Pitfalls with the MAKO Robotic-Arm-Assisted Total Knee Arthroplasty
Abstract
1. Introduction
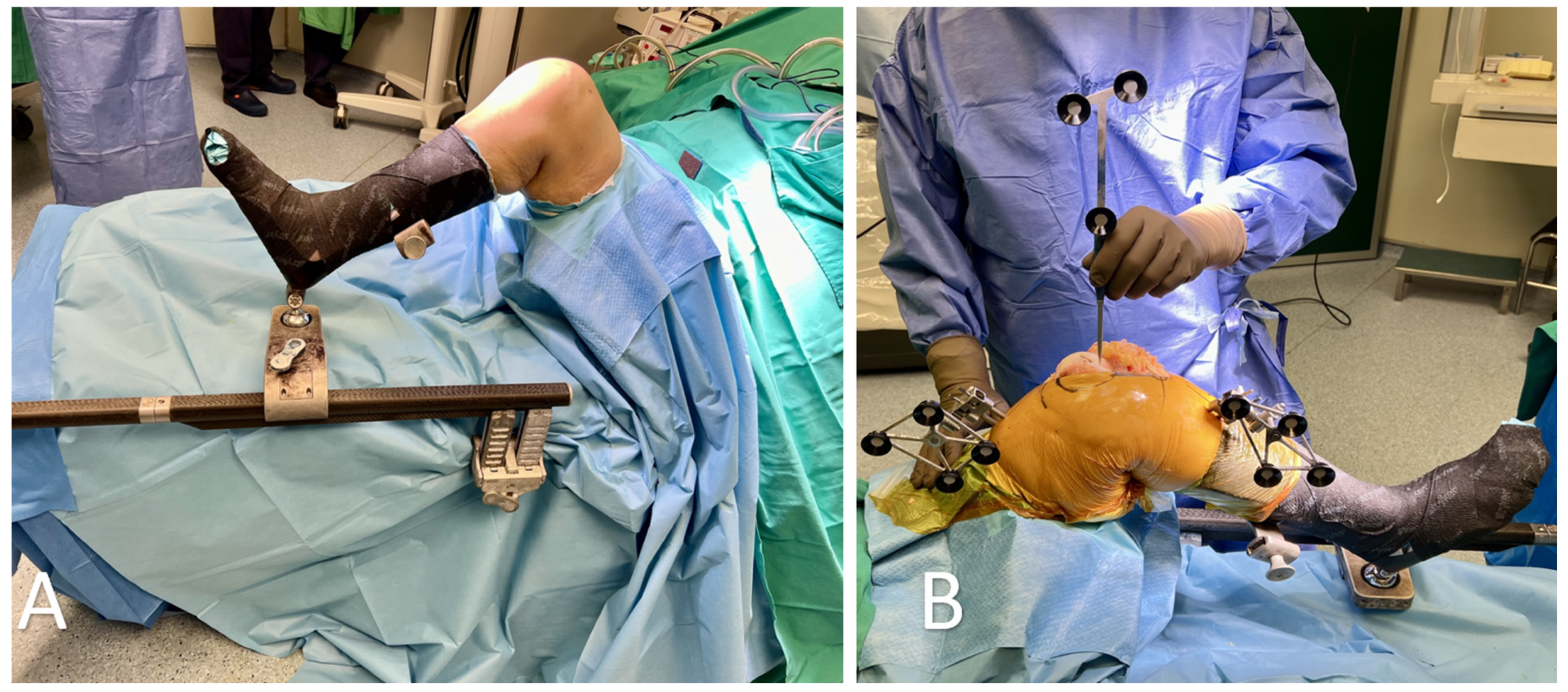
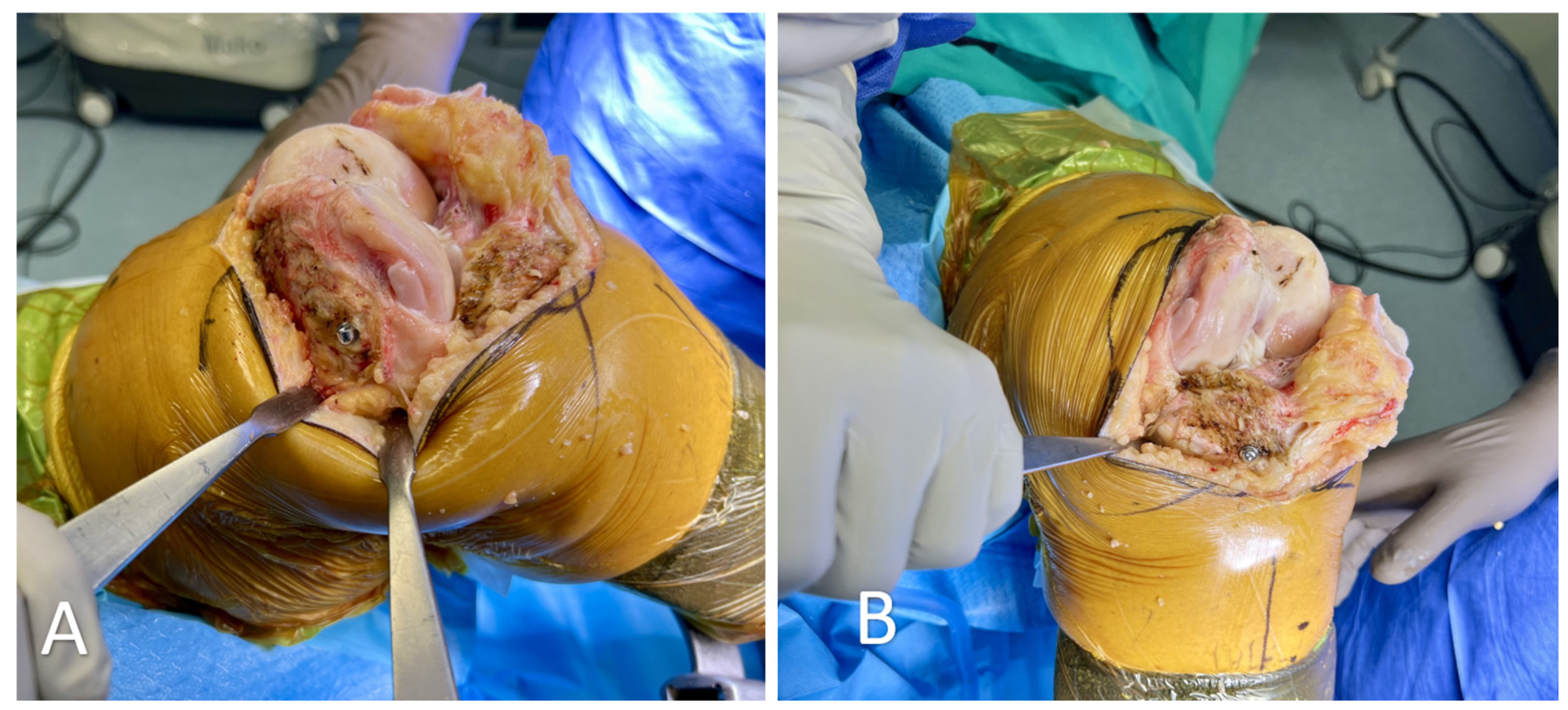
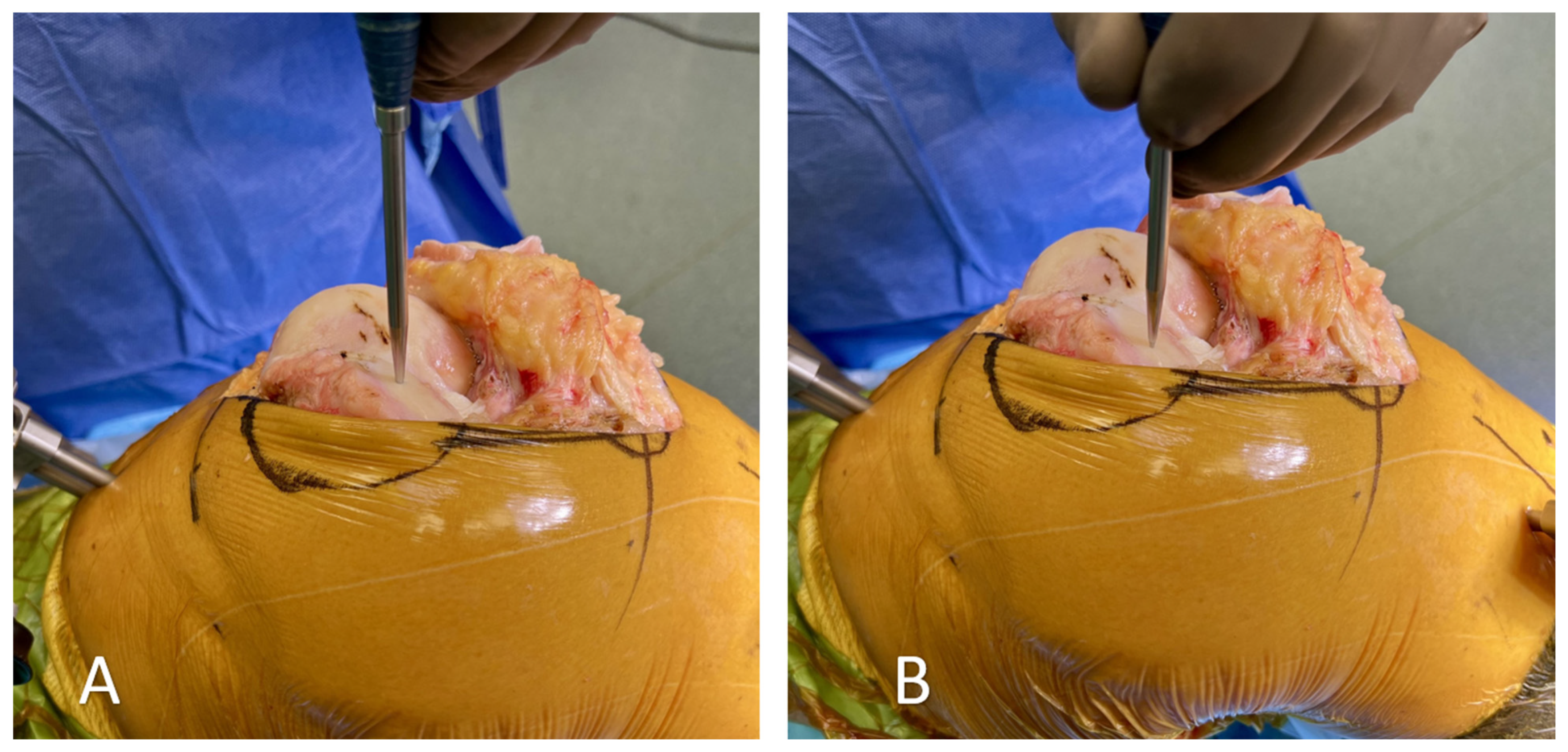
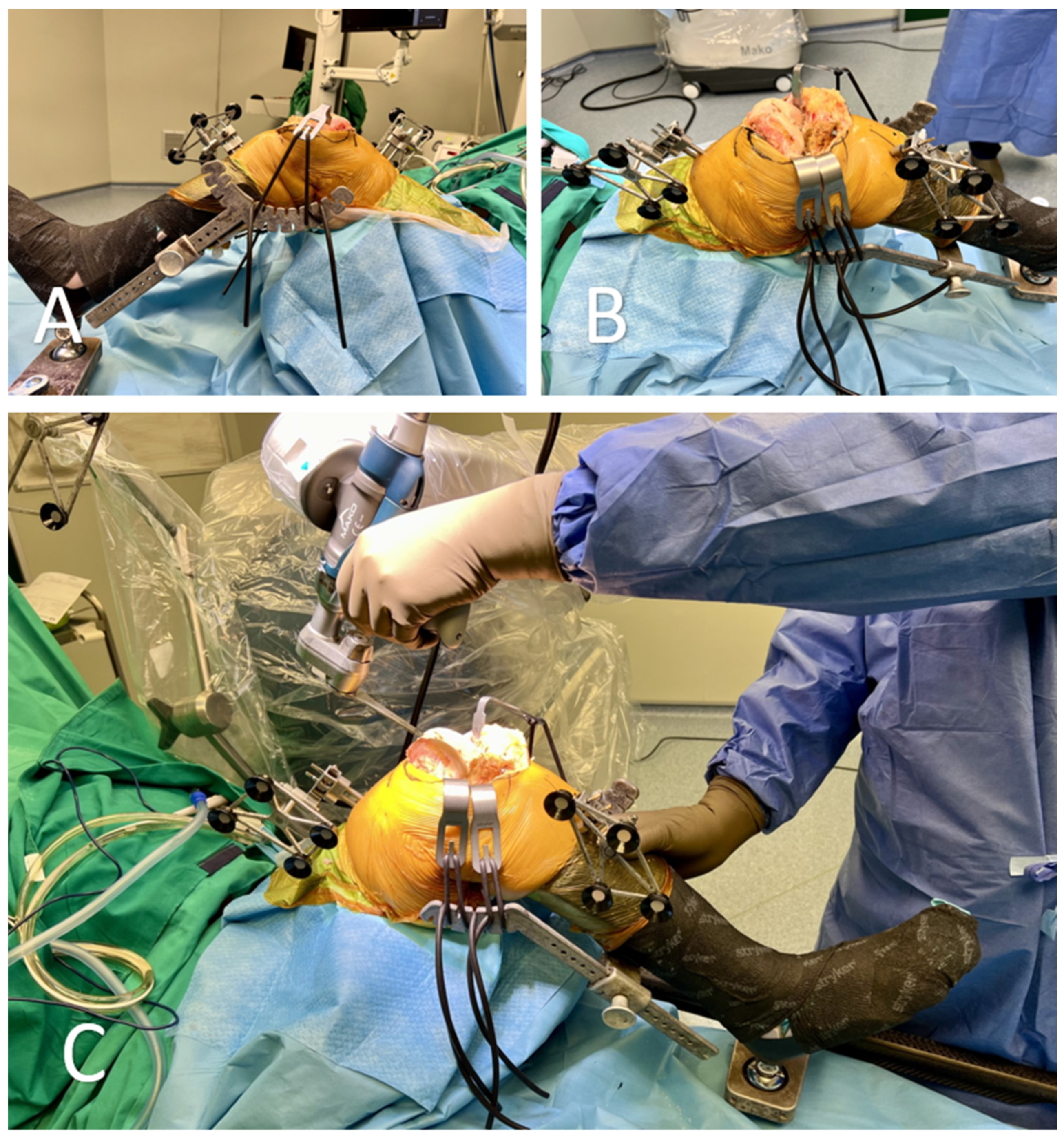
2. Troubleshooting and Limitations in RATKA
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roche, M. The MAKO robotic-arm knee arthroplasty system. Arch. Orthop. Trauma. Surg. 2021, 141, 2043–2047. [Google Scholar] [CrossRef]
- Batailler, C.; Fernandez, A.; Swan, J.; Servien, E.; Haddad, F.S.; Catani, F.; Lustig, S. MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3585–3598. [Google Scholar] [CrossRef]
- Besiris, G.T.; Koutserimpas, C.; Karamitros, A.; Karaiskos, I.; Tsakalou, D.; Raptis, K.; Kourelis, K.; Paxinos, O.; Kotsirakis, A.; Vlasis, K. Topical use of tranexamic acid in primary total knee arthroplasty: A comparative study. G. Chir.-J. Ital. Surg. Assoc. 2020, 41, 126–130. [Google Scholar]
- Kalavrytinos, D.; Koutserimpas, C.; Kalavrytinos, I.; Dretakis, K. Expanding Robotic Arm-Assisted Knee Surgery: The First Attempt to Use the System for Knee Revision Arthroplasty. Case Rep. Orthop. 2020, 2020, 4806987. [Google Scholar] [CrossRef]
- Price, A.J.; Alvand, A.; Troelsen, A.; Katz, J.N.; Hooper, G.; Gray, A.; Carr, A.; Beard, D. Knee replacement. Lancet 2018, 392, 1672–1682. [Google Scholar] [CrossRef]
- Maccagnano, G.; Pesce, V.; Noia, G.; Coviello, M.; Vicenti, G.; Vitiello, R.; Ziranu, A.; Spinarelli, A.; Moretti, B. The effects of a new protocol on blood loss in total knee arthroplasty. Orthop. Rev. 2022, 14, 37625. [Google Scholar] [CrossRef]
- Zhang, J.; Ndou, W.S.; Ng, N.; Gaston, P.; Simpson, P.M.; Macpherson, G.J.; Patton, J.T.; Clement, N.D. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2677–2695. [Google Scholar] [CrossRef] [PubMed]
- Prakash, R.; Agrawal, Y. Robotic technology in total knee arthroplasty. Br. J. Hosp. Med. 2023, 84, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Koutserimpas, C.; Dretakis, K. The evolution of robotic arm-assisted arthroplasty in Greece. G. Chir.-J. Ital. Surg. Assoc. 2020, 41, 73–78. [Google Scholar]
- Vermue, H.; Luyckx, T.; de Grave, P.W.; Ryckaert, A.; Cools, A.-S.; Himpe, N.; Victor, J. Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Khlopas, A.; Sodhi, N.; Sultan, A.A.; Chughtai, M.; Molloy, R.M.; Mont, M.A. Robotic Arm–Assisted Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 2002–2006. [Google Scholar] [CrossRef] [PubMed]
- Oussedik, S.; Abdel, M.P.; Victor, J.; Pagnano, M.W.; Haddad, F.S. Alignment in total knee arthroplasty. Bone Jt. J. 2020, 102, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Pietrzak, J.R.T.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: A prospective cohort study. Bone Jt. J. 2018, 100, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Deckey, D.G.; Rosenow, C.S.; Verhey, J.T.; Brinkman, J.C.; Mayfield, C.K.; Clarke, H.D.; Bingham, J.S. Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Jt. J. 2021, 103 (Suppl. A), 74–80. [Google Scholar] [CrossRef] [PubMed]
- Khlopas, A.; Sodhi, N.; Hozack, W.J.; Chen, A.F.; Mahoney, O.M.; Kinsey, T.; Orozco, F.; Mont, M.A. Patient-Reported Functional and Satisfaction Outcomes after Robotic-Arm-Assisted Total Knee Arthroplasty: Early Results of a Prospective Multicenter Investigation. J. Knee Surg. 2020, 33, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.F.; Eccles, C.J.; Bhimani, S.J.; Denehy, K.M.; Bhimani, R.B.; Smith, L.S.; Malkani, A.L. Improved Patient Satisfaction following Robotic-Assisted Total Knee Arthroplasty. J. Knee Surg. 2021, 34, 730–738. [Google Scholar] [CrossRef]
- Marchand, R.C.; Sodhi, N.; Khlopas, A.; Sultan, A.A.; Harwin, S.F.; Malkani, A.L.; Mont, M.A. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J. Knee Surg. 2017, 30, 849–853. [Google Scholar] [CrossRef]
- Marchand, R.C.; Sodhi, N.; Anis, H.K.; Ehiorobo, J.; Newman, J.M.; Taylor, K.; Condrey, C.; Hepinstall, M.S.; Mont, M.A. One-Year Patient Outcomes for Robotic-Arm-Assisted versus Manual Total Knee Arthroplasty. J. Knee Surg. 2019, 32, 1063–1068. [Google Scholar] [CrossRef]
- Hickey, M.D.B.; Masri, B.A.; Hodgson, A.J. Can Technology Assistance be Cost Effective in TKA? A Simulation-Based Analysis of a Risk-prioritized, Practice-specific Framework. Clin. Orthop. Relat. Res. 2023, 481, 157–173. [Google Scholar] [CrossRef]
- Kayani, B.; Konan, S.; Huq, S.S.; Tahmassebi, J.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1132–1141. [Google Scholar] [CrossRef]
- Marchand, K.B.; Ehiorobo, J.; Mathew, K.K.; Marchand, R.C.; Mont, M.A. Learning Curve of Robotic-Assisted Total Knee Arthroplasty for a High-Volume Surgeon. J. Knee Surg. 2022, 35, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Naziri, Q.; Cusson, B.C.; Chaudhri, M.; Shah, N.V.; Sastry, A. Making the transition from traditional to robotic-arm assisted TKA: What to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J. Orthop. 2019, 16, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Dragosloveanu, S.; Petre, M.A.; Capitanu, B.S.; Dragosloveanu, C.D.M.; Cergan, R.; Scheau, C. Initial Learning Curve for Robot-Assisted Total Knee Arthroplasty in a Dedicated Orthopedics Center. J. Clin. Med. 2023, 12, 6950. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.; Davis, E.T.; Parsons, H.; Mannion, E.G.; Khatri, C.; Ellard, D.R.; Blyth, M.J.; Clement, N.D.; Deehan, D.; Flynn, N.; et al. Robotic Arthroplasty Clinical and cost Effectiveness Randomised controlled trial (RACER-knee): A study protocol. BMJ Open 2023, 13, e068255. [Google Scholar] [CrossRef]
- Hua, Y.; Salcedo, J. Cost-effectiveness analysis of robotic-arm assisted total knee arthroplasty. PLoS ONE 2022, 17, e0277980. [Google Scholar] [CrossRef]
- Bagaria, V.; Sadigale, O.S.; Pawar, P.P.; Bashyal, R.K.; Achalare, A.; Poduval, M. Robotic-Assisted Knee Arthroplasty (RAKA): The Technique, the Technology and the Transition. Indian. J. Orthop. 2020, 54, 745–756. [Google Scholar] [CrossRef]
| Limitations and Pitfalls (Surgeon-Related) | Recommendations and Mitigations |
|---|---|
| (1) Learning curve and duration of the procedure | Adequate training and experience |
| (2) Checkpoints and pin insertion | Ensure precise placement of pins and careful verification during the procedure. Avoid accidental movement. |
| (3) Probe registration | Adapt probe force for cartilage defects and perform registrations with gentle touches. |
| (4) Mapping | Utilize leg holders to access difficult points, and re-verify extra registration points |
| (5) Soft tissue injuries during cutting | Surgeon vigilance to prevent damage to surrounding soft tissues. Utilize the cutting window provided by the system, but do not rely on the system for the recognition of the soft tissues. |
| Limitations and Pitfalls (System-Related) | Recommendations and Mitigations |
|---|---|
| (1) Patient’s short stature and obesity | Careful pin insertion and stabilization of the patient’s leg. |
| (2) Vibration during the operation | Ensure a stable operating environment to minimize vibration effects. Use the leg holder. |
| (3) OR floor requirements | Ensure a flat and sturdy OR floor for proper system function. |
| (4) Power supply and battery capacity | Regularly monitor and maintain the power supply and battery capacity. |
| (5) High cost | Consider the cost implications for purchasing, operations, and maintenance, especially for low-volume centers. Lowering costs and non-device-specific systems may lead to a wide expansion of robotics in the future. |
| (6) Mako Product Specialist presence | Ensure the availability of a specialist for critical system aspects. |
| (7) Stryker implants limitation | Only use Stryker implants with the system as it is a closed system. Future applications may include other prostheses making the system’s application wider. |
| (8) Wireless connection interruptions | Have backup wired connections in case of interruptions. |
| (9) Saw stopping due to cable issues | Maintain and replace cables and instruments as necessary. |
| (10) Robot arm joint issues (J1–J6) | Monitor and service robot arm joints to avoid interruptions during surgery. Perform pre-surgery checks. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dretakis, K.; Koutserimpas, C. Pitfalls with the MAKO Robotic-Arm-Assisted Total Knee Arthroplasty. Medicina 2024, 60, 262. https://doi.org/10.3390/medicina60020262
Dretakis K, Koutserimpas C. Pitfalls with the MAKO Robotic-Arm-Assisted Total Knee Arthroplasty. Medicina. 2024; 60(2):262. https://doi.org/10.3390/medicina60020262
Chicago/Turabian StyleDretakis, Konstantinos, and Christos Koutserimpas. 2024. "Pitfalls with the MAKO Robotic-Arm-Assisted Total Knee Arthroplasty" Medicina 60, no. 2: 262. https://doi.org/10.3390/medicina60020262
APA StyleDretakis, K., & Koutserimpas, C. (2024). Pitfalls with the MAKO Robotic-Arm-Assisted Total Knee Arthroplasty. Medicina, 60(2), 262. https://doi.org/10.3390/medicina60020262





