A Comparative Study of Endoscopic versus Percutaneous Epidural Neuroplasty in Lower Back Pain: Outcomes at Six-Month Follow Up
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Inclusion and Exclusion Criteria
2.3. Outcome Assessments and Follow-Up
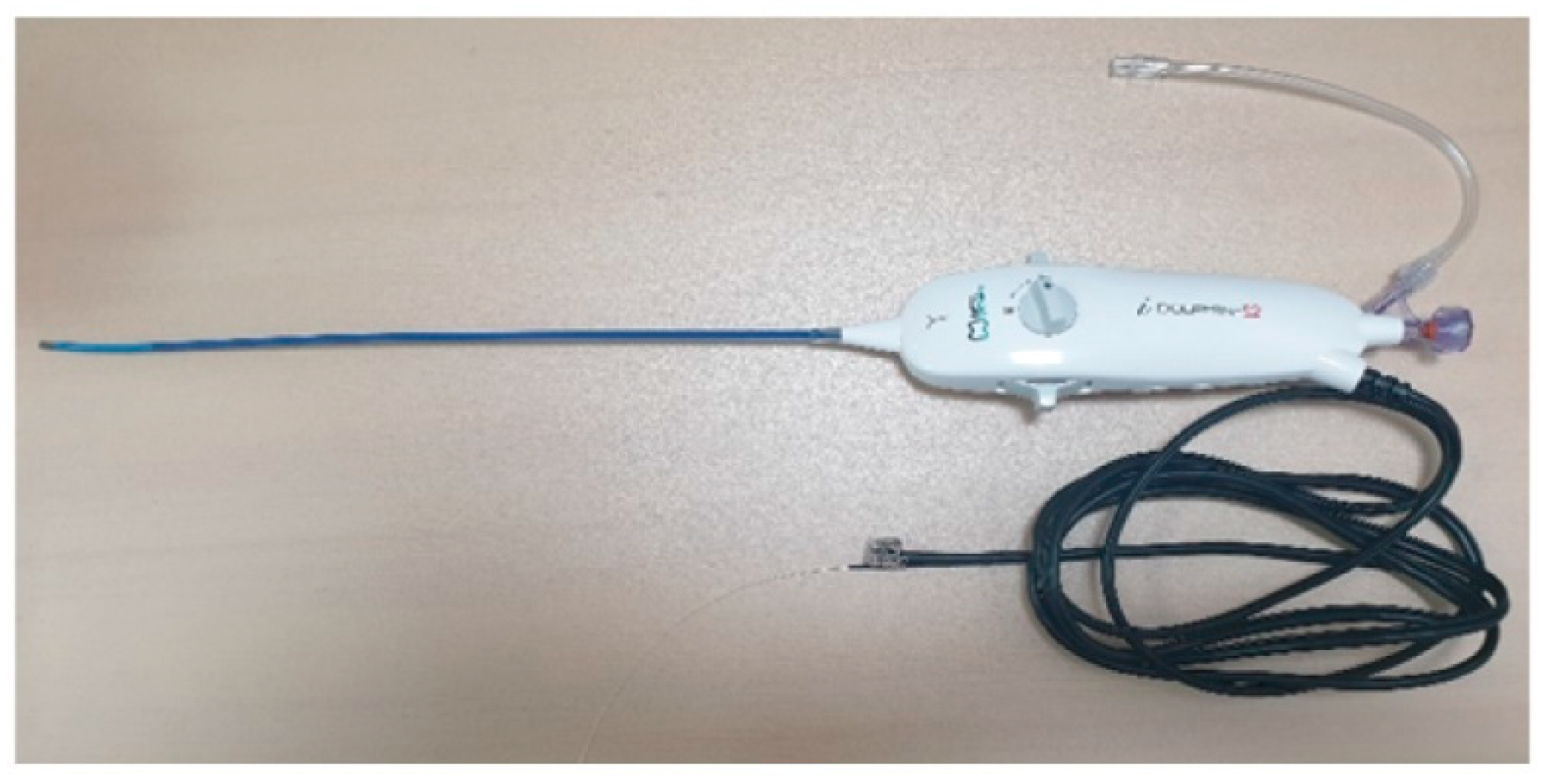
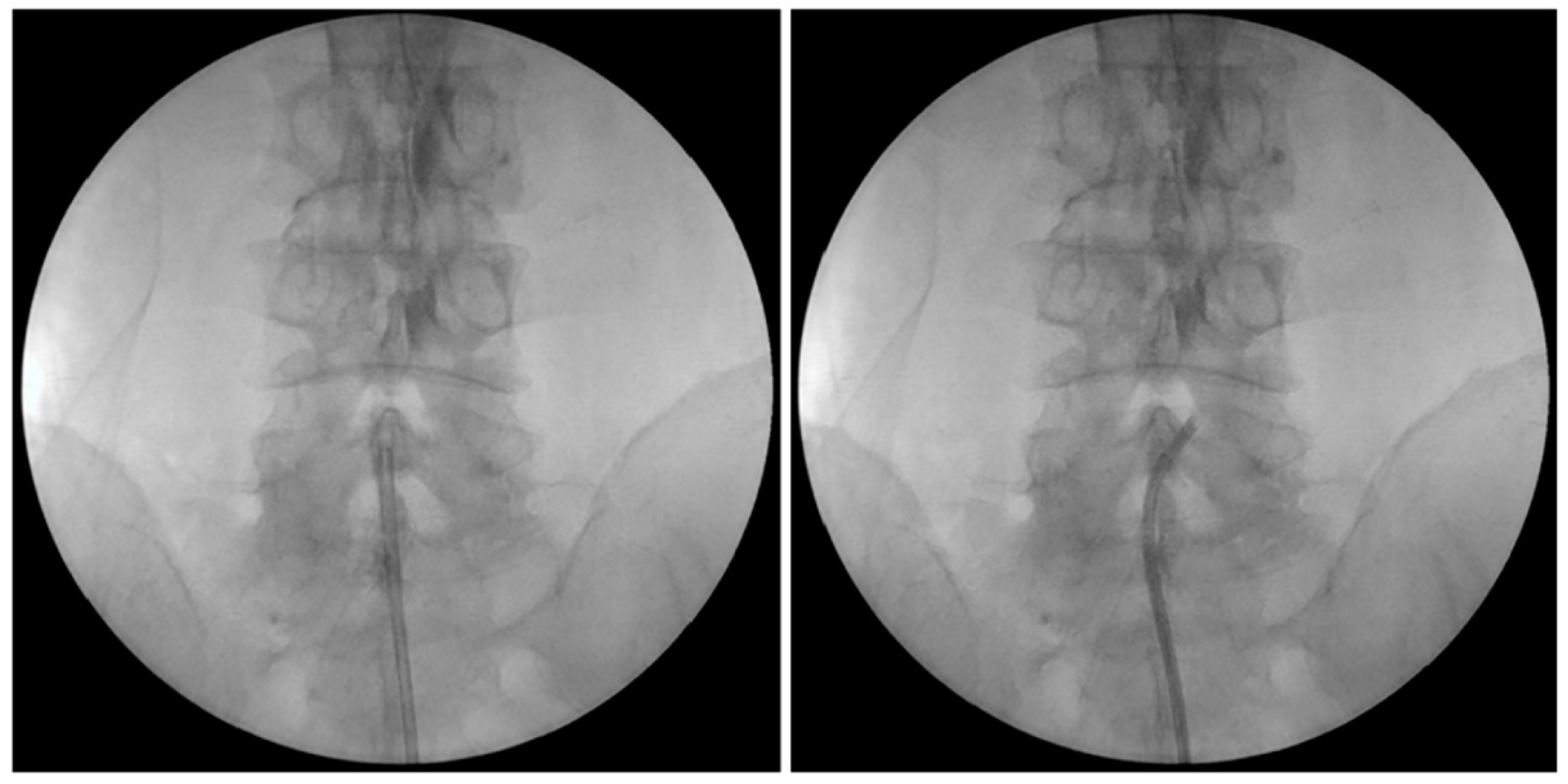
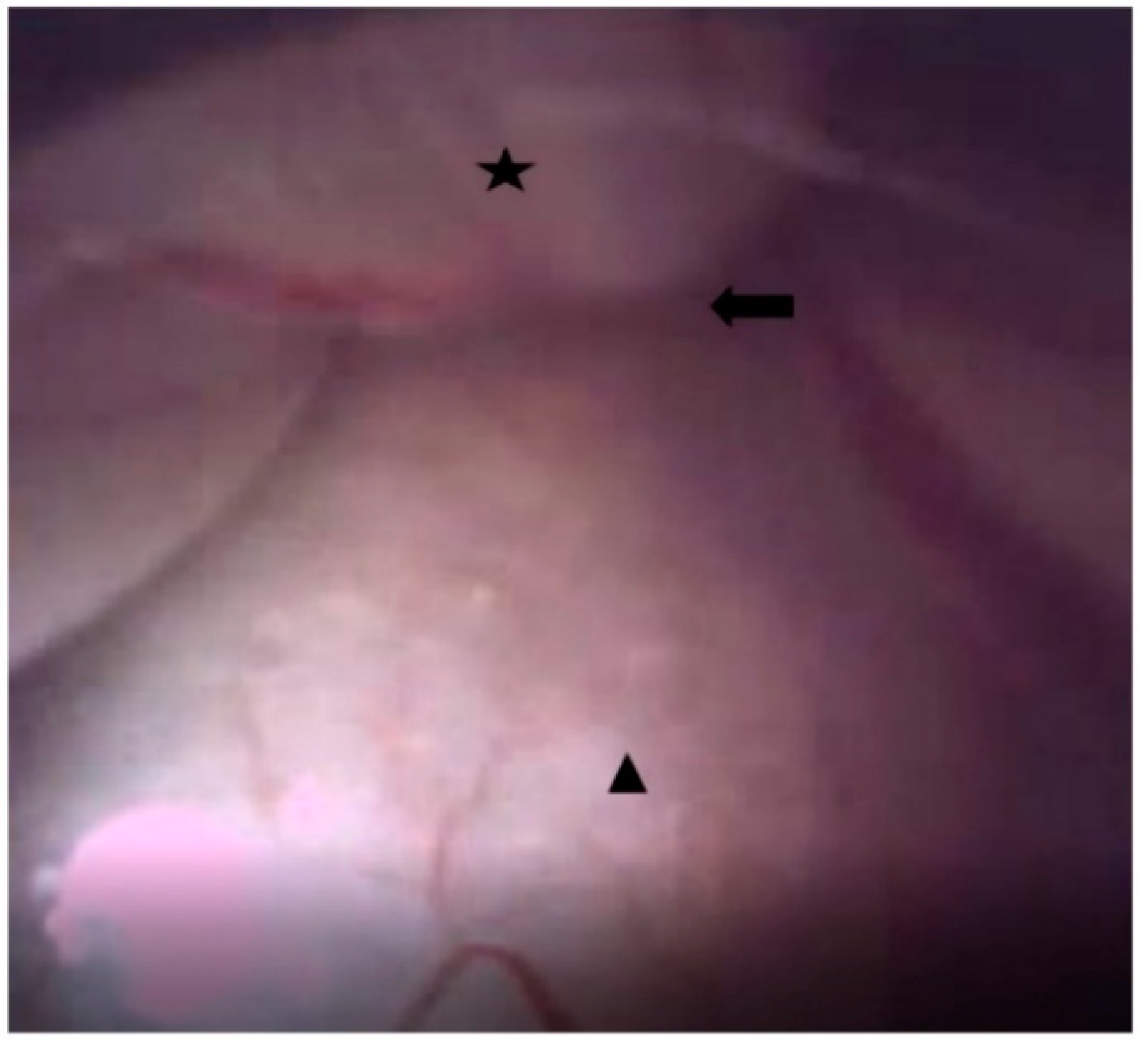
2.4. Endoscopic Epidural Neuroplasty
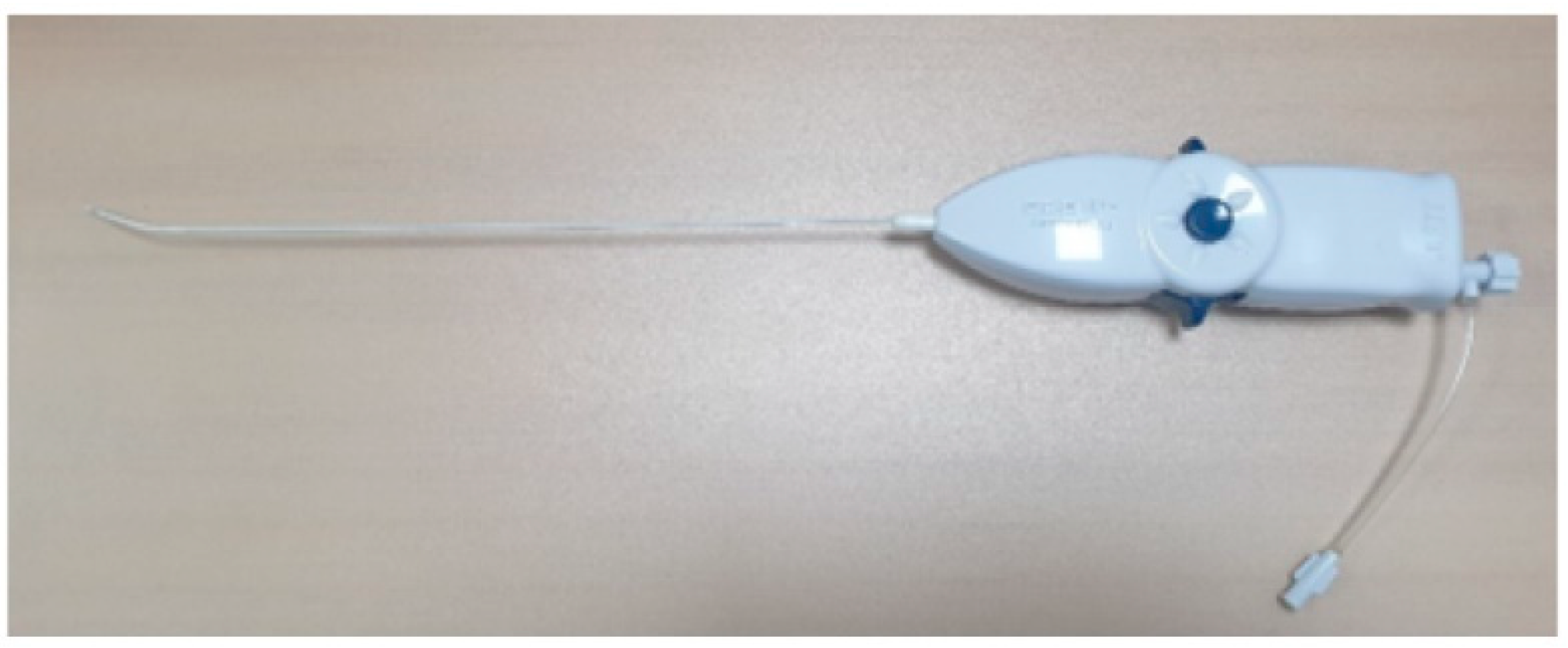
2.5. PEN with Steering Catheter
2.6. Statistical Analyses
3. Results
3.1. Participants
3.2. Clinical Outcomes
3.3. Factors Associated with Pain Relief
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moon, B.J.; Yi, S.; Ha, Y.; Kim, K.N.; Yoon, D.H.; Shin, D.A. Clinical Efficacy and Safety of Trans-Sacral Epiduroscopic Laser Decompression Compared to Percutaneous Epidural Neuroplasty. Pain Res. Manag. 2019, 2019, 2893460. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Pampati, V.; Bakhit, C.E.; Pakanati, R.R. Non-endoscopic and endoscopic adhesiolysis in post-lumbar laminectomy syndrome: A one-year outcome study and cost effectiveness analysis. Pain Physician 1999, 2, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Beyaz, S.G. Seizures and transient neurological deficits during epiduroscopy in a patient with failed back surgery syndrome. Pain Med. 2015, 16, 825–827. [Google Scholar] [CrossRef] [PubMed]
- Jo, D.H.; Kim, E.D.; Oh, H.J. The Comparison of the Result of Epiduroscopic Laser Neural Decompression between FBSS or Not. Korean J. Pain 2014, 27, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Avellanal, M.; Diaz-Reganon, G. Interlaminar approach for epiduroscopy in patients with failed back surgery syndrome. Br. J. Anaesth. 2008, 101, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Passavanti, Z.; Leschka, S.; Wildermuth, S.; Forster, T.; Dietrich, T.J. Differentiating epidural fibrosis from disc herniation on contrast-enhanced and unenhanced MRI in the postoperative lumbar spine. Skelet. Radiol. 2020, 49, 1819–1827. [Google Scholar] [CrossRef] [PubMed]
- Helm, S., II; Racz, G.B.; Gerdesmeyer, L.; Justiz, R.; Hayek, S.M.; Kaplan, E.D.; El Terany, M.A.; Knezevic, N.N. Percutaneous and Endoscopic Adhesiolysis in Managing Low Back and Lower Extremity Pain: A Systematic Review and Meta-analysis. Pain Physician 2016, 19, E245–E282. [Google Scholar] [CrossRef] [PubMed]
- Dhagat, P.K.; Jain, M.; Singh, S.N.; Arora, S.; Leelakanth, K. Failed Back Surgery Syndrome: Evaluation with Magnetic Resonance Imaging. J. Clin. Diagn. Res. JCDR 2017, 11, Tc06–Tc09. [Google Scholar] [CrossRef] [PubMed]
- Hazer, D.B.; Acarbaş, A.; Rosberg, H.E. The outcome of epiduroscopy treatment in patients with chronic low back pain and radicular pain, operated or non-operated for lumbar disc herniation: A retrospective study in 88 patients. Korean J. Pain 2018, 31, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.S.; Bae, J.Y.; In, C.B.; Choi, E.J.; Lee, P.B.; Nahm, F.S. Epiduroscopic Removal of a Lumbar Facet Joint Cyst. Korean J. Pain 2015, 28, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Rabinovitch, D.L.; Peliowski, A.; Furlan, A.D. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. Off. J. N. Am. Spine Soc. 2009, 9, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.B.; Heavner, J.E. Visual impairment following epidural fluid injections and epiduroscopy: A review. Pain Med. 2005, 6, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Jo, D.H. Epiduroscopy as a Diagnostic Tool for the Lower Back Pain and/or Leg Pain. Korean J. Pain 2016, 29, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Marchesini, M.; Flaviano, E.; Bellini, V.; Baciarello, M.; Bignami, E.G. Complication of epiduroscopy: A brief review and case report. Korean J. Pain 2018, 31, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Zaed, I.; Bossi, B.; Ganau, M.; Tinterri, B.; Giordano, M.; Chibbaro, S. Current state of benefits of Enhanced Recovery After Surgery (ERAS) in spinal surgeries: A systematic review of the literature. Neurochirurgie 2022, 68, 61–68. [Google Scholar] [CrossRef] [PubMed]

| Parameters | EEN (N = 73) | PEN (N = 34) | p-Value | |
|---|---|---|---|---|
| Age (Mean, years) | 56.20 ± 17.04 | 67.5 ± 14.04 | 0.003 * | |
| Sex (M:F) | 43:30 | 19:15 | 0.304 | |
| Height (cm) | 163.15 ± 30.66 | 162.35 ± 8.52 | 0.887 | |
| Weight (kg) | 69.72 ± 18.65 | 65.94 ± 8.50 | 0.309 | |
| BMI (kg/m2) | 25.19 ± 3.19 | 25.00 ± 2.56 | 0.794 | |
| Procedure time (min) | 66.84 ± 13.87 | 32.21 ± 6.05 | <0.001 * | |
| Diagnosis N (%) | Herniated lumbar disc | 43 (0.59) | 19 (0.56) | 0.772 |
| Spinal stenosis (mild/moderate/severe, number) | 18 (0.25) (0:10:8) | 11 (0.32) (0:6:5) | ||
| Post spinal surgery syndrome | 12 (0.16) | 4 (0.12) | ||
| Laser used N(%) | 6 (0.10) | 0 | ||
| Used saline (mL) | 131.31 ± 20.96 | 0 | ||
| Medication | Before EEN | 6 Months after EEN | p Value | |
| EEN | Gabapentin dose (mg) | 722.6 ± 259.9 | 651.6 ± 206.1 | 0.2462 |
| Pregabalin dose (mg) | 275 ± 170.6 | 260.3 ± 156.9 | 0.6721 | |
| Tramadol dose (mg) | 116.1 ± 48.5 | 108.4 ± 42.4 | 0.3119 | |
| Buprenorphine patch dose (µg/h) | 7.5 ± 4.5 | 7.3 ± 3.9 | 0.8615 | |
| Oxycodon dose (mg) | 30 ± 10 | 25 ± 9.6 | 0.4382 | |
| Fentanyl patch dose (µg/h) | 20.8 ± 5.9 | 20.8 ± 5.9 | 1 | |
| Medication | Before PEN | 6 Months after PEN | p Value | |
| PEN | Gabapentin dose (mg) | 543.8 ± 264.5 | 475 ± 188.7 | 0.4197 |
| Pregabalin dose (mg) | 276.4 ± 168 | 251.4 ± 132.9 | 0.6337 | |
| Tramadol dose (mg) | 120.5 ± 36.6 | 117.9 ± 37.1 | 0.7906 | |
| Buprenorphine patch dose (µg/h) | 7.5 ± 2.5 | 5.6 ± 1.7 | 0.1235 | |
| Oxycodon dose (mg) | 20 ± 0 | 18.3 ± 2.4 | 0.4227 | |
| Fentanyl patch dose (µg/h) | none | none | none | |
| p Value | Medication | Before PEN | 6 Months after PEN | p Value |
| (EEN vs. PEN) | Gabapentin dose (mg) | 0.03984 * | 0.0072 * | - |
| Pregabalin dose (mg) | 0.9771 | 0.8237 | - | |
| Tramadol dose (mg) | 0.6265 | 0.2821 | - | |
| Buprenorphine patch dose (µg/h) | 1 | 0.1311 | - | |
| Oxycodon dose (mg) | 0.0756 | 0.1949 | ||
| Fentanyl patch dose (µg/h) | none | none |
| Characteristics | Level | PEN | EEN | |
|---|---|---|---|---|
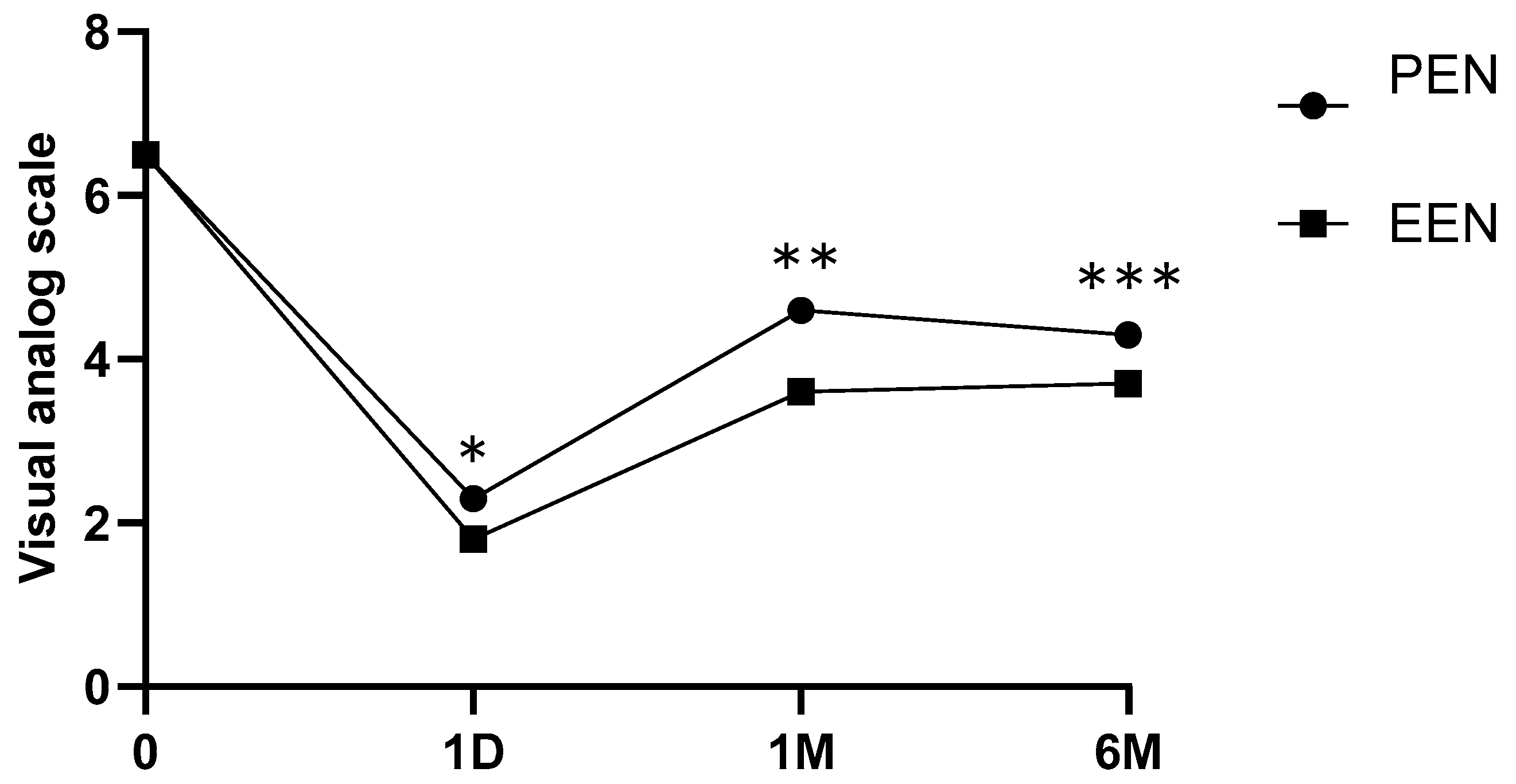
| VAS | Time | N (%) | 34 (0.3) | 73 (0.7) |
| Pre | 6.5 (0.8) | 6.5 (0.9) | ||
| immediate_Post | 2.3 (0.7) | 1.8 (0.7) | ||
| 1 mon | 4.6 (1.0) | 3.6 (0.7) | ||
| 6 mon | 4.3 (0.7) | 3.7 (0.8) | ||
| Age | Mean (SD) | 67.5 (14.6) | 55.7 (17.4) | |
| Sex | N (%) | 34 (0.3) | 73 (0.7) | |
| M | 19 (55.9) | 43 (58.9) | ||
| F | 15 (44.1) | 30 (41.1) | ||
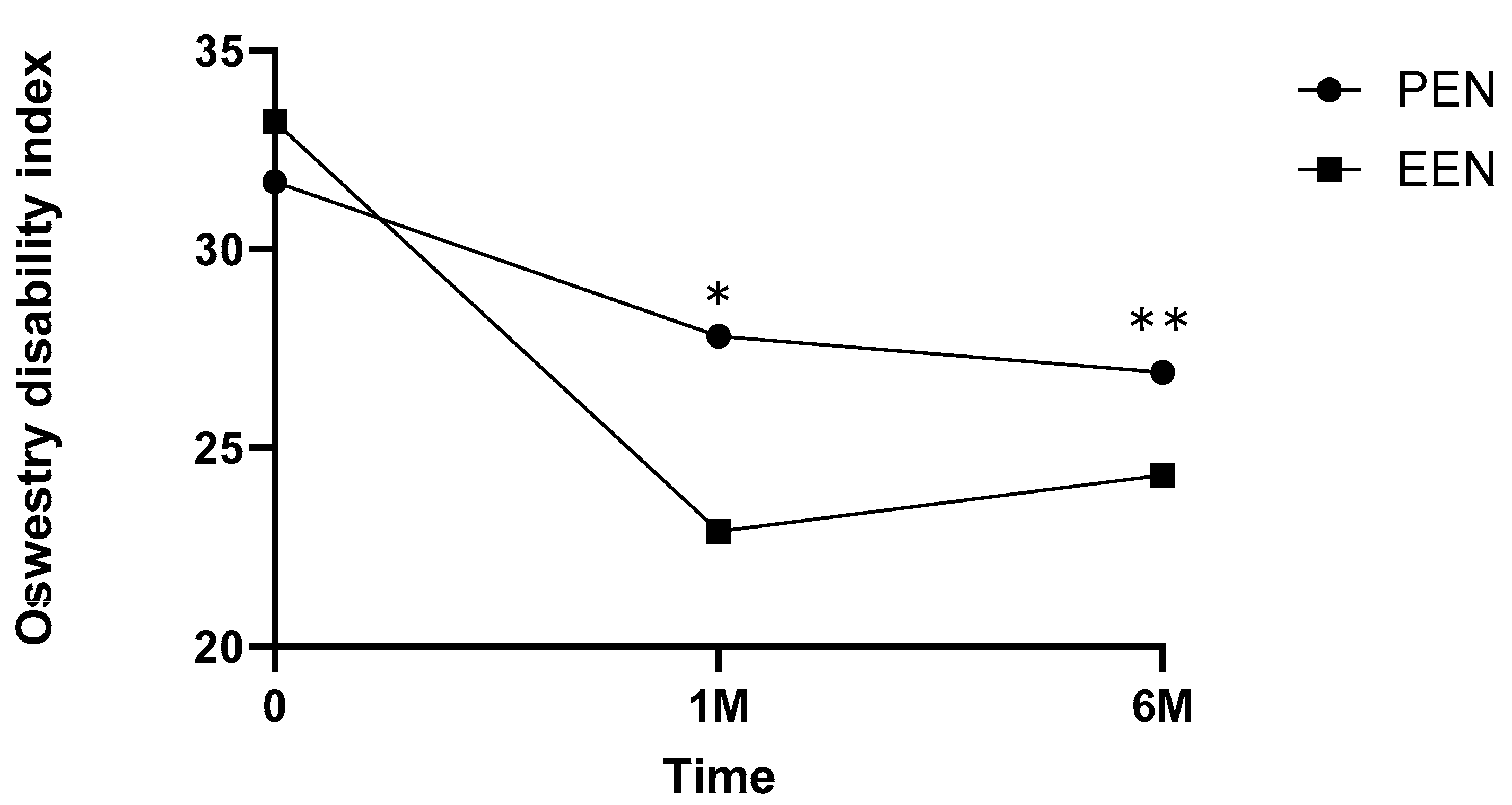
| ODI | Time | N (%) | 34 (0.3) | 73 (0.7) |
| Pre | 31.7 (3.6) | 33.2 (3.0) | ||
| 1 mon | 27.8 (1.8) | 22.9 (2.2) | ||
| 6 mon | 26.9 (2.3) | 24.3 (3.2) | ||
| Age | Mean (SD) | 67.5 (14.6) | 55.7 (17.4) | |
| Sex | N (%) | 34 (0.3) | 73 (0.7) | |
| M | 19 (55.9) | 43 (58.9) | ||
| F | 15 (44.1) | 30 (41.1) |
| Independent Variable | Dependent Variable | Beta (95% CI) | p-Value | |
|---|---|---|---|---|
| Saline volume | VAS | 1 day | −0.003472 | 0.019 * |
| 1 month | 0.0010754 | 0.157 | ||
| 6 months | 0.0000911 | 0.925 | ||
| ODI | 1 month | 0.0007815 | 0.331 | |
| 6 months | 0.001533 | 0.039 * | ||
| Procedure time | VAS | 1 day | −0.002024 | 0.222 |
| 1 month | 0.0017468 | 0.075 | ||
| 6 months | 0.002609 | 0.036 * | ||
| ODI | 1 month | 0.0000558 | 0.953 | |
| 6 months | 0.001148 | 0.263 | ||
| Age | VAS | 1 day | 0.005128 | 0.003 * |
| 1 month | 0.000629 | 0.503 | ||
| 6 months | 0.001043 | 0.371 | ||
| ODI | 1 month | −0.0004532 | 0.650 | |
| 6 months | 0.0002543 | 0.790 | ||
| Body mass index | VAS | 1 day | −0.0186 | 0.119 |
| 1 month | −0.002268 | 0.708 | ||
| 6 months | −0.009225 | 0.223 | ||
| ODI | 1 month | 0.006302 | 0.271 | |
| 6 months | 0.002679 | 0.636 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.B.; Koh, J.C.; Jo, D.; Kim, J.H.; Chang, W.S.; Lim, K.T.; Lee, H.G.; Moon, H.S.; Kim, E.; Lee, S.Y.; et al. A Comparative Study of Endoscopic versus Percutaneous Epidural Neuroplasty in Lower Back Pain: Outcomes at Six-Month Follow Up. Medicina 2024, 60, 839. https://doi.org/10.3390/medicina60050839
Choi JB, Koh JC, Jo D, Kim JH, Chang WS, Lim KT, Lee HG, Moon HS, Kim E, Lee SY, et al. A Comparative Study of Endoscopic versus Percutaneous Epidural Neuroplasty in Lower Back Pain: Outcomes at Six-Month Follow Up. Medicina. 2024; 60(5):839. https://doi.org/10.3390/medicina60050839
Chicago/Turabian StyleChoi, Jong Bum, Jae Chul Koh, Daehyun Jo, Jae Hyung Kim, Won Sok Chang, Kang Taek Lim, Hyung Gon Lee, Ho Sik Moon, Eunsoo Kim, Sun Yeul Lee, and et al. 2024. "A Comparative Study of Endoscopic versus Percutaneous Epidural Neuroplasty in Lower Back Pain: Outcomes at Six-Month Follow Up" Medicina 60, no. 5: 839. https://doi.org/10.3390/medicina60050839
APA StyleChoi, J. B., Koh, J. C., Jo, D., Kim, J. H., Chang, W. S., Lim, K. T., Lee, H. G., Moon, H. S., Kim, E., Lee, S. Y., Park, K., Choi, Y. H., Park, S. J., Oh, J., Lee, S. Y., Park, B., Jun, E. K., Ko, Y. S., Kim, J. S., ... Kim, N. E. (2024). A Comparative Study of Endoscopic versus Percutaneous Epidural Neuroplasty in Lower Back Pain: Outcomes at Six-Month Follow Up. Medicina, 60(5), 839. https://doi.org/10.3390/medicina60050839






