Retrospective Cohort Study of Early versus Delayed Ballon Kyphoplasty Intervention for Osteoporotic Vertebral Fracture Treatment
Abstract
1. Introduction
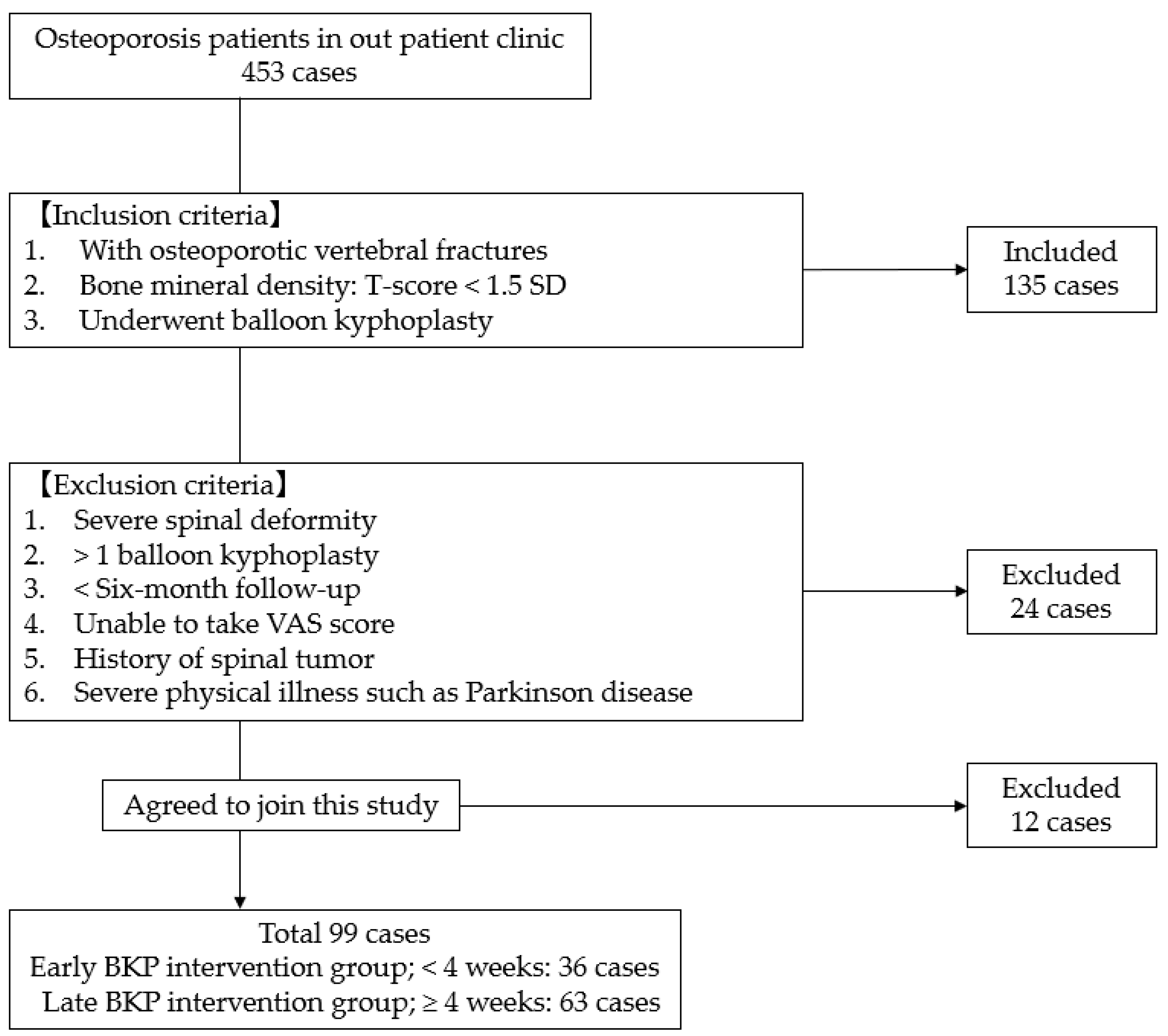
2. Materials and Methods
2.1. Clinical Evaluation
2.2. Radiological Evaluation
2.3. Statistical Evaluation
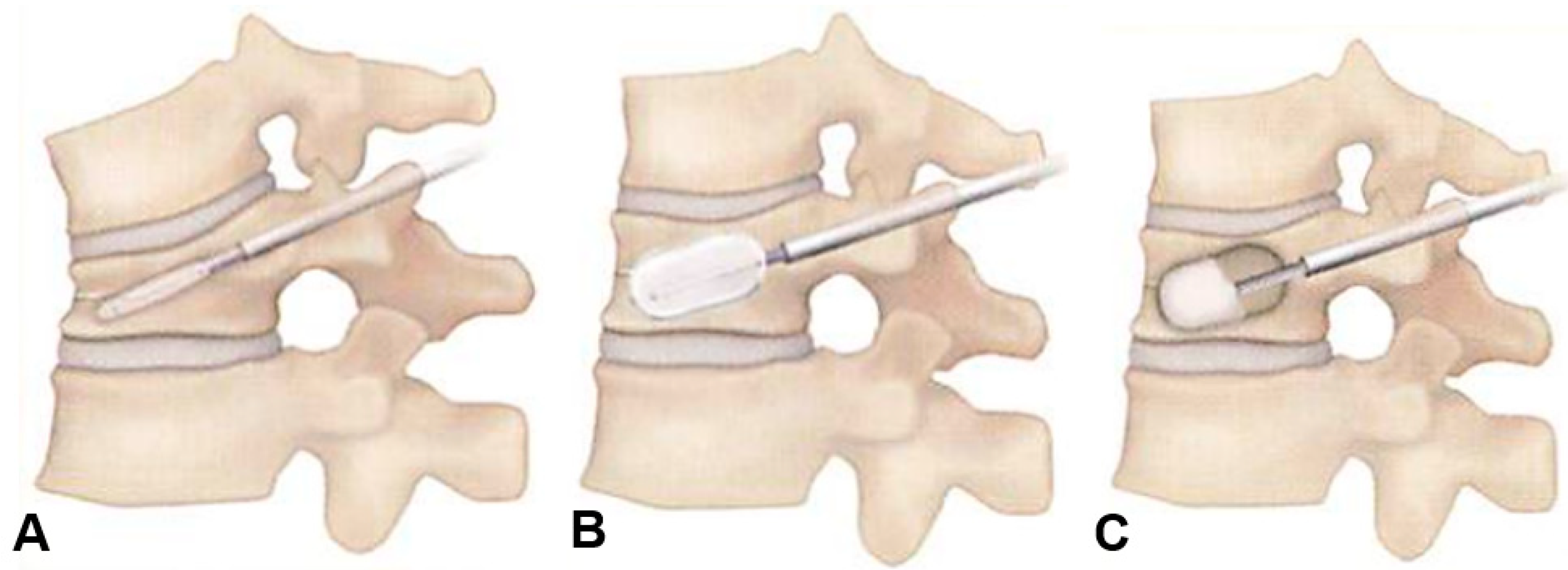
2.4. Surgery
3. Results
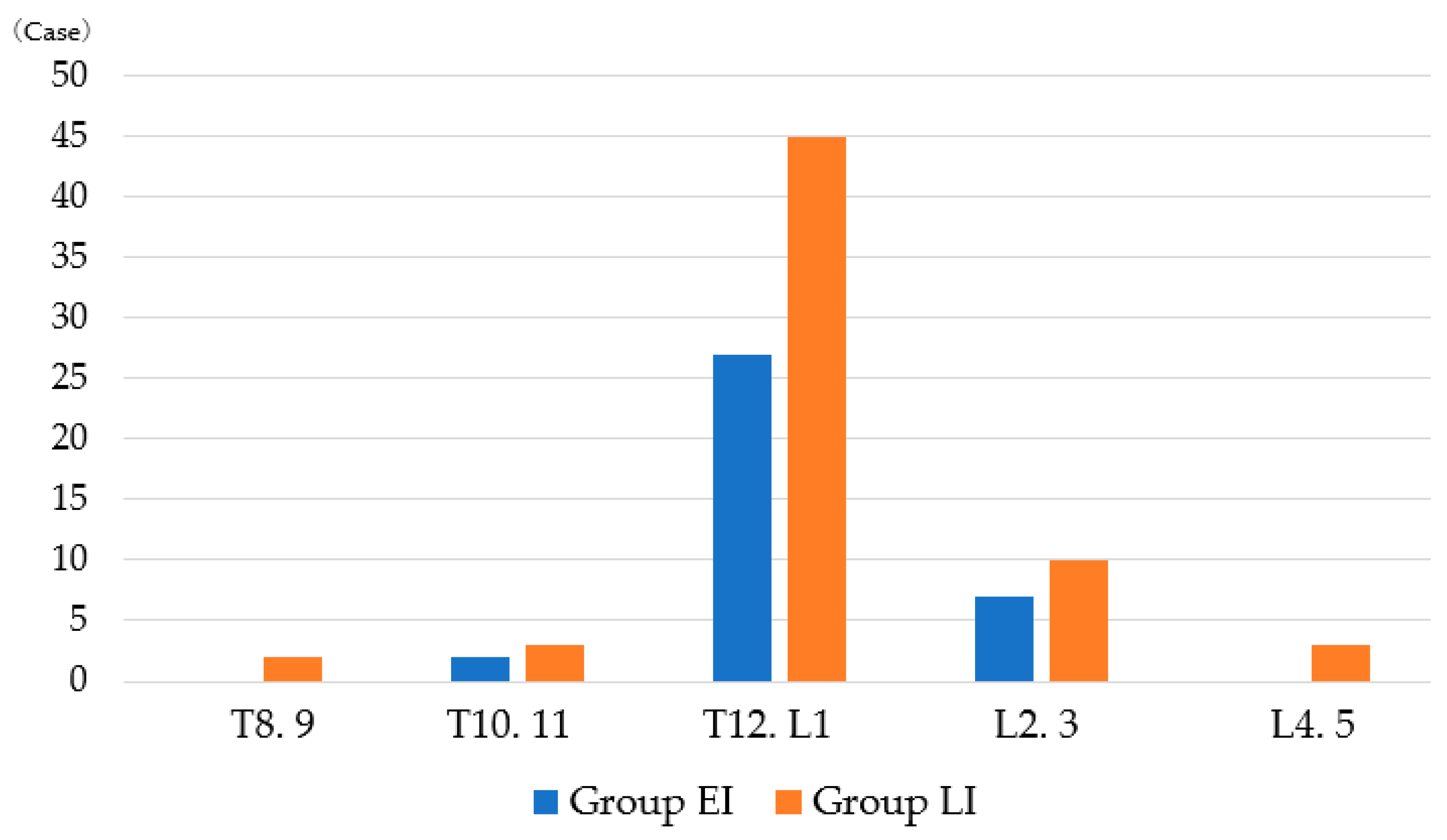
3.1. Patient Demographics
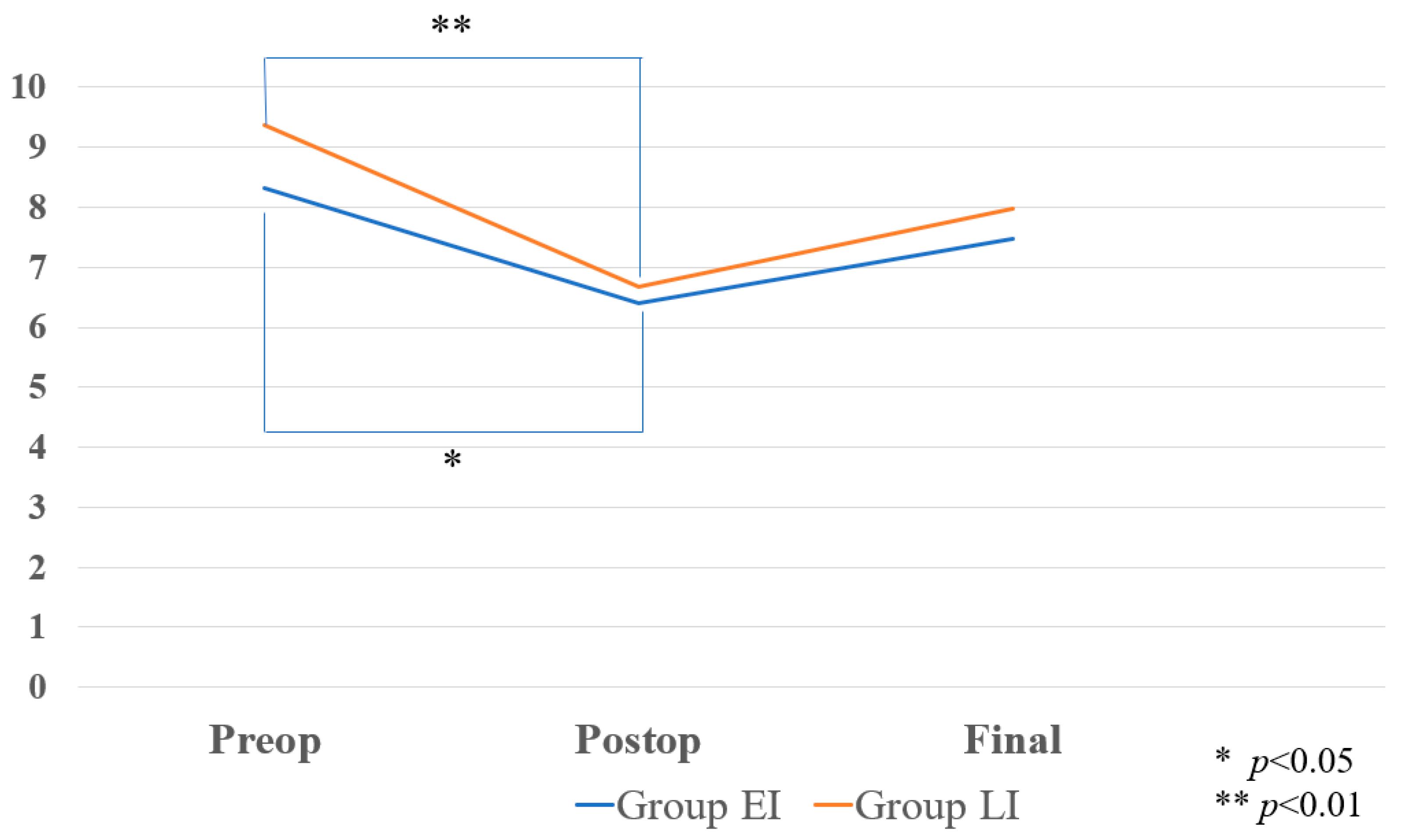
3.2. Clinical Results
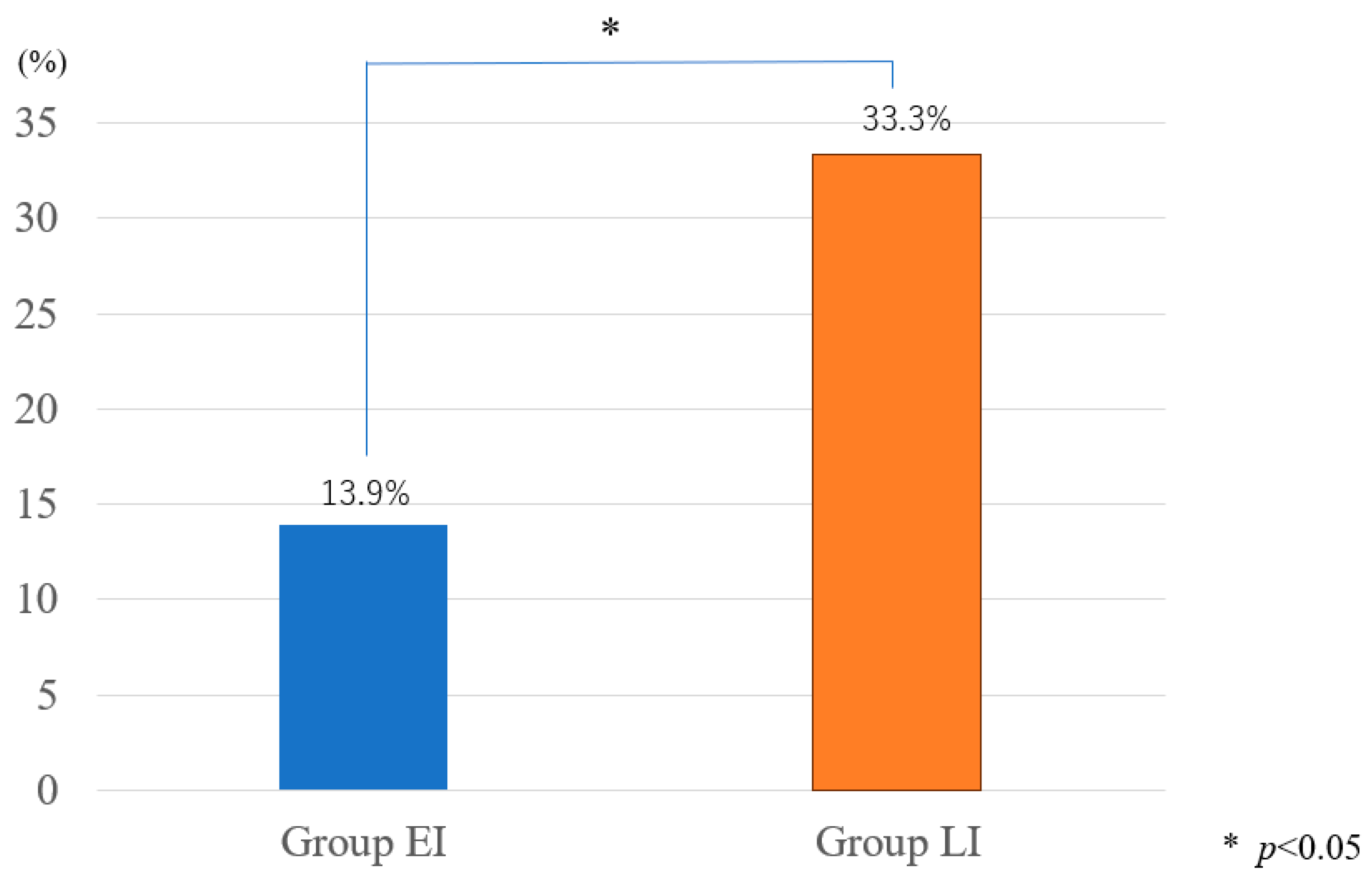
3.3. Radiographic Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kanis, J.; Johnell, O.; Oden, A.; De Laet, C.; Jonsson, B.; Dawson, A. Ten-year risk of osteoporotic fracture and the effect of risk factors on screening strategies. Bone 2002, 30, 251–258. [Google Scholar] [CrossRef]
- Reginster, J.Y.; Burlet, N. Osteoporosis: A still increasing prevalence. Bone 2006, 38, S4–S9. [Google Scholar] [CrossRef]
- Ploeg, W.T.; Veldhuizen, A.G.; The, B.; Sietsma, M.S. Percutaneous vertebroplasty as a treatment for osteoporotic vertebral compression fractures: A systematic review. Eur. Spine J. 2006, 15, 1749–1758. [Google Scholar] [CrossRef]
- Johnell, O. Advances in osteoporosis: Better identification of risk factors can reduce morbidity and mortality. J. Intern. Med. 1996, 239, 299–304. [Google Scholar] [CrossRef]
- Minamide, A.; Maeda, T.; Yamada, H.; Murakami, K.; Okada, M.; Enyo, Y.; Nakagawa, Y.; Iwasaki, H.; Tsutsui, S.; Takami, M.; et al. Early versus delayed kyphoplasty for thoracolumbar osteoporotic vertebral fractures: The effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin. Neurol. Neurosurg. 2018, 173, 176–181. [Google Scholar] [CrossRef]
- Ito, Y.; Hasegawa, Y.; Toda, K.; Nakahara, S. Pathogenesis, and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002, 2, 101–106. [Google Scholar] [CrossRef]
- Takahashi, S.; Hoshino, M.; Terai, H.; Toyoda, H.; Suzuki, A.; Tamai, K.; Watanabe, K.; Tsujio, T.; Yasuda, H.; Kono, H.; et al. Differences in short-term clinical and radiological outcomes depending on timing of balloon kyphoplasty for painful osteoporotic vertebral fracture. J. Orthop. Sci. 2018, 23, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Garfin, S.R.; Yuan, H.A.; Reiley, M.A. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001, 26, 1511–1515. [Google Scholar] [CrossRef] [PubMed]
- Oh, G.S.; Kim, H.S.; Ju, C.I.; Kim, S.W.; Lee, S.M.; Shin, H. Comparison of the results of balloon kyphoplasty performed at different times after injury. J. Korean Neurosurg. Soc. 2010, 47, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Klazen, C.A.; Lohle, P.N.; de Vries, J.; Jansen, F.H.; Tielbeek, A.V.; Blonk, M.C.; Venmans, A.; van Rooij, W.J.J.; Schoemaker, M.C.; Juttmann, J.R.; et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): An open-label randomised trial. Lancet 2010, 376, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Edidin, A.A.; Ong, K.L.; Lau, E.; Kurtz, S.M. Morbidity, and mortality after vertebral fractures: Comparison of vertebral augmentation and nonoperative management in the Medicare population. Spine 2015, 40, 1228–1241. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Xu, J.; Wang, Q.; Zhang, L.; Yin, S.; Qian, B.; Li, X.; Wen, T.; Jia, Z. Timing of Percutaneous Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures. Pain Physician 2023, 26, 231–243. [Google Scholar] [PubMed]
- Crandall, D.; Slaughter, D.; Hankins, P.J.; Moore, C.; Jerman, J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: Early results. Spine J. 2004, 4, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Self, M.; Mooney, J.; Amburgy, J.; Agee, B.; Schoel, L.; Pritchard, P.; Chambers, M. Analysis of injected cement volume and clinical outcomes following kyphoplasty for vertebral compression fractures. Surg. Neurol. Int. 2020, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Röder, C.; Boszczyk, B.; Perler, G.; Aghayev, E.; Külling, F.; Maestretti, G. Cement volume is the most important modifiable predictor for pain relief in BKP: Results from SWISS spine, a nationwide registry. Eur. Spine J. 2013, 22, 2241–2248. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Harvey, N.C.; McCloskey, E.; Bruyère, O.; Veronese, N.; Lorentzon, M.; Cooper, C.; Rizzoli, R.; Adib, G.; Al-Daghri, N.; et al. Algorithm for the management of patients at low, high, and very high risk of osteoporotic fractures. Osteoporos. Int. 2020, 31, 1–12. [Google Scholar] [CrossRef]
- Zhou, X.; Meng, X.; Zhu, H.; Zhu, Y.; Yuan, W. Early versus late percutaneous kyphoplasty for treating osteoporotic vertebral compression fracture: A retrospective study. Clin. Neurol. Neurosurg. 2019, 180, 101–105. [Google Scholar] [CrossRef]
- Goldstein, S.; Smorgick, Y.; Mirovsky, Y.; Anekstein, Y.; Blecher, R.; Tal, S. Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J. Clin. Neurosci. 2016, 31, 122–126. [Google Scholar] [CrossRef]
- Garg, B.; Dixit, V.; Batra, S.; Malhotra, R.; Sharan, A. Non-surgical management of acute osteoporotic vertebral compression fracture: A review. J. Clin. Orthop. Trauma 2017, 8, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Evaniew, N. Vertebral Augmentation for Osteoporotic Compression Fractures: Review of the Fracture Reduction Evaluation Trial. J. Long Term Eff. Med. Implant. 2016, 26, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Peng, Y.; Li, J. Comparison of clinical and radiological outcomes of vertebral body stenting versus percutaneous kyphoplasty for the treatment of osteoporotic vertebral compression fracture: A systematic review and meta-analysis. Jt. Dis. Relat. Surg. 2024, 35, 218–230. [Google Scholar] [CrossRef] [PubMed]
- Rousing, R.; Hansen, K.L.; Andersen, M.O.; Jespersen, S.M.; Thomsen, K.; Lauritsen, J.M. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: A clinical randomized study. Spine 2010, 35, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Berenson, J.; Pflugmacher, R.; Jarzem, P.; Zonder, J.; Schechtman, K.; Tillman, J.B.; Bastian, L.; Ashraf, T.; Vrionis, F.; Cancer Patient Fracture Evaluation (CAFE) Investigators. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: A multicentre, randomised controlled trial. Lancet Oncol. 2011, 12, 225–235. [Google Scholar] [CrossRef]
- Cooper, C.; Atkinson, E.J.; O’Fallon, W.M.; Melton, L.J. Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985–1989. J. Bone Miner. Res. 1992, 7, 221–227. [Google Scholar] [CrossRef]
- Son, H.J.; Park, S.J.; Kim, J.K.; Park, J.S. Mortality risk after the first occurrence of osteoporotic vertebral compression fractures in the general population: A nationwide cohort study. PLoS ONE 2023, 18, e0291561. [Google Scholar] [CrossRef]
- Patel, N.; Jacobs, D.; John, J.; Fayed, M.; Nerusu, L.; Tandron, M.; Dailey, W.; Ayala, R.; Sibai, N.; Forrest, P.; et al. Balloon Kyphoplasty vs Vertebroplasty: A Systematic Review of Height Restoration in Osteoporotic Vertebral Compression Fractures. J. Pain Res. 2022, 15, 1233–1245. [Google Scholar] [CrossRef] [PubMed]
- Kallmes, D.F.; Schweickert, P.A.; Marx, W.F.; Jensen, M.E. Vertebroplasty in the, mid− and upper thoracic spine. AJNR Am. J. Neuroradiol. 2002, 23, 1117–112026. [Google Scholar]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef]
- Kanis, J.A.; Cooper, C.; Rizzoli, R.; Reginster, J.Y.; Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar] [CrossRef]
- Guan, H.; Yang, H.; Mei, X.; Liu, T.; Guo, J. Early or delayed operation, which is more optimal for kyphoplasty? A retrospective study on cement leakage during kyphoplasty. Injury 2012, 43, 1698–1703. [Google Scholar] [CrossRef]
- Baroud, G.; Bohner, M. Biomechanical impact of vertebroplasty. Postoper. Biomech. Vertebroplasty Jt. Bone Spine 2006, 73, 144–150. [Google Scholar] [CrossRef]
- Zhao, G.; Liu, X.; Li, F. Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporos. Int. 2016, 27, 2823–2834. [Google Scholar] [CrossRef]
- Li, Y.; Tao, W.; Wan, Q.; Li, Q.; Yang, Y.; Lin, Y.; Zhang, S.; Li, W. Erratum for Jiang et al., Zoonotic and Potentially Host-Adapted Enterocytozoon bieneusi Genotypes in Sheep and Cattle in Northeast China and an Increasing Concern about the Zoonotic Importance of Previously Considered Ruminant-Adapted Genotypes. Appl. Environ. Microbiol. 2015, 81, 5278. [Google Scholar]
- Yang, C.C.; Chien, J.T.; Tsai, T.Y.; Yeh, K.T.; Lee, R.P.; Wu, W.T. Earlier Vertebroplasty for Osteoporotic Thoracolumbar Compression Fracture May Minimize the Subsequent Development of Adjacent Fractures: A Retrospective Study. Pain Physician 2018, 21, E483–E491. [Google Scholar]
- He, B.; Zhao, J.; Zhang, M.; Jiang, G.; Tang, K.; Quan, Z. Effect of Surgical Timing on the Refracture Rate after Percutaneous Vertebroplasty: A Retrospective Analysis of at Least 4-Year Follow-Up. BioMed Res. Int. 2021, 2021, 5503022. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Taylor, R.J.; Fritzell, P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures. Spine 2006, 31, 2747–2755. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Sun, H.; Liu, S.; Sang, L.; Wang, K.; Dong, Y.; Qi, X. Cement Leakage in Vertebral Compression Fractures between Unilateral and Bilateral Percutaneous Vertebral Augmentation: A Meta-Analysis. Turk. Neurosurg. 2022; online ahead of print. [Google Scholar]
- Chen, Y.J.; Chen, W.H.; Chen, H.T.; Hsu, H.C. Repeat needle insertion in vertebroplasty to prevent re-collapse of the treated vertebrae. Eur. J. Radiol. 2012, 81, 558–561. [Google Scholar] [CrossRef]
- Kishikawa, Y. Initial non-weight-bearing therapy is important for preventing vertebral body collapse in elderly patients with clinical vertebral fractures. Int. J. Gen. Med. 2012, 5, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Erkan, S.; Ozalp, T.R.; Yercan, H.S.; Okcu, G. Does timing matter in performing kyphoplasty? Acute versus chronic compression fractures. Acta Orthop. Belg. 2009, 75, 396–404. [Google Scholar] [PubMed]

| Group EI | Group LI | p Value | |
|---|---|---|---|
| Number | 36 | 63 | |
| Age at surgery (year) | 81.8 ± 5.0 | 80.1 ± 8.2 | 0.338 |
| Sex (male/female) | 11/25 | 25/38 | 0.364 |
| Follow-up (month) | 11.2 ± 7.4 | 12.1 ± 9.4 | 0.451 |
| Group EI (n = 36) | Group LI (n = 63) | p Value | |
|---|---|---|---|
| BMI (g/cm2) | 23.3 ± 3.3 | 21.7 ± 3.7 | 0.101 |
| Surgery duration (min) | 30.2 ± 7.4 | 37.1 ± 8.9 | 0.0004 ** |
| Final VAS (mm) | 11.3 ± 10.9 | 13.5 ± 13.2 | 0.722 |
| Revision surgery | 3/36 (8.3%) | 4/63 (6.3%) | 0.711 |
| Group EI (n = 36) | Group LI (n = 63) | p Value | |
|---|---|---|---|
| Preop LKA (degree) | 8.31 ± 6.48 | 9.37 ± 6.84 | 0.457 |
| Postop LKA (degree) | 6.41 ± 5.22 | 6.68 ± 5.28 | 0.726 |
| Final LKA (degree) | 7.47 ± 5.33 | 7.97 ± 6.10 | 0.827 |
| Preop VKA (degree) | 12.8 ± 7.38 | 14.9 ± 6.73 | 0.179 |
| Postop VKA (degree) | 5.72 ± 4.15 | 7.70 ± 5.01 | 0.100 |
| Final VKA (degree) | 9.61 ± 5.83 | 9.86 ± 6.05 | 0.870 |
| Cement volume (mL) | 7.42 ± 1.54 | 6.3 ± 1.93 | 0.007 ** |
| Cement leakage | 11 (30.1%) | 12 (19.0%) | 0.192 |
| AVF | 3 (8.3%) | 21 (33.3%) | 0.034 * |
| BMD (g/cm2) | −2.09 ± 0.96 | −1.96 ± 1.41 | 0.911 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, A.; Parihar, U.; Kumawat, C.; El Kader Al Askar, A.; Tanaka, M.; Gunjotikar, S.; Taoka, T.; Komatsubara, T.; Fujiwara, Y.; Uotani, K.; et al. Retrospective Cohort Study of Early versus Delayed Ballon Kyphoplasty Intervention for Osteoporotic Vertebral Fracture Treatment. Medicina 2024, 60, 519. https://doi.org/10.3390/medicina60040519
Miyamoto A, Parihar U, Kumawat C, El Kader Al Askar A, Tanaka M, Gunjotikar S, Taoka T, Komatsubara T, Fujiwara Y, Uotani K, et al. Retrospective Cohort Study of Early versus Delayed Ballon Kyphoplasty Intervention for Osteoporotic Vertebral Fracture Treatment. Medicina. 2024; 60(4):519. https://doi.org/10.3390/medicina60040519
Chicago/Turabian StyleMiyamoto, Akiyoshi, Umesh Parihar, Chetan Kumawat, Abd El Kader Al Askar, Masato Tanaka, Sharvari Gunjotikar, Takuya Taoka, Tadashi Komatsubara, Yoshihiro Fujiwara, Koji Uotani, and et al. 2024. "Retrospective Cohort Study of Early versus Delayed Ballon Kyphoplasty Intervention for Osteoporotic Vertebral Fracture Treatment" Medicina 60, no. 4: 519. https://doi.org/10.3390/medicina60040519
APA StyleMiyamoto, A., Parihar, U., Kumawat, C., El Kader Al Askar, A., Tanaka, M., Gunjotikar, S., Taoka, T., Komatsubara, T., Fujiwara, Y., Uotani, K., & Arataki, S. (2024). Retrospective Cohort Study of Early versus Delayed Ballon Kyphoplasty Intervention for Osteoporotic Vertebral Fracture Treatment. Medicina, 60(4), 519. https://doi.org/10.3390/medicina60040519







