Elevated Cardiac Troponin I as a Mortality Predictor in Hospitalised COVID-19 Patients
Abstract
1. Introduction
2. Materials and Methods
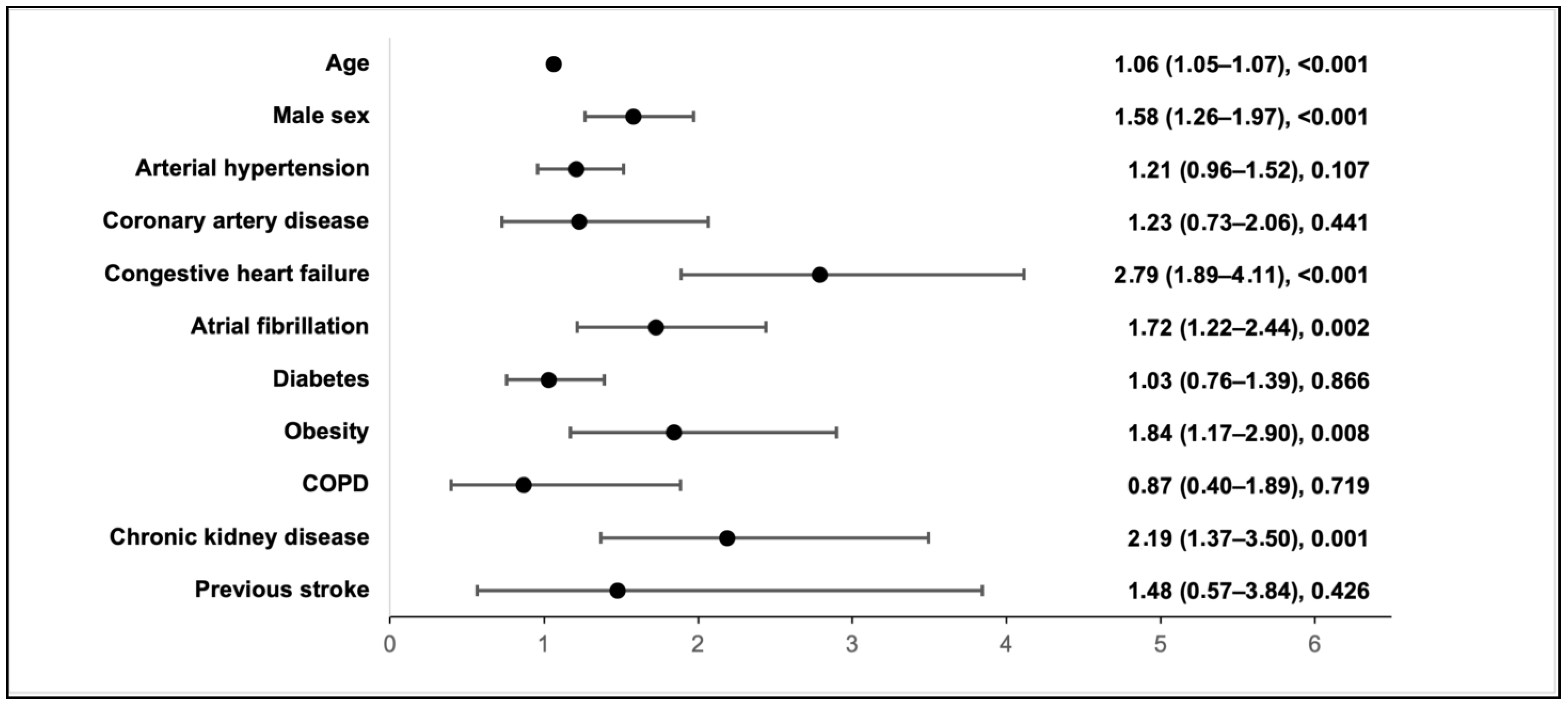
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fairweather, D.; Beetler, D.J.; Di Florio, D.N.; Musigk, N.; Heidecker, B.; Cooper, L.T. COVID-19, Myocarditis and Pericarditis. Circ. Res. 2023, 132, 1302–1319. [Google Scholar] [CrossRef] [PubMed]
- Devaux, C.A.; Camoin-Jau, L. An update on angiotensin-converting enzyme 2 structure/functions, polymorphism, and duplicitous nature in the pathophysiology of coronavirus disease 2019: Implications for vascular and coagulation disease associated with severe acute respiratory syndrome coronavirus infection. Front. Microbiol. 2022, 13, 1042200. [Google Scholar] [CrossRef] [PubMed]
- Lindner, D.; Fitzek, A.; Bräuninger, H.; Aleshcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.-P.; et al. Association of Cardiac Infection with SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020, 5, 1281. [Google Scholar] [CrossRef] [PubMed]
- Bearse, M.; Hung, Y.P.; Krauson, A.J.; Bonanno, L.; Boyraz, B.; Harris, C.K.; Helland, T.L.; Hilburn, C.F.; Hutchison, B.; Jobbagy, S.; et al. Factors associated with myocardial SARS-CoV-2 infection, myocarditis, and cardiac inflammation in patients with COVID-19. Mod. Pathol. 2021, 34, 1345–1357. [Google Scholar] [CrossRef] [PubMed]
- Terzic, C.M.; Medina-Inojosa, B.J. Cardiovascular Complications of Coronavirus Disease-2019. Phys. Med. Rehabil. Clin. North Am. 2023, 34, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Liu, F.; Wang, L. COVID-19 and cardiovascular diseases. J. Mol. Cell Biol. 2021, 13, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Vosko, I.; Zirlik, A.; Bugger, H. Impact of COVID-19 on Cardiovascular Disease. Viruses 2023, 15, 508. [Google Scholar] [CrossRef] [PubMed]
- Nandy, S.; Wan, S.-H.; Brenes-Salazar, J. Cardiovascular Manifestations of COVID-19. CCR 2021, 17, e230421187503. [Google Scholar] [CrossRef] [PubMed]
- Kubiliute, I.; Vitkauskaite, M.; Urboniene, J.; Svetikas, L.; Zablockiene, B.; Jancoriene, L. Clinical characteristics and predictors for in-hospital mortality in adult COVID-19 patients: A retrospective single center cohort study in Vilnius, Lithuania. PLoS ONE 2023, 18, e0290656. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef]
- Martens, C.R.; Accornero, F. Viruses in the Heart: Direct and Indirect Routes to Myocarditis and Heart Failure. Viruses 2021, 13, 1924. [Google Scholar] [CrossRef] [PubMed]
- Schultheiss, H.P.; Baumeier, C.; Pietsch, H.; Bock, C.T.; Poller, W.; Escher, F. Cardiovascular consequences of viral infections: From COVID to other viral diseases. Cardiovasc. Res. 2021, 117, 2610–2623. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, S.Z.; Tabassum, R.; Hamed, H.; Rehman, S.U.; Qadri, I. Hepatitis C Virus-Associated Extrahepatic Manifestations in Lung and Heart and Antiviral Therapy-Related Cardiopulmonary Toxicity. Viral Immunol. 2017, 30, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Zemaitis, L.; Alzbutas, G.; Gecyte, E.; Gecys, D.; Lesauskaite, V. SARS-CoV-2: Two Years in the Pandemic: What Have We Observed from Genome Sequencing Results in Lithuania? Microorganisms 2022, 10, 1229. [Google Scholar] [CrossRef]
- Battaglini, D.; Lopes-Pacheco, M.; Castro-Faria-Neto, H.C.; Pelosi, P.; Rocco, P.R.M. Laboratory Biomarkers for Diagnosis and Prognosis in COVID-19. Front. Immunol. 2022, 13, 857573. [Google Scholar] [CrossRef]
- Lala, A.; Johnson, K.W.; Januzzi, J.L.; Russak, A.J.; Paranjpe, I.; Richter, F.; Zhao, S.; Somani, S.; Van Vleck, T.; Vaid, A.; et al. Prevalence and Impact of Myocardial Injury in Patients Hospitalized with COVID-19 Infection. J. Am. Coll. Cardiol. 2020, 76, 533–546. [Google Scholar] [CrossRef] [PubMed]
- De Marzo, V.; Di Biagio, A.; Della Bona, R.; Vena, A.; Arboscello, E.; Emirjona, H.; Mora, S.; Giacomini, M.; Da Rin, G.; Pelosi, P.; et al. Prevalence and prognostic value of cardiac troponin in elderly patients hospitalized for COVID-19. J. Geriatr. Cardiol. 2021, 18, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, Y.; Januzzi, J.L.; Jaffe, A.S. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19. J. Am. Coll. Cardiol. 2020, 76, 1244–1258. [Google Scholar] [CrossRef]
- Li, C.; Jiang, J.; Wang, F.; Zhou, N.; Veronese, G.; Moslehi, J.J.; Ammirati, E.; Wang, D.W. Longitudinal correlation of biomarkers of cardiac injury, inflammation, and coagulation to outcome in hospitalized COVID-19 patients. J. Mol. Cell. Cardiol. 2020, 147, 74–87. [Google Scholar] [CrossRef]
- Metkus, T.S.; Sokoll, L.J.; Barth, A.S.; Czarny, M.J.; Hays, A.G.; Lowenstein, C.J.; Michos, E.D.; Nolley, E.P.; Post, W.S.; Resar, J.R.; et al. Myocardial Injury in Severe COVID-19 Compared with Non–COVID-19 Acute Respiratory Distress Syndrome. Circulation 2021, 143, 553–565. [Google Scholar] [CrossRef]
- Lombardi, C.M.; Carubelli, V.; Iorio, A.; Inciardi, R.M.; Bellasi, A.; Canale, C.; Camporotondo, R.; Catagnano, F.; Dalla Vecchia, L.A.; Giovinazzo, S.; et al. Association of Troponin Levels with Mortality in Italian Patients Hospitalized with Coronavirus Disease 2019: Results of a Multicenter Study. JAMA Cardiol. 2020, 5, 1274. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, N.; Sohrabi, C.; Merino, D.P.; Tyrlis, A.; Atieh, A.E.; Saberwal, B.; Lim, W.-Y.; Creta, A.; Khanji, M.; Rusinova, R.; et al. High sensitivity troponin and COVID-19 outcomes. Acta Cardiol. 2022, 77, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.; Osborne, V.; Lane, S.; Roy, D.; Dhanda, S.; Evans, A.; Shakir, S. Remdesivir in Treatment of COVID-19: A Systematic Benefit-Risk Assessment. Drug Saf. 2020, 43, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Nabati, M.; Parsaee, H. Potential Cardiotoxic Effects of Remdesivir on Cardiovascular System: A Literature Review. Cardiovasc. Toxicol. 2022, 22, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Rafaniello, C.; Ferrajolo, C.; Sullo, M.G.; Gaio, M.; Zinzi, A.; Scavone, C.; Gargano, F.; Coscioni, E.; Rossi, F.; Capuano, A. Cardiac Events Potentially Associated to Remdesivir: An Analysis from the European Spontaneous Adverse Event Reporting System. Pharmaceuticals 2021, 14, 611. [Google Scholar] [CrossRef] [PubMed]
- RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Caiazzo, E.; Rezig, A.O.M.; Bruzzese, D.; Ialenti, A.; Cicala, C.; Cleland, J.G.F.; Guzik, T.J.; Maffia, P.; Pellicori, P. Systemic administration of glucocorticoids, cardiovascular complications and mortality in patients hospitalised with COVID-19, SARS, MERS or influenza: A systematic review and meta-analysis of randomised trials. Pharmacol. Res. 2022, 176, 106053. [Google Scholar] [CrossRef]
- Chapman, A.R.; Bularga, A.; Mills, N.L. High-Sensitivity Cardiac Troponin Can Be an Ally in the Fight against COVID-19. Circulation 2020, 141, 1733–1735. [Google Scholar] [CrossRef]
- De Michieli, L.; Jaffe, A.S.; Sandoval, Y. Use and Prognostic Implications of Cardiac Troponin in COVID-19. Cardiol. Clin. 2022, 40, 287–300. [Google Scholar] [CrossRef] [PubMed]


| Demographic and Clinical Characteristic (N = 2019) | N (%) | Laboratory Characteristics | N | Median (IQR) |
|---|---|---|---|---|
| Age, years, median (IQR) | 60 (50–69) | Haemoglobin, g/L | 2019 | 140.0 (127.0–150.0) |
| Male | 1130 (55.97) | WBC, ×109/L | 2019 | 6.34 (4.76–8.61) |
| Female | 889 (44.03) | Neutrophils, ×109/L | 2019 | 4.66 (3.28–6.69) |
| Any comorbid condition | 1000 (49.53) | Lymphocytes, ×109/L | 2019 | 1.0 (0.71–1.40) |
| Arterial hypertension | 802 (39.72) | Platelets, ×109/L | 2019 | 195.0 (153.0–253.0) |
| Coronary artery disease | 79 (3.91) | cTnI | 2019 | 9.70 (5.0–23.0) |
| Congestive heart failure | 160 (7.92) | Glucose, mmol/L | 1984 | 6.22 (5.54–7.30) |
| Atrial fibrillation | 203 (10.05) | Creatinine, µmol/L | 2019 | 81.0 (67.0–100.0) |
| Diabetes mellitus | 277 (13.72) | eGFR, mL/min/1.73 m2 | 2019 | 84.0 (64.0–96.0) |
| Obesity | 106 (5.25) | Urea, mmol/L | 1883 | 5.50 (4.07–7.91) |
| COPD | 34 (1.68) | Sodium, mmol/L | 2019 | 140.0 (137.0–143.0) |
| Chronic kidney disease | 109 (5.40) | Potassium, mmol/L | 2019 | 4.20 (3.87–4.50) |
| Previous stroke | 23 (1.14) | ALT, U/L | 1993 | 33.0 (21.0–53.0) |
| Invasive mechanical ventilation | 170 (8.42) | AST, U/L | 1986 | 37.0 (26.98–57.0) |
| Treatment with antibiotics | 1514 (74.99) | LDH, U/L | 1910 | 308.0 (243.0–410.0) |
| Treatment with antivirals (Remdesivir) | 711 (35.22) | CRP, mg/L | 2018 | 63.25 (25.45–125.53) |
| Treatment with systemic steroids | 1371 (67.90) | Ferritin, µg/L | 1939 | 471.0 (235.00–1 002.0) |
| In-hospital mortality | 247 (12.23) | IL-6, ng/L | 1892 | 30.40 (15.01–57.30) |
| Length of hospital stay, days, median (IQR) | 11 (8–16) | D-dimer, µg/L | 1972 | 490.0 (295.0–910.0) |
| Characteristic | cTnI < 19 ng/L (N = 1416), n (%) | 19 ≤ cTnI ≤ 100 ng/L (N = 431), n (%) | cTnI > 100 ng/L (N = 172), n (%) | p-Value 1 | p-Value 2 | p-Value 3 |
|---|---|---|---|---|---|---|
| Age in years, median (IQR) | 57 (47–65) | 67 (58–77) | 74 (62–81) | <0.001 | <0.001 | <0.001 |
| Male | 771 (54.45) | 253 (58.70) | 106 (61.63) | 0.120 | 0.074 | 0.508 |
| Any underlying condition | 584 (41.24) | 287 (66.59) | 129 (75.00) | <0.001 | <0.001 | 0.044 |
| Hypertension | 481 (33.97) | 220 (51.04) | 101 (58.72) | <0.001 | <0.001 | 0.088 |
| Coronary artery disease | 33 (2.33) | 27 (6.26) | 19 (11.05) | <0.001 | <0.001 | 0.046 |
| Congestive heart failure | 50 (3.53) | 72 (16.71) | 38 (22.09) | <0.001 | <0.001 | 0.122 |
| Atrial fibrillation | 74 (5.23) | 81 (18.79) | 48 (27.91) | <0.001 | <0.001 | 0.014 |
| Diabetes | 160 (11.30) | 82 (19.03) | 35 (20.35) | <0.001 | 0.001 | 0.711 |
| Obesity | 63 (4.45) | 29 (6.73) | 14 (8.14) | 0.057 | 0.033 | 0.543 |
| COPD | 17 (1.20) | 11 (2.55) | 6 (3.49) | 0.044 | 0.031 | 0.587 |
| Chronic kidney disease | 37 (2.61) | 46 (10.67) | 26 (15.12) | <0.001 | <0.001 | 0.129 |
| Previous stroke | 7 (0.49) | 10 (2.32) | 6 (3.49) | 0.002 | 0.001 | 0.410 |
| Complications | ||||||
| Pulmonary embolism | 20 (1.41) | 17 (3.94) | 16 (9.30) | 0.001 | <0.001 | 0.009 |
| Stroke | 12 (0.85) | 15 (3.48) | 3 (1.74) | <0.001 | 0.216 | 0.258 |
| Remdesivir | 513 (36.23) | 162 (37.59) | 36 (20.93) | 0.608 | <0.001 | <0.001 |
| Systemic steroids | 961 (67.87) | 315 (73.09) | 95 (55.23) | 0.040 | 0.001 | <0.001 |
| Antibiotics use | 1066 (75.28) | 336 (77.96) | 112 (65.12) | 0.255 | 0.004 | 0.001 |
| Invasive ventilation | 61 (4.31) | 66 (15.31) | 43 (25.00) | <0.001 | <0.001 | 0.005 |
| Length of hospital stay, days | 11 (7–15) | 12 (8–19) | 13 (8–21) | <0.001 | 0.001 | 0.579 |
| In-hospital mortality | 76 (5.37) | 106 (24.59) | 65 (37.79) | <0.001 | <0.001 | 0.001 |
| Variable | cTnI < 19 ng/L (N = 1416), Median (IQR) | 19 ≤ cTnI ≤ 100 ng/L (N = 431), Median (IQR) | cTnI > 100 ng/L (N = 172), Median (IQR) | p-Value 1 | p-Value 2 | p-Value 3 |
|---|---|---|---|---|---|---|
| Haemoglobin, g/L | 142.00 (130.00–151.00) | 135.00 (121.00–147.00) | 133.00 (116.00–145.75) | <0.001 | <0.001 | 0.164 |
| WBC, ×109/L | 6.15 (4.65–8.06) | 6.72 (5.02–9.41) | 8.83 (6.08–12.38) | <0.001 | <0.001 | <0.001 |
| Neutrophils, ×109/L | 4.42 (3.14–6.15) | 4.95 (3.50–7.53) | 7.10 (4.38–10.23) | <0.001 | <0.001 | <0.001 |
| Lymphocytes, ×109/L | 1.04 (0.77–1.40) | 0.90 (0.60–1.39) | 0.80 (0.53–1.30) | <0.001 | <0.001 | 0.071 |
| Platelets, ×109/L | 195.00 (154.00–252.00) | 192.00 (151.00–245.00) | 207.00 (150.25–261.25) | 0.202 | 0.495 | 0.195 |
| Glucose, mmol/L | 6.07 (5.46–6.92) | 6.67 (5.82–8.23) | 7.64 (6.02–9.76) | <0.001 | <0.001 | 0.003 |
| Creatinine, µmol/L | 78.00 (65.00–91.00) | 92.00 (72.00–125.00) | 103.50 (77.00–148.75) | <0.001 | <0.001 | 0.018 |
| eGFR, mL/min/1.73 m2 | 88.00 (73.08–98.30) | 68.40 (43.60–89.00) | 57.20 (34.00–82.00) | <0.001 | <0.001 | 0.002 |
| Urea, mmol/L | 4.91 (3.74–6.48) | 7.37 (5.24–11.14) | 10.17 (6.68–16.25) | <0.001 | <0.001 | <0.001 |
| Sodium, mmol/L | 140.75 (137.88–143.00) | 140.00 (136.10–143.00) | 139.00 (135.00–142.00) | 0.001 | 0.002 | 0.386 |
| Potassium, mmol/: | 4.15 (3.90–4.50) | 4.20 (3.80–4.60) | 4.20 (3.85–4.60) | 0.468 | 0.075 | 0.314 |
| ALT, U/L | 33.00 (21.00–53.00) | 31.00 (19.35–50.00) | 32.50 (19.00–59.75) | 0.066 | 0.676 | 0.552 |
| AST, U/L | 35.00 (25.72–53.00) | 40.00 (29.08–61.07) | 50.00 (31.00–78.75) | <0.001 | <0.001 | 0.004 |
| LDH, U/L | 295.00 (236.00–388.00) | 335.00 (264.00–487.00) | 385.50 (280.75–564.75) | <0.001 | <0.001 | 0.031 |
| CRP, mg/L | 59.00 (24.43–108.90) | 85.60 (32.60–157.60) | 92.08 (19.88–146.30) | <0.001 | 0.003 | 0.486 |
| Ferritin, µg/L | 441.00 (225.50–952.55) | 543.00 (252.50–1115.50) | 543.29 (239.70–1286.73) | 0.011 | 0.046 | 0.739 |
| IL-6, ng/L | 27.70 (13.90–51.05) | 42.50 (19.85–71.05) | 34.15 (16.85–87.73) | <0.001 | 0.001 | 0.739 |
| D-dimer, µg/L | 430.00 (270.00–720.00) | 677.50 (410.00–1330.00) | 1 255.00 (587.50–2360.00) | <0.001 | <0.001 | <0.001 |
| Characteristic | In-Hospital Mortality | |
|---|---|---|
| HR (95% CI) | p-Value | |
| TnI < 19 ng/L | Reference | |
| 19 ≤ TnI ≤ 100 ng/L | 2.58 (1.83–3.62) | <0.001 |
| TnI > 100 ng/L | 2.97 (2.01–4.39) | <0.001 |
| Age in years | 1.05 (1.03–1.06) | <0.001 |
| Arterial hypertension | 0.71 (0.53–0.95) | 0.019 |
| Coronary artery disease | 1.03 (0.63–1.67) | 0.906 |
| Congestive heart failure | 1.81 (1.33–2.46) | <0.001 |
| Atrial fibrillation | 1.45 (1.06–1.98) | 0.021 |
| Diabetes | 0.92 (0.66–1.29) | 0.636 |
| Obesity | 2.40 (1.50–3.84) | <0.001 |
| COPD | 1.75 (0.96–3.18) | 0.068 |
| Chronic kidney disease | 0.70 (0.46–1.05) | 0.083 |
| Previous stroke | 1.67 (0.88–3.16) | 0.114 |
| Treatment with remdesivir | 0.61 (0.43–0.86) | 0.005 |
| Treatment with systemic steroids | 1.40 (1.00–1.96) | 0.051 |
| Antibiotics | 0.85 (0.59–1.24) | 0.413 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubiliute, I.; Urboniene, J.; Majauskaite, F.; Bobkov, E.; Svetikas, L.; Jancoriene, L. Elevated Cardiac Troponin I as a Mortality Predictor in Hospitalised COVID-19 Patients. Medicina 2024, 60, 842. https://doi.org/10.3390/medicina60060842
Kubiliute I, Urboniene J, Majauskaite F, Bobkov E, Svetikas L, Jancoriene L. Elevated Cardiac Troponin I as a Mortality Predictor in Hospitalised COVID-19 Patients. Medicina. 2024; 60(6):842. https://doi.org/10.3390/medicina60060842
Chicago/Turabian StyleKubiliute, Ieva, Jurgita Urboniene, Fausta Majauskaite, Edgar Bobkov, Linas Svetikas, and Ligita Jancoriene. 2024. "Elevated Cardiac Troponin I as a Mortality Predictor in Hospitalised COVID-19 Patients" Medicina 60, no. 6: 842. https://doi.org/10.3390/medicina60060842
APA StyleKubiliute, I., Urboniene, J., Majauskaite, F., Bobkov, E., Svetikas, L., & Jancoriene, L. (2024). Elevated Cardiac Troponin I as a Mortality Predictor in Hospitalised COVID-19 Patients. Medicina, 60(6), 842. https://doi.org/10.3390/medicina60060842







