Insights from Chilean NCDs Hospitalization Data during COVID-19
Abstract
1. Introduction
2. Materials and Methods
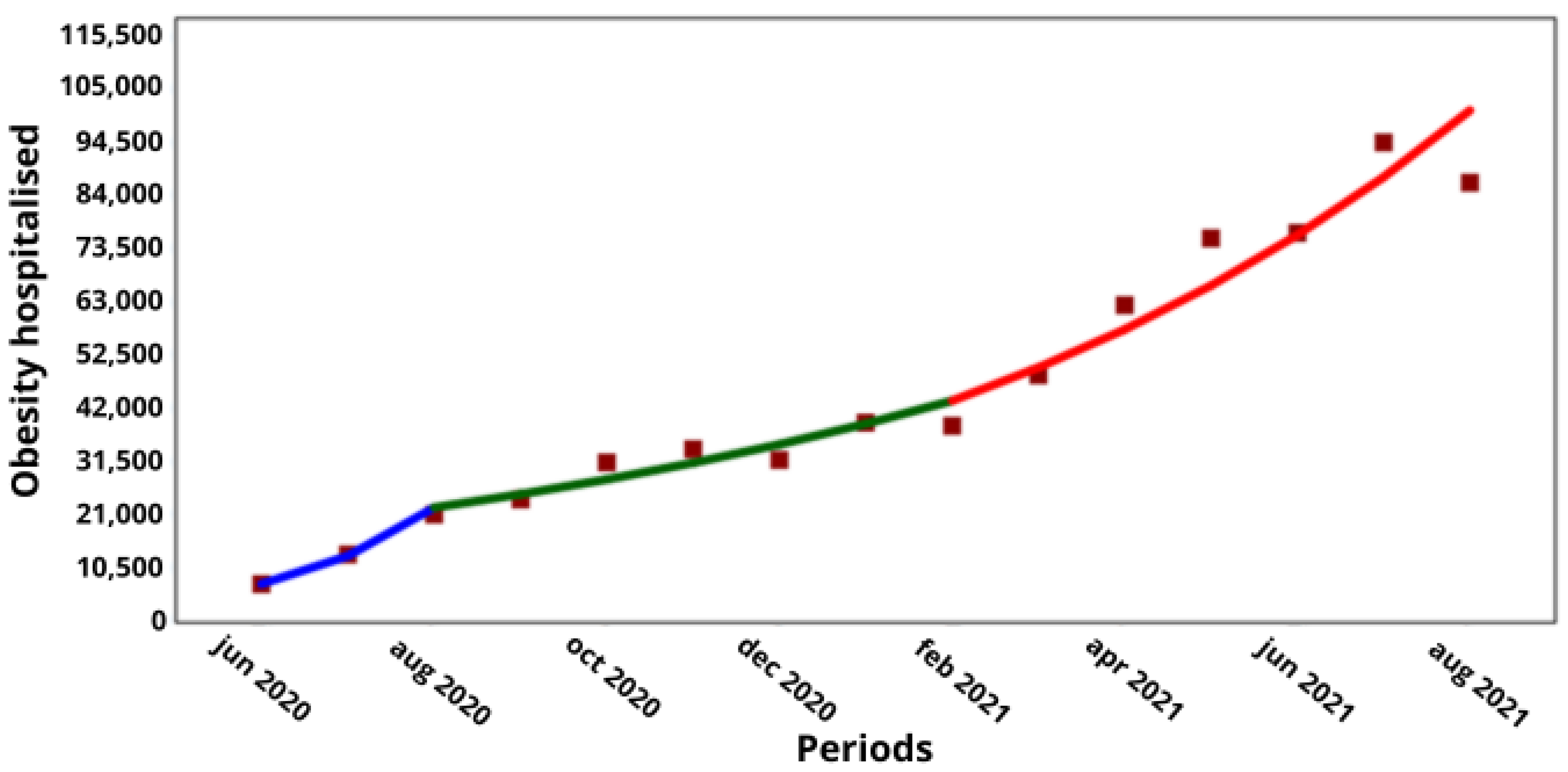
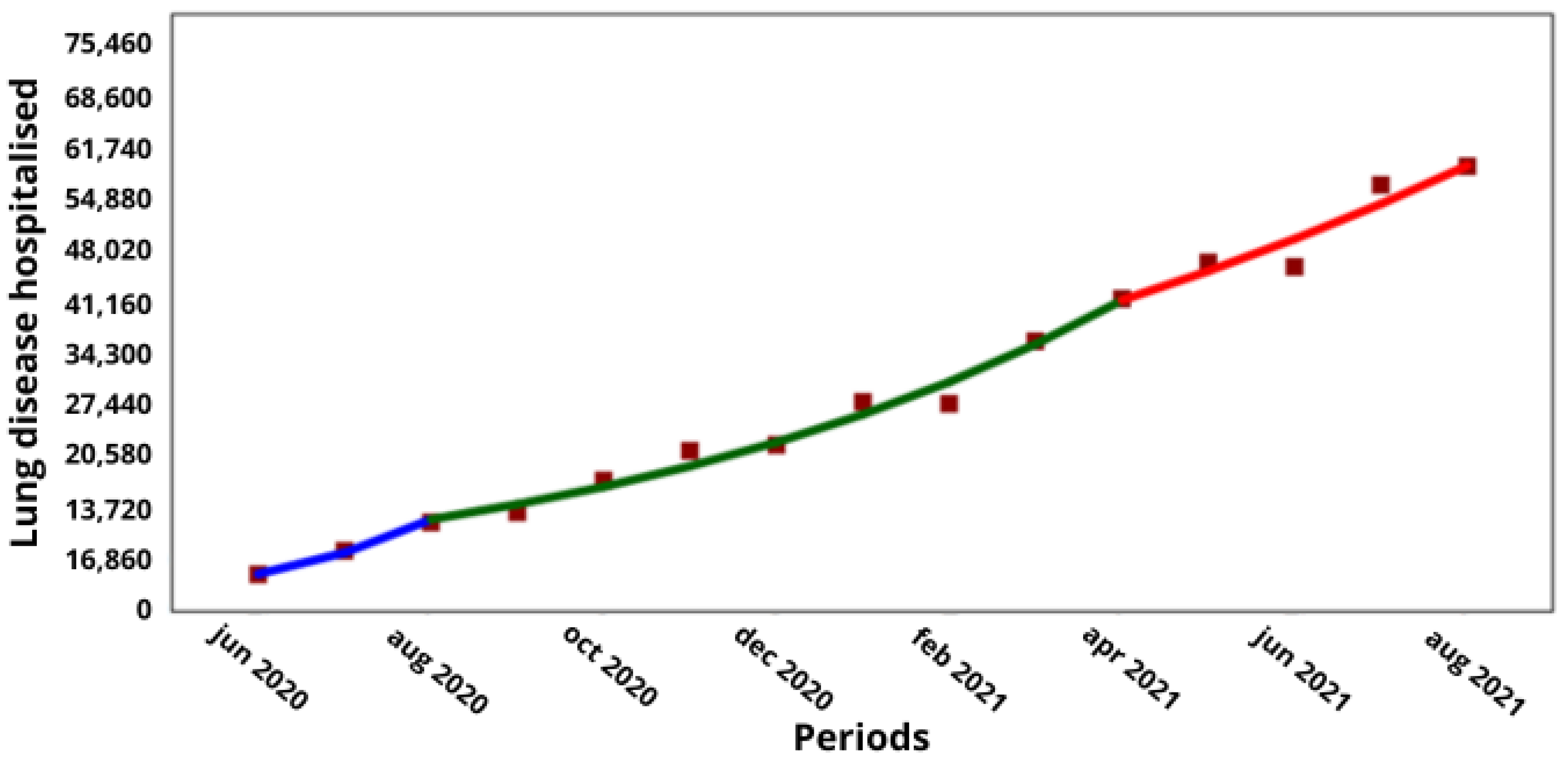
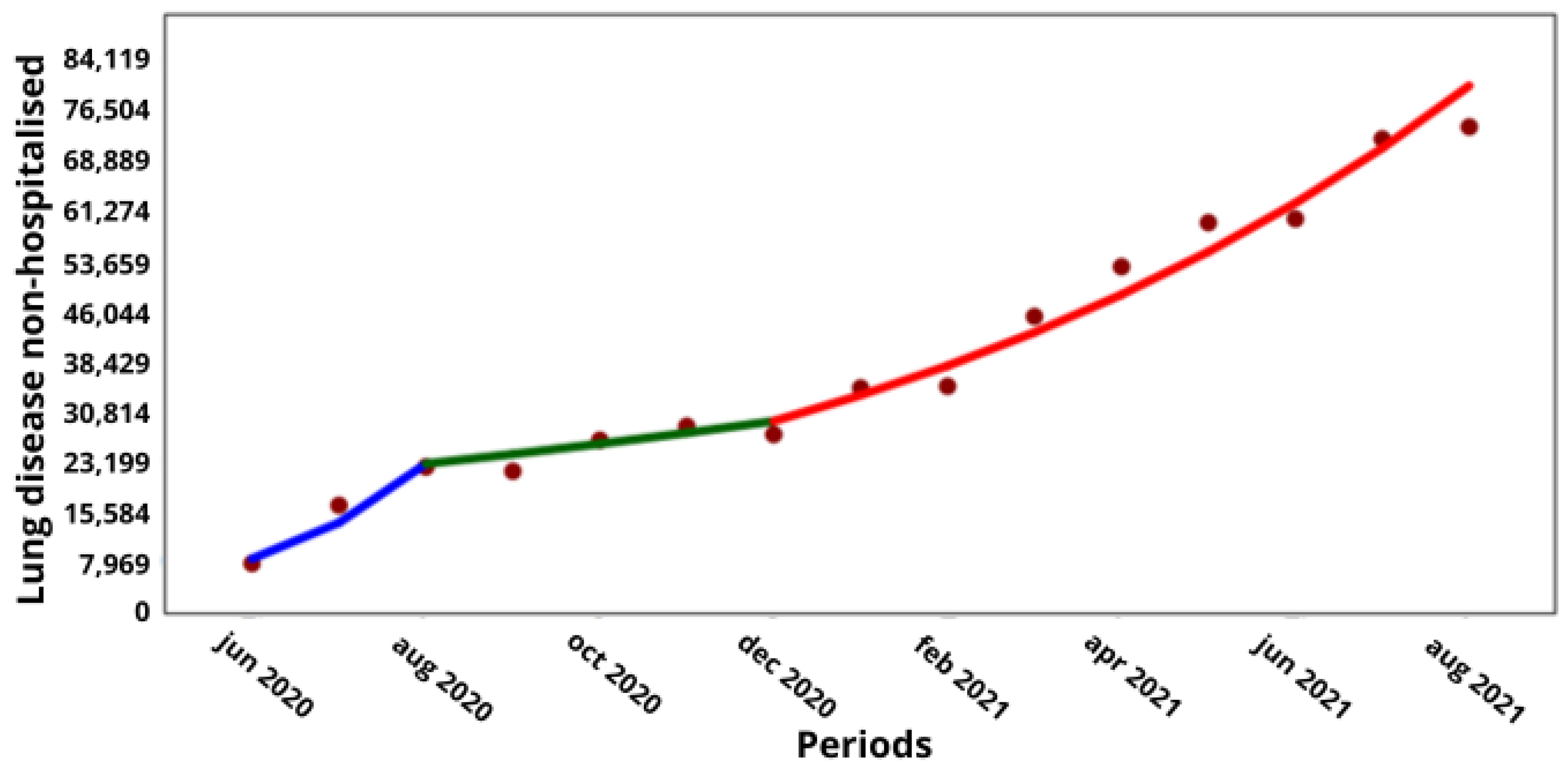
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NCDs | Non-communicable Diseases |
| AMPC | Average Monthly Percentage Change |
| MPC | Monthly Percentage Change |
| PA | Physical Activity |
| BMI | Body Mass Index |
| CI | Confidence Interval |
| HBP | High Blood Pressure |
| CVD | Cardiovascular Disease |
| CLuD | Chronic Lung Disease |
| CHD | Chronic Heart Disease |
| CKD | Chronic Kidney Disease |
| CND | Chronic Neurological Disease |
| ICP | Immunocompromised |
| CLiD | Chronic Liver Disease |
References
- Liu, Y.C.; Kuo, R.L.; Shih, S.R. COVID-19: The first documented coronavirus pandemic in history. Biomed. J. 2020, 43, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Lüthy, I.A.; Ritacco, V.; Kantor, I.N. One hundred years after the “Spanish” flu. Medicina 2018, 78, 113–118. Available online: https://www.medicinabuenosaires.com/PMID/29659361.pdf (accessed on 6 March 2024). [PubMed]
- Jackson, J.; Weiss, A.; Schwarzenberg, A.; Nelson, M.; Sutter, K.; Sutherland, M. Global Economic Effects of COVID-19. Congressional Research Service. Updated 4 October 2021. 2021. CRS Reports. Available online: https://sgp.fas.org/crs/row/R46270.pdf (accessed on 6 March 2024).
- Balanzá-Martínez, V.; Kapczinski, F.; de Azevedo Cardoso, T.; Atienza-Carbonell, B.; Rosa, A.R.; Mota, J.C.; De Boni, R.B. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev. Psiquiatr. Salud Ment. 2021, 14, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Sanyaolu, A.; Okorie, C.; Marinkovic, A.; Patidar, R.; Younis, K.; Desai, P.; Hosein, Z.; Padda, I.; Mangat, J.; Altaf, M. Comorbidity and its impact on patients with COVID-19. SN Compr. Clin. Med. 2020, 2, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Lai, F.T.; Guthrie, B.; Wong, S.Y.; Yip, B.H.; Chung, G.K.; Yeoh, E.K.; Chung, R.Y. Sex-specific intergenerational trends in morbidity burden and multimorbidity status in Hong Kong community: An age-period-cohort analysis of repeated population surveys. BMJ Open 2019, 9, e023927. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.; Frith, E.; Pedisic, Z.; Kang, M.; Loprinzi, P.D. Secular trends in the association between obesity and hypertension among adults in the United States, 1999–2014. Eur. J. Intern. Med. 2019, 62, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.; Gao, J.; Zhou, Z.; Yang, X.; Xu, Y.; Zhou, Z.; Chen, G. Prevalences and trends of chronic diseases in Shaanxi Province, China: Evidence from representative cross-sectional surveys in 2003, 2008 and 2013. PLoS ONE 2018, 13, e0202886. [Google Scholar] [CrossRef]
- FEN, Facultad de Economía y Negocios (Universidad de Chile). IMD Ranking: Chile Remains the Most Competitive Country in the Region. 2020. University Communication. Available online: https://fen.uchile.cl/en/noticia/ver/imd-ranking-chile-remains-the-most-competitive-country-in-the-region (accessed on 6 March 2024).
- Fraser, E. Long term respiratory complications of COVID-19. BMJ 2020, 370, m3001. [Google Scholar] [CrossRef] [PubMed]
- OECD, Organisation for Economic Cooperation and Development. Health at a Glance 2021: OECD Indicators. Official Report. 2021. Available online: https://www.oecd-ilibrary.org/sites/908b2da3-en/index.html?itemId=/content/component/908b2da3-en (accessed on 6 March 2024).
- Petermann-Rocha, F.; Martínez-Sanguinetti, M.A.; Leiva-Ordoñez, A.M.; Celis-Morales, C. Carga global de morbilidad y mortalidad atribuible a factores de riesgo entre los años 1990 y 2019:¿ Cuál es la realidad chilena? Rev. MÉDica Chile 2021, 149, 484–486. [Google Scholar] [CrossRef]
- Petermann, F.; Durán, E.; Labraña, A.M.; Martínez, M.A.; Leiva, A.M.; Garrido-Méndez, A.; Poblete-Valderrama, F.; Díaz-Martínez, X.; Salas, C.; Celis-Morales, C. Factores de riesgo asociados al desarrollo de hipertensión arterial en Chile. Rev. MÉDica Chile 2017, 145, 996–1004. [Google Scholar] [CrossRef]
- Leiva, A.M.; Martínez, M.A.; Petermann, F.; Garrido-Méndez, A.; Poblete-Valderrama, F.; Díaz-Martínez, X.; Celis-Morales, C. Factores asociados al desarrollo de diabetes mellitus tipo 2 en Chile. Nutr. Hosp. 2018, 35, 400–407. [Google Scholar] [CrossRef]
- MinSal (Ministerio de Salud de Chile; Ministry of Health of Chile), Departamento de Epidemiología-División de Planificación Sanitaria, Subsecretaría de Salud Pública. Encuesta Nacional de Salud 2016–2017 Primeros Resultados. Gobernamental Report. 2017. Available online: https://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf (accessed on 6 March 2024).
- MinCiencia (Ministerio de Ciencia, Tecnología, Conocimiento, e Innovación; Ministry of Science, Technology, Knowledge and Innovation). GitHub Repository from MinCiencia. 2021. Available online: https://github.com/MinCiencia (accessed on 6 March 2024).
- MinCiencia (Ministerio de Ciencia, Tecnología, Conocimiento, e Innovación; Ministry of Science, Technology, Knowledge and Innovation). GitHub repository of COVID-19 data from MinCiencia. Updated 4 September, 2021. COVID-19 Reports Formerly. 2021. Available online: https://www.minsal.cl/nuevo-coronavirus-2019-ncov__trashed/casos-confirmados-en-chile-covid-19/ (accessed on 6 March 2024).
- Celis-Morales, C.; Salas-Bravo, C.; Yáñez, A.; Castillo, M. Inactividad física y sedentarismo. La otra cara de los efectos secundarios de la Pandemia de COVID-19. Rev. MÉDica Chile 2020, 148, 885–886. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, D.J.; Brawner, C.A.; Ehrman, J.K.; Keteyian, S. Cardiorespiratory fitness attenuates the impact of risk factors associated with COVID-19 hospitalization. Mayo Clin. Proc. 2021, 96, 822–823. [Google Scholar] [CrossRef]
- Brawner, C.A.; Ehrman, J.K.; Bole, S.; Kerrigan, D.J.; Parikh, S.S.; Lewis, B.K.; Gindi, R.M.; Keteyian, C.; Abdul-Nour, K.; Keteyian, S.J. Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019. Mayo Clin. Proc. 2021, 96, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Bergman, J.; Ballin, M.; Nordström, A.; Nordström, P. Risk factors for COVID-19 diagnosis, hospitalization, and subsequent all-cause mortality in Sweden: A nationwide study. Eur. J. Epidemiol. 2021, 36, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.E.; Grannis, S.J.; Lembcke, L.R.; Valvi, N.; Roberts, A.R.; Embi, P.J. The synchronicity of COVID-19 disparities: Statewide epidemiologic trends in SARS-CoV-2 morbidity, hospitalization, and mortality among racial minorities and in rural America. PLoS ONE 2021, 16, e0255063. [Google Scholar] [CrossRef] [PubMed]
- Denis, F.; Fontanet, A.; Le Douarin, Y.M.; Le Goff, F.; Jeanneau, S.; Lescure, F.X. A self-assessment web-based app to assess trends of the COVID-19 pandemic in France: Observational study. J. Med. Internet Res. 2021, 23, e26182. [Google Scholar] [CrossRef]
- Guimarães, R.; Villela, D.; Xavier, D.; Saldanha, R.; Barcellos, C.; de Freitas, C.; Portela, M. Increasing impact of COVID-19 on young adults: Evidence from hospitalisations in Brazil. Public Health 2021, 198, 297–300. [Google Scholar] [CrossRef]
- Simetin, I.; Svajda, M.; Ivanko, P.; Dimnjakovic, J.; Belavic, A.; Istvanovic, A.; Poljicanin, T. COVID-19 incidence, hospitalizations and mortality trends in Croatia and school closures. Public Health 2021, 198, 164–170. [Google Scholar] [CrossRef]
- MinSal (Ministerio de Salud de Chile; Ministry of Health of Chile). Se inicia Proceso de Vacunación MASIVA Contra COVID-19. Official News. 2021. Available online: https://www.minsal.cl/se-inicia-proceso-de-vacunacion-masiva-contra-covid-19/ (accessed on 6 March 2024).
- Gutiérrez-Jara, J.P.; Saracini, C. Risk perception influence on vaccination program on covid-19 in chile: A mathematical model. Int. J. Environ. Res. Public Health 2022, 19, 2022. [Google Scholar] [CrossRef]
- Irecta Najera, C.A.; Álvarez Gordillo, G.d.C. Mecanismos moleculares de la obesidad y el rol de las adipocinas en las enfermedades metabólicas. Rev. Cuba. Investig. BiomÉDicas 2016, 35, 174–183. Available online: http://ref.scielo.org/v4ngkb (accessed on 6 March 2024).
- Bergens, O.; Nilsson, A.; Kadi, F. Cardiorespiratory fitness does not offset adiposity-related systemic inflammation in physically active older women. J. Clin. Endocrinol. Metab. 2019, 104, 4119–4126. [Google Scholar] [CrossRef]
- Rebollo-Ramos, M.; Velázquez-Díaz, D.; Corral-Pérez, J.; Barany-Ruiz, A.; Pérez-Bey, A.; Fernández-Ponce, C.; García-Cózar, F.J.; Ponce-González, J.G.; Cuenca-García, M. Aerobic fitness, Mediterranean diet and cardiometabolic risk factors in adults. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2020, 67, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Boidin, M.; Handfield, N.; Ribeiro, P.A.; Desjardins-Crépeau, L.; Gagnon, C.; Lapierre, G.; Gremeaux, V.; Lalongé, J.; Nigam, A.; Juneau, M.; et al. Obese but fit: The benefits of fitness on cognition in obese older adults. Can. J. Cardiol. 2020, 36, 1747–1753. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, J.; Millet, G.P.; Burtscher, M. Low cardiorespiratory and mitochondrial fitness as risk factors in viral infections: Implications for COVID-19. Br. J. Sport. Med. 2021, 55, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Mihalick, V.L.; Canada, J.M.; Arena, R.; Abbate, A.; Kirkman, D.L. Cardiopulmonary exercise testing during the COVID-19 pandemic. Prog. Cardiovasc. Dis. 2021, 67, 35–39. [Google Scholar] [CrossRef]
- Zheng, Y.Y.; Ma, Y.T.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef]
- Salgado-Aranda, R.; Pérez-Castellano, N.; Núñez-Gil, I.; Orozco, A.J.; Torres-Esquivel, N.; Flores-Soler, J.; Chamaisse-Akari, A.; Mclnerney, A.; Vergara-Uzcategui, C.; Wang, L.; et al. Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study. Infect. Dis. Ther. 2021, 10, 801–814. [Google Scholar] [CrossRef] [PubMed]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br. J. Sport. Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef]
- Af Geijerstam, A.; Mehlig, K.; Börjesson, M.; Robertson, J.; Nyberg, J.; Adiels, M.; Rosengren, A.; Åberg, M.; Lissner, L. Fitness, strength and severity of COVID-19: A prospective register study of 1,559,187 Swedish conscripts. BMJ Open 2021, 11, e051316. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, J.P.; Lesser, I.A.; Thomson, C.J.; Giles, L.V. Does higher self-reported cardiorespiratory fitness reduce the odds of hospitalization from COVID-19? J. Phys. Act. Health 2021, 18, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.A.; Arneja, J.; St. Cyr, K.; Sturrock, S.L.; Brooks, J.D. The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study. PLoS ONE 2021, 16, e0250508. [Google Scholar] [CrossRef] [PubMed]
- Clavario, P.; De Marzo, V.; Lotti, R.; Barbara, C.; Porcile, A.; Russo, C.; Beccaria, F.; Bonavia, M.; Bottaro, L.C.; Caltabellotta, M.; et al. Assessment of functional capacity with cardiopulmonary exercise testing in non-severe COVID-19 patients at three months follow-up. Int. J. Cardiol. 2020, 340, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Faghy, M.A.; Sylvester, K.P.; Cooper, B.G.; Hull, J.H. Cardiopulmonary exercise testing in the COVID-19 endemic phase. Br. J. Anaesth. 2020, 125, 447–449. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Desarrollo Social y Familia; Ministry of Social Development and Family of Chile. Se inicia Proceso de Vacunación Masiva Contra COVID-19. Official News. 2021. Available online: https://eligevivirsano.gob.cl/noticias/autoridades-detallaron-alcances-de-banda-horaria-elige-vivir-sano-que-rige-desde-hoy/ (accessed on 6 March 2024).
- Salinas, J.; Bello, S.; Chamorro, H.; Gonzalez, C.G. Consejeria en alimentación, actividad fÍsica y tabaco: Instrumento fundamental en la practica profesional. Rev. Chil. Nutr. 2016, 43, 434–442. [Google Scholar] [CrossRef]
- Berra, K.; Rippe, J.; Manson, J.E. Making physical activity counseling a priority in clinical practice: The time for action is now. JAMA 2015, 314, 2617–2618. [Google Scholar] [CrossRef] [PubMed]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA 2017, 318, 167–174. [Google Scholar] [CrossRef]
- Hurtado, A.F.V.; Ramos, O.A.; Jácome, S.J.; Cabrera, M.d.M.M. Actividad física y ejercicio en tiempos de COVID-19. Ces Med. 2020, 34, 51–58. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.; Altenburg, T.M.; Chinapaw, M.J. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–17. [Google Scholar] [CrossRef]
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J.-Physiol.-Heart Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef] [PubMed]

| AMPC (95% CI) | MPC (95% CI) | |||
|---|---|---|---|---|
| Hospitalized | Period 1 1 | Period 2 | Period 3 | |
| HBP | * (15.8–25.9) | ** (32–122.9) | *** (12.2–18.8) 2 | (−3.9–24.8) 6 |
| Diabetes | * (15.7–25.7) | ** (30.9–111.9) | *** (12.1–18.6) 2 | (−3.6; 24.9) 6 |
| Obesity | * (15.6–26.2) | ** (30.7–129.8) | ** (4.4–18.5) 3 | *** (10.8–21.9) 7 |
| Asthma | * (13.6–26.2) | 62 * (16.4–125.5) | *** (10.5–18.8) 2 | (−5.5–31.5) 6 |
| CVD | * (11.7–23.1) | ** (30–103.2) | 14 (−8.8–42.5) 4 | *** (7.9–12.4) 9 |
| CLuD | * (14.7–24.2) | ** (21.2–103.1) | *** (12.5–20.5) 5 | * (0.8–18.7) 8 |
| CHD | 17 * (11.5–22.8) | ** (27.7–98.2) | (−8.3–42.3) 4 | *** (7.9–12.4) 9 |
| CKD | * (12.7–24.2) | 72 ** (37.7–114.9) | (−7.1–45) 4 | *** (7.3–11.8) 9 |
| CND | * (11.6–21.3) | ** (23.5–108.7) | *** (7.5–13.9) 2 | 9 (−4.4–24.3) 6 |
| ICP | * (19.3–29.8) | *** (90.9–224.4) | *** (8.3–14.8) 2 | (−4.5–24.6) 6 |
| CLiD | * (12.3–24.2) | ** (31.2–107.9) | (-9.8–43) 4 | *** (8.8–13.4) 9 |
| AMPC (95% CI) | MPC (95% CI) | |||
|---|---|---|---|---|
| Hospitalized | Period 1 1 | Period 2 2 | Period 3 3 | |
| HBP | * (12.8–23.3) | ** (20.7–100.2) | (−4.6–22.8) | *** (11.8–18.1) |
| Diabetes | 19 * (13.8–24.4) | ** (27–111.3) | 8 (−4.9–22.6) | *** (12.1–18.5) |
| Obesity | * (13.1–23.4) | 64 ** (27.7–110.6) | (−6.6–19.9) | 15 *** (11.9–18.2) |
| Asthma | * (15–26.7) | ** (24.7–117) | (−4.4–26.2) | *** (13.7–20.7) |
| CVD | * (15–26.7) | ** (21.7–90.7) | (−5.1–18.8) | *** (9.8–15.3) |
| CLuD | * (12.7–22.1) | ** (30–105.3) | (−5.1–19.2) | *** (10.6–16.2) |
| CHD | * (12.4–21.7) | 57 ** (25.2–97.1) | (−4.7–19.5) | *** (10.9–16.5) |
| CKD | * (11.8–20.5) | ** (31.7–101.5) | (−5.3–17.2) | *** (9.4–14.6) |
| CND | * (12.5–21.4) | ** (32.8–105.6) | (−6–16.9) | *** (10.5–15.9) |
| ICP | * (24.9–36) | *** (179.5–354.4) | (−8.4–16.7) | *** (10.8–16.9) |
| CLiD | * (11.5–21.7) | 56 ** (21.6–100.2) | (−7.4–18.8) | *** (11–17.2) |
| Variables | Hospitalized | Non-Hospitalized | t (p) | ||
|---|---|---|---|---|---|
| Mean (SD) | IQR | Mean (SD) | IQR | ||
| HBP | 237,632.1 (140,532.4) | 230,780.0 | 74,5742.3 (414,399.1) | 694,754 | −7.162 *** |
| Diabetes | 146,988 (86,796.6) | 142,115.5 | 373,147.9 (217,732.2) | 346,605 | −6.6318 *** |
| Obesity | 45,941.4 (27,334.8) | 41,364.5 | 180,184.6 (98,749.6) | 157822 | −7.2693 *** |
| Asthma | 22,956.4 (13,543.6) | 21,542.5 | 210,070.1 (131,771.1) | 217,493.5 | −6.1267 *** |
| CVD | 23,764.2 (11,529.9) | 17,778.0 | 39,246.8 (18,772.1) | 30,737.5 | −8.022 *** |
| CLuD | 29,226.2 (16,961.9) | 28,756.0 | 38,726.2 (19,734.5) | 31,846 | −10.72 *** |
| CHD | 23,856.7 (11,578.3) | 17,695.5 | 34,092.6 (17,542.9) | 28,631 | −6.3285 *** |
| CKD | 26,333.6 (12801.8) | 19,466.0 | 27,461.6 (12,760.3) | 20,488 | −2.3457 * |
| CND | 14,540.4 (6860.5) | 10,585.5 | 20,200.4 (9970.1) | 15,616.5 | −6.7446 *** |
| ICP | 14,351.1 (7612.4) | 11,842.5 | 26,126 (14,456.3) | 22,214 | −6.6058 *** |
| CLiD | 6589.8 (3369.4) | 5249.5 | 4837.6 (2463.5) | 4019 | 6.886 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vásquez-Gómez, J.A.; Saracini, C. Insights from Chilean NCDs Hospitalization Data during COVID-19. Medicina 2024, 60, 770. https://doi.org/10.3390/medicina60050770
Vásquez-Gómez JA, Saracini C. Insights from Chilean NCDs Hospitalization Data during COVID-19. Medicina. 2024; 60(5):770. https://doi.org/10.3390/medicina60050770
Chicago/Turabian StyleVásquez-Gómez, Jaime Andrés, and Chiara Saracini. 2024. "Insights from Chilean NCDs Hospitalization Data during COVID-19" Medicina 60, no. 5: 770. https://doi.org/10.3390/medicina60050770
APA StyleVásquez-Gómez, J. A., & Saracini, C. (2024). Insights from Chilean NCDs Hospitalization Data during COVID-19. Medicina, 60(5), 770. https://doi.org/10.3390/medicina60050770







