Are We Able to Prevent Neonatal Readmission? A Retrospective Analysis from a Pediatrics Department in Ploiești, Romania
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hensman, A.M.; Erickson-Owens, D.A.; Sullivan, M.C.; Quilliam, B.J. Determinants of Neonatal Readmission in Healthy Term Infants: Results from a Nested Case–Control Study. Am. J. Perinatol. 2021, 38, 1078–1087. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, R.; Shori, N.; Bone, A.; Jawad, M. P645 An Audit to Improve Neonatal Readmission Number at Wexford General Hospital. Arch. Dis. Child. 2019, 104, A407–A408. [Google Scholar] [CrossRef]
- Bawazeer, M.; Alsalamah, R.K.; Almazrooa, D.R.; Alanazi, S.K.; Alsaif, N.S.; Alsubayyil, R.S.; Althubaiti, A.; Mahmoud, A.F. Neonatal Hospital Readmissions: Rate and Associated Causes. J. Clin. Neonatol. 2021, 10, 233–238. [Google Scholar] [CrossRef]
- Claudet, I.; De Montis, P.; Debuisson, C.; Maréchal, C.; Honorat, R.; Grouteau, E. Fréquentation Des Urgences Pédiatriques Par Les Nouveau-Nés. Arch. Pediatr. 2012, 19, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Pérez Solís, D.; Pardo de la Vega, R.; Fernández González, N.; Ibáñez Fernández, A.; Prieto Espuñes, S.; Fanjul Fernández, J.L. Neonatal visits to a pediatric emergency service. An. Pediatr. 2003, 59, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Ung, S.; Woolfenden, S.; Holdgate, A.; Lee, M.; Leung, M. Neonatal Presentations to a Mixed Emergency Department. J. Paediatr. Child Health 2007, 43, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Assandri Dávila, E.; Ferreira García, M.I.; Bello Pedrosa, O.; de Leonardis Capelo, D. Neonatal hospitalization through a hospital emergency service in Uruguay. An. Pediatr. 2005, 63, 413–417. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fernández Ruiz, C.; Trenchs Sainz de la Maza, V.; Curcoy Barcenilla, A.I.; Lasuen del Olmo, N.; Luaces Cubells, C. Neonatal management in the emergency department of a tertiary children’s hospital. An. Pediatr. 2006, 65, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Feenstra, M.M.; Nilsson, I.; Danbjørg, D.B. Broken Expectations of Early Motherhood: Mothers’ Experiences of Early Discharge after Birth and Readmission of Their Infants. J. Clin. Nurs. 2019, 28, 870–881. [Google Scholar] [CrossRef]
- Plotogea, M.; Isam, A.J.; Frincu, F.; Zgura, A.; Bacinschi, X.; Sandru, F.; Duta, S.; Petca, R.C.; Edu, A. An Overview of Cytomegalovirus Infection in Pregnancy. Diagnostics 2022, 12, 2429. [Google Scholar] [CrossRef]
- Teodorescu, C.; Dobjanschi, C.; Isopescu, F.; Rusu, E.; Edu, A.; Radulian, G. Contribution of Maternal Obesity and Weight Gain in Pregnancy to the Occurrence of Gestational Diabetes. Arch. Biol. Sci. 2015, 67, 583–589. [Google Scholar] [CrossRef]
- Edu, A.; Teodorescu, C.; Dobjanschi, C.G.; Socol, Z.Z.; Teodorescu, V.; Matei, A.; Albu, D.F.; Radulian, G. Placenta Changes in Pregnancy with Gestational Diabetes. Romanian J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 2016, 57, 507–512. [Google Scholar]
- Jugulete, G.; Pacurar, D.; Pavelescu, M.L.; Safta, M.; Gheorghe, E.; Borcoș, B.; Pavelescu, C.; Oros, M.; Merișescu, M. Clinical and Evolutionary Features of SARS-CoV-2 Infection (COVID-19) in Children, a Romanian Perspective. Children 2022, 9, 1282. [Google Scholar] [CrossRef] [PubMed]
- Becheanu, C.A.; Ţincu, I.F.; Smădeanu, R.E.; Coman, O.A.; Coman, L.; Ţincu, R.C.; Păcurar, D. Benefits of Oligofructose and Inulin in Management of Functional Diarrhoea in Children—Interventional Study. Farm. J. 2019, 67, 3. Available online: https://farmaciajournal.com/issue-articles/benefits-of-oligofructose-and-inulin-in-management-of-functional-diarrhoea-in-children-interventional-study/ (accessed on 17 January 2024). [CrossRef]
- Young, P.C.; Korgenski, K.; Buchi, K.F. Early Readmission of Newborns in a Large Health Care System. Pediatrics 2013, 131, e1538–e1544. [Google Scholar] [CrossRef] [PubMed]
- Păcurar, D.; Leşanu, G.; Dijmărescu, I.; Ţincu, I.F.; Gherghiceanu, M.; Orăşeanu, D. Genetic Disorder in Carbohydrates Metabolism: Hereditary Fructose Intolerance Associated with Celiac Disease. Rom. J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 2017, 58, 1109–1113. [Google Scholar]
- Becheanu, C.A.; Ţincu, I.F.; Leşanu, G. Feeding Practices among Romanian Children in the First Year of Life. Hong Kong J. Paediatr. 2018, 23, 13–19. [Google Scholar]
- Río, I.; Luque, A.; Castelló-Pastor, A.; Sandín-Vázquez, M.D.V.; Larraz, R.; Barona, C.; Jané, M.; Bolúmar, F. Uneven Chances of Breastfeeding in Spain. Int. Breastfeed. J. 2012, 7, 22. [Google Scholar] [CrossRef]
- von der Lippe, E.; Brettschneider, A.-K.; Gutsche, J.; Poethko-Müller, C. Factors influencing the prevalence and duration of breastfeeding in Germany: Results of the KiGGS study: First follow up (KiGGS Wave 1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2014, 57, 849–859. [Google Scholar] [CrossRef]
- Giovannini, M.; Riva, E.; Banderali, G.; Scaglioni, S.; Veehof, S.H.E.; Sala, M.; Radaelli, G.; Agostoni, C. Feeding Practices of Infants through the First Year of Life in Italy. Acta Paediatr. Oslo Nor. 1992 2004, 93, 492–497. [Google Scholar] [CrossRef]
- Simionescu, A.A.; Horobeţ, A.; Marin, E.; Belaşcu, L. Who Indicates Caesarean Section? A Cross-Sectional Survey in a Tertiary Level Maternity on Patients and Doctors’ Profiles at Childbirth. Obstet. Şi Ginecol. 2021, 2, 62. [Google Scholar] [CrossRef]
- Walsh, A.; Pieterse, P.; Mishra, N.; Chirwa, E.; Chikalipo, M.; Msowoya, C.; Keating, C.; Matthews, A. Improving Breastfeeding Support through the Implementation of the Baby-Friendly Hospital and Community Initiatives: A Scoping Review. Int. Breastfeed. J. 2023, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Nicolescu, A.; Cinteză, E. Esențialul În Cardiologia Pediatrica; Amaltea: Bucharest, Romania, 2022; ISBN 9789731622255. [Google Scholar]
- De Mare, K.E.; Bourne, D.; Rischitelli, B.; Fan, W.Q. Early Readmission of Exclusively Breastmilk-Fed Infants Born by Means of Normal Birth or Cesarean Is Multifactorial and Associated with Perinatal Maternal Mental Health Concerns. Birth 2024, 51, 186–197. [Google Scholar] [CrossRef] [PubMed]
| Diagnosis | Number of Patients Diagnosed |
|---|---|
| Mild protein energy malnutrition | 27 (25%) |
| Fever | 22 (20.3%) |
| Bronchiolitis | 19 (17.5%) |
| Diarrhea and infectious gastroenteritis | 16 (14.8%) |
| Acute rhinoconjunctivitis | 10 (9.2%) |
| Pyodermitis | 5 (4.6%) |
| Late-onset sepsis | 4 (3.7%) |
| Urinary tract infection | 3 (2.7%) |
| Jaundice | 1 (0.9%) |
| Influenza | 1 (0.9%) |
| Number of Patients (n = 108) | |
|---|---|
| Gender | |
| 65 (60.1%) |
| 43 (39.8%) |
| APGAR score | |
| 96 (88.8%) |
| 11 (10.1%) |
| 1 (0.92%) |
| Type of birth | |
| 60 (55.5%) |
| 48 (44.4%) |
| Maternal age (years) | |
| 12 (11.1%) |
| 81 (75%) |
| 15 (13.8%) |
| Number of children | |
| 84 (77.7%) |
| 21 (19.4%) |
| 2 (1.85%) |
| 1 (0.92%) |
| Gestational age and birthweight | |
| 93 (86.1%) |
| 7 (6.48%) |
| 8 (7.4%) |
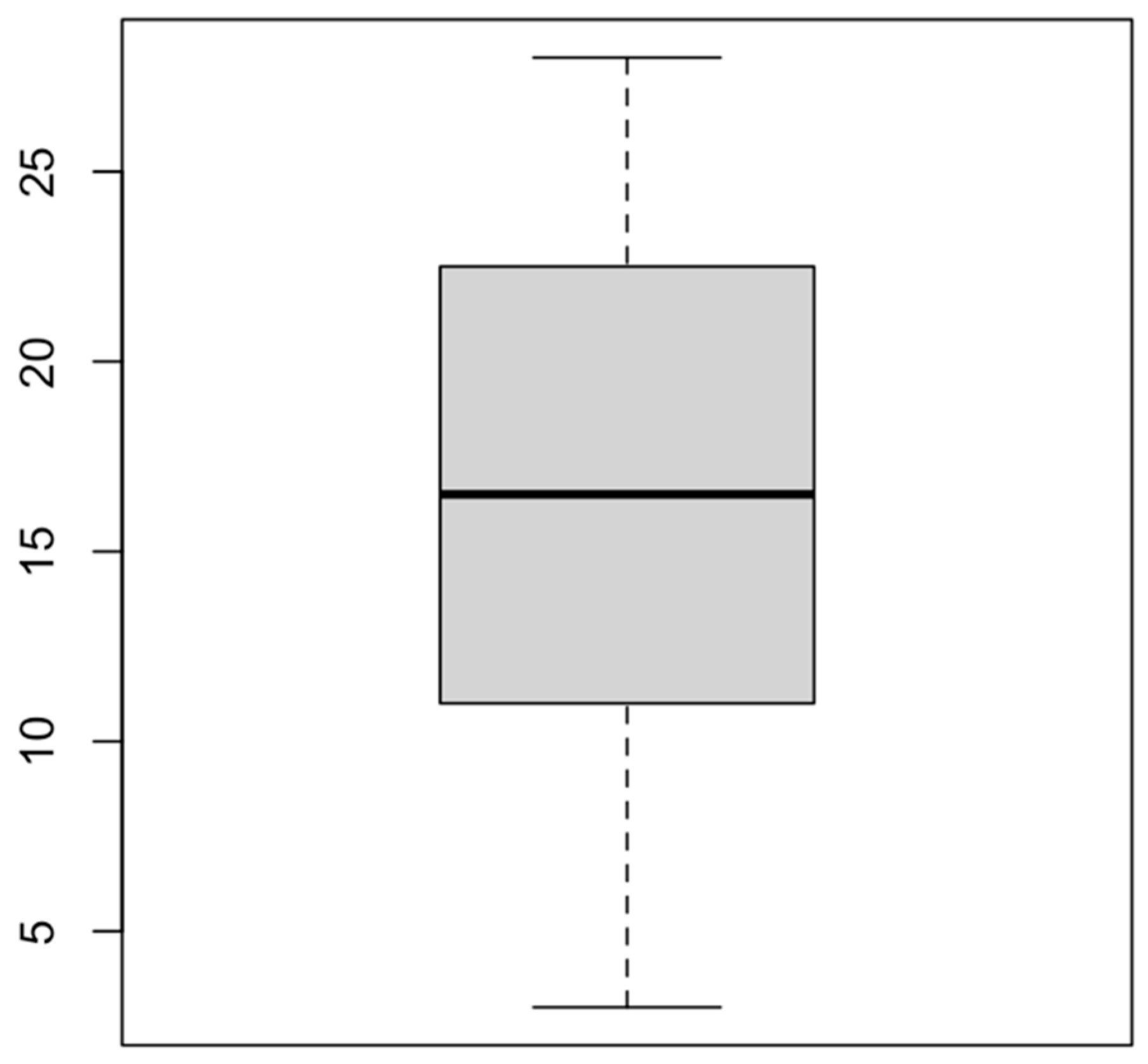
| Length of hospital stay (pediatric unit) | |
| 80 (74.1%) |
| 28 (25.9%) |
| Feeding | |
| 19 (17.6%) |
| 36 (33.3%) |
| 37 (34.2%) |
| 16 (14.8%) |
| Area | |
| 76 (70.3%) |
| 32 (29.6%) |
| Newborn age at admission | |
| 13 (12.1%) |
| 31 (28.7%) |
| 31 (28.7%) |
| 33 (30.5%) |
| Newborn age at discharge after birth (Maternity) | |
| 37 (34.2%) |
| 60 (55.5%) |
| 9 (8.33%) |
| 2 (1.85%) |
| Variables | Relationship (p-Value) * |
|---|---|
| Gender | 0.169 |
| APGAR score | 0.95 |
| Maternal age | 0.056 |
| Type of birth | 0.65 |
| Number of children | <0.001 |
| Area of residence | 0.37 |
| Age (days) at discharge from maternity unit | <0.001 |
| Gestational age | 0.76 |
| Type of feeding | 0.68 |
| Investigations and Results | Number of Patients |
|---|---|
| Umbilical swab | |
| 3 (2.7%) |
| 1 (0.92%) |
| 2 (1.85%) |
| Nasal swab | |
| 20 (18.5%) |
| 2 (1.85%) |
| 1 (0.92%) |
| Ophthalmic swab—Staphylococcus aureus | 2 (1.85%) |
| Urine culture | |
| 3 (2.7%) |
| 4 (3.7%) |
| Positive COVID-19 Antigen/PCR ** | 4 (3.7%) |
| Positive Type A Influenza Antigen | 1 (0.92%) |
| Positive Respiratory Syncytial Virus (RSV) Antigen | 1 (0.92%) |
| Positive Rotavirus Antigen | 2 (1.85%) |
| High CRP (C-reactive protein) (>5 mg/dL) | 16 (14.8%) |
| Complete blood count revealing anemia (hemoglobin < 12 g/dL, hematocrit < 35%) | 17 (15.7%) |
| Hyperbilirubinemia (total serum bilirubin > 10 mg/dL) | 14 (12.9%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roșca, I.; Constantin, A.T.; Popescu, D.E.; Jura, A.M.C.; Miu, A.; Turenschi, A. Are We Able to Prevent Neonatal Readmission? A Retrospective Analysis from a Pediatrics Department in Ploiești, Romania. Medicina 2024, 60, 705. https://doi.org/10.3390/medicina60050705
Roșca I, Constantin AT, Popescu DE, Jura AMC, Miu A, Turenschi A. Are We Able to Prevent Neonatal Readmission? A Retrospective Analysis from a Pediatrics Department in Ploiești, Romania. Medicina. 2024; 60(5):705. https://doi.org/10.3390/medicina60050705
Chicago/Turabian StyleRoșca, Ioana, Andreea Teodora Constantin, Daniela Eugenia Popescu, Ana Maria Cristina Jura, Anca Miu, and Alina Turenschi. 2024. "Are We Able to Prevent Neonatal Readmission? A Retrospective Analysis from a Pediatrics Department in Ploiești, Romania" Medicina 60, no. 5: 705. https://doi.org/10.3390/medicina60050705
APA StyleRoșca, I., Constantin, A. T., Popescu, D. E., Jura, A. M. C., Miu, A., & Turenschi, A. (2024). Are We Able to Prevent Neonatal Readmission? A Retrospective Analysis from a Pediatrics Department in Ploiești, Romania. Medicina, 60(5), 705. https://doi.org/10.3390/medicina60050705







