Embedded Ileal Fish Bone Removed via Deep Enteroscopy in a Patient with Abdominal Pain and Hematochezia: A Case Report
Abstract
1. Introduction
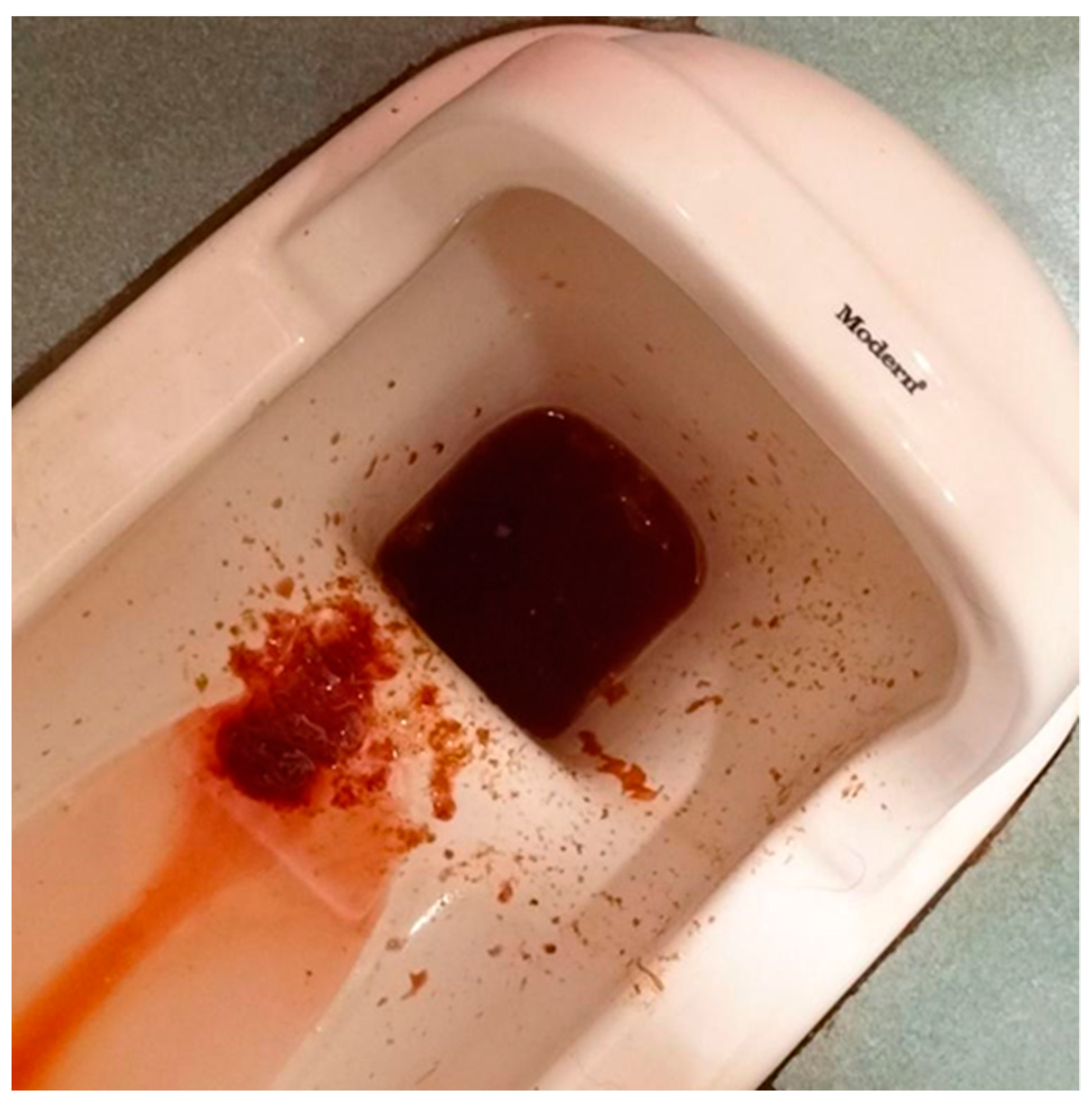
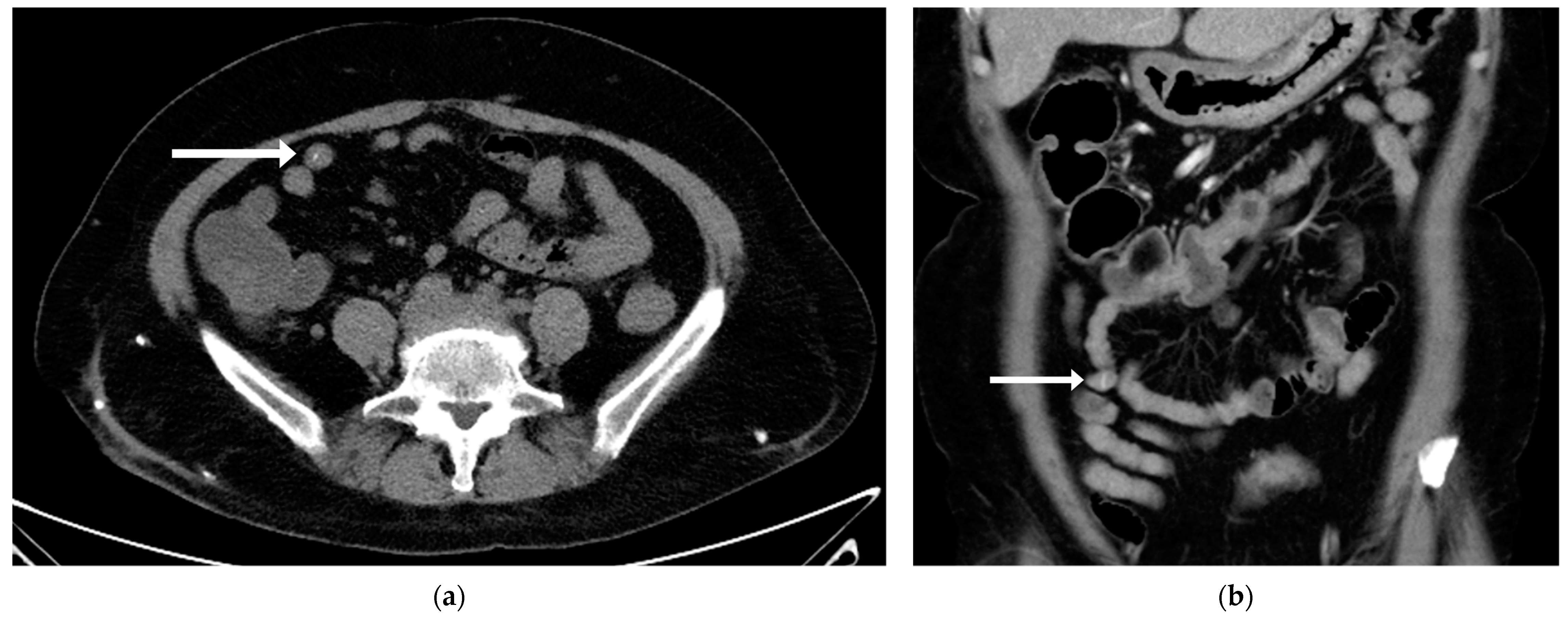
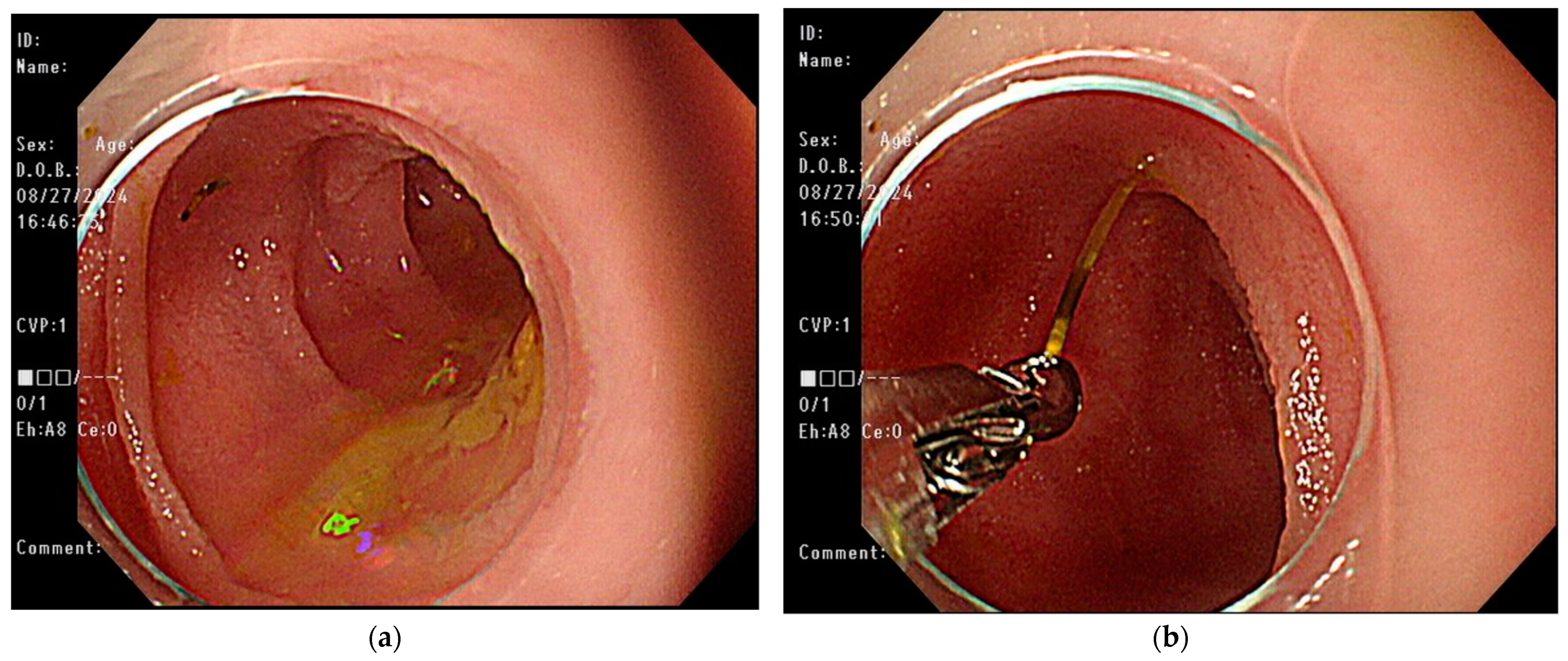
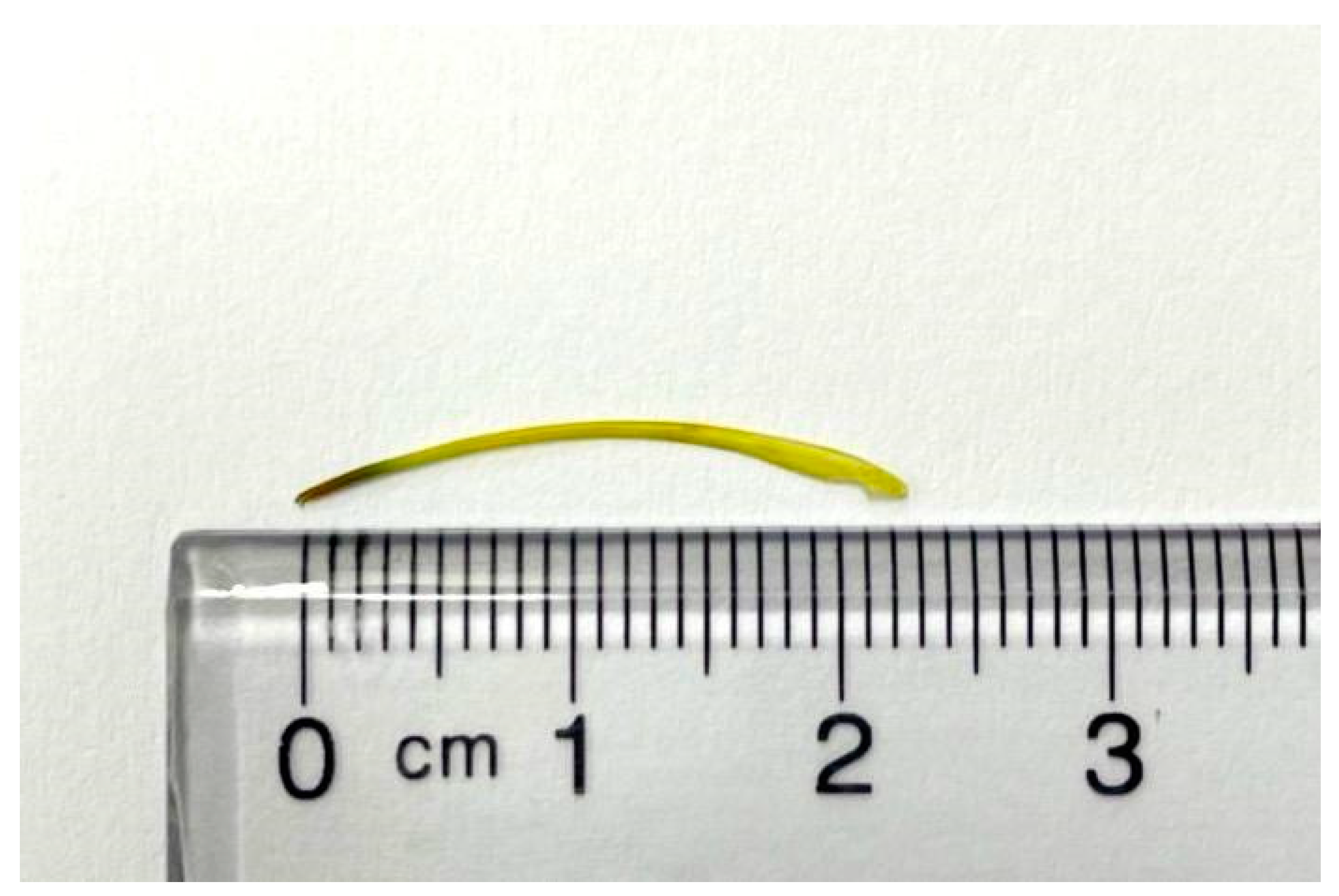
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Birk, M.; Bauerfeind, P.; Deprez, P.H.; Hafner, M.; Hartmann, D.; Hassan, C.; Hucl, T.; Lesur, G.; Aabakken, L.; Meining, A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Shishido, T.; Suzuki, J.; Ikeda, R.; Kobayashi, Y.; Katori, Y. Characteristics of fish-bone foreign bodies in the upper aero-digestive tract: The importance of identifying the species of fish. PLoS ONE 2021, 16, e0255947. [Google Scholar] [CrossRef] [PubMed]
- Bathla, G.; Teo, L.L.; Dhanda, S. Pictorial essay: Complications of a swallowed fish bone. Indian J. Radiol. Imaging 2011, 21, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Bekkerman, M.; Sachdev, A.H.; Andrade, J.; Twersky, Y.; Iqbal, S. Endoscopic Management of Foreign Bodies in the Gastrointestinal Tract: A Review of the Literature. Gastroenterol. Res. Pract. 2016, 2016, 8520767. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes-Costa, P.; Carvalho, L.; Rodrigues, J.P.; Tulio, M.A.; Marques, S.; Carmo, J.; Bispo, M.; Chagas, C. Endoscopic Management of Foreign Bodies in the Upper Gastrointestinal Tract: An Evidence-Based Review Article. GE Port. J. Gastroenterol. 2016, 23, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.U. Oroesophageal Fish Bone Foreign Body. Clin. Endosc. 2016, 49, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.P.; Kwon, O.J.; Shim, H.S.; Kim, R.B.; Kim, J.H.; Woo, S.H. Analysis of Clinical Feature and Management of Fish Bone Ingestion of Upper Gastrointestinal Tract. Clin. Exp. Otorhinolaryngol. 2015, 8, 261–267. [Google Scholar] [CrossRef]
- Mulita, F.; Papadopoulos, G.; Tsochatzis, S.; Kehagias, I. Laparoscopic removal of an ingested fish bone from the head of the pancreas: Case report and review of literature. Pan. Afr. Med. J. 2020, 36, 123. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Luo, X.; Zhang, J. Successful laparoscopic treatment for sustained abdominal pain due to fish bone migrating into the neck of the pancreas: A case report and thinking about surgical approach through the literature review. Surg. Case Rep. 2021, 7, 91. [Google Scholar] [CrossRef] [PubMed]
- Han, J.-H.; Cha, R.-R.; Kwak, J.-Y.; Jeon, H.; Lee, S.-S.; Jung, J.J.; Cho, J.K.; Kim, H.J. Two Cases of Severe Complications Due to an Esophageal Fish Bone Foreign Body. Medicina 2023, 59, 1504. [Google Scholar] [CrossRef]
- Yi, Z.; Chen, C.; Tuo, B.; Li, T.; Liu, X. An extremely dangerous case of acute massive upper gastrointestinal bleeding: A case report. BMC Gastroenterol. 2022, 22, 67. [Google Scholar] [CrossRef]
- Zhang, Y.Y.; Li, S.; Yuan, X.L.; Hu, B. Aorto-esophageal fistula caused by fishbone ingestion: A case report on staged endovascular and endoscopic treatment. BMC Gastroenterol. 2021, 21, 46. [Google Scholar] [CrossRef] [PubMed]
- Dung, L.T.; Duc, N.M.; My, T.T.; Linh, L.T.; Luu, V.D.; Thong, P.M. Cecum perforation due to a fish bone. Oxf. Med. Case Rep. 2021, 2021, omab025. [Google Scholar] [CrossRef] [PubMed]
- Elbakouri, A.; Yaqine, K.; Bouali, M.; Elhattabi, K.; Bensardi, F.; Fadil, A. Fish bone perforation of the small bowel: A case report. Ann. Med. Surg. 2021, 65, 102348. [Google Scholar] [CrossRef] [PubMed]
- Ngoc Nguyen, S.; Duy Nguyen, T.; Tung Vu, L.; Ngoc Bao Hoang, C. Intestinal perforation caused by fishbone in a child with the misdiagnosis of acute appendicitis: A case report. Clin. Case Rep. 2021, 9, e04584. [Google Scholar] [CrossRef]
- Shahid, F.; Abdalla, S.O.; Elbakary, T.; Elfaki, A.; Ali, S.M. Fish Bone Causing Perforation of the Intestine and Meckel’s Diverticulum. Case Rep. Surg. 2020, 2020, 8887603. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Yang, W.; Zhu, Y.; Fang, Y.; Qiu, J.; Qiu, J.; Lin, L.; Wu, W.; Lin, C.; Wang, Y. Ingested a fish bone-induced ileal perforation: A case report. Medicine 2020, 99, e19508. [Google Scholar] [CrossRef]
- Wang, X.; Su, S.; Chen, Y.; Wang, Z.; Li, Y.; Hou, J.; Zhong, W.; Wang, Y.; Wang, B. The removal of foreign body ingestion in the upper gastrointestinal tract: A retrospective study of 1,182 adult cases. Ann. Transl. Med. 2021, 9, 502. [Google Scholar] [CrossRef] [PubMed]
- Yi, L.; Cheng, Z.; Zhou, Y.; Wang, Q.; Liu, Y.; Liu, K.; Wang, T.; Zhong, X. Fishbone foreign body ingestion in duodenal papilla: A cause of abdominal pain resembling gastric ulcer. BMC Gastroenterol. 2020, 20, 323. [Google Scholar] [CrossRef] [PubMed]
- Koito, Y.; Asano, T.; Matsumoto, S.; Mashima, H. Endoscopic Mucosal Incision to Remove a Fish Bone Completely Embedded Under the Esophageal Mucosa: A Case Report and Literature Review. Am. J. Case Rep. 2022, 23, e936773. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, G.; Gu, Z.; Qiu, J.; Wu, C.; Wu, J.; Huang, W.; Shen, G.; Qian, Z. Laparoscopic diagnosis and extraction of an ingested fish bone that penetrated the stomach: A case report. Medicine 2019, 98, e18373. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, T.; Osada, T.; Asaoka, D.; Mori, H.; Beppu, K.; Sakamoto, N.; Suzuki, S.; Sai, J.K.; Nagahara, A.; Otaka, M.; et al. Double-balloon endoscopy for treatment of long-term abdominal discomfort due to small bowel penetration by an eel bone. Med. Sci. Monit. 2008, 14, Cs107–Cs109. [Google Scholar] [PubMed]
- Alkhatib, A.A.; Umar, S.B.; Patel, N.C.; Harrison, M.E. Balloon-assisted enteroscopy for the treatment of a sealed jejunal perforation: Removal of a penetrating fish bone (with video). Gastrointest. Endosc. 2013, 77, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Shimozaki, K.; Kimura, K.; Arahata, K.; Ito, A.; Takarabe, S.; Kaida, S.; Kishikawa, H.; Nishida, J.; Kanai, T. Removal of gastrointestinal foreign bodies (fish bones) by endoscopy. Prog. Dig. Endosc. 2016, 89, 120–121. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cortegoso Valdivia, P.; Skonieczna-Zydecka, K.; Elosua, A.; Sciberras, M.; Piccirelli, S.; Rullan, M.; Tabone, T.; Gawel, K.; Stachowski, A.; Leminski, A.; et al. Indications, Detection, Completion and Retention Rates of Capsule Endoscopy in Two Decades of Use: A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 1105. [Google Scholar] [CrossRef] [PubMed]
- Zagorowicz, E.S.; Pietrzak, A.M.; Wronska, E.; Pachlewski, J.; Rutkowski, P.; Kraszewska, E.; Regula, J. Small bowel tumors detected and missed during capsule endoscopy: Single center experience. World J. Gastroenterol. 2013, 19, 9043–9048. [Google Scholar] [CrossRef]
- Kim, J.; Lee, B.J.; Ham, N.S.; Oh, E.H.; Choi, K.D.; Ye, B.D.; Byeon, J.S.; Eun, C.S.; Kim, J.S.; Yang, D.H. Balloon-Assisted Enteroscopy for Retrieval of Small Intestinal Foreign Bodies: A KASID Multicenter Study. Gastroenterol. Res. Pract. 2020, 2020, 3814267. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Hirooka, Y.; Watanabe, O.; Yamamura, T.; Nagura, A.; Yoshimura, T.; Nakano, A.; Ando, T.; Ohmiya, N.; Goto, H. Minimally invasive extraction of a foreign body from the small intestine using double-balloon endoscopy. Nagoya J. Med. Sci. 2015, 77, 189–194. [Google Scholar]
| Author | Patient | Symptoms | Impaction Site | Management | Fish Bone Length | Outcome |
|---|---|---|---|---|---|---|
| Shibuya et al. [22] | 33/M | Postprandial discomfort in the upper abdomen | Jejunum | Antegrade DBE with forceps | 1.1 cm | Resolution of symptoms |
| Alkhatib et al. [23] | 67/M | LLQ dull abdominal pain, nausea, chills | Mid-jejunum | Antegrade DBE with a snare | 2.2 cm | Resolution of symptoms |
| Shimozaki et al. [24] | 49/F | Upper abdominal pain | Proximal jejunum | Antegrade SBE with forceps | N/A | Resolution of symptoms |
| Our case | 51/F | Lower abdominal cramping pain, hematochezia | Distal ileum | Retrograde SBE with forceps | 2.3 cm | Resolution of symptoms |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.-Y.; Chang, C.-F.; Huang, T.-Y.; Huang, I.-H. Embedded Ileal Fish Bone Removed via Deep Enteroscopy in a Patient with Abdominal Pain and Hematochezia: A Case Report. Medicina 2025, 61, 30. https://doi.org/10.3390/medicina61010030
Chen H-Y, Chang C-F, Huang T-Y, Huang I-H. Embedded Ileal Fish Bone Removed via Deep Enteroscopy in a Patient with Abdominal Pain and Hematochezia: A Case Report. Medicina. 2025; 61(1):30. https://doi.org/10.3390/medicina61010030
Chicago/Turabian StyleChen, Hsin-Yang, Chao-Feng Chang, Tien-Yu Huang, and I-Hsuan Huang. 2025. "Embedded Ileal Fish Bone Removed via Deep Enteroscopy in a Patient with Abdominal Pain and Hematochezia: A Case Report" Medicina 61, no. 1: 30. https://doi.org/10.3390/medicina61010030
APA StyleChen, H.-Y., Chang, C.-F., Huang, T.-Y., & Huang, I.-H. (2025). Embedded Ileal Fish Bone Removed via Deep Enteroscopy in a Patient with Abdominal Pain and Hematochezia: A Case Report. Medicina, 61(1), 30. https://doi.org/10.3390/medicina61010030






