc | c,b < d < a | a < d < c < b | c < d < b < a | |
| η2 | 0.000 | 0.002 | 0.024 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, G.-K.; Roh, S.-Y.; Hwang, S.-H. The Associations Between Physical Activity, Body Perception, and Self-Rated Health in Korean Adults: An Analysis of the 2023 Korean Community Health Survey. Medicina 2025, 61, 1898. https://doi.org/10.3390/medicina61111898
Kim G-K, Roh S-Y, Hwang S-H. The Associations Between Physical Activity, Body Perception, and Self-Rated Health in Korean Adults: An Analysis of the 2023 Korean Community Health Survey. Medicina. 2025; 61(11):1898. https://doi.org/10.3390/medicina61111898
Chicago/Turabian StyleKim, Geun-Kook, Su-Yeon Roh, and Sung-Ho Hwang. 2025. "The Associations Between Physical Activity, Body Perception, and Self-Rated Health in Korean Adults: An Analysis of the 2023 Korean Community Health Survey" Medicina 61, no. 11: 1898. https://doi.org/10.3390/medicina61111898
APA StyleKim, G.-K., Roh, S.-Y., & Hwang, S.-H. (2025). The Associations Between Physical Activity, Body Perception, and Self-Rated Health in Korean Adults: An Analysis of the 2023 Korean Community Health Survey. Medicina, 61(11), 1898. https://doi.org/10.3390/medicina61111898





