Increase in Strength After Multimodal Pain Management Concept in Patients with Cervical Radiculopathy—A Non-Randomized, Uncontrolled Clinical Trial
Abstract
1. Introduction
2. Aim of This Study
3. Material and Methods
3.1. Measurement
3.2. Therapeutic Procedure
3.3. Statistical Analysis
4. Results
4.1. Patients
4.2. Interrater Reliability
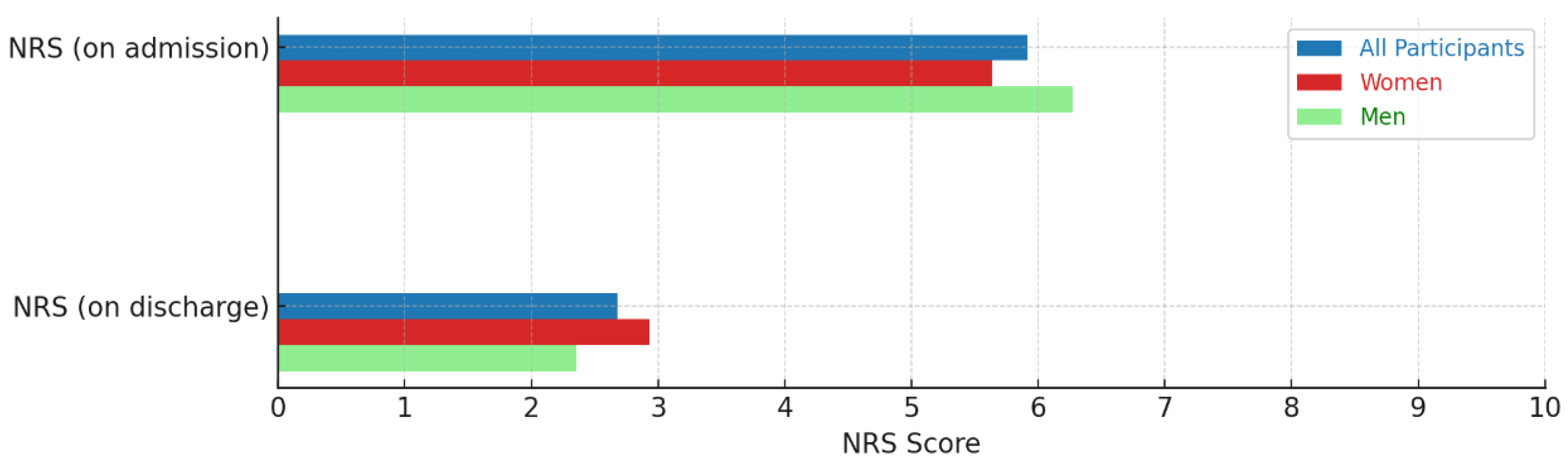
4.3. Pain Development
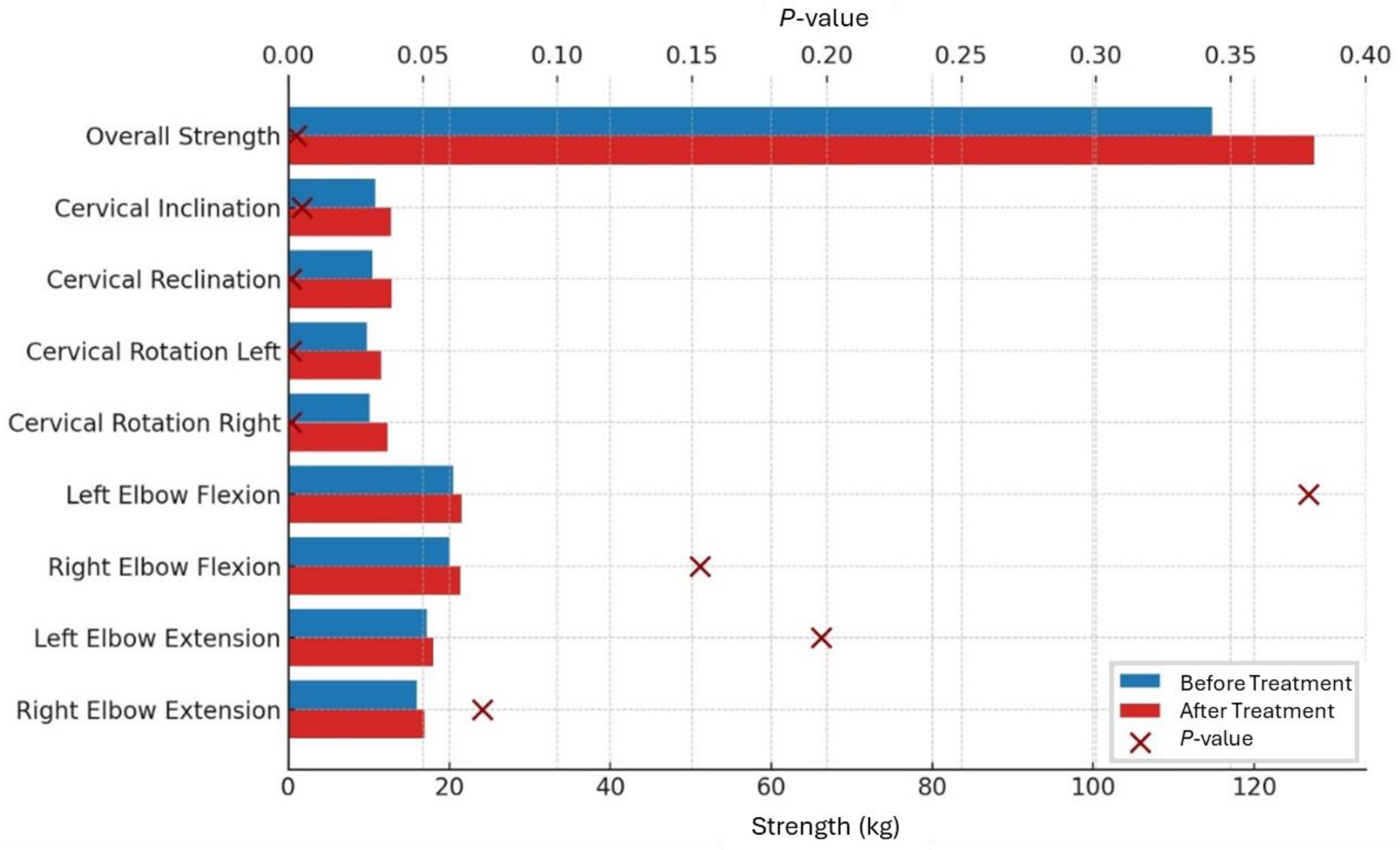
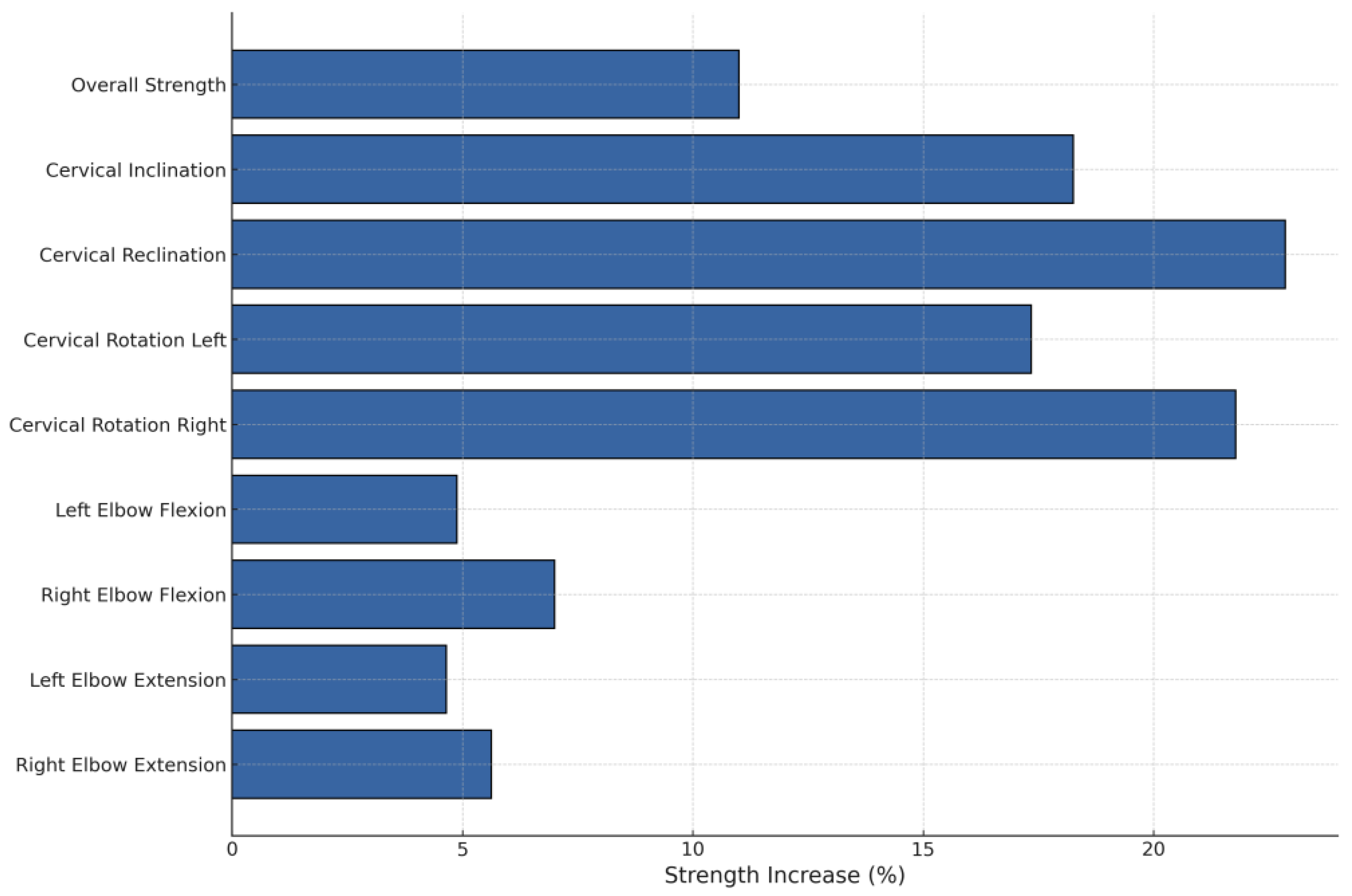
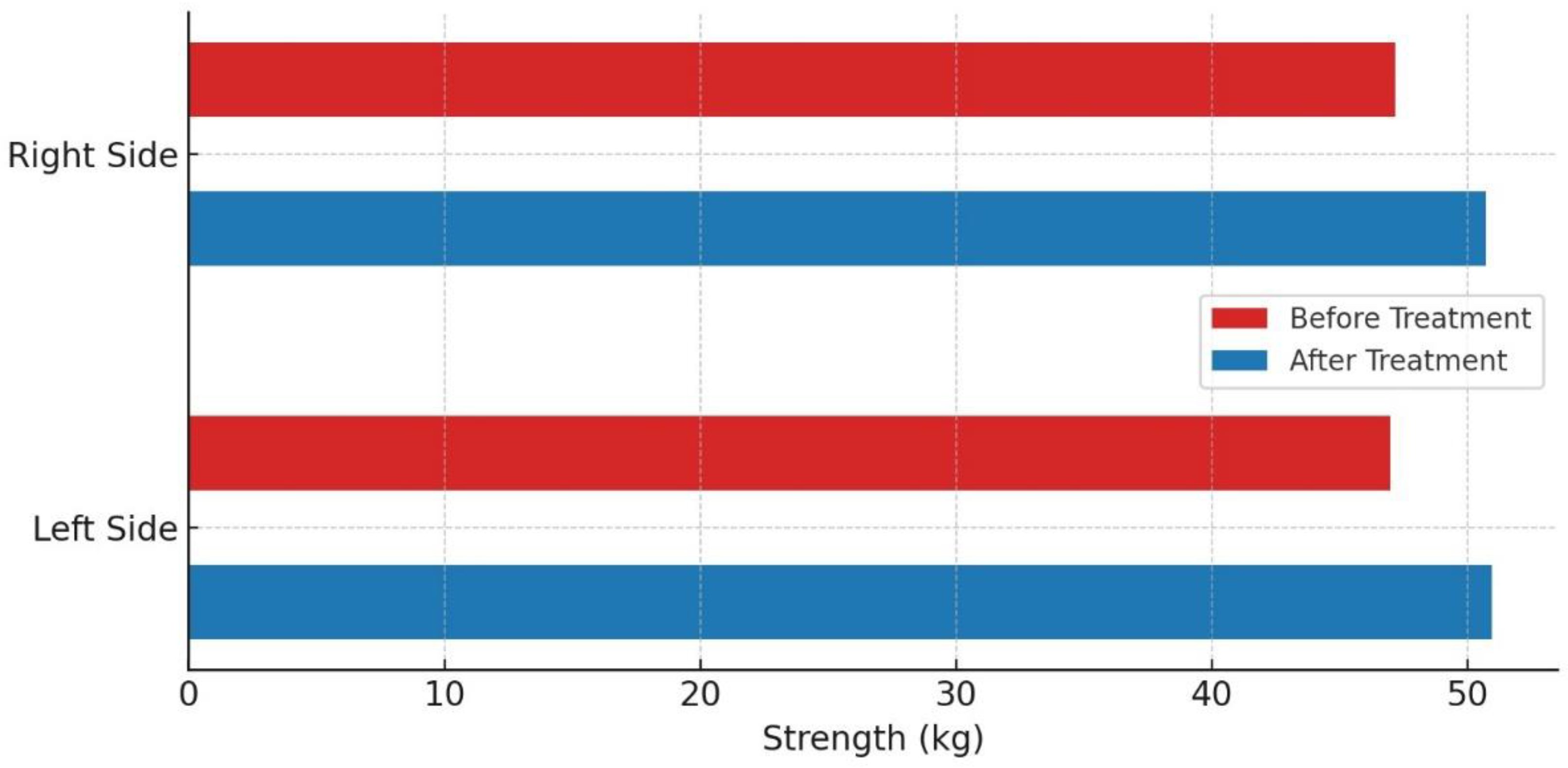
4.4. Developing Strengths
5. Discussion
6. Limitation
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Childress, M.A.; Becker, B.A. Nonoperative Management of Cervical Radiculopathy. Am. Fam. Physician 2016, 93, 746–754. [Google Scholar] [PubMed]
- González-Uriel, P. Clinical anatomy of cervical spondylosis. Eur. J. Anat. 2020. Available online: https://www.academia.edu/44592385/Clinical_anatomy_of_cervical_spondylosis (accessed on 4 November 2024).
- GBD 2021 Neck Pain Collaborators. Global, regional, and national burden of neck pain, 1990–2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2024, 6, e142. [Google Scholar] [CrossRef] [PubMed]
- Vos, C.J.; Verhagen, A.P.; Passchier, J.; Koes, B.W. Clinical Course and Prognostic Factors in Acute Neck Pain: An Inception Cohort Study in General Practice. Pain Med. 2008, 9, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Paksaichol, A.; Janwantanakul, P.; Purepong, N.; Pensri, P.; Beek, A.J. van der Office workers’ risk factors for the development of non-specific neck pain: A systematic review of prospective cohort studies. Occup. Environ. Med. 2012, 69, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Binti Karim, N.; Chowdhury Asha, A.; Aminul, I.; Mandal, A.; Islam, T.; Rahaman, K.S. Features of Neck Pain and its Related Factors Among Patients With Cervical Spondylosis. Int. J. Epidemiol. Res. 2018, 5, 92–97. [Google Scholar] [CrossRef]
- Hilderink, P.H.; Burger, H.; Deeg, D.J.; Beekman, A.T.; Oude Voshaar, R.C. The Temporal Relation Between Pain and Depression: Results From the Longitudinal Aging Study Amsterdam. Psychosom. Med. 2012, 74, 945. [Google Scholar] [CrossRef] [PubMed]
- Viana, M.C.; Lim, C.C.W.; Garcia Pereira, F.; Aguilar-Gaxiola, S.; Alonso, J.; Bruffaerts, R.; de Jonge, P.; Caldas-de-Almeida, J.M.; O’Neill, S.; Stein, D.J.; et al. Previous Mental Disorders and Subsequent Onset of Chronic Back or Neck Pain: Findings From 19 Countries. J. Pain 2018, 19, 99–110. [Google Scholar] [CrossRef]
- Xie, Y.; Coombes, B.K.; Thomas, L.; Johnston, V. Time Course and Risk Profile of Work-Related Neck Disability: A Longitudinal Latent Class Growth Analysis. Phys. Ther. 2022, 102, pzac050. [Google Scholar] [CrossRef]
- Hviid Andersen, J.; Kaergaard, A.; Frost, P.; Frølund Thomsen, J.; Peter Bonde, J.; Fallentin, N.; Borg, V.; Mikkelsen, S. Physical, Psychosocial, and Individual Risk Factors for Neck/Shoulder Pain With Pressure Tenderness in the Muscles Among Workers Performing Monotonous, Repetitive Work. Spine 2002, 27, 660. [Google Scholar] [CrossRef]
- Verwoerd, M.; Wittink, H.; Maissan, F.; de Raaij, E.; Smeets, R.J.E.M. Prognostic factors for persistent pain after a first episode of nonspecific idiopathic, non-traumatic neck pain: A systematic review. Musculoskelet. Sci. Pract. 2019, 42, 13–37. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, B.; Curran-Everett, D.; Maluf, K.S. Psychosocial, Physical, and Neurophysiological Risk Factors for Chronic Neck Pain: A Prospective Inception Cohort Study. J. Pain 2015, 16, 1288–1299. [Google Scholar] [CrossRef]
- Anderson, B.G.; Benzinger, B.; Chickness, J.; Hietanen, C.; Hill, K.; Lucas, J.-M.P.; Tuck, J.; Ghassibi, M. Effects of Cervical Spine Exercise Protocol on Neck Pain, Pericervical Muscle Endurance, and Range of Motion in Medical Students: A Prospective Study. Cureus 2022, 14, e27160. [Google Scholar] [CrossRef] [PubMed]
- Benditz, A.; Brunner, M.; Zeman, F.; Greimel, F.; Florian, V.; Boluki, D.; Grifka, J.; Weber, M.; Renkawitz, T. Effectiveness of a multimodal pain management concept for patients with cervical radiculopathy with focus on cervical epidural injections. Sci. Rep. 2017, 7, 7866. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.E.M.; Ostelo, R.W.J.G.; Guzman, J.; van Tulder, M.W. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst. Rev. 2014, 2014, CD000963. [Google Scholar] [CrossRef] [PubMed]
- Buchner, M.; Zahlten, A.; Schiltenwolf, M.; Neubauer, E. Therapy outcome after multidisciplinary treatment for chronic neck and chronic low back pain: A prospective clinical study in 365 patients. Scand. J. Rheumatol. 2006, 35, 363–367. [Google Scholar] [CrossRef]
- Panjabi, M.M.; Cholewicki, J.; Nibu, K.; Grauer, J.; Babat, L.B.; Dvorak, J. Critical load of the human cervical spine: An in vitro experimental study. Clin. Biomech. 1998, 13, 11–17. [Google Scholar] [CrossRef]
- Gross, A.; Kay, T.M.; Paquin, J.P.; Blanchette, S.; Lalonde, P.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; Gelley, G.; et al. Exercises for mechanical neck disorders. Cochrane Database Syst. Rev. 2015. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004250.pub5/full (accessed on 19 February 2024). [CrossRef]
- Berg, H.E.; Berggren, G.; Tesch, P.A. Dynamic neck strength training effect on pain and function. Arch. Phys. Med. Rehabil. 1994, 75, 661–665. [Google Scholar] [CrossRef]
- Kaka, B.; Ogwumike, O.O.; Adeniyi, A.F.; Maharaj, S.S.; Ogunlade, S.O.; Bello, B. Effectiveness of neck stabilisation and dynamic exercises on pain intensity, depression and anxiety among patients with non-specific neck pain: A randomised controlled trial. Scand. J. Pain 2018, 18, 321–331. [Google Scholar] [CrossRef]
- Salo, P.K.; Häkkinen, A.H.; Kautiainen, H.; Ylinen, J.J. Effect of neck strength training on health-related quality of life in females with chronic neck pain: A randomized controlled 1-year follow-up study. Health Qual. Life Outcomes 2010, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.S.; Meziat-Filho, N.; Ferreira, A.S.; Tedla, J.S.; Kandakurti, P.K.; Kakaraparthi, V.N. Comparison of neck extensor muscle endurance and cervical proprioception between asymptomatic individuals and patients with chronic neck pain. J. Bodyw. Mov. Ther. 2021, 26, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Burns, S.P.; Spanier, D.E. Break-technique handheld dynamometry: Relation between angular velocity and strength measurements. Arch. Phys. Med. Rehabil. 2005, 86, 1420–1426. [Google Scholar] [CrossRef] [PubMed]
- Validity and Reliability of the Numeric Rating Scale in Non-Myogenic Low Back Pain Patients|Academic Physiotherapy Conference Proceeding. Available online: https://proceedings.ums.ac.id/index.php/apc/article/view/4396 (accessed on 12 November 2024).
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Schonstein, E.; Kenny, D.; Keating, J.; Koes, B.; Herbert, R.D. Physical Conditioning Programs for Workers With Back and Neck Pain: A Cochrane Systematic Review. Spine 2003, 28, E391. [Google Scholar] [CrossRef]
- Letzel, J.; Angst, F.; Weigl, M.B. Multidisciplinary biopsychosocial rehabilitation in chronic neck pain: A naturalistic prospective cohort study with intraindividual control of effects and 12-month follow-up. Eur. J. Phys. Rehabil. Med. 2019, 55, 665–675. [Google Scholar] [CrossRef]
- Falla, D.; Lindstrøm, R.; Rechter, L.; Boudreau, S.; Petzke, F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: A randomized controlled study. Eur. J. Pain 2013, 17, 1517–1528. [Google Scholar] [CrossRef]
- Weigl, M.; Letzel, J.; Angst, F. Prognostic factors for the improvement of pain and disability following multidisciplinary rehabilitation in patients with chronic neck pain. BMC Musculoskelet. Disord. 2021, 22, 330. [Google Scholar] [CrossRef]
- Leaver, A.M.; Refshauge, K.M.; Maher, C.G.; McAuley, J.H. Conservative interventions provide short-term relief for non-specific neck pain: A systematic review. J. Physiother. 2010, 56, 73–85. [Google Scholar] [CrossRef]
- Strimpakos, N. The assessment of the cervical spine. Part 2: Strength and endurance/fatigue. J. Bodyw. Mov. Ther. 2011, 15, 417–430. [Google Scholar] [CrossRef]
- Gogia, P.P.; Sabbahi, M.A. Changes in Fatigue Characteristics of Cervical Paraspinal Muscles with Posture. Spine 1991, 16, 1135. [Google Scholar] [CrossRef] [PubMed]
- Martins, T.S.; Pinheiro-Araujo, C.F.; Gorla, C.; Florencio, L.L.; Martins, J.; Fernández-de-las-Peñas, C.; Oliveira, A.S.; Bevilaqua-Grossi, D. Neck Strength Evaluated With Fixed and Portable Dynamometers in Asymptomatic Individuals: Correlation, Concurrent Validity, and Agreement. J. Manip. Physiol. Ther. 2022, 45, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Salo, P.; Nykänen, M.; Kautiainen, H.; Häkkinen, A. Decreased isometric neck strength in women with chronic neck pain and the repeatability of neck strength measurements. Arch. Phys. Med. Rehabil. 2004, 85, 1303–1308. [Google Scholar] [CrossRef]
- Niemier, K.; Schindler, M.; Volk, T.; Baum, K.; Wolf, B.; Eberitsch, J.; Seidel, W. Efficacy of epidural steroid injections for chronic lumbar pain syndromes without neurological deficits. A randomized, double blind study as part of a multimodal treatment concept. Schmerz Berl. Ger. 2015, 29, 300–307. [Google Scholar] [CrossRef]
- O’Riordan, C.; Clifford, A.; Van De Ven, P.; Nelson, J. Chronic Neck Pain and Exercise Interventions: Frequency, Intensity, Time, and Type Principle. Arch. Phys. Med. Rehabil. 2014, 95, 770–783. [Google Scholar] [CrossRef] [PubMed]
- Romaratezabala, E.; Urrate, M.; Ramirez-Campillo, R.; Yanci, J. Effects of a Mobility and Dynamic Strength Intervention Program on the Range of Motion, Strength, and Strength Asymmetry in People with Neck or Low Back Pain. Kinesiology 2023, 55, 183–191. [Google Scholar] [CrossRef]
- Ylinen, J.; Ruuska, J. Clinical use of neck isometric strength measurement in rehabilitation. Arch. Phys. Med. Rehabil. 1994, 75, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Tudini, F. Magnitude, validity and responsiveness of dynamometer measured neck retraction strength in patients referred with neck pain to out-patient physical therapy. J. Phys. Ther. Sci. 2022, 34, 694–696. [Google Scholar] [CrossRef]
- Highland, T.R.; Dreisinger, T.E.; Vie, L.L.; Russell, G.S. Changes in isometric strength and range of motion of the isolated cervical spine after eight weeks of clinical rehabilitation. Spine 1992, 17, S77–S82. [Google Scholar] [CrossRef]
- Tudini, F.; Myers, B.; Bohannon, R. Reliability and validity of measurements of cervical retraction strength obtained with a hand-held dynamometer. J. Man. Manip. Ther. 2019, 27, 222–228. [Google Scholar] [CrossRef]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-held Dynamometry Correlation With the Gold Standard Isokinetic Dynamometry: A Systematic Review. PM&R 2011, 3, 472–479. [Google Scholar] [CrossRef]
- Vannebo, K.T.; Iversen, V.M.; Fimland, M.S.; Mork, P.J. Test-retest reliability of a handheld dynamometer for measurement of isometric cervical muscle strength. J. Back Musculoskelet. Rehabil. 2018, 31, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Selistre, L.F.A.; de Sousa Melo, C.; Noronha, M.A. de Reliability and Validity of Clinical Tests for Measuring Strength or Endurance of Cervical Muscles: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 1210–1227. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.D.; Heer, D.M.; Roy, T.C.; Santos, D.M.; Whitman, J.M.; Wainner, R.S. Reliability of a Measurement of Neck Flexor Muscle Endurance. Phys. Ther. 2005, 85, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Narayan, Y.; Amell, T. Cervical strength of young adults in sagittal, coronal, and intermediate planes. Clin. Biomech. 2001, 16, 380–388. [Google Scholar] [CrossRef]
- O’Leary, S.; Hoogma, C.; Solberg, Ø.M.; Sundberg, S.; Pedler, A.; Van Wyk, L. Comparative Strength and Endurance Parameters of the Craniocervical and Cervicothoracic Extensors and Flexors in Females With and Without Idiopathic Neck Pain. J. Appl. Biomech. 2019, 35, 209–215. [Google Scholar] [CrossRef]
- Falla, D.; O’Leary, S.; Farina, D.; Jull, G. The change in deep cervical flexor activity after training is associated with the degree of pain reduction in patients with chronic neck pain. Clin. J. Pain 2012, 28, 628–634. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kwag, K.I. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J. Phys. Ther. Sci. 2016, 28, 269–273. [Google Scholar] [CrossRef]
- Krause, D.A.; Neuger, M.D.; Lambert, K.A.; Johnson, A.E.; DeVinny, H.A.; Hollman, J.H. Effects of examiner strength on reliability of hip-strength testing using a handheld dynamometer. J. Sport Rehabil. 2014, 23, 56–64. [Google Scholar] [CrossRef]
- Thorborg, K.; Bandholm, T.; Schick, M.; Jensen, J.; Hölmich, P. Hip strength assessment using handheld dynamometry is subject to intertester bias when testers are of different sex and strength. Scand. J. Med. Sci. Sports 2013, 23, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Kiatkulanusorn, S.; Luangpon, N.; Suato, B.P.; Klarod, K.; Srijunto, W.; Wipatin, P.; Kinandana, P.; Watechagit, S.; Kaoien, C.; Werasirirat, P. Ability and Reproducibility to Exert Force for Testing Muscle Strength by a Handheld Dynamometer of the Various Examiners: Sex and Body Weight Factors. J. Exerc. Physiol. Online 2023, 26, 11–23. [Google Scholar]

| Medical Application Within MPM | Number of Treatments |
|---|---|
| Medical training therapy | 5 |
| Group exercises | 4 |
| Aqua gymnastics | 5 |
| Progressive muscle relaxation | 3 |
| Coordination training group | 4 |
| Psychological group therapy/individual therapy | 3 |
| All Participants (N = 25) | Women (N = 14) | Men (N = 11) | |
|---|---|---|---|
| Age (years) | 59.64 (42–84) | 58.78 (42–77) | 60.73 (42–84) |
| Height (centimeters) | 171.72 (150–192) | 164.5 (152–183) | 180.91 (162–192) |
| Weight (kilogram) | 81.02 (50–115) | 76.14 (50–150) | 87.23 (70–105) |
| BMI | 27.4 (20.2–42) | 27.99 (20.2–42) | 26.4 (23.6–34.6) |
| NRS (on admission) | 5.92 (2–9) | 5.64 (2–9) | 6.27 (3–8) |
| NRS (on discharge) | 2.68 (0–9) | 2.93 (0–9) | 2.36 (0–7) |
| Muscle Group | Before Treatment (kg) | After Treatment (kg) | p-Value |
|---|---|---|---|
| Overall Strength | 114.78 | 127.41 | 0.003 |
| Cervical Inclination | 10.79 | 12.76 | 0.005 |
| Cervical Reclination | 10.50 | 12.90 | <0.001 |
| Cervical Rotation Left | 9.80 | 11.50 | <0.001 |
| Cervical Rotation Right | 10.10 | 12.30 | <0.001 |
| Left Elbow Flexion | 20.50 | 21.50 | 0.379 |
| Right Elbow Flexion | 20.00 | 21.40 | 0.153 |
| Left Elbow Extension | 17.20 | 18.00 | 0.198 |
| Right Elbow Extension | 16.00 | 16.90 | 0.072 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zirkl, G.; Schaumburger, J.; Gehentges, M.; Kaiser, M. Increase in Strength After Multimodal Pain Management Concept in Patients with Cervical Radiculopathy—A Non-Randomized, Uncontrolled Clinical Trial. Medicina 2024, 60, 1961. https://doi.org/10.3390/medicina60121961
Zirkl G, Schaumburger J, Gehentges M, Kaiser M. Increase in Strength After Multimodal Pain Management Concept in Patients with Cervical Radiculopathy—A Non-Randomized, Uncontrolled Clinical Trial. Medicina. 2024; 60(12):1961. https://doi.org/10.3390/medicina60121961
Chicago/Turabian StyleZirkl, Gerd, Jens Schaumburger, Matthias Gehentges, and Moritz Kaiser. 2024. "Increase in Strength After Multimodal Pain Management Concept in Patients with Cervical Radiculopathy—A Non-Randomized, Uncontrolled Clinical Trial" Medicina 60, no. 12: 1961. https://doi.org/10.3390/medicina60121961
APA StyleZirkl, G., Schaumburger, J., Gehentges, M., & Kaiser, M. (2024). Increase in Strength After Multimodal Pain Management Concept in Patients with Cervical Radiculopathy—A Non-Randomized, Uncontrolled Clinical Trial. Medicina, 60(12), 1961. https://doi.org/10.3390/medicina60121961





