Exploring Reverse Sural Flap Necrosis in Lupus-like Syndrome: Challenges and Strategies in Lower Limb Reconstruction—A Case Presentation
Abstract
1. Introduction
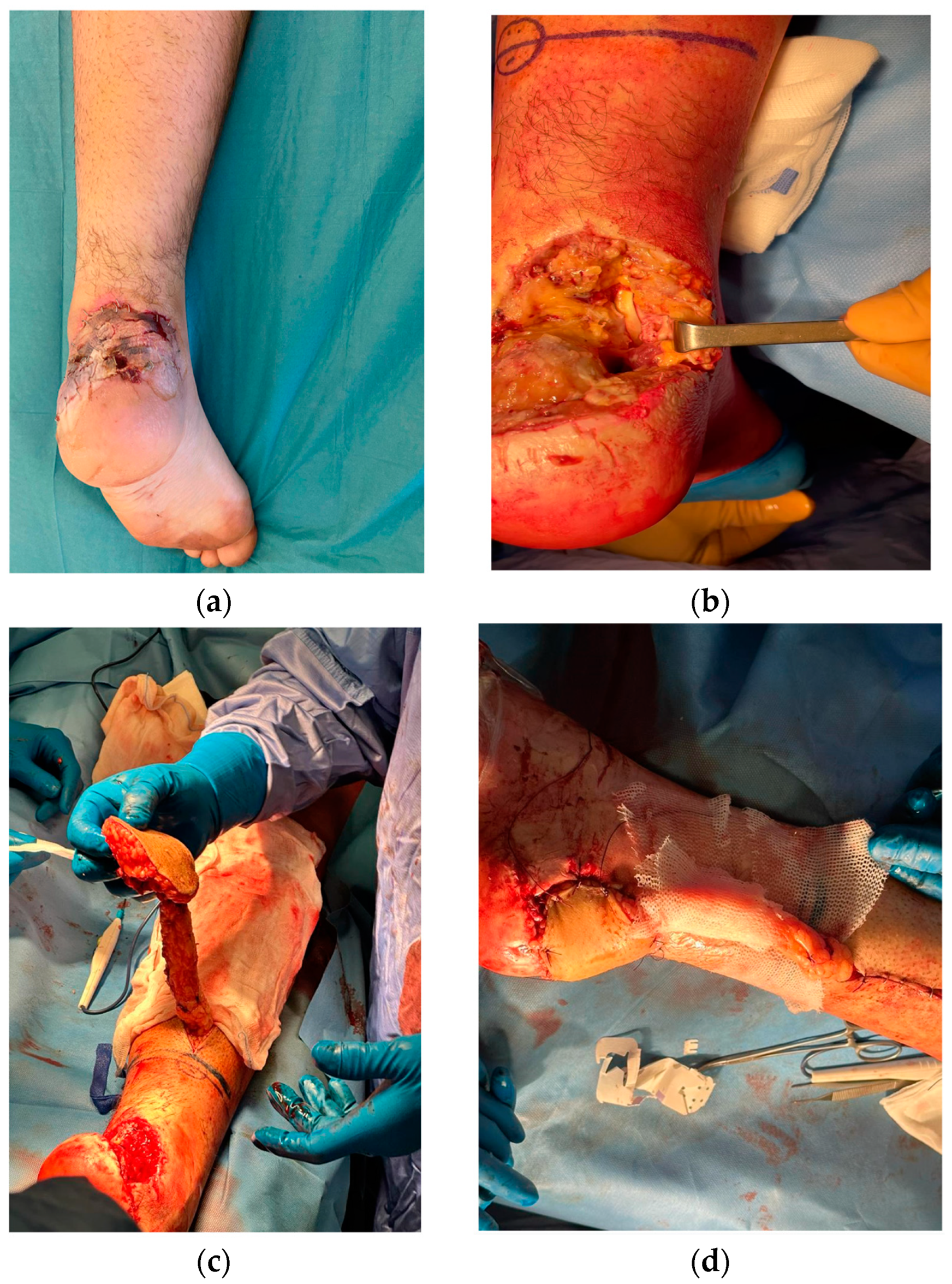
2. Case Presentation
3. Discussion
4. Conclusions
- Utility of the reverse sural flap: it is a valuable technique for addressing lower limb defects, offering good esthetic outcomes and preserving vital vessels;
- Risk of necrosis: the flap is susceptible to necrosis, making thorough preoperative assessments essential;
- Preoperative evaluations: these should include careful assessment of vascularization, autoimmune profiles, and cardiovascular conditions;
- Necrosis management: postoperative monitoring should be vigilant, with timely intervention at the first sign of compromised vascular supply.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xiong, L.; Gazyakan, E.; Kremer, T.; Hernekamp, F.J.; Harhaus, L.; Saint-Cyr, M.; Kneser, U.; Hirche, C. Free flaps for reconstruction of soft tissue defects in lower extremity: A meta-analysis on microsurgical outcome and safety. Microsurgery 2016, 36, 511–524. [Google Scholar] [CrossRef] [PubMed]
- Chi, Z.; Chen, Y.; Chu, T.; Gao, W.; Li, Z.; Yan, H.; Song, Y. Distally based sural neuro-fasciocutaneous perforator flap for foot and ankle reconstruction: Surgical modifications for flap pedicle and donor site closure without skin graft. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Donski, P.K.; Fogdestam, I. Distally based fasciocutaneous flap from the sural region. A preliminary report. Scand. J. Plast. Reconstr. Surg. 1983, 17, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Finkemeier, C.G.; Neiman, R. Reverse Sural Artery Pedicle Flap. J. Orthop. Trauma 2016, 30 (Suppl. S2), S41–S42. [Google Scholar] [CrossRef]
- Masquelet, A.C.; Romana, M.C.; Wolf, G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: Anatomic study and clinical experience in the leg. Plast. Reconstr. Surg. 1992, 89, 1115–1121. [Google Scholar] [CrossRef]
- Yilmaz, M.; Karatas, O.; Barutcu, A. The distally based superficial sural artery island flap: clinical experiences and modifications. Plast. Reconstr. Surg. 1998, 102, 2358–2367. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.H.; Tan, B.K.; Song, C. The perforator-sparing variant of the reverse sural artery flap for lower extremity reconstruction. Plast. Reconstr. Surg. 2007, 119, 2091–2098. [Google Scholar]
- Ozturk, C.N.; Ozturk, C.; Weinfeld, A.B. Use of reverse sural artery flap for reconstruction of lower extremity wounds: A review of 68 cases. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 58–64. [Google Scholar]
- Robertson, S.A.; Jeevaratnam, J.A.; Agrawal, A.; Cutress, R.I. Mastectomy skin flap necrosis: challenges and solutions. Breast Cancer 2017, 9, 141–152. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ekrol, I.; Brøgger, H.; Bruland, O.S. Venous insufficiency as a risk factor for flap necrosis after reconstructive surgery. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1997, 31, 111–116. [Google Scholar]
- Bengur, F.B.; Saadoun, R.; Moroni, E.A.; Khan, N.I.; Bottegal, M.T.; Sridharan, S.; Kubik, M.W.; Solari, M.G. Venous Thromboembolism Rates After Free Flap Reconstruction of the Head and Neck Region. Ann. Plast. Surg. 2023, 90, S447–S451. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.S.; Camacho, J.M.; Shifchik, A.; Kalmanovich, J.; Burke, E.; Harb, S.; Patrus, A.; Cheng, D.; Behnam, A. From Risk Assessment to Intervention: A Systematic Review of Thrombosis in Plastic Surgery. Cureus 2023, 15, e41557. [Google Scholar] [CrossRef] [PubMed]
- Boissiere, F.; Gandolfi, S.; Riot, S.; Kerfant, N.; Jenzeri, A.; Hendriks, S.; Grolleau, J.L.; Khechimi, M.; Herlin, C.; Chaput, B. Flap Venous Congestion and Salvage Techniques: A Systematic Literature Review. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3327. [Google Scholar] [CrossRef] [PubMed]
- Herlin, C.; Bertheuil, N.; Bekara, F.; Boissiere, F.; Sinna, R.; Chaput, B. Leech therapy in flap salvage: Systematic review and practical recommendations. Ann. Chir. Plast. Esthet. 2017, 62, e1–e13. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Li, H.; Chow, Y.; Blake, W. Non-operative adjuncts for the prevention of mastectomy skin flap necrosis: A systematic review and meta-analysis. ANZ J. Surg. 2023, 93, 65–75. [Google Scholar] [CrossRef]
- Odorico, S.K.; Reuter Munoz, K.; Nicksic, P.J.; Gunderson, K.A.; Wood, K.; Nkana, Z.H.; Bond, E.; Poore, S.O. Surgical and demographic predictors of free flap salvage after takeback: A systematic review. Microsurgery 2023, 43, 78–88. [Google Scholar] [CrossRef]
- Shen, A.Y.; Lonie, S.; Lim, K.; Farthing, H.; Hunter-Smith, D.J.; Rozen, W.M. Free Flap Monitoring, Salvage, and Failure Timing: A Systematic Review. J. Reconstr. Microsurg. 2021, 37, 300–308. [Google Scholar] [CrossRef]
- Dang, J.; Lin, M.; Tan, C.; Pham, C.H.; Huang, S.; Hulsebos, I.F.; Yenikomshian, H.; Gillenwater, J. Use of Infrared Thermography for Assessment of Burn Depth and Healing Potential: A Systematic Review. J. Burn Care Res. 2021, irab108. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.B.; Ferreira, C.H.V.; de Mendonca, P.G.M.; Sorrenti, L.; Kiyohara, L.Y. Harvesting Sural Flap with Covered Pedicle. Acta Ortop. Bras. 2023, 31, e257850. [Google Scholar] [CrossRef]
- Ciofu, R.N.; Zamfirescu, D.G.; Popescu, S.A.; Lascar, I. Reverse sural flap for ankle and heel soft tissues reconstruction. J. Med. Life 2017, 10, 94–98. [Google Scholar]
- Tripathee, S.; Basnet, S.J.; Lamichhane, A.; Hariani, L. How Safe Is Reverse Sural Flap?: A Systematic Review. Eplasty 2022, 22, e18. [Google Scholar] [PubMed]
- Clivatti, G.M.; Nascimento, B.B.D.; Ribeiro, R.D.A.; Milcheski, D.A.; Ayres, A.M.; Gemperli, R. Reverse Sural Flap for Lower Limb Reconstruction. Acta Ortop. Bras. 2022, 30, e248774. [Google Scholar] [CrossRef] [PubMed]
- Park, K.H.; Oh, C.W.; Kim, J.W.; Lee, H.J.; Kim, H.J. Reliability of reverse sural artery fasciocutaneous flap in older adult patients: Comparison study between older and younger patients. Injury 2023, 54, 110915. [Google Scholar] [CrossRef]
- Puneky, G.A.; Batchler, K.A.; Kollapaneni, S.S.; Blair, J.A.; Davis, J.M. Simplified soft tissue coverage of the distal lower extremity: The reverse sural flap. OTA Int. 2023, 6, e235. [Google Scholar] [CrossRef] [PubMed]
- Yammine, K.; Eric, M.; Nasser, J.; Chahine, A. Effectiveness of the Reverse Sural Flap in Covering Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. Plast. Surg. (Oakv) 2022, 30, 368–377. [Google Scholar] [CrossRef]
- Baumeister, S.P.; Spierer, R.; Erdmann, D.; Sweis, R.; Levin, L.S.; Germann, G.K. A realistic complication analysis of 70 sural artery flaps in a multimorbid patient group. Plast. Reconstr. Surg. 2003, 112, 129–140. [Google Scholar] [CrossRef]
- Grandjean, A.; Romana, C.; Fitoussi, F. Distally based sural flap for ankle and foot coverage in children. Orthop. Traumatol. Surg. Res. 2016, 102, 111–116. [Google Scholar] [CrossRef]
- O’Donnell, T.F., Jr.; Passman, M.A. Clinical practice guidelines of the Society for Vascular Surgery (SVS) and the American Venous Forum (AVF)—Management of venous leg ulcers. Introduction. J. Vasc. Surg. 2014, 60, 1S–2S. [Google Scholar] [CrossRef]
- Cuomo, R.; Diluiso, G.; Ruben Giardino, F.; Nisi, G.; Grimaldi, L. The Present and the Future of ALT Free Flap: Regeneration Concept in Lower Extremities Reconstruction. J. Investig. Surg. 2021, 34, 643–644. [Google Scholar] [CrossRef]
- Cuomo, R.; Nisi, G.; Brandi, C.; Grimaldi, L. Pedicled Skin Flaps of the Face: What to Keep in Mind. J. Investig. Surg. 2020, 33, 673–674. [Google Scholar] [CrossRef]
- Livermore, N.R.; Schoenbrunner, A.R.; Janis, J.E. A Critical Examination of the Science and Role of Compression Garments in Aesthetic Surgery. Plast. Reconstr. Surg. 2021, 148, 682e–685e. [Google Scholar] [CrossRef] [PubMed]
- Casella, D.; Fusario, D.; Pesce, A.L.; Marcasciano, M.; Lo Torto, F.; Luridiana, G.; De Luca, A.; Cuomo, R.; Ribuffo, D. Portable Negative Pressure Wound Dressing in Oncoplastic Conservative Surgery for Breast Cancer: A Valid Ally. Medicina 2023, 59, 1703. [Google Scholar] [CrossRef]
- Pozzi, M.; Cuomo, R.; Giardino, F.R.; Brandi, C.; Nisi, G.; Grimaldi, L. A case of necrotizing fasciitis from a pedicure: When beauty centers become life-threatening. Acta Biomed. 2022, 93, e2022126. [Google Scholar] [CrossRef]
- Torre, G.; Avvedimento, S.; Guastafierro, A.; Faenza, M.; Pieretti, G.; Cuomo, R.; Izzo, S.; Ciccarelli, F. Brachial plexus block versus wide-awake local anaesthesia for open reduction internal fixation surgery in distal radius fracture: A preliminary retrospective report. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2776–2820. [Google Scholar] [CrossRef] [PubMed]
- Karacalar, A. Axial bilobed flap based on the median and medial superficial sural arteries: A case report. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2001, 35, 207–210. [Google Scholar] [CrossRef]
- Bello, N.; Meyers, K.J.; Workman, J.; Marcano Belisario, J.; Cervera, R. Systematic Literature Review and Meta-analysis of Venous Thromboembolism Events in Systemic Lupus Erythematosus. Rheumatol. Ther. 2023, 10, 7–34. [Google Scholar] [CrossRef]
- Cuomo, R.; Nisi, G.; Brandi, C.; Grimaldi, L. Surgical Implications of Ischemia Reperfusion Damage and Future Perspectives. J. Investig. Surg. 2021, 34, 118–119. [Google Scholar] [CrossRef]
- Erdmann, D.; Levin, S. Delayed reverse sural flap for staged reconstruction of the foot and lower leg. Plast. Reconstr. Surg. 2006, 118, 571–572. [Google Scholar] [CrossRef]
- Türker, T.; Hines, E.; Haddad, D. Hemodynamics in Distally Based Sural Flaps for Lower Leg Reconstruction: A Literature Review. J. Hand Microsurg. 2023, 15, 253–257. [Google Scholar] [CrossRef]
- Athanaselis, E.D.; Fyllos, A.; Zibis, A.H.; Karachalios, T.; Hantes, M.; Dailiana, Z.; Malizos, K.; Varitimidis, S. A single-center surgical experience with the reverse sural artery flap as a reliable solution for lower leg soft tissue defects, with minimum two-year follow-up. Cureus 2021, 13. [Google Scholar] [CrossRef]
- Prakash, O.; Ali, S.S.; Khurram, M.F.; Yaseen, M. Reverse Sural Artery Flap–A Versatile Option in Distal Lower-limb Reconstruction. J. Orthop. Traumatol. Rehabil. 2024, 16, 20–23. [Google Scholar] [CrossRef]
- Wang, P.; Gu, L.; Qin, Z.; Wang, Q.; Ma, J. Efficacy and safety of topical nitroglycerin in the prevention of mastectomy flap necrosis: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 6753. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K.; Jakubietz, M.G.; Gilbert, F.; Fenwick, A.; Meffert, R.H.; Jakubietz, R.G. Muscle Cuff in Distal Pedicled Adipofascial Sural Artery Flaps: A Retrospective Case Control Study. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3464. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceccaroni, A.; Cuomo, R.; Pentangelo, P.; Gentile, A.; Marra, C.; Rozen, W.M.; Seth, I.; Lim, B.; Alfano, C. Exploring Reverse Sural Flap Necrosis in Lupus-like Syndrome: Challenges and Strategies in Lower Limb Reconstruction—A Case Presentation. Medicina 2024, 60, 2053. https://doi.org/10.3390/medicina60122053
Ceccaroni A, Cuomo R, Pentangelo P, Gentile A, Marra C, Rozen WM, Seth I, Lim B, Alfano C. Exploring Reverse Sural Flap Necrosis in Lupus-like Syndrome: Challenges and Strategies in Lower Limb Reconstruction—A Case Presentation. Medicina. 2024; 60(12):2053. https://doi.org/10.3390/medicina60122053
Chicago/Turabian StyleCeccaroni, Alessandra, Roberto Cuomo, Paola Pentangelo, Antonioenrico Gentile, Caterina Marra, Warren Matthew Rozen, Ishith Seth, Bryan Lim, and Carmine Alfano. 2024. "Exploring Reverse Sural Flap Necrosis in Lupus-like Syndrome: Challenges and Strategies in Lower Limb Reconstruction—A Case Presentation" Medicina 60, no. 12: 2053. https://doi.org/10.3390/medicina60122053
APA StyleCeccaroni, A., Cuomo, R., Pentangelo, P., Gentile, A., Marra, C., Rozen, W. M., Seth, I., Lim, B., & Alfano, C. (2024). Exploring Reverse Sural Flap Necrosis in Lupus-like Syndrome: Challenges and Strategies in Lower Limb Reconstruction—A Case Presentation. Medicina, 60(12), 2053. https://doi.org/10.3390/medicina60122053








