Comparison of Pudendal Nerve Block and Spinal Anesthesia in Proctological Surgeries: Efficacy, Safety, and Patient Outcomes
Abstract
1. Introduction
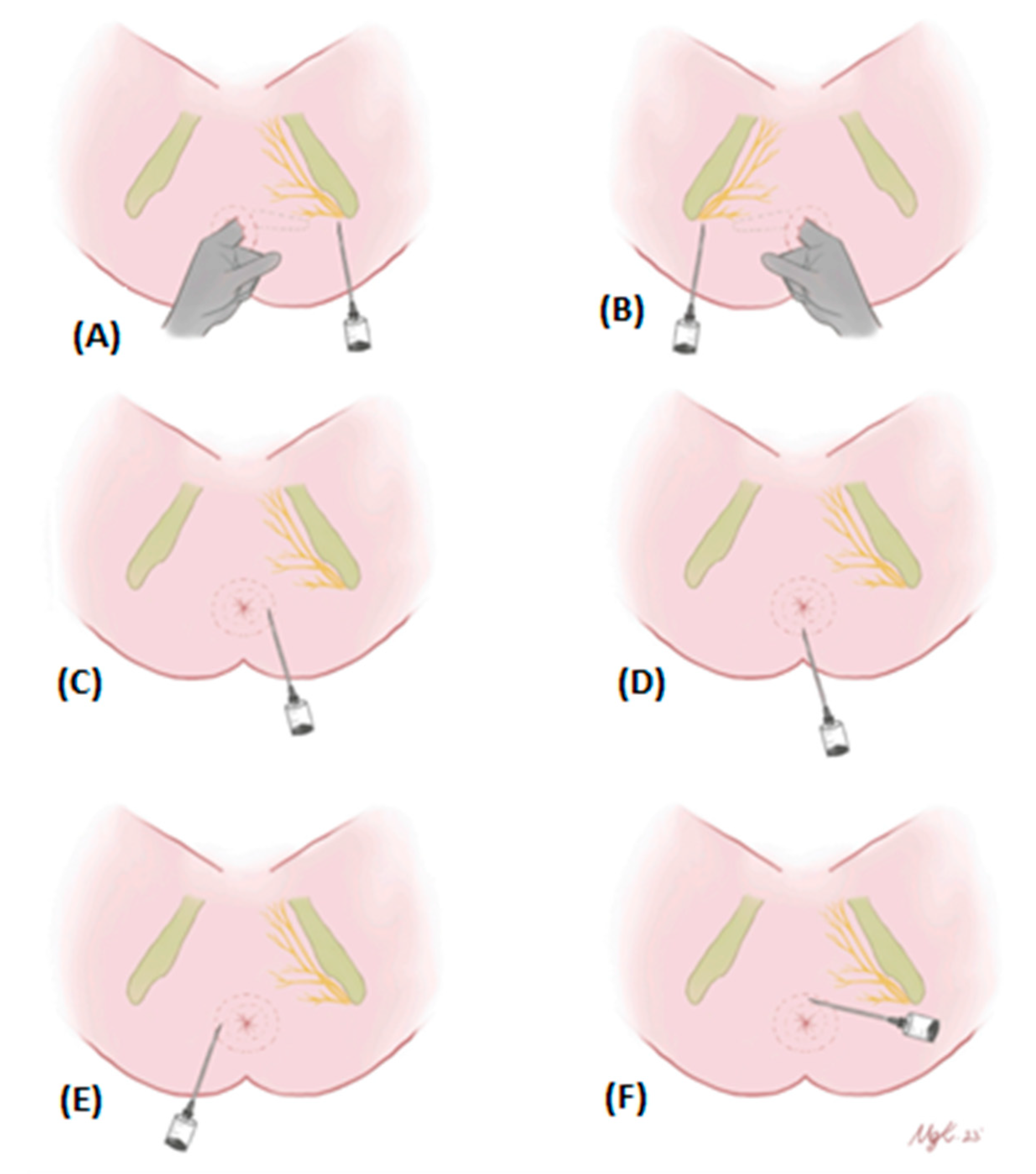
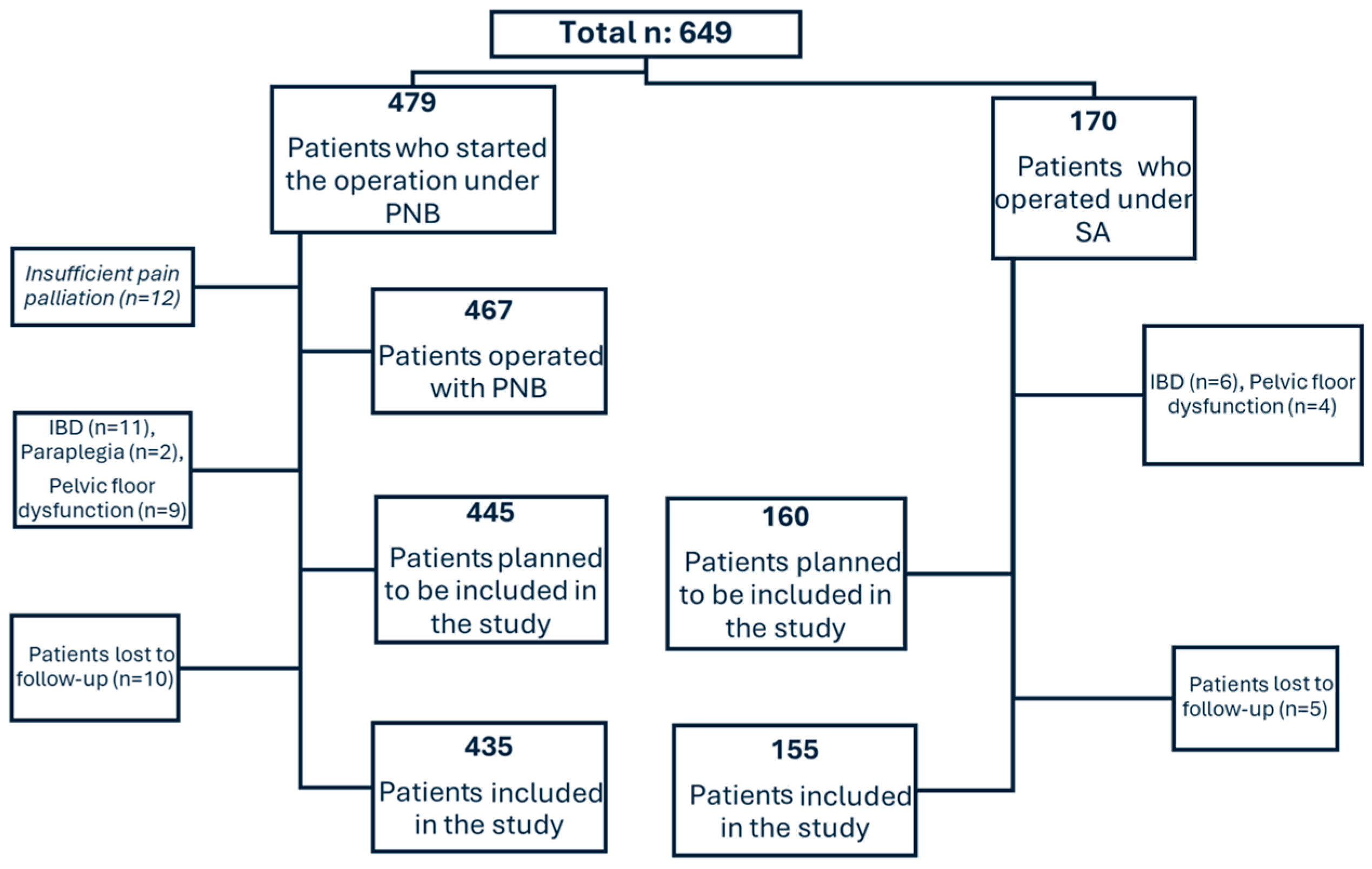
2. Materials and Methods
2.1. Study Design
2.2. Patient Selection Criteria
2.3. Variables and Definitions
2.4. Study Setting
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Postoperative Pain Outcomes
3.3. Postoperative Functional Outcomes
3.4. Early Complications, Surgery Duration, and Hospital Stay
4. Discussion
4.1. Pain Management
4.2. Functional Outcomes
4.3. Complications
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vander Mijnsbrugge, G.; Molenaar, C.; Buyl, R.; Westert, G.; van der Wees, P. How is your proctology patient really doing? Outcome measurement in proctology: Development, design and validation study of the Proctoprom. Tech. Coloproctol. 2020, 24, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Abdi, S.; Shenouda, P.; Patel, N.; Saini, B.; Bharat, Y.; Calvillo, O. A novel technique for pudendal nerve block. Pain Physician 2004, 7, 319. [Google Scholar] [CrossRef] [PubMed]
- Bonatti, L.; Soncini, S.; Bellocchia, A.B.; Selivanov, D.; Cestino, L.; Festa, F.; Natta, F.; Quaglino, F. Pudendal nerve block: A safe, simple and effective approach in surgical proctological patients. Minerva Surg. 2021, 77, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Elbetti, C.; Caminati, F.; Giani, I.; Feroci, F.; Zalla, T.; Calussi, M.; Dreoni, P.; Talamo, G. Tailored anal block (TAB): A new anesthesia procedure for surgical treatment of hemorrhoids in an outpatient setting. Tech. Coloproctol. 2019, 23, 497–500. [Google Scholar] [CrossRef]
- Falco, N.; Tutino, R.; Fontana, T.; Gullo, R.; Licari, L.; Raspanti, C.; De Marco, P.; Colli, F.; Venturelli, P.; Salamone, G. Outpatient management of proctologic disease. Which techniques for local anesthesia? The experience of a single center. Il G. Di Chir.-J. Ital. Surg. Assoc. 2019, 40, 182–187. [Google Scholar]
- Myles, P.S.; Troedel, S.; Boquest, M.; Reeves, M. The pain visual analog scale: Is it linear or nonlinear? Anesth. Analg. 1999, 89, 1517. [Google Scholar] [CrossRef]
- Üstün, T.B.; Kostanjsek, N.; Chatterji, S.; Rehm, J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Mongelli, F.; Treglia, G.; La Regina, D.; Di Giuseppe, M.; Galafassi, J.; Majno-Hurst, P.E.; Christoforidis, D. Pudendal nerve block in hemorrhoid surgery: A systematic review and meta-analysis. Dis. Colon Rectum 2021, 64, 617–631. [Google Scholar] [CrossRef]
- Van Backer, J.T.; Jordan, M.R.; Leahy, D.T.; Moore, J.S.; Callas, P.; Dominick, T.; Cataldo, P.A. Preemptive analgesia decreases pain following anorectal surgery: A prospective, randomized, double-blinded, placebo-controlled trial. Dis. Colon Rectum 2018, 61, 824–829. [Google Scholar] [CrossRef]
- Janković, R.; Stošić, M. Specific aspects OF anesthesia IN proctology. Facta Univ. Ser. Med. Biol. 2019, 21, 21–24. [Google Scholar] [CrossRef]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
- Rotigliano, N.; Füglistaler, I.; Guenin, M.; Dursunoglu, G.; Freiermuth, D.; Von Flüe, M.; Steinemann, D. Perianal block with ropivacaine as a supplement to anaesthesia in proctological surgery: Double-blind randomized placebo-controlled trial (PERCEPT). J. Br. Surg. 2020, 107, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Tepetes, K.; Symeonidis, D.; Christodoulidis, G.; Spyridakis, M.; Hatzitheofilou, K. Pudendal nerve block versus local anesthesia for harmonic scalpel hemorrhoidectomy: A prospective randomized study. Tech. Coloproctology 2010, 14, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, M.; Saporito, A.; La Regina, D.; Tasciotti, E.; Ghielmini, E.; Vannelli, A.; Pini, R.; Mongelli, F. Ultrasound-guided pudendal nerve block in patients undergoing open hemorrhoidectomy: A double-blind randomized controlled trial. Int. J. Color. Dis. 2020, 35, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Steen, C.J.; Lam, D.; Chandra, R.; Chua, J.Y.; An, V.; Keck, J.O. Pudendal nerve block for posthemorrhoidectomy pain: A prospective, single-blinded randomized control trial. Dis. Colon Rectum 2022, 65, 546–551. [Google Scholar] [CrossRef]
- Sammour, T.; Barazanchi, A.W.H.; Hill, A.G.; on behalf of the PROSPECT group (Collaborators). Evidence-based management of pain after excisional haemorrhoidectomy surgery: A PROSPECT review update. World J. Surg. 2017, 41, 603–614. [Google Scholar] [CrossRef]
- Imbelloni, L.E.; Vieira, E.M.; Carneiro, A.F. Postoperative analgesia for hemorrhoidectomy with bilateral pudendal blockade on an ambulatory patient: A controlled clinical study. J. Coloproctology 2012, 32, 291–296. [Google Scholar] [CrossRef]
- Aldabbas, R.; Kreshan, M. Comparison between anesthetic approaches with Pudendal nerve block on postoperative pain profile after anorectal surgery: Our experience at King Hussein medical center. J. R. Med. Serv. 2014, 21, 13–20. [Google Scholar] [CrossRef]
- Alkhaldi, H.M.; Salaita, W.M.; Shabaneh, M.A.; Al-Horut, M.I.; Aldabbas, R.M.A.A.; Uraiqat, A.A. Postoperative outcome comparison between pudendal nerve block and caudal block after lateral open internal sphincterotomy. Med. Arch. 2015, 69, 187. [Google Scholar] [CrossRef]
- Poskus, T.; Jakubauskas, M.; Čekas, K.; Jakubauskiene, L.; Strupas, K.; Samalavičius, N.E. Local perianal anesthetic infiltration is safe and effective for anorectal surgery. Front. Surg. 2021, 8, 730261. [Google Scholar] [CrossRef]
- Waldum, Å.H.; Staff, A.C.; Lukasse, M.; Falk, R.S.; Sørbye, I.K.; Jacobsen, A.F. Intrapartum pudendal nerve block analgesia and risk of postpartum urinary retention: A cohort study. Int. Urogynecol. J. 2021, 32, 2383–2391. [Google Scholar] [CrossRef]
- Nemati Honar, B.; Mirkheshti, A.; Mahdinezhad, A.; Memary, E. Pain Management Following Anorectal Surgery Using PatientControlled Analgesia vs. Pudendal Nerve Block: A Clinical Trial. Trauma Mon. 2018, 23, e15180. [Google Scholar]
- Slopnick, E.A.; Sears, S.B.; Chapman, G.C.; Sheyn, D.D.; Abrams, M.K.; Roberts, K.M.; Pollard, R.; Mangel, J. Pudendal nerve block analgesia at the time of vaginal surgery: A randomized, double-blinded, sham-controlled trial. Urogynecology 2023, 29, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Yasrab, M.; Naqvi, S.E.H.; Ahmed, F.; Ahmed, M.; Rana, S.; Khushdil, A. Preventing Catheter Related Bladder Discomfort (CRBD) in male patients undergoing Lower Urinary tract surgery with Bilateral Pudendal Nerve Block: A Randomized Controlled Trial. Pak. Armed Forces Med. J. 2022, 72, 389–393. [Google Scholar] [CrossRef]
| PNB | SA | |
|---|---|---|
| Preoperative Period | ||
| Admission | Day Surgery | Inpatient Admission |
| Enema | None | None |
| Fasting | None | 6 h Before Surgery |
| Intraoperative Period | ||
| Position | Lithotomy | Lithotomy |
| Type of Anesthesia | Isolated Pudendal Block | Standard Spinal Anesthesia |
| Surgical Procedure |
|
|
| Surgeon | Same | Same |
| Postoperative Period | ||
| Postoperative follow up | Recovery Room | Inpatient Ward |
| Oral Intake | Immediately | Postoperative 4th Hour |
| Diagnosis | PNB (n: 435) | SA (n: 155) | Operation | PNB | SA | Total (n: 590) |
|---|---|---|---|---|---|---|
| Hemorrhoidal Disease (%) | 175 (72.6) | 66 (27.4) | Hemorrhoidectomy (%) | 25 (50) | 25 (50) | 50 |
| LHP (%) | 133 (78.7) | 36 (21.3) | 169 | |||
| Hemorrhoidopexy (%) | 5 (62.5) | 3 (37.5) | 8 | |||
| Thrombectomy (%) | 12 (85.7) | 2 (14.3) | 14 | |||
| Anal fistula (%) | 197 (77) | 59 (23) | Fistulotomy (%) | 115 (78.2) | 32 (21.8) | 147 |
| Seton (%) | 76 (75.2) | 25 (24.8) | 101 | |||
| LAFT (%) | 6 (75) | 2 (25) | 8 | |||
| Anal fissure (%) | 28 (66.7) | 14 (33.3) | LIS (%) | 28 (66.7) | 14 (33.3) | 42 |
| Anal wart (%) | 5 (55.6) | 4 (44.4) | Excision cauterization (%) | 5 (55.6) | 4 (44.4) | 9 |
| Anal abscess (%) | 30 (71.4) | 12 (28.6) | Abscess drainage (%) | 30 (71.4) | 12 (28.6) | 42 |
| Follow-up period/month (iqr) | 16 (10–23) | 14 (8–25) | 16 (9–23) |
| PNB (iqr) | Intragroup pf | SA (iqr) | Intragroup pf | p† | ||
|---|---|---|---|---|---|---|
| HD | Hemorrhoidectomy | V0 = 4 (2–5) | V0-V1 > 0.999 | V0 = 4 (3–6) | V0-V1 = 0.472 | 0.317 |
| npnb: 25, nsa: 25 | V1 = 3 (2–5) | V0-V2 < 0.001 | V1 = 5 (4–7) | V0-V2 < 0.001 | <0.001 | |
| V2 = 1 (1–2) | V1-V2 = 0.003 | V2 = 2 (1–3) | V1-V2 < 0.001 | 0.023 | ||
| LHP | V0 = 5 (6–2.5) | V0-V1 < 0.001 | V0 = 6 (3–7) | V0-V1 > 0.999 | 0.396 | |
| npnb: 133, nsa: 36 | V1 = 3 (1–4) | V0-V2 < 0.001 | V1 = 5 (4–6) | V0-V2 = 0.033 | 0.002 | |
| V2 = 2 (1–3) | V1-V2 = 0.023 | V2 = 1 (0–1) | V1-V2 = 0.069 | 0.010 | ||
| Hemorrhoidopexy | V0 = 4 (3–7) | pf = 0.50 | V0 = 3 (3–4) | pf = 0.086 | >0.999 | |
| npnb: 5, nsa: 3 | V1 = 2 (1–3) | V1 = 3 (3–4) | 0.071 | |||
| V2 = 3 (1–3) | V2 = 1 (1–2) | 0.786 | ||||
| Thrombectomy | V0 = 3.5 (2–5) | pf = 0.192 | V0 = 6 (5–7.5) | pf = 0.135 | 0.198 | |
| npnb: 12, nsa: 2 | V1 = 3 (2–4) | V1 = 4 (4–5) | 0.132 | |||
| V2 = 2 (1.25–3) | V2 = 1 (1–1.5) | 0.440 | ||||
| FIA | Fistulotomy | V0 = 5 (1–6) | V0-V1 = 0.005 | V0 = 5 (1.5–6) | V0-V1 < 0.001 | 0.531 |
| npnb: 115, nsa: 32 | V1 = 6 (5–7) | V0-V2 < 0.001 | V1 = 7 (6.25–9) | V0-V2 = 0.031 | <0.001 | |
| V2 = 1 (1–2) | V1-V2 < 0.001 | V2 = 2 (1–2) | V1-V2 < 0.001 | 0.090 | ||
| Seton | V0 = 5 (1–6) | V0-V1 = 0.056 | V0 = 5 (1–6) | V0-V1 > 0.999 | 0.753 | |
| npnb: 76, nsa: 25 | V1 = 2 (2–3) | V0-V2 < 0.001 | V1 = 4 (4–5) | V0-V2 < 0.001 | <0.001 | |
| V2 = 1 (1–2.75) | V1-V2 = 0.002 | V2 = 2 (1–3) | V1-V2 = 0.001 | 0.067 | ||
| LAFT | V0 = 3 (0.75–5.75) | pf = 0.405 | V0 = 2 (2–5) | pf = 0.223 | 0.429 | |
| npnb: 6, nsa: 2 | V1 = 2 (1–3.75) | V1 = 4 (4–4) | 0.286 | |||
| V2 = 2 (0.75–2.5) | V2 = 1 (1–1.5) | 0.857 | ||||
| AF | LIS | V0 = 4 (4–7) | V0-V1 > 0.999 | V0 = 4 (3.75–7) | V0-V1 > 0.999 | 0.955 |
| npnb: 28, nsa: 14 | V1 = 4.5 (4–6.75) | V0-V2 < 0.001 | V1 = 6 (4.75–8.25) | V0-V2 = 0.014 | 0.045 | |
| V2 = 1 (1–2) | V1-V2 < 0.001 | V2 = 1 (1–2) | V1-V2 = 0.001 | 0.966 | ||
| AW | Excision cauterization | V0 = 5 (2.5–7.5) | V0-V1 = 0.618 | V0 = 3 (1.25–4.75) | V0-V1 = 0.102 | 0.315 |
| npnb: 5 nsa: 4 | V1 = 7 (5.5–7.5) | V0-V2 = 0.618 | V1 = 8.5 (7.25–9) | V0-V2 > 0.999 | 0.059 | |
| V2 = 3 (1–4.5) | V1-V2 = 0.034 | V2 = 3 (1.25–4) | V1-V2 = 0.102 | >0.999 | ||
| PA | Abscess drainage | V0 = 7 (6–8) | V0-V1 = 0.002 | V0 = 6 (5.25–8) | V0-V1 > 0.999 | 0.314 |
| npnb: 30, nsa: 12 | V1 = 4 (3–6) | V0-V2 < 0.001 | V1 = 6 (5.25–7.75) | V0-V2 = 0.002 | <0.001 | |
| V2 = 1.5 (1–2.25) | V1-V2 = 0.005 | V2 = 2 (2–3) | V1-V2 < 0.001 | 0.129 |
| PNB (iqr) | Intragroup p§ | SA (iqr) | Intragroup p§ | p† | ||||
|---|---|---|---|---|---|---|---|---|
| HH | Hemorrhoidectomy | D0 | 10.3 (5.4–21.8) | <0.001 | D0 | 12.6 (5.4–28.8) | 0.009 | 0.415 |
| npnb: 25, nsa: 25 | D1 | 5.1 (2.6–14.6) | D1 | 13 (7.4–16.8) | 0.009 | |||
| LHP | D0 | 11 (5–27.9) | <0.001 | D0 | 6.9 (2.9–31.3) | 0.413 | 0.403 | |
| npnb: 133, nsa: 36 | D1 | 6 (2.4–14.4) | D1 | 10.2 (9.3–22.7) | 0.093 | |||
| Hemorrhoidopexy | D0 | 11 (4.9–30.5) | 0.043 | D0 | 5.8 (4.1–20) | 0.109 | 0.571 | |
| npnb: 5, nsa: 3 | D1 | 9.8 (3.1–18.8) | D1 | 8.1 (6.3–21.9) | 0.786 | |||
| Thrombectomy | D0 | 14.6 (3.7–39.7) | 0.004 | D0 | 21.3–33.4 | 0.180 | 0.440 | |
| npnb: 12, nsa: 2 | D1 | 7.5 (1.4–17.3) | D1 | 14.6–16.8 | 0.352 | |||
| FIA | Fistulotomy | D0 | 13.5 (1.9–37.2) | <0.001 | D0 | 15.6 (3.6–38.5) | 0.018 | 0.400 |
| npnb: 115, nsa: 32 | D1 | 9.3 (1.9–19.9) | D1 | 13.8 (4.2–23.6) | 0.047 | |||
| Seton | D0 | 11.1 (4.3–25.6) | <0.001 | D0 | 15.6 (3.3–43.8) | 0.045 | 0.549 | |
| npnb: 76, nsa: 25 | D1 | 5.7 (2.5–18.8) | D1 | 10.6 (5.5–27.2) | 0.029 | |||
| LAFT | D0 | 6.6 (5.1–26.2) | 0.043 | D0 | 5.8–32.8 | 0.655 | >0.999 | |
| npnb: 6, nsa: 2 | D1 | 3.1 (2.7–9.1) | D1 | 6.9–18.4 | 0.143 | |||
| AF | LIS | D0 | 20.8 (20.8–32.8) | <0.001 | D0 | 21.1 (20.8–32.9) | 0.048 | 0.589 |
| npnb: 28, nsa: 14 | D1 | 18.5 (14.7–21.8) | D1 | 23.3 (19.7–25.7) | 0.012 | |||
| AS | Excision cauterization | D0 | 20.8 (10.4–30.7) | 0.080 | D0 | 19.9 (17.9–22.9) | 0.465 | 0.905 |
| npnb: 5 nsa: 4 | D1 | 17.7 (5.5–24.5) | D1 | 16.3 (8.8–23.4) | 0.730 | |||
| Bleeding | Urinary Retention | SSI | FI (Temporary or Permanent) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PNB | SA | p | PNB | SA | p | PNB | SA | p | PNB | SA | p | |
| Hemorrhoidectomy (%) | 3 (12) | 4 (16) | >0.999 | 0 (0) | 2 (8) | 0.490 | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| npnb: 25, nsa: 25 | ||||||||||||
| LHP (%) | 2 (1.5) | 1 (2.8) | 0.515 | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| npnb: 133, nsa: 36 | ||||||||||||
| Hemorrhoidopexy (%) | 0 (0) | 0 (0) | - | 0 (0) | 2 (66.7) | 0.107 | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| npnb: 5, nsa: 3 | ||||||||||||
| Thrombectomy (%) | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| npnb: 12, nsa: 2 | ||||||||||||
| Fistulotomy (%) | 5 (4.3) | 2 (6.3) | 0.646 | 1 (0.9) | 3 (9.4) | 0.032 | 2 (1.7) | 2 (6.3) | 0.207 | 4 (3.5) | 2 (6.3) | 0.611 |
| npnb: 115, nsa: 32 | ||||||||||||
| Seton (%) | 1 (1.3) | 1 (4) | 0.436 | 0 (0) | 3 (12) | 0.014 | 2 (2.6) | 2 (8) | 0.255 | 0 (0) | 0 (0) | - |
| npnb: 76, nsa: 25 | ||||||||||||
| LAFT (%) | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - | 0 (0) | 0 (0) | - |
| npnb: 6, nsa: 2 | ||||||||||||
| LIS (%) | 2 (7.1) | 1 (7.1) | >0.999 | 0 (0) | 2 (14.3) | 0.106 | 1 (3.6) | 1 (7.1) | >0.999 | 0 (0) | 1 (7.1) | 0.333 |
| npnb: 28, nsa: 14 | ||||||||||||
| Excision cauterization (%) | 0 (0) | 1 (25) | 0.444 | 0 (0) | 0 (0) | - | 1 (20) | 1 (25) | >0.999 | 0 (0) | 0 (0) | - |
| npnb: 5 nsa: 4 | ||||||||||||
| abscess drainage (%) | 1 (3.3) | 1 (8.3) | 0.495 | 1 (3.3) | 2 (16.7) | 0.192 | 1 (3.3) | 1 (8.3) | 0.495 | 0 (0) | 0 (0) | - |
| Total (%) | 14 (3.2) | 11 (7.1) | 0.050 | 2 (0.5) | 14 (9) | <0.001 | 7 (1.6) | 7 (4.5) | 0.060 | 4 (0.9) | 3 (1.9) | 0.387 |
| Pudental (±SD) | Spinal (±SD) | p § | ||
|---|---|---|---|---|
| Hemorrhoidectomy | OD/min | 27.8 (5.2) | 40.64 (6.1) | <0.001 |
| HD/h | 1.7 (0.8) | 29.4 (8.9) | <0.001 | |
| LHP | OD/min | 22.9 (4.9) | 42.3 (8) | <0.001 |
| HD/h | 1.4 (0.6) | 28.6 (9.3) | <0.001 | |
| LIS | OD/min | 15.6 (1.8) | 30.7 (1.9) | <0.001 |
| HD/h | 1.6 (0.8) | 27.2 (6.5) | <0.001 | |
| Seton | OD/min | 24.6 (5.9) | 41.2 (7.4) | <0.001 |
| HD/h | 1.6 (0.8) | 27.7 (5.2) | <0.001 | |
| Fistulotomy | OD/min | 19.8 (5.31) | 36.3 (4.6) | <0.001 |
| HD/h | 1.6 (0.8) | 27.6 (5.1) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şahin, S.; Yazkan, C.; Dere, Ö.; Kayılıoğlu, I.; Özcan, Ö. Comparison of Pudendal Nerve Block and Spinal Anesthesia in Proctological Surgeries: Efficacy, Safety, and Patient Outcomes. Medicina 2024, 60, 1651. https://doi.org/10.3390/medicina60101651
Şahin S, Yazkan C, Dere Ö, Kayılıoğlu I, Özcan Ö. Comparison of Pudendal Nerve Block and Spinal Anesthesia in Proctological Surgeries: Efficacy, Safety, and Patient Outcomes. Medicina. 2024; 60(10):1651. https://doi.org/10.3390/medicina60101651
Chicago/Turabian StyleŞahin, Samet, Cenk Yazkan, Özcan Dere, Ilgaz Kayılıoğlu, and Önder Özcan. 2024. "Comparison of Pudendal Nerve Block and Spinal Anesthesia in Proctological Surgeries: Efficacy, Safety, and Patient Outcomes" Medicina 60, no. 10: 1651. https://doi.org/10.3390/medicina60101651
APA StyleŞahin, S., Yazkan, C., Dere, Ö., Kayılıoğlu, I., & Özcan, Ö. (2024). Comparison of Pudendal Nerve Block and Spinal Anesthesia in Proctological Surgeries: Efficacy, Safety, and Patient Outcomes. Medicina, 60(10), 1651. https://doi.org/10.3390/medicina60101651






