Prevalence of Vitamin D Deficiency Among Adults in Kazakhstan: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
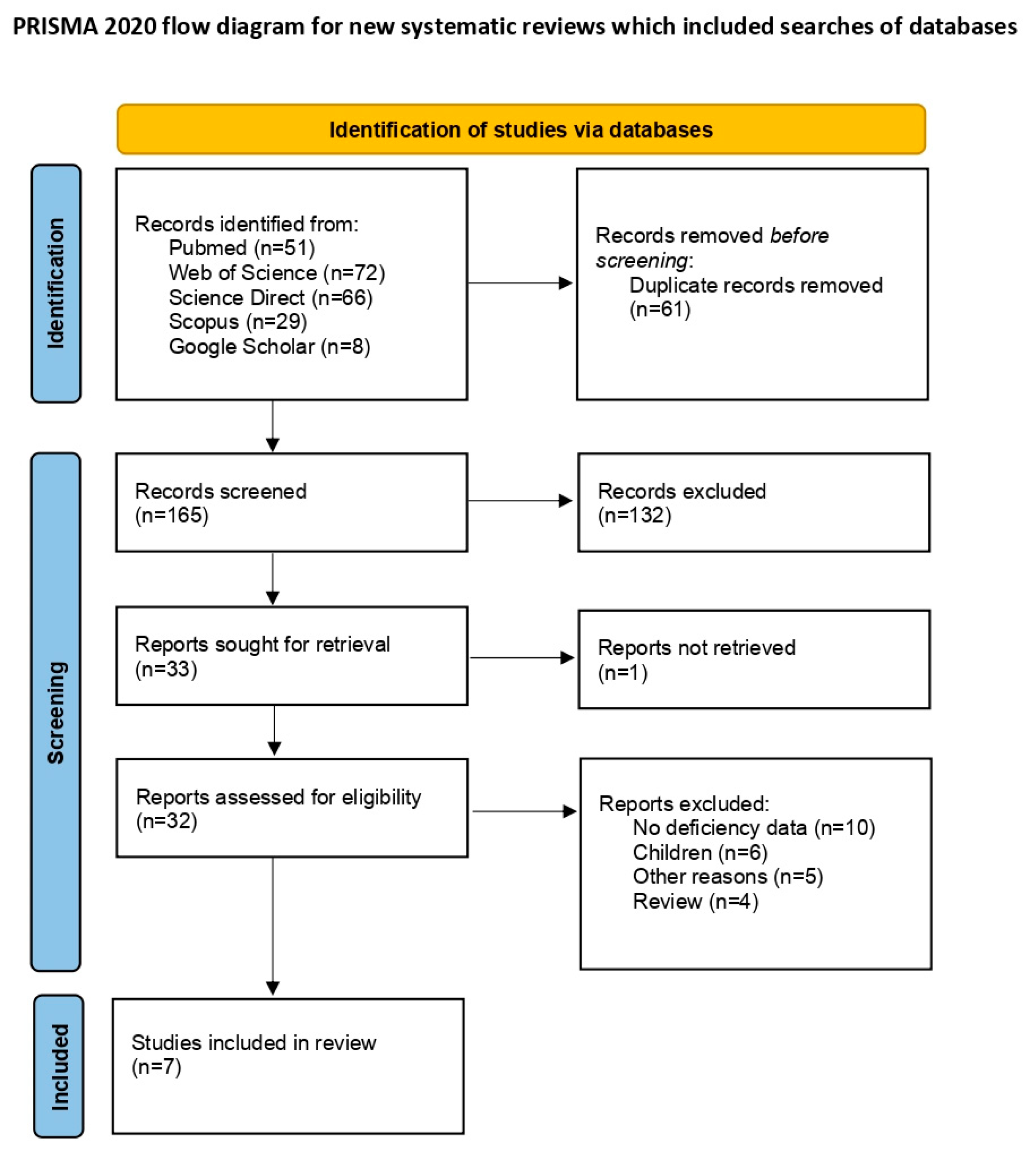
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Selection of Studies and Data Extraction
2.4. Risk of Bias (Quality) Assessment
2.5. Statistical Strategy for Data Synthesis
3. Results
3.1. Included Study Characteristics
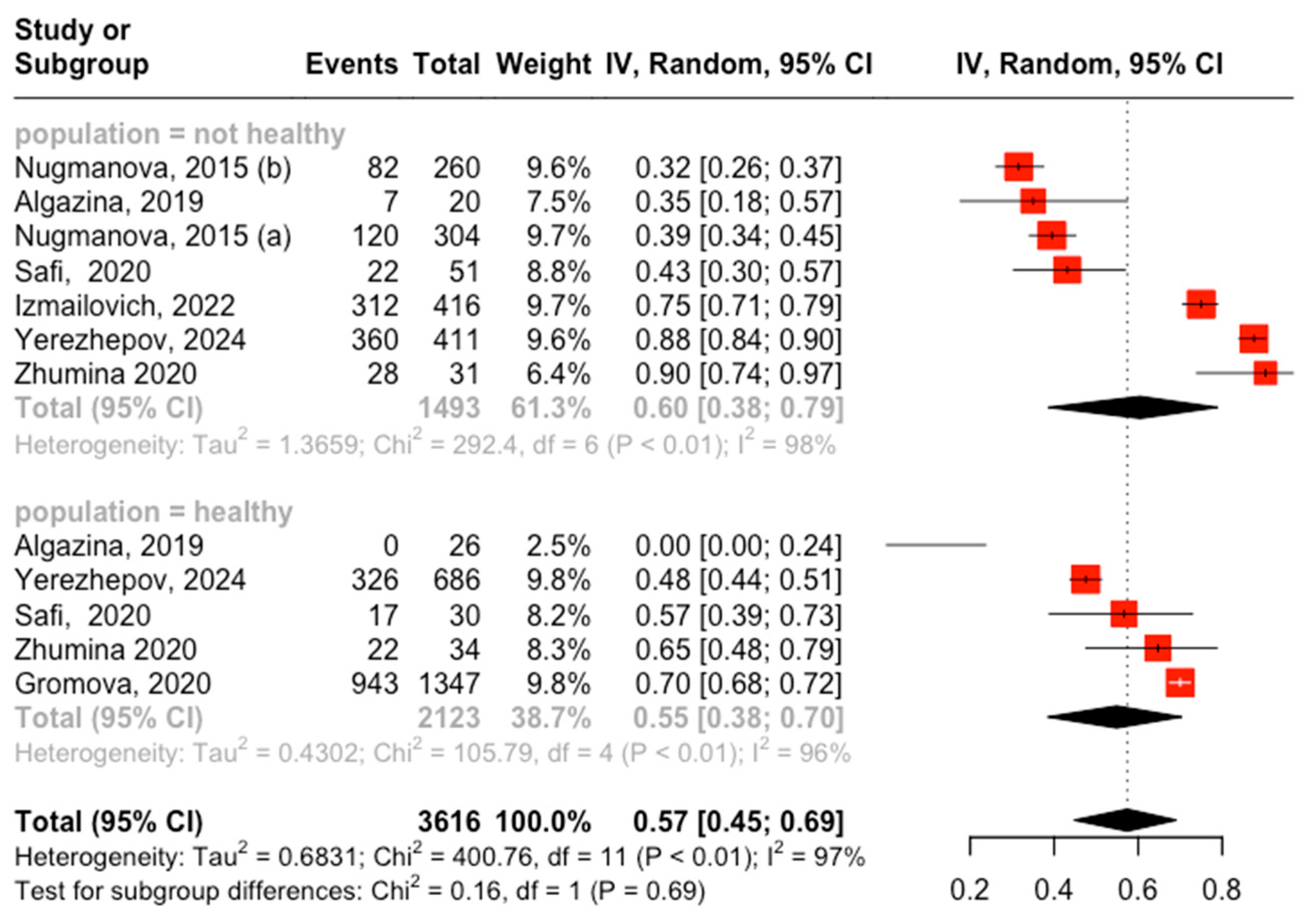
3.2. Prevalence of Vitamin D Deficiency
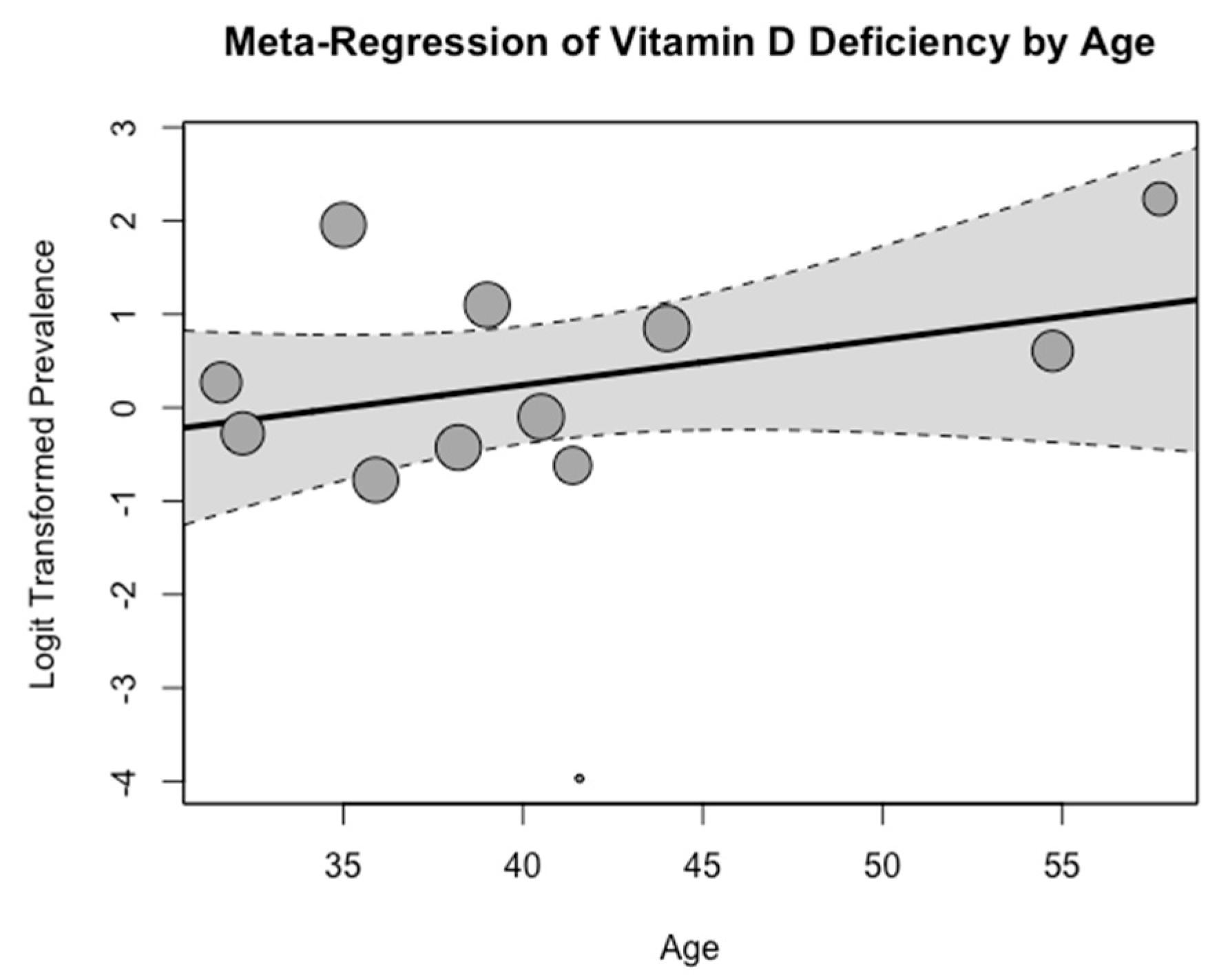
3.3. Meta-Regression Analysis
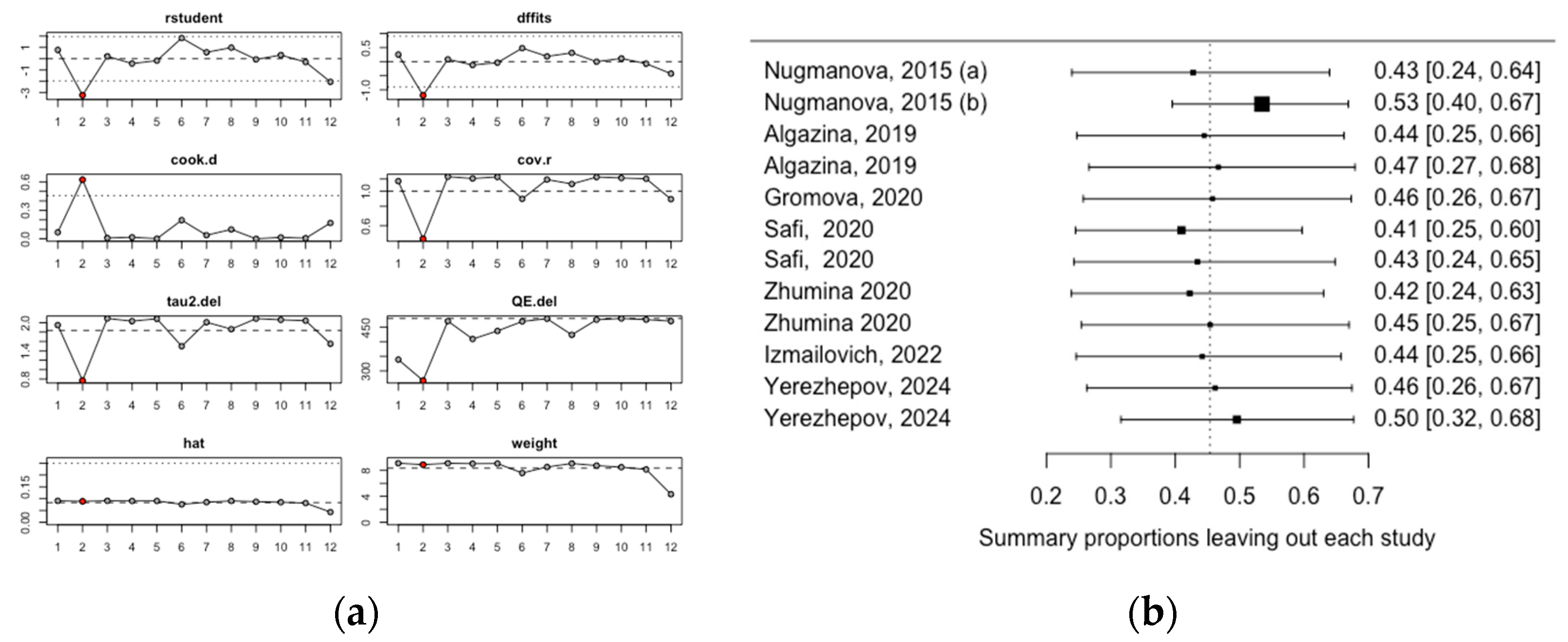
3.4. Heterogeneity Assessment
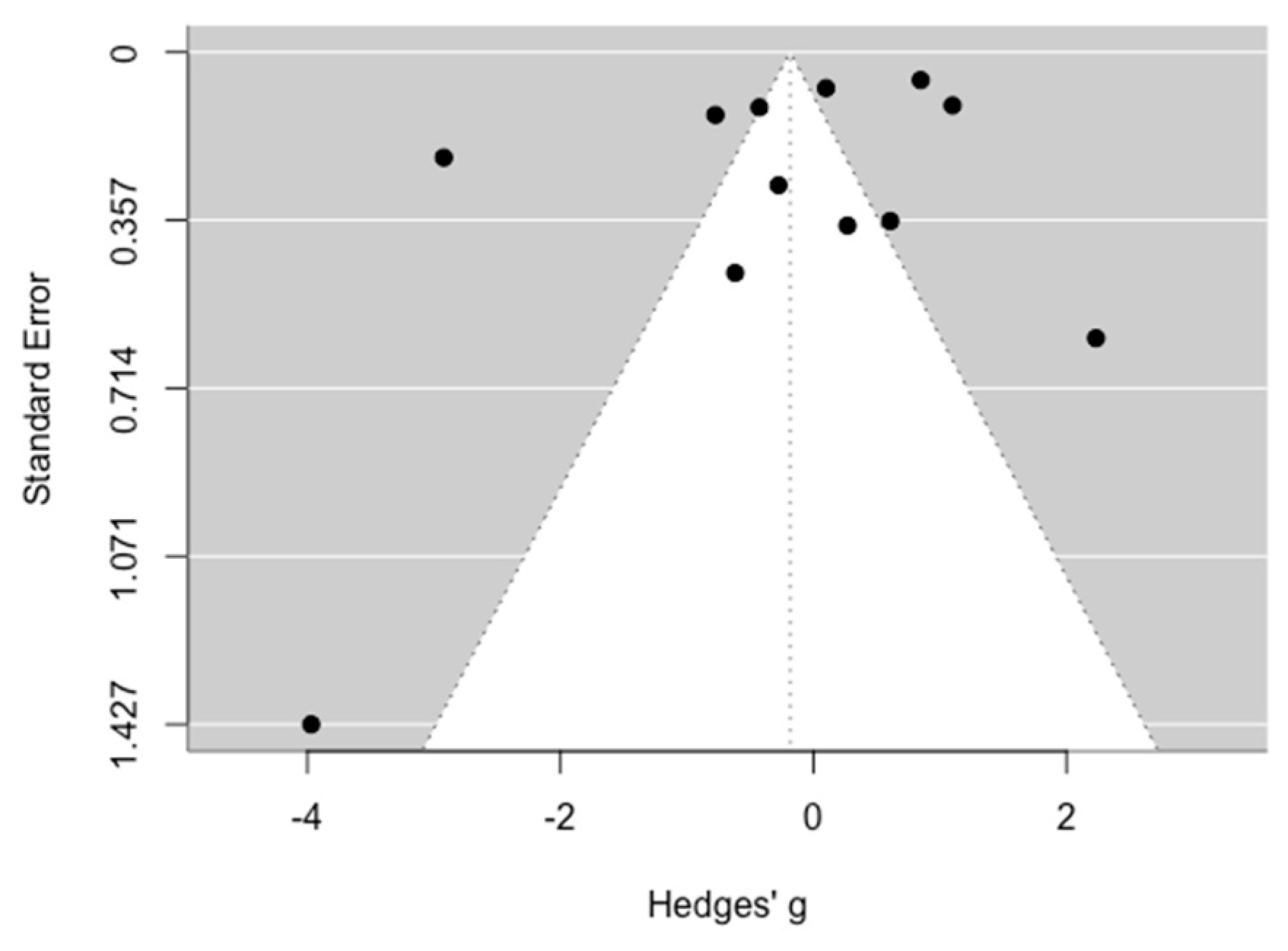
3.5. Publication Bias Assessment
3.6. Risk of Bias (Quality) Assessment Results
4. Discussion
Limitations
5. Conclusions
Future Research Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bouillon, R.; Marcocci, C.; Carmeliet, G.; Bikle, D.; White, J.H.; Dawson-Hughes, B.; Lips, P.; Munns, C.F.; Lazaretti-Castro, M.; Giustina, A.; et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr. Rev. 2019, 40, 1109–1151. [Google Scholar] [CrossRef] [PubMed]
- Minich, D.M.; Henning, M.; Darley, C.; Fahoum, M.; Schuler, C.B.; Frame, J. Is Melatonin the “Next Vitamin D”?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements. Nutrients 2022, 14, 3934. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma Concentrations of 25-Hydroxyvitamin D in Meat Eaters, Fish Eaters, Vegetarians and Vegans: Results from the EPIC-Oxford Study. Public Health Nutr. 2011, 14, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Grant, W.B.; Karras, S.N.; Zittermann, A.; Pilz, S. Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 Μg) of Vitamin D for Adults in the General Population. Nutrients 2024, 16, 391. [Google Scholar] [CrossRef]
- van Schoor, N.; de Jongh, R.; Lips, P. Worldwide Vitamin D Status. Feldman Pike’s Vitam. D 2024, 2, 47–75. [Google Scholar] [CrossRef]
- Ma, S.; Li, W.; Tojibaev, K.S.; Turginov, O.; Yang, W.; Ma, K. Regionwide and Nationwide Floristic Richness Reveal Vascular Plant Diversity in Central Asia. Plants 2024, 13, 2275. [Google Scholar] [CrossRef]
- Gromova, O.; Doschanova, A.; Lokshin, V.; Tuletova, A.; Grebennikova, G.; Daniyarova, L.; Kaishibayeva, G.; Nurpeissov, T.; Khan, V.; Semenova, Y.; et al. Vitamin D Deficiency in Kazakhstan: Cross-Sectional Study. J. Steroid Biochem. Mol. Biol. 2020, 199, 105565. [Google Scholar] [CrossRef]
- Yerezhepov, D.; Gabdulkayum, A.; Akhmetova, A.; Kozhamkulov, U.A.; Rakhimova, S.E.; Kairov, U.Y.; Zhunussova, G.; Kalendar, R.N.; Akilzhanova, A. Vitamin D Status, VDR, and TLR Polymorphisms and Pulmonary Tuberculosis Epidemiology in Kazakhstan. Nutrients 2024, 16, 558. [Google Scholar] [CrossRef]
- Akhmetova, V.; Balji, Y.; Kandalina, Y.; Iskineyeva, A.; Mukhamejanova, A.; Baspakova, A.; Uzakov, Y.; Issayeva, K.; Zamaratskaia, G. Self-Reported Consumption Frequency of Meat and Fish Products among Young Adults in Kazakhstan. Nutr. Health 2024, 30, 309–318. [Google Scholar] [CrossRef]
- National Institute for Health and Care Research PROSPERO. International Prospective Register of Systematic Reviews. Available online: https://www.crd.york.ac.uk/prospero/ (accessed on 27 March 2024).
- Karibayeva, I.; Abydynova, A. PROSPERO. Available online: https://www.crd.york.ac.uk/prospero/#recordDetails (accessed on 20 November 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Ottawa Hospital Research Institute. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 20 November 2024).
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ 2017, 358, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Posit team RStudio: Integrated Development Environment for R. Available online: http://www.posit.co/ (accessed on 22 January 2024).
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide; Chapman & Hall/CRC Press: Boca Raton, FL, USA; London, UK, 2021; Volume Chapter 4, ISBN 978-0-367-61007-4. [Google Scholar]
- Zhumalina, A.K.; Kim, I.S.; Delyagin, W.M. Vitamin D Level and Indicators of Bone Tissue Metabolism in Kazakh Infants. Russ. Fam. Dr. 2023, 27, 23–29. [Google Scholar] [CrossRef]
- Zhumalina, A.; Tusupkaliev, B.; Mania, A.; Kim, I.; Zharlykasinova, M. The Importance of Determining the Level of Bone Metabolism Markers and Vitamin D in the First Year of Life in the Kazakh Population. J. Pediatr. Pharmacol. Ther. 2024, 29, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Donayeva, A.; Amanzholkyzy, A.; Abdelazim, I.A.; Rakhyzhanova, S.; Mannapova, A.; Abilov, T.; Khamidullina, Z.; Bimagambetova, K.; Gubasheva, G.; Kulzhanova, D.; et al. The Relationship between Vitamin D and Adolescents’ Parathyroid Hormone and Bone Mineral Density. Prz. Menopauzalny 2024, 23, 1–5. [Google Scholar] [CrossRef]
- Amanzholkyzy, A.; Donayeva, A.; Kulzhanova, D.; Abdelazim, I.A.; Abilov, T.; Baubekov, Z.; Samaha, I.I. Relation between Vitamin D and Adolescents’ Serum Prolactin. Prz. Menopauzalny 2023, 22, 202–206. [Google Scholar] [CrossRef]
- Donayeva, A.; Amanzholkyzy, A.; Abdelazim, I.A.; Saparbayev, S.; Nurgaliyeva, R.; Kaldybayeva, A.; Zhexenova, A.; Stankevicius, E.; Khamidullina, Z.; Gubasheva, G.; et al. The Relation between Vitamin D and the Adolescents’ Mid-Luteal Estradiol and Progesterone. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 6792–6799. [Google Scholar] [CrossRef]
- Donayeva, A.; Kulzhanova, D.; Amanzholkyzy, A.; Abdelazim, I.A.; Abilov, T.; Baubekov, Z.; Samaha, I.I. Relationship between Vitamin D and Adolescents’ Hypothyroidism—A Cross-Sectional Study. Prz. Menopauzalny 2023, 22, 186–190. [Google Scholar] [CrossRef]
- Nugmanova, Z.S.; Patel, N.; Akhmetova, G.M.; Kurmangalieva, G.S.; Abdumananova, M.K.; Akanov, A.A.; Kovtunenko, N.G.; McNutt, L.A. Relationship between Vitamin D and Human Immunodeficiency Virus (HIV) Viral Load among HIV-Infected Patients in Kazakhstan. J. Infect. Dev. Ctries. 2015, 9, 1277–1283. [Google Scholar] [CrossRef][Green Version]
- Algazina, T.; Touir, G.; Pshembayeva, S.; Jetpisbayeva, Z.; Batpenova, G. The Role of Vitamin D in the Development of Psoriasis and Acne. Georgian Med. News 2019, 290, 96–100. [Google Scholar]
- Safi, A.; Orazov, M.; Kalinchenko, S. The Role of Cholecalciferol Deficiency in the Pathogenesis of Polycystic Ovary Syndrome. Women’s Health 2020, 16, 1745506520969606–1745506520969616. [Google Scholar] [CrossRef]
- Zhumina, A.G.; Li, K.; Konovalova, A.A.; Li, Y.A.; Ishmuratova, M.Y.; Pogossyan, G.P.; Danilenko, M. Plasma 25-Hydroxyvitamin D Levels and VDR Gene Expression in Peripheral Blood Mononuclear Cells of Leukemia Patients and Healthy Subjects in Central Kazakhstan. Nutrients 2020, 12, 1229. [Google Scholar] [CrossRef] [PubMed]
- Izmailovich, M.; Gazaliyeva, M.; Glushkova, N.; Semenova, Y.; Burankulova, S.; Shaydarova, S.; Bayazitova, M.; Kuznetsova, I. Association between Serum 25-Hydroxyvitamin D Concentration and Severity of Seasonal Allergic Rhinitis in Karaganda Region (Kazakhstan). J. Clin. Med. Kazakhstan 2022, 19, 46–50. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Noncommunicable Disease Surveillance, Monitoring and Reporting. Available online: https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf (accessed on 20 November 2024).
- Karibayeva, I.; Moiynbayeva, S.; Akhmetov, V.; Yerkenova, S.; Shaikova, K.; Moshkalova, G.; Mussayeva, D.; Tarakova, B.; Semenova, Y.; Ivankov, A.; et al. Interrupted Time Series Analysis of the Impact of the COVID-19 Pandemic and Compulsory Social Health Insurance System on Fertility Rates: A Study of Live Births in Kazakhstan, 2019–2023. Front. Public Health 2024, 12, 1454420–1454430. [Google Scholar] [CrossRef] [PubMed]
- Tochieva, Z.U.; Iskakova, F.A.; Abzaliev, K. Dynamics of Deaths and Mortality Rate in Kazakhstan Population. Heart Vessel. Transplant. 2023, 7, 1–10. [Google Scholar] [CrossRef]
- Kornberg, S.; Gundersen, M. Kazakhstan to Move to Single Time Zone in March. Available online: https://www.timeanddate.com/news/time/kazakhstan-single-time-zone.html (accessed on 20 November 2024).
- Demay, M.B.; Pittas, A.G.; Bikle, D.D.; Diab, D.L.; Kiely, M.E.; Lazaretti-Castro, M.; Lips, P.; Mitchell, D.M.; Murad, M.H.; Powers, S.; et al. Vitamin D for the Prevention of Disease: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2024, 109, 1907–1947. [Google Scholar] [CrossRef]
- Marwaha, R.K.; Dabas, A. Interventions for Prevention and Control of Epidemic of Vitamin D Deficiency. Indian. J. Pediatr. 2019, 86, 532–537. [Google Scholar] [CrossRef]
- Cooper, A. The Role of Advanced Nursing Practitioners in Improving Chronic Disease Management: A Quantitative Analysis. Res. Rev. J. Nurs. Health Sci. 2023, 9, 1–2. [Google Scholar] [CrossRef]
- Gregor, R.A.; Sebach, A.M. Nurse Practitioner–Led Vitamin D Screening and Supplementation Program in Rural Primary Care. J. Nurse Pract. 2022, 18, 155–158. [Google Scholar] [CrossRef]
- Shepin, O.; Petruchuk, O.; Korotkih, R.; Davletshin, F. The Dispanserization and Public Health. Report 2: The Population Health and the Organization of Preventive Medical Examinations. Probl. Sotsialnoi Gig. Zdr. Istor. Med. 2011, 3, 3–7. [Google Scholar]
- Al-Oanzi, Z.H.; Alenazy, F.O.; Alhassan, H.H.; Alruwaili, Y.; Alessa, A.I.; Alfarm, N.B.; Alanazi, M.O.; Alghofaili, S.I. The Role of Vitamin D in Reducing the Risk of Metabolic Disturbances That Cause Cardiovascular Diseases. J. Cardiovasc. Dev. Dis. 2023, 10, 209. [Google Scholar] [CrossRef]
- Rebelos, E.; Tentolouris, N.; Jude, E. The Role of Vitamin D in Health and Disease: A Narrative Review on the Mechanisms Linking Vitamin D with Disease and the Effects of Supplementation. Drugs 2023, 83, 665–685. [Google Scholar] [CrossRef]
| First Author, Year | Region/City | Study Design | Disease Name/Healthy | Sample | Male | Age (Mean ± SD) | 25(OH)D (ng/mL) (Mean ± SD) | Numberwith VDD |
|---|---|---|---|---|---|---|---|---|
| Nugmanova, 2015 [23] | Almaty | Case–control | HIV undet. (a) HIV det. (b) | 304 (a) 260 (b) | 168 (a) 143 (b) | 38.2 ± 9.0 (a) 35.9 ± 8.7 (b) | 25.90 ± 13.20 (a) 26.40 ± 11.40 (b) | 120 (a) 82 (b) |
| Algazina, 2019 [24] | Astana | Case–control | Psoriasis Healthy | 20 (NH) 26 (H) | 10 (NH) 13 (H) | 41.38 ± 4.2 (NH) 41.57 ± 5.67 (H) | NA | 7 (NH) 0 (H) |
| Gromova, 2020 [7] | Multiple | Cross-sectional | Healthy | 1347 | 528 | 44 ± 14 | NA | 943 |
| Safi, 2020 [25] | Astana | Case–control | PCOS Healthy | 51 (NH) 30 (H) | 0 0 | 18–44 | 16.25 17.52 | 22 (NH) 17 (H) |
| Zhumina, 2020 [26] | Karaganda | Case–control | Leukemia Healthy | 31 (NH) 34 (H) | 14 (NH) 17 (H) | 57.71 ± 13.7 (NH) 54.73 ± 15.1 (H) | 10.85 ± 7.00 (NH) 21.61 ± 7.78 (H) | 28 (NH) 22 (H) |
| Izmailovich, 2022 [27] | Karaganda | Cross-sectional | Allergic Rhinitis | 416 | 149 | 39 ± 8 | 16.10 ± 6.90 | 312 |
| Yerezhepov, 2024 [8] | Multiple | Case–control | Tuberculosis Healthy | 411 (NH) 686 (H) | 224 (NH) 303 (H) | 35 ± 13.1 (NH) 40.5 ± 13.9 (H) | 12.90 ± 3.80 (NH) 24.80 ± 3.10 (H) | 360 (NH) 326 (H) |
| Study | Selection | Comparability | Exposure | Total |
|---|---|---|---|---|
| Case–control studies | ||||
| Nugmanova, 2015 [23] | 4 | 1 | 3 | 8 |
| Algazina, 2019 [24] | 3 | 1 | 3 | 7 |
| Safi, 2020 [25] | 4 | 1 | 3 | 8 |
| Zhumina, 2020 [26] | 4 | 1 | 2 | 7 |
| Yerezhepov, 2024 [8] | 4 | 1 | 3 | 8 |
| Cross-sectional studies | ||||
| Gromova, 2020 [7] | 3 | 1 | 2 | 6 |
| Izmailovich, 2022 [27] | 3 | 1 | 2 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karibayeva, I.; Bilibayeva, G.; Yerzhanova, A.; Alekesheva, R.; Iglikova, A.; Maxudova, M.; Ussebayeva, N. Prevalence of Vitamin D Deficiency Among Adults in Kazakhstan: A Systematic Review and Meta-Analysis. Medicina 2024, 60, 2043. https://doi.org/10.3390/medicina60122043
Karibayeva I, Bilibayeva G, Yerzhanova A, Alekesheva R, Iglikova A, Maxudova M, Ussebayeva N. Prevalence of Vitamin D Deficiency Among Adults in Kazakhstan: A Systematic Review and Meta-Analysis. Medicina. 2024; 60(12):2043. https://doi.org/10.3390/medicina60122043
Chicago/Turabian StyleKaribayeva, Indira, Galiya Bilibayeva, Aya Yerzhanova, Roza Alekesheva, Assiya Iglikova, Makhigul Maxudova, and Neilya Ussebayeva. 2024. "Prevalence of Vitamin D Deficiency Among Adults in Kazakhstan: A Systematic Review and Meta-Analysis" Medicina 60, no. 12: 2043. https://doi.org/10.3390/medicina60122043
APA StyleKaribayeva, I., Bilibayeva, G., Yerzhanova, A., Alekesheva, R., Iglikova, A., Maxudova, M., & Ussebayeva, N. (2024). Prevalence of Vitamin D Deficiency Among Adults in Kazakhstan: A Systematic Review and Meta-Analysis. Medicina, 60(12), 2043. https://doi.org/10.3390/medicina60122043






