Analysis of Risk Factor Changes for Myopia in Korean Adolescents Before and After the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
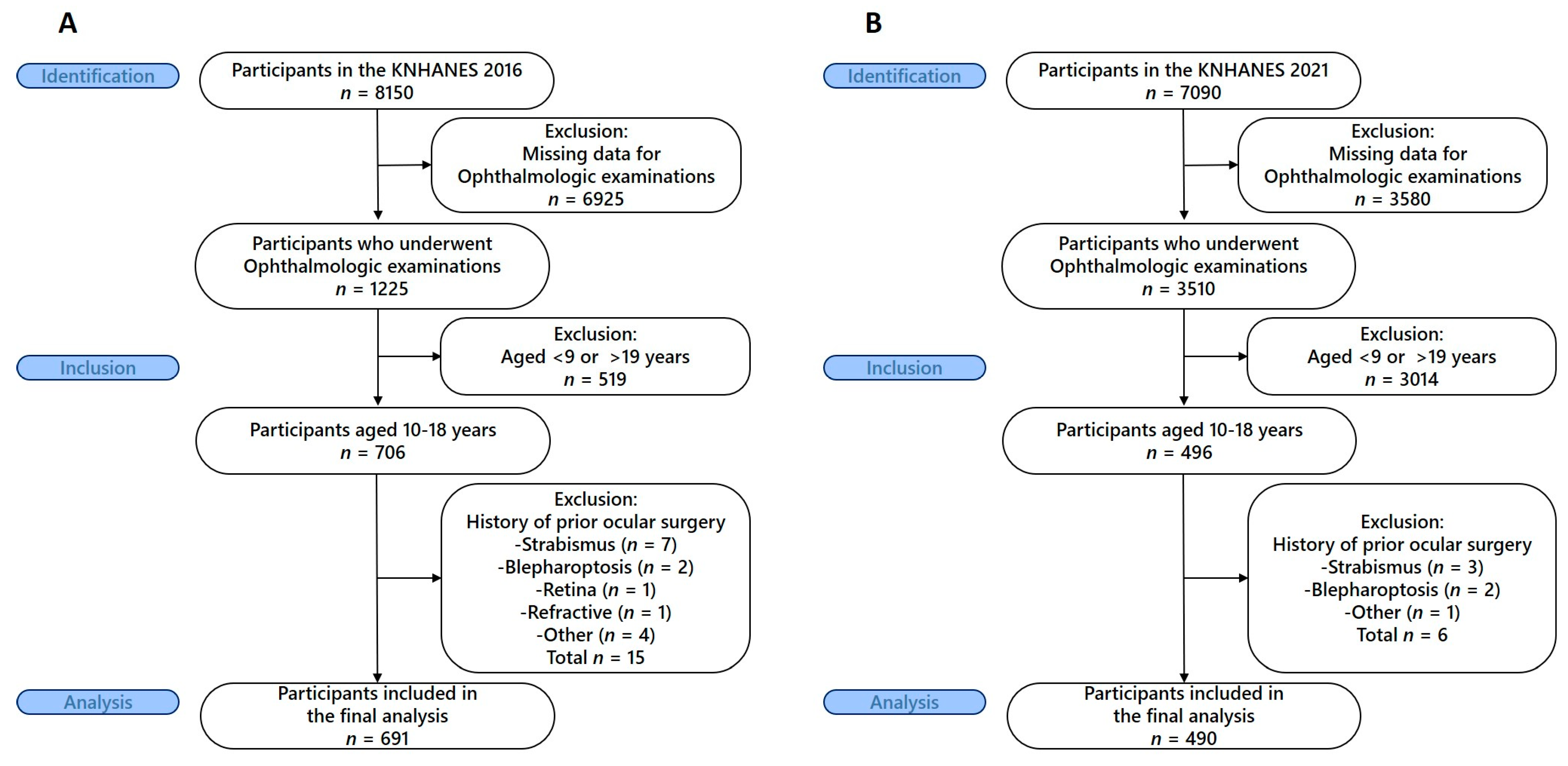
2.2. Participants
2.3. Variables
2.3.1. Outcome Measures
2.3.2. Exposure Variables
2.3.3. Statistical Methods
3. Results
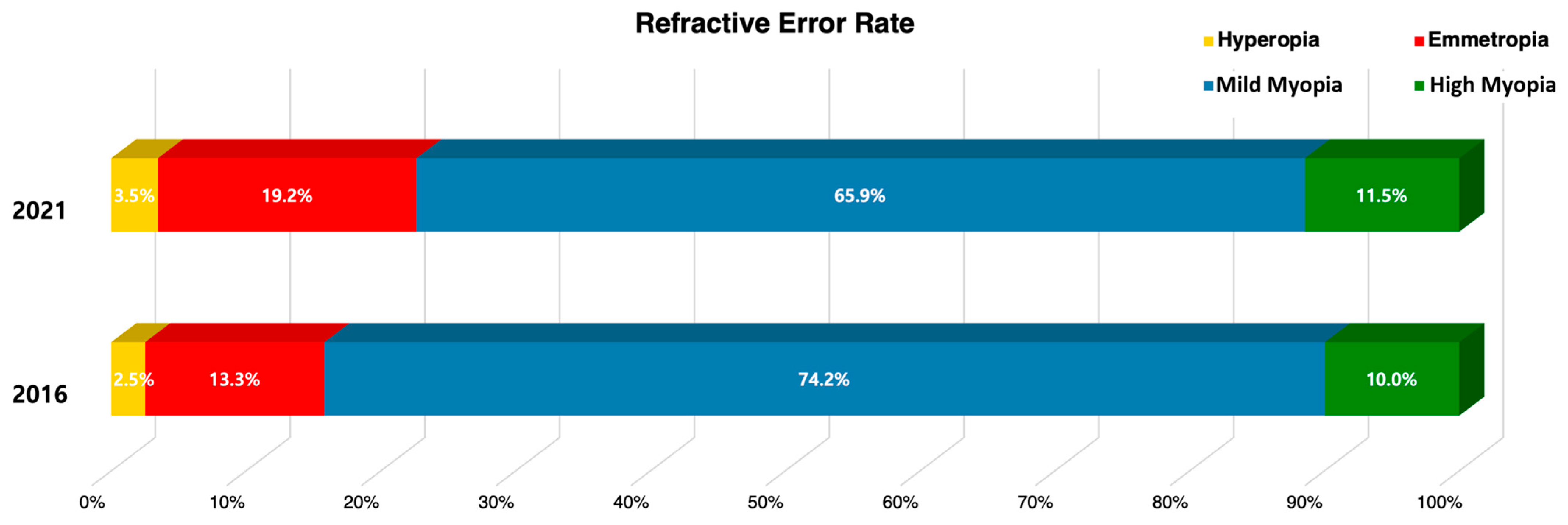
3.1. Changes in Refractive Error Distribution Before and After COVID-19
3.2. Participant Characteristics by Refractive Error Groups
3.3. Factors Associated with Refractive Errors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| No. | Variables | Pre-COVID-19 (2016) | Post-COVID-19 (2021) |
|---|---|---|---|
| Model 1 | Sex, town, age | 5.0% | 12.2% |
| Model 2 | model 1+ BMI | 7.3% | 13.2% |
| Model 3 | model 1+ near work time | 5.8% | 12.4% |
| Model 4 | model 2 + near work time | 7.9% | 13.4% |
| Model 5 | model 4 + Average Daily Sedentary Time | 6.4% | 11.5% |
| Model 6 | model 5 + sleep duration | 6.6% | 11.6% |
References
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Burton, M.J.; Ramke, J.; Marques, A.P.; Bourne, R.R.A.; Congdon, N.; Jones, I.; Ah Tong, B.A.M.; Arunga, S.; Bachani, D.; Bascaran, N.; et al. The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. Lancet Glob. Health 2021, 9, e489–e551. [Google Scholar] [CrossRef]
- Yoon, K.C.; Mun, G.H.; Kim, S.D.; Kim, S.H.; Kim, C.Y.; Park, K.H.; Park, Y.J.; Baek, S.H.; Song, S.J.; Shin, J.P.; et al. Prevalence of eye diseases in South Korea: Data from the Korea National Health and Nutrition Examination Survey 2008–2009. Korean J. Ophthalmol. 2011, 25, 421–433. [Google Scholar] [CrossRef]
- Rim, T.H.; Kim, S.H.; Lim, K.H.; Choi, M.; Kim, H.Y.; Baek, S.H. Refractive errors in Koreans: The Korea National Health and Nutrition Examination Survey 2008–2012. Korean J. Ophthalmol. 2016, 30, 214–224. [Google Scholar] [CrossRef]
- Jung, S.K.; Lee, J.H.; Kakizaki, H.; Jee, D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest. Ophthalmol. Vis. Sci. 2012, 53, 5579–5583. [Google Scholar] [CrossRef]
- Lim, D.H.; Han, J.; Chung, T.-Y.; Kang, S.; Yim, H.W. The high prevalence of myopia in Korean children with influence of parental refractive errors: The 2008–2012 KNHANES. PLoS ONE 2018, 13, e0207690. [Google Scholar]
- Zhang, X.; Qu, X.; Zhou, X. Association between parental myopia and the risk of myopia in a child. Exp. Ther. Med. 2015, 9, 2420–2428. [Google Scholar] [CrossRef]
- McCullough, S.; Adamson, G.; Breslin, K.M.M.; McClelland, J.F.; Doyle, L.; Saunders, K.J. Axial growth and refractive change in white European children and young adults: Predictive factors for myopia. Sci. Rep. 2020, 10, 15189. [Google Scholar] [CrossRef] [PubMed]
- Hammond, C.J.; Snieder, H.; Gilbert, C.E.; Spector, T.D. Genes and environment in refractive error: The twin eye study. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1232–1236. [Google Scholar]
- Ha, A.; Lee, Y.J.; Lee, M.; Shim, S.R.; Kim, Y.K. Digital screen time and myopia: A systematic review and dose–response meta-analysis. JAMA Netw. Open 2025, 8, e2460026. [Google Scholar] [CrossRef] [PubMed]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef]
- Mei, Z.; Zhang, Y.; Jiang, W.; Lam, C.; Luo, S.; Cai, C.; Luo, S. Efficacy of outdoor interventions for myopia in children and adolescents: A systematic review and meta-analysis of randomized controlled trials. Front. Public Health 2024, 12, 1452567. [Google Scholar]
- Laan, D.; Tan, E.T.C.; Huis In ’t Veld, P.I.; Jellema, H.M.; Jenniskens, K. Myopia progression in children during home confinement in the COVID-19 pandemic: A systematic review and meta-analysis. J. Optom. 2024, 17, 100493. [Google Scholar]
- Wang, J.; Han, Y.; Musch, D.C.; Li, Y.; Wei, N.; Qi, X.; Ding, D.; Li, X.; Song, L.; Zhang, Y.; et al. Evaluation and follow-up of myopia prevalence among school-aged children subsequent to the COVID-19 home confinement in Feicheng, China. JAMA Ophthalmol. 2023, 141, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Kneepkens, S.C.M.; de Vlieger, J.; Tideman, J.W.L.; Enthoven, C.A.; Polling, J.R.; Klaver, C.C.W. Myopia risk behaviour related to the COVID-19 lockdown in Europe: The Generation R study. Ophthalmic Physiol. Opt. 2023, 43, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Seo, J.S.; Yoo, W.S.; Kim, G.N.; Kim, R.B.; Chae, J.E.; Chung, I.; Seo, S.W.; Kim, S.J. Factors associated with myopia in Korean children: KNHANES 2016–2017 (VII). BMC Ophthalmol. 2020, 20, 31. [Google Scholar] [CrossRef]
- Lee, S.; Lee, H.J.; Lee, K.G.; Kim, J. Obesity and high myopia in children and adolescents: Korea National Health and Nutrition Examination Survey. PLoS ONE 2022, 17, e0265317. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.; Zhang, B.; Lin, L.; Chen, R.; Chen, S.; Zhao, Y.; Qu, J. Comparison of myopic progression before, during, and after COVID-19 lockdown. Ophthalmology 2021, 128, 1655–1657. [Google Scholar] [CrossRef]
- Mu, J.; Zhong, H.; Jiang, M.; Yang, W. Epidemiological characteristics of myopia among school-age children before, during, and after the COVID-19 pandemic: A cohort study in Shenzhen, China. Front. Med. 2024, 11, 1368219. [Google Scholar] [CrossRef]
- Zhang, X.; Cheung, S.S.; Chan, H.N.; Zhang, Y.; Wang, Y.M.; Yip, B.H.; Kam, K.W.; Yu, M.; Cheng, C.Y.; Young, A.L.; et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: A population-based prospective study. Br. J. Ophthalmol. 2022, 106, 1772–1778. [Google Scholar] [CrossRef]
- Ma, M.; Xiong, S.; Zhao, S.; Zheng, Z.; Sun, T.; Li, C. COVID-19 home quarantine accelerated the progression of myopia in children aged 7 to 12 years in China. Invest. Ophthalmol. Vis. Sci. 2021, 62, 37. [Google Scholar] [CrossRef]
- Kim, H.; Shahraki, K.; Suh, D.W. Myopia trends among children and adolescents: A nationwide study in South Korea. J. AAPOS 2024, 28, 103969. [Google Scholar] [CrossRef]
- Acinikli, K.Y.; Erbaş, İ.M.; Besci, Ö.; Demir, K.; Abacı, A.; Böber, E. Has the frequency of precocious puberty and rapidly progressive early puberty increased in girls during the COVID-19 pandemic? J. Clin. Res. Pediatr. Endocrinol. 2022, 14, 302–307. [Google Scholar] [CrossRef]
- Yang, Y.; Liao, H.; Zhao, L.; Wang, X.; Yang, X.; Ding, X.; Li, X.; Jing, Z.; Zhang, X.; Zhang, Q.; et al. Green space morphology and school myopia in China. JAMA Ophthalmol. 2024, 142, 115–122. [Google Scholar] [CrossRef]
- Jeong, C.-E.; Lee, H.; Lee, J.E. Intake of energy and macronutrients according to household income among elementary, middle, and high school students before and during the COVID-19 pandemic: A cross-sectional study. Korean J. Community Nutr. 2024, 29, 234–252. [Google Scholar] [CrossRef] [PubMed]
- Lanza, M.; Ruggiero, A.; Ruggiero, M.; Iodice, C.M.; Simonelli, F. Analysis of refractive errors in a large Italian cohort of pediatric subjects post the COVID-19 pandemic. Life 2023, 13, 1569. [Google Scholar] [CrossRef] [PubMed]
- Peled, A.; Nitzan, I.; Megreli, J.; Derazne, E.; Tzur, D.; Pinhas-Hamiel, O.; Afek, A.; Twig, G. Myopia and BMI: A nationwide study of 1.3 million adolescents. Obesity 2022, 30, 1691–1698. [Google Scholar] [CrossRef]
- Kim, J.M.; Choi, Y.J. Association between dietary nutrient intake and prevalence of myopia in Korean adolescents: Evidence from the 7th KNHANES. Front. Pediatr. 2024, 11, 1285465. [Google Scholar] [CrossRef]
- Foreman, J.; Salim, A.T.; Praveen, A.; Fonseka, D.; Ting, D.S.W.; He, M.G.; Bourne, R.R.A.; Crowston, J.; Wong, T.Y.; Dirani, M. Association between digital smart device use and myopia: A systematic review and meta-analysis. Lancet Digit. Health 2021, 3, e806–e818. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Kim, C.S.; Park, J.M.; Gwon, S.S. Changes in the health status of children and adolescents before, during, and after the COVID-19 pandemic: Focus on health examination results. Korean J. Public Health Nurs. 2024, 38, 132–149. [Google Scholar] [CrossRef]
- Jin, E.; Lee, C.E.; Li, H.; Tham, Y.-C.; Chen, D.Z. Association between sleep and myopia in children and adolescents: A systematic review and meta-analysis. Graefes Arch. Clin. Exp. Ophthalmol. 2024, 262, 2027–2038. [Google Scholar] [CrossRef] [PubMed]
| Variables | Pre–COVID-19 (2016) | Post–COVID-19 (2021) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyperopia | Emmetropia | Mild Myopia | High Myopia | Total e | p | Hyperopia | Emmetropia | Mild Myopia | High Myopia | Total e | p | ||
| Refractive error | N | 20 | 100 | 505 | 66 | 19 | 93 | 329 | 49 | ||||
| mean ± SD | 1.24 ± 0.19 | −0.04 ± 0.03 | −2.78 ± 0.08 | −7.30 ± 0.17 | 0.74 ± 0.08 | −0.05 ± 0.03 | −2.64 ± 0.10 | −7.93 ± 0.31 | |||||
| range (D) | +0.50~+3.00 | −0.38~+0.38 | −5.88~−0.50 | −10.63~−6.00 | +0.50~+1.63 | −0.38~+0.38 | −5.88~−0.50 | −14.00~−6.00 | |||||
| Gender, n (%) a | Male | 9 (2.52) | 54 (13.23) | 261 (74.83) | 34 (9.42) | 358 (52.6) | 0.974 | 12 (3.97) | 53 (20.92) | 172 (65.23) | 21 (9.88) | 258 (51.0) | 0.612 |
| Female | 11 (2.51) | 46 (13.37) | 244 (73.54) | 32 (10.58) | 333 (47.4) | 7 (2.94) | 40 (17.37) | 157 (66.59) | 28 (13.10) | 232 (49.0) | |||
| Area of residence, n (%) a | Urban | 14 (1.97) | 82 (12.56) | 437 (75.4%) | 56 (9.99) | 589 (87.4) | 0.049 | 13 (3.06) | 71 (17.96) | 269 (66.79) | 42 (12.18) | 395 (85.7) | 0.198 |
| Rural | 6 (6.28) | 18 (18.42) | 68 (65.45) | 10 (9.86) | 102 (12.6) | 6 (5.85) | 22 (26.46) | 60 (60.56) | 7 (7.13) | 95 (14.3) | |||
| Age b | 12.91 ± 0.47 | 13.56 ± 0.38 | 14.29 ± 0.11 | 15.37 ± 0.33 | 0.000 | 12.29 ± 0.59 | 12.93 ± 0.30 | 13.87 ± 0.16 | 15.46 ± 0.33 | 0.000 | |||
| Height b | 159.49 ± 3.17 | 157.22 ± 1.35 | 161.73 ± 0.49 | 166.70 ± 1.30 | 0.000 | 152.10 ± 2.76 | 157.52 ± 1.50 | 161.89 ± 0.78 | 165.04 ± 1.14 | 0.000 | |||
| Weight b | 51.01 ± 2.80 | 51.23 ± 1.87 | 54.71 ± 0.72 | 63.57 ± 2.14 | 0.000 | 47.01 ± 3.15 | 53.63 ± 2.18 | 57.80 ± 1.40 | 60.05 ± 2.05 | 0.001 | |||
| BMI b | 19.83 ± 0.74 | 20.38 ± 0.53 | 20.65 ± 0.22 | 22.74 ± 0.64 | 0.009 | 19.91 ± 0.77 | 21.18 ± 0.64 | 21.73 ± 0.38 | 21.97 ± 0.69 | 0.125 | |||
| BMI Group, n (%) a | low | 2 (2.90) | 9 (16.64) | 48 (71.28) | 6 (9.18) | 65 (10.0) | 0.232 | - | 5 (17.59) | 18 (64.86) | 6 (17.55) | 29 (7.1) | 0.805 |
| normal | 16 (3.01) | 70 (12.78) | 356 (76.31) | 39 (7.91) | 481 (68.4) | 13 (4.29) | 59 (19.37) | 210 (65.15) | 29 (11.19) | 311 (63.5) | |||
| overweight | - | 8 (15.50) | 45 (71.12) | 8 (13.38) | 61 (8.8) | 1 (1.44) | 12 (21.07) | 40 (72.00) | 3 (5.49) | 56 (9.3) | |||
| obesity | 2 (1.33) | 13 (11.94) | 56 (67.51) | 13 (19.22) | 84 (12.8) | 5 (3.02) | 17 (18.41) | 60 (65.57) | 11 (13.00) | 93 (20.1) | |||
| Home income, (%) a | Q1 | 4 (3.66) | 4 (4.15) | 57 (82.82) | 7 (9.37) | 72 (11.8) | 0.051 | 1 (0.92) | 4 (7.76) | 25 (82.62) | 3 (8.70) | 33 (6.2) | 0.328 |
| Q2 | 3 (1.39) | 37 (21.25) | 118 (71.62) | 7 (5.73) | 165 (24.5) | 4 (2.62) | 23 (20.02) | 84 (65.88) | 11 (11.48) | 122 (25.4) | |||
| Q3 | 8 (3.47) | 27 (11.88) | 162 (74.14) | 23 (10.52) | 220 (31.7) | 11 (6.20) | 38 (21.17) | 118 (62.63) | 16 (10.00) | 183 (37.1) | |||
| Q4 | 5 (2.03) | 32 (12.06) | 167 (73.16) | 28 (12.75) | 232 (32.0) | 3 (1.43) | 28 (18.51) | 101 (66.29) | 19 (13.76) | 151 (31.3) | |||
| Sleep duration (hour) b,c,d | 7.87 ± 0.37 | 7.60 ± 0.15 | 7.62 ± 0.07 | 7.26 ± 0.19 | 0.261 | 8.41 ± 0.42 | 7.59 ± 0.24 | 7.49 ± 0.09 | 7.31 ± 0.20 | 0.047 | |||
| Rate of Perceived Stress, n(%) a,c,d | Yes | 8 (2.03) | 44 (10.46) | 278 (74.70) | 48 (12.81) | 378 (72.9) | 0.557 | 9 (2.90) | 48 (15.84) | 189 (66.71) | 34 (14.54) | 280 (77.0) | 0.895 |
| No | 2 (1.33) | 20 (14.31) | 107 (74.16) | 15 (10.21) | 144 (27.1) | 2 (1.65) | 13 (15.86) | 58 (69.23) | 11 (13.26) | 84 (23.0) | |||
| Average Daily Sedentary Time (hour) b,c,d | 9.77 ± 1.29 | 10.51 ± 0.36 | 10.89 ± 0.18 | 11.38 ± 0.37 | 0.290 | 10.53 ± 1.27 | 10.98 ± 0.35 | 11.38 ± 0.16 | 11.64 ± 0.35 | 0.499 | |||
| Near Work (hour), n (%) a,† | ≤1 | 1 (1.90) | 12 (26.46) | 28 (68.44) | 1 (3.20) | 42 (5.6) | 0.234 | 6 (6.08) | 19 (20.68) | 65 (63.84) | 9 (9.39) | 99 (19.8) | 0.785 |
| 1–2 h | 6 (2.47) | 32 (15.86) | 125 (74.86) | 13 (6.81) | 176 (24.9) | 2 (1.98) | 16 (22.40) | 45 (61.92) | 9 (13.70) | 72 (16.7) | |||
| 3 h | 4 (2.13) | 16 (11.50) | 121 (74.72) | 17 (11.64) | 158 (22.8) | 3 (4.58) | 7 (13.19) | 40 (66.25) | 7 (15.98) | 57 (13.5) | |||
| ≥4 | 9 (2.80) | 40 (11.22) | 231 (74.33) | 35 (11.65) | 315 (46.7) | 8 (2.62) | 51 (19.12) | 179 (67.95) | 24 (10.31) | 262 (50.0) | |||
| Near Work (hour), n (%) a,‡ | ≤1 | 2 (13.41) | 6 (35.02) | 13 (51.57) | - | 21 (3.6) | 0.050 | ||||||
| 1–2 h | 2 (2.13) | 18 (21.81) | 43 (70.46) | 4 (5.60) | 67 (13.9) | ||||||||
| 3 h | 3 (1.63) | 21 (22.71) | 74 (68.98) | 7 (6.68) | 105 (19.9) | ||||||||
| ≥4 | 12 (3.77) | 48 (16.56) | 199 (64.73) | 38 (14.94) | 297 (62.6) | ||||||||
| Variables (Reference) | Pre-COVID 19 (2016) | Post-COVID 19 (2021) | |||||
|---|---|---|---|---|---|---|---|
| B | 95% CI | p-Value | B | 95% CI | p-Value | ||
| Sex (Female) | 0.190 | −0.168~0.548 | 0.296 | 0.621 | 0.105~1.137 | 0.019 | |
| Town (rural) | −0.441 | −1.233~0.351 | 0.274 | −0.865 | −1.365~−0.365 | 0.001 | |
| Age | −0.193 | −0.275~−0.111 | 0.000 | −0.324 | −0.429~−0.218 | 0.000 | |
| BMI Group (normal) | Low | 0.648 | −0.102~1.399 | 0.090 | −1.327 | −2.394~−0.260 | 0.015 |
| Overweight | −0.340 | −1.087~0.408 | 0.372 | 0.252 | −0.669~1.173 | 0.589 | |
| Obesity | −0.741 | −1.373~−0.109 | 0.022 | −0.344 | −1.118~0.431 | 0.381 | |
| Home income (Q1, lowest) | Q2 | 0.455 | −0.194~1.104 | 0.169 | 0.537 | −0.411~1.485 | 0.270 |
| Q3 | 0.053 | −0.627~0.733 | 0.878 | 0.882 | 0.064~1.699 | 0.030 | |
| Q4 | −0.174 | −0.810~0.462 | 0.591 | 0.057 | −0.841~0.955 | 0.900 | |
| Sleep duration | 0.262 | 0.062~0.462 | 0.011 | 0.331 | 0.077~0.584 | 0.011 | |
| Rate of Perceived Stress (No) | 0.130 | −0.396~0.657 | 0.625 | −0.104 | −0.855~0.647 | 0.785 | |
| Average Daily Sedentary Time | −0.105 | −0.194~−0.017 | 0.020 | −0.063 | −0.164~0.039 | 0.225 | |
| Near Work 1 (≤1 h/day) † | 1–2 h | −0.845 | −1.659~−0.031 | 0.042 | 0.029 | −0.898~0.956 | 0.951 |
| 3 h | −1.150 | −2.035~−0.265 | 0.011 | −0.063 | −0.990~0.864 | 0.894 | |
| 4≤ | −1.171 | −1.951~−0.390 | 0.003 | −0.080 | −0.830~0.671 | 0.835 | |
| Near Work 2 (≤1 h/day) ‡ | 1–2 h | −0.853 | −2.359~0.654 | 0.266 | |||
| 3 h | −0.913 | −2.380~0.555 | 0.222 | ||||
| 4≤ | −1.542 | −2.998~−0.086 | 0.038 | ||||
| Variables (Reference) | Pre–COVID-19 (2016) | Post–COVID-19 (2021) | |||||
|---|---|---|---|---|---|---|---|
| B | 95% CI | p-Value | B | 95% CI | p-Value | ||
| Adjusted Mean | 0.915 | −0.517~2.347 | 0.208 | 3.866 | 2.247~5.485 | 0.000 | |
| Sex (Female) | 0.207 | −0.143~0.557 | 0.244 | −0.544 | −1.039~−0.050 | 0.031 | |
| Town (rural) | −0.434 | −1.156~0.288 | 0.237 | −0.685 | −1.229~−0.142 | 0.014 | |
| Age | −0.185 | −0.268~−0.102 | 0.000 | −0.312 | −0.422~−0.203 | 0.000 | |
| BMI Group (normal) | Low | 0.720 | 0.027~1.412 | 0.042 | −0.948 | −1.809~−0.088 | 0.031 |
| Overweight | −0.355 | −1.131~0.421 | 0.367 | −0.017 | −0.954~0.920 | 0.971 | |
| Obesity | −0.650 | −1.256~−0.044 | 0.036 | −0.407 | −1.169~0.355 | 0.292 | |
| Near Work time † (≤1 h/day) | 1–2 h | −0.716 | −1.436~0.032 | 0.060 | −1.612 | −2.986~−0.238 | 0.022 |
| 3 h | −0.853 | −1.666~−0.041 | 0.040 | −1.311 | −2.571~−0.051 | 0.042 | |
| 4≤ | −0.757 | −1.499~−0.016 | 0.045 | −1.167 | −2.094~−0.241 | 0.014 | |
| F(P) = 5.212(0.000), R2 = 7.9% | F(P) = 9.134(0.000), R2 = 13.4% | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Kim, S.R.; Park, M. Analysis of Risk Factor Changes for Myopia in Korean Adolescents Before and After the COVID-19 Pandemic. Medicina 2025, 61, 1798. https://doi.org/10.3390/medicina61101798
Lee S, Kim SR, Park M. Analysis of Risk Factor Changes for Myopia in Korean Adolescents Before and After the COVID-19 Pandemic. Medicina. 2025; 61(10):1798. https://doi.org/10.3390/medicina61101798
Chicago/Turabian StyleLee, Seeun, So Ra Kim, and Mijung Park. 2025. "Analysis of Risk Factor Changes for Myopia in Korean Adolescents Before and After the COVID-19 Pandemic" Medicina 61, no. 10: 1798. https://doi.org/10.3390/medicina61101798
APA StyleLee, S., Kim, S. R., & Park, M. (2025). Analysis of Risk Factor Changes for Myopia in Korean Adolescents Before and After the COVID-19 Pandemic. Medicina, 61(10), 1798. https://doi.org/10.3390/medicina61101798






