Current Developments in the Management of Amblyopia with the Use of Perceptual Learning Techniques
Abstract
:1. Introduction
1.1. Background
1.2. Pathogenesis
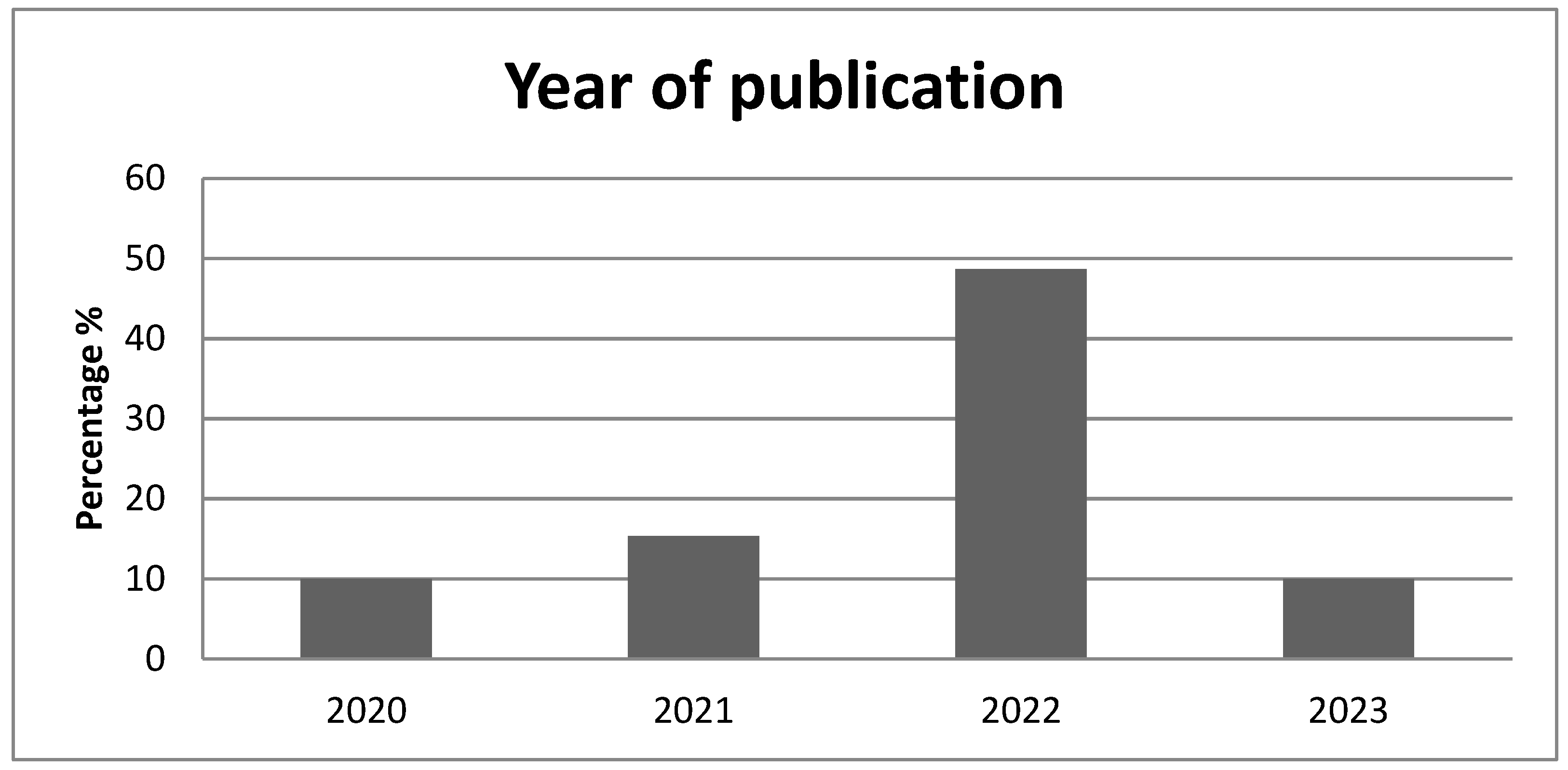
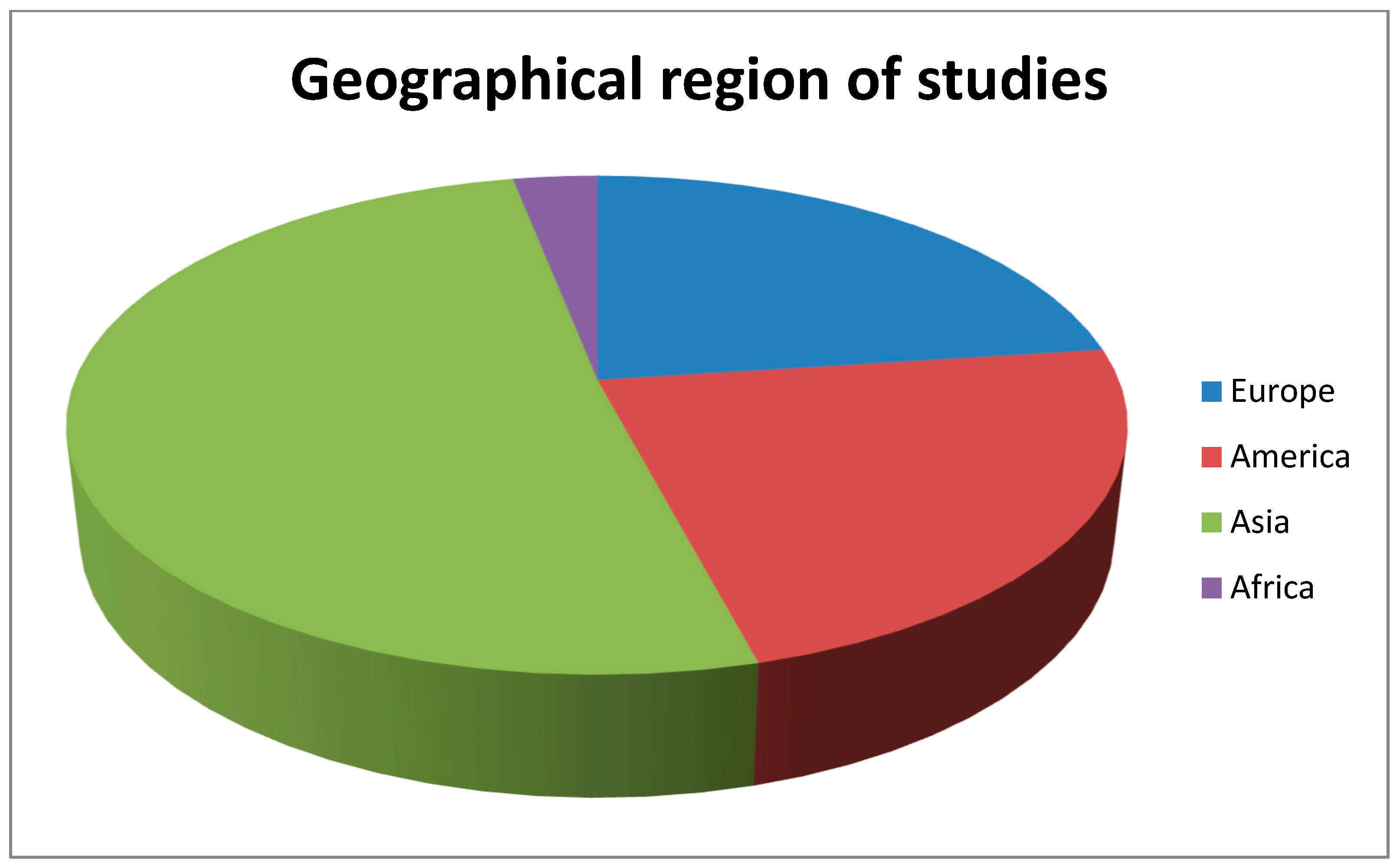
2. Materials and Methods
2.1. Objective
2.2. Eligibility Criteria
- Inclusion criteria:
- -
- Studies published in English;
- -
- Only studies performed in humans;
- -
- All types of amblyopia.
- Exclusion criteria:
- -
- Studies previous to the year 2020;
- -
- Articles not referring to perceptual learning as a treatment for amblyopia;
- -
- Review articles.
3. Results
3.1. Binocular Approaches
3.1.1. Monocular Perceptual Learning
3.1.2. Binocular Perceptual Learning
- -
- -
- -
- Partial presentation: Different elements of a visual scene are presented in each eye (as complementary parts of a puzzle), and the whole image can be perceived through binocular fusion [24].
- Interactive video games;
- Virtual reality/augmented reality;
- Passive dichoptic movie/video viewing;
- Vision therapy;
- *Transcranial electric stimulation (t-ES).
Interactive Video Games
- -
- Occlu-tab (or Occlu-pad): Occlutab (Yaguchi Electric Co., Ltd., Ishinomaki, Japan) (or Occlupad as it was alternatively named in a few countries) is a modified i-Pad tablet device with the addition of a linear polarization filter on the display resulting in a “white screen” appearance to the naked eye. Patients use the device to play various video games while wearing specially designed polarizing glasses, which make the game elements visible only to the amblyopic eye while the fellow eye can see a white screen. The glasses have circular polarization filters so that the amblyopic eye can still see the image displayed, even if patients rotate the tablet or tilt their heads [33]. The game tasks require the use of a palm-sized tangible block (like a touch mouse), promoting simultaneous training of eye-hand coordination skills [33]. Two randomized control studies (RCTs), with more than 200 amblyopic children in total, have compared the effectiveness of this videogame treatment in combination with refractive correction versus either corrective spectacles alone or eye patching, respectively [33,42]. Both yielded a significantly greater improvement in VA in the game group [33,42]. One study included children 4 to 6 years old, while the other included patients within and beyond the critical period (up to 12 years old).
- -
- i-Pod: Another RCT investigated the treatment effect of a modified “Tetris” falling blocks game loaded on an i-Pod touch device in older patients (>7 years old, including adults) [39]. Selective-dichoptic presentation of the game elements was achieved by depicting the falling blocks with different colors from the bottom-lying blocks and with the use of red-green filter glasses in the study group. The training sessions began with the presentation of stimuli in maximum contrast to the amblyopic eye and reduced contrast to the sound eye in order to overcome interocular suppression. During the training course, the contrast for the fellow eye gradually increased. Results showed a significant improvement in VA in the study group, with additional improvement in stereoacuity [39]. Similar results have been reported in a case–control study with adult participants playing a dichoptic Tetris game on a stock i-Pad tablet device [34].
- -
- Online PL platforms: Other treatment protocols consist of network-based training platforms, where patients perform online PL tasks from their home computer, and the training data and progression rates are stored online and could be remotely monitored by the clinician [28,45]. These platforms include appropriate algorithms to generate tailor-made training plans according to each patient’s age, refraction, baseline VA and stereoacuity, and adjust the plan according to their progress [28,65]. The patients wear filter glasses during the sessions while the software is presenting 3D images or random-dot anaglyphic stimuli intended to stimulate stereoscopic perception [28,45]. These perceptual games were proven effective in children aging within and beyond the critical period, resulting in VA and stereoacuity improvement, with stable results throughout a 6 month follow-up [28,45].
Virtual Reality/Augmented Reality
Passive Dichoptic Movie/Video Viewing
Vision Therapy
Transcranial Electric Stimulation (tES)
3.2. Predictive Factors for Perceptual Learning Treatment Outcome
3.3. Advantages and Disadvantages of Perceptual Learning Treatment
3.3.1. Advantages
- -
- Addresses multiple amblyopia impairments: A great number of studies support that the various PL treatments are effective in improving VA of the amblyopic eye, with superior, or at least equal results compared to patching [27,37,40,54,57,58,61,67]. Furthermore, the PL approaches have a definite advantage in restoring other visual deficits, like stereoacuity, CS, and crowding effect, as well as visuomotor deficits, while patching has no impact on them [13,27,28,31,34,37,40,44,46,49,54,57,59,61].
- -
- More entertaining: Playing video games is definitely more appealing and pleasant for young patients than wearing an eye patch [13]. By incorporating game principles (scenario- storyline, targets and enemies, levels of increasing difficulty with goals and rewards), therapy becomes more intriguing [28]. Similarly, watching animated movies in 3D mode is more exciting than watching 2-dimensionally with one eye also covered.
- -
- No social stigma: Many patients wearing a visible-to-others eye patch or foggy spectacle report low self-esteem, depression, frustration, feelings of isolation, and poor social acceptance [13]. This burden is often the reason for poor compliance in the occlusion treatment [13]. On the other hand, children attending PL activities do not experience similar psychological stress.
- -
- -
- Faster treatment effects: Many studies have pointed out that PL programs generate equivalent visual outcomes in a shorter time (at least 5-fold faster) compared to patching [13,27,30,34,47,50,58,61]. Thus, this improves adherence and brings optimal results [49,52]. Additionally, when PL is combined with electric brain stimulation, the improvement rate is even greater, reducing the number of sessions required to achieve therapeutic results [66].
- -
- Sustainable effects: Studies report stable results for PL treatments, lasting long after treatment cessation [13,23,51], even 6 months later [45]. A recent prospective cohort study assessed the risk of recurrence after contrast-rebalanced dichoptic treatment in 100 effectively treated children and reported a 28% regression risk up to 3 years follow-up [68]. The secondary analysis found a similar recurrence risk to the successfully treated children with patching or atropine at 12 months (24%) [68]. Further long-term follow-up studies are needed, though, to verify these preliminary results.
- -
- Beneficial for children, adults, and cases resistant to occlusion: PL has shown favorable results in children within and above the critical period, as well as in adults, where patching is not effective [33,51,61]. Furthermore, PL seems to offer some benefit to patients who were unresponsive to occlusion [30,37].
- -
- Low adverse effects rates: Reported potential adverse effects of dichoptic therapy are diplopia (double vision)-usually transient, eye strain, reverse amblyopia (worsening of VA in the previously better-seeing eye), manifestation or worsening of pre-existing strabismus, drowsiness, and headache [29,36,52]. Persistent diplopia is quite rare, while transient diplopia is reported in approximately 15% of treated cases [29]. Strabismus patients are prone to develop diplopia as a result of interocular suppression rebalance [29]. Especially those beginning treatment at an age above the critical period or adults with a history of strabismus surgery in childhood are at higher risk for intractable diplopia [29]. Other studies recorded no side effects to their participants [36,52].
3.3.2. Disadvantages
- -
- PL is more complex and costly: While occlusion treatment requires a simple and cheap eye patch, PL therapies are mainly delivered through sophisticated and expensive electronic equipment, like computers, tablets, game consoles, or even VR goggles, and they often require an internet connection [13,27,39,47]. Furthermore, there is a considerable cost for the development and modification of games or training software [47]. We have already discussed a certain approach that enables plain household screens for dichoptic PL presentation with the use of polarizing films [41].
- -
- Additionally, while most PL programs are home-based, there are several others that are designed to be conducted in an office setting [27,47]. This involves additional costs for transportation from and to the clinic, absence of work hours for parents, as well as payment for the personnel supervising the training sessions [47].
- -
- PL interactive video games are inappropriate for younger children: Patients under 5.5 years old lack the cognitive maturity to comprehend game tasks and settings, and lengthy sessions could be too tedious for them [13,47]. Therefore, this type of treatment is not suitable for preschool children that require immediate intervention. On the contrary, passive movie viewing could be effectively applied to these patients, as they do not require understanding and interaction.
3.4. Compliance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Webber, A.L.; Wood, J. Amblyopia: Prevalence, natural history, functional effects and treatment. Clin. Exp. Optom. 2005, 88, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Birch, E.E. Amblyopia and binocular vision. Prog. Retin. Eye Res. 2013, 33, 67–84. [Google Scholar] [CrossRef] [PubMed]
- Bhutada, I.; Skelly, P.; Jacobs, J.; Murray, J.; Shaikh, A.G.; Ghasia, F.F. Reading difficulties in amblyopia: Consequence of visual sensory and oculomotor dysfunction. J. Neurol. Sci. 2022, 442, 120438. [Google Scholar] [CrossRef] [PubMed]
- Mostafaie, A.; Ghojazadeh, M.; Hosseinifard, H.; Manaflouyan, H.; Farhadi, F.; Taheri, N.; Pashazadeh, F. A systematic review of Amblyopia prevalence among the children of the world. Rom. J. Ophthalmol. 2020, 64, 342–355. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Wang, W.; Li, J.; Wang, Y.; Hu, X.; Feng, L.; Ye, Q.; Luo, Y.; Zhu, Z.; Li, J.; et al. Effects of Perceptual Learning on Deprivation Amblyopia in Children with Limbal Dermoid: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 1879. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, B.; Stacy, R.C.; Kruger, J.; Cestari, D.M. Deprivation amblyopia and congenital hereditary cataract. Semin. Ophthalmol. 2013, 28, 321–326. [Google Scholar] [CrossRef]
- Brin, T.A.; Chow, A.; Carter, C.; Oremus, M.; Bobier, W.; Thompson, B. Efficacy of vision-based treatments for children and teens with amblyopia: A systematic review and meta-analysis of randomised controlled trials. BMJ Open Ophthalmol. 2021, 6, e000657. [Google Scholar] [CrossRef]
- Birch, E.E.; Holmes, J.M. The clinical profile of amblyopia in children younger than 3 years of age. J. AAPOS 2010, 14, 494–497. [Google Scholar] [CrossRef]
- Pediatric Eye Disease Investigator Group. The clinical profile of moderate amblyopia in children younger than 7 years. Arch. Ophthalmol. 2002, 120, 281–287. [Google Scholar] [CrossRef]
- Kelly, K.R.; Hunter, J., Jr.; Norouzi, D.M.; Jost, R.M.; White, A.J.; Cheng-Patel, C.S.; Beauchamp, C.L.; Dao, L.M.; Luu, B.A.; Stager, D.; et al. Reach Kinematics During Binocular Viewing in 7- to 12-Year-Old Children With Strabismus. Investig. Ophthalmol. Vis. Sci. 2021, 62, 21. [Google Scholar] [CrossRef]
- Kiorpes, L.; Daw, N. Cortical correlates of amblyopia. Vis. Neurosci. 2018, 35, E016. [Google Scholar] [CrossRef] [PubMed]
- Godinez, A.; Martín-González, S.; Ibarrondo, O.; Levi, D.M. Scaffolding depth cues and perceptual learning in VR to train stereovision: A proof of concept pilot study. Sci. Rep. 2021, 11, 10129. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.F. Reasons why we might want to question the use of patching to treat amblyopia as well as the reliance on visual acuity as the primary outcome measure. BMJ Open Ophthalmol. 2022, 7, e000914. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.F.; Thompson, B.; Baker, D.H. Binocular vision in amblyopia: Structure, suppression and plasticity. Ophthalmic. Physiol. Opt. 2014, 34, 146–162. [Google Scholar] [CrossRef] [PubMed]
- Hensch, T.K.; Quinlan, E.M. Critical periods in amblyopia. Vis. Neurosci. 2018, 35, E014, Erratum in Vis. Neurosci. 2018, 35, E024. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.; Concetta Morrone, M.; Bex, P.; Lozama, A.; Sabel, B.A. Harnessing brain plasticity to improve binocular vision in amblyopia: An evidence-based update. Eur. J. Ophthalmol. 2023. [Google Scholar] [CrossRef]
- Zhu, B.; Liao, M.; Liu, L. Measuring the impact of suppression on visual acuity in children with amblyopia using a dichoptic visual acuity chart. Front. Neurosci. 2022, 16, 860620. [Google Scholar] [CrossRef]
- Chow, A.; Silva, A.E.; Tsang, K.; Ng, G.; Ho, C.; Thompson, B. Binocular Integration of Perceptually Suppressed Visual Information in Amblyopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 11. [Google Scholar] [CrossRef]
- Li, J.; Thompson, B.; Lam, C.S.; Deng, D.; Chan, L.Y.; Maehara, G.; Woo, G.C.; Yu, M.; Hess, R.F. The role of suppression in amblyopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4169–4176. [Google Scholar] [CrossRef]
- Murray, J.; Gupta, P.; Dulaney, C.; Garg, K.; Shaikh, A.G.; Ghasia, F.F. Effect of Viewing Conditions on Fixation Eye Movements and Eye Alignment in Amblyopia. Investig. Ophthalmol. Vis. Sci. 2022, 63, 33. [Google Scholar] [CrossRef]
- Lin, W.; Wei, J.; Wang, W.; Zou, L.; Zhou, S.; Jiang, N.; Reynaud, A.; Zhou, J.; Yu, X.; Hess, R.F. Rapid alternate monocular deprivation does not affect binocular balance and correlation in human adults. eNeuro 2022, 9, ENEURO.0509-21.2022. [Google Scholar] [CrossRef]
- Ghasia, F.; Wang, J. Amblyopia and fixation eye movements. J. Neurol. Sci. 2022, 441, 120373. [Google Scholar] [CrossRef] [PubMed]
- Rodán, A.; Candela Marroquín, E.; Jara García, L.C. An updated review about perceptual learning as a treatment for amblyopia. J. Optom. 2022, 15, 3–34. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.M.; Hunter, D.G.; Gaier, E.D. Emerging therapies for amblyopia. Semin. Ophthalmol. 2021, 36, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Hou, C.; Nicholas, S.C. Perceptual learning with dichoptic attention tasks improves attentional modulation in V1 and IPS and reduces interocular suppression in human amblyopia. Sci. Rep. 2022, 12, 9660, Erratum in Sci. Rep. 2022, 12, 10884. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Liu, L.; Dong, X.; Bao, M. Effects of altered-reality training on interocular disinhibition in amblyopia. Ann. N. Y. Acad. Sci. 2023, 1522, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Leal Vega, L.; Piñero, D.P.; Hernández Rodríguez, C.J.; Martín, A.M.; Morales-Quezada, L.; Álvarez, A.I.V.; Lara, J.F.A.; Martín, M.B.C. Study protocol for a randomized controlled trial of the NEIVATECH virtual reality system to improve visual function in children with anisometropic amblyopia. BMC Ophthalmol. 2022, 22, 253. [Google Scholar] [CrossRef]
- Zheng, C.Y.; Xu, W.; Wu, S.Q.; Han, D.X. A randomized study of network-based perception learning in the treatment of amblyopia children. Int. J. Ophthalmol. 2022, 15, 800–806. [Google Scholar] [CrossRef]
- Dahlmann-Noor, A.H.; Greenwood, J.A.; Skilton, A.; Baker, D.; Ludden, S.; Davis, A.; Dehbi, H.-M.; Dakin, S.C. Phase 2a randomised controlled feasibility trial of a new ‘balanced binocular viewing’ treatment for unilateral amblyopia in children age 3-8 years: Trial protocol. BMJ Open 2022, 12, e051423. [Google Scholar] [CrossRef]
- Huang, Y.T.; Lin, H.J.; Liao, W.L.; Tsai, Y.Y.; Hsieh, Y.C. Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study. Children 2022, 9, 205. [Google Scholar] [CrossRef]
- Hou, C. A novel method for utilizing dichoptic attention tasks in amblyopic training. MethodsX 2022, 9, 101829. [Google Scholar] [CrossRef] [PubMed]
- Milla, M.; Molina-Martín, A.; Piñero, D.P. Long-Term Efficacy of the Combination of Active Vision Therapy and Occlusion in Children with Strabismic and Anisometropic Amblyopia. Children 2022, 9, 1012. [Google Scholar] [CrossRef] [PubMed]
- Handa, T.; Thakkar, H.; Ramakrishnan, M.; Shah, K.; Prajapati, V.; Sayed, S.; Joshi, A.; Ishigaki, Y. Comparison of the effectiveness of amblyopia treatment with eye-patch and binocular Occlu-tab for the same treatment duration. Indian J. Ophthalmol. 2022, 70, 1722–1726. [Google Scholar] [CrossRef] [PubMed]
- Ojiabo, S.N.; Munsamy, A.J. The Effect of Home-Based Dichoptic Therapy on Young Adults with Non-Strabismic Anisometropic Amblyopia on Stereo Acuity. Clin. Optom. 2022, 14, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Tan, F.; Yang, X.; Fan, Y.; Liao, Y. The Study of Short-Term Plastic Visual Perceptual Training Based on Virtual and Augmented Reality Technology in Amblyopia. J. Ophthalmol. 2022, 2022, 2826724. [Google Scholar] [CrossRef] [PubMed]
- Mirmohammadsadeghi, A.; Sadeghi, M.; Kasaee, A.; Akbari, M.R. Anaglyphic Three-Dimensional Movie: A Simple Binocular Method to Treat Anisometropic or Strabismic Amblyopia in Adults. J. Curr. Ophthalmol. 2022, 34, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Rodríguez, C.J.; Fukumitsu, H.; Ruiz-Fortes, P.; Soto-Negro, R.; Merino-Suárez, M.; Piñero, D.P. Efficacy of Perceptual Learning-Based Vision Training as an Adjuvant to Occlusion Therapy in the Management of Amblyopia: A Pilot Study. Vision 2021, 5, 15. [Google Scholar] [CrossRef]
- He, Y.; Feng, L.; Zhou, Y.; Zhuang, Y.; Xu, Z.; Yao, Y.; Chen, X.; Jiang, R.; Yuan, J.; Ye, Q.; et al. Characteristics and predictive factors of visual function improvements after monocular perceptual learning in amblyopia. Heliyon 2023, 9, e17281. [Google Scholar] [CrossRef]
- Pang, P.C.K.; Lam, C.S.Y.; Hess, R.F.; Thompson, B. Effect of dichoptic video game treatment on mild amblyopia—A pilot study. Acta Ophthalmol. 2021, 99, e423–e432. [Google Scholar] [CrossRef]
- Jost, R.M.; Hudgins, L.A.; Dao, L.M.; Stager, D.R.; Luu, B.; Beauchamp, C.L.; Hunter, J.S.; Giridhar, P.; Wang, Y.-Z.; Birch, E.E. Randomized clinical trial of streaming dichoptic movies versus patching for treatment of amblyopia in children aged 3 to 7 years. Sci. Rep. 2022, 12, 4157. [Google Scholar] [CrossRef]
- Iwata, Y.; Handa, T.; Ishikawa, H. Comparison of Amblyopia Treatment Effect with Dichoptic Method Using Polarizing Film and Occlusion Therapy Using an Eye Patch. Children 2022, 9, 1285. [Google Scholar] [CrossRef] [PubMed]
- Manny, R.E.; Holmes, J.M.; Kraker, R.T.; Li, Z.; Waters, A.L.O.; Kelly, K.R.; Kong, L.; Crouch, E.R.; Lorenzana, I.J.O.; Alkharashi, M.S.; et al. A Randomized Trial of Binocular Dig Rush Game Treatment for Amblyopia in Children Aged 4 to 6 Years. Optom. Vis. Sci. 2022, 99, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Maniglia, M.; Velez, F.; Demer, J.L.; Seitz, A.R.; Pineles, S. Short-term Perceptual Learning Game Does Not Improve Patching-Resistant Amblyopia in Older Children. J. Pediatr. Ophthalmol. Strabismus. 2020, 57, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Saxena, R.; Dhiman, R.; Phuljhele, S.; Sharma, P. Comparison of Dichoptic Therapy Versus Occlusion Therapy in Children With Anisometropic Amblyopia: A Prospective Randomized Study. J. Pediatr. Ophthalmol. Strabismus. 2023, 60, 210–217. [Google Scholar] [CrossRef]
- Martín-González, S.; Portela-Camino, J.; Ruiz-Alcocer, J.; Illarramendi-Mendicute, I.; Garrido-Mercado, R. Stereoacuity Improvement using Random-Dot Video Games. J. Vis. Exp. 2020, e60236. [Google Scholar] [CrossRef]
- Liu, X.Y.; Zhang, Y.W.; Gao, F.; Chen, F.; Zhang, J.Y. Dichoptic Perceptual Training in Children With Amblyopia With or Without Patching History. Investig. Ophthalmol. Vis. Sci. 2021, 62, 4. [Google Scholar] [CrossRef]
- Kadhum, A.; Tan, E.T.C.; Levi, D.M.; Colpa, L.; Fronius, M.; Simonsz, H.J.; Loudon, S.E. Barriers to successful dichoptic treatment for amblyopia in young children. Graefes. Arch. Clin. Exp. Ophthalmol. 2021, 259, 3149–3157. [Google Scholar] [CrossRef]
- Molina-Martín, A.; Leal-Vega, L.; de Fez, D.; Martínez-Plaza, E.; Coco-Martín, M.B.; Piñero, D.P. Amblyopia Treatment through Immersive Virtual Reality: A Preliminary Experience in Anisometropic Children. Vision 2023, 7, 42. [Google Scholar] [CrossRef]
- Xiao, S.; Gaier, E.D.; Wu, H.C.; Angjeli, E.; Nuth, P.L.; Bohra, L.I.; Miller, A.M.; Mazow, M.L.; Stout, A.U.; Morse, C.L.; et al. Digital therapeutic improves visual acuity and encourages high adherence in amblyopic children in open-label pilot study. J. AAPOS 2021, 25, 87.e1–87.e6. [Google Scholar] [CrossRef]
- Kadhum, A.; Tan, E.T.C.; Fronius, M.; Baart, S.J.; Levi, D.M.; Joosse, M.V.; Simonsz, H.J.; Loudon, S.E. Supervised dichoptic gaming versus monitored occlusion therapy for childhood amblyopia: Effectiveness and efficiency. Acta Ophthalmol. 2023. [Google Scholar] [CrossRef]
- Bankó, É.M.; Barboni, M.T.S.; Markó, K.; Körtvélyes, J.; Németh, J.; Nagy, Z.Z.; Vidnyánszky, Z. Fixation instability, astigmatism, and lack of stereopsis as factors impeding recovery of binocular balance in amblyopia following binocular therapy. Sci. Rep. 2022, 12, 10311, Erratum in Sci. Rep. 2022, 12, 13249. [Google Scholar] [CrossRef] [PubMed]
- Wygnanski-Jaffe, T.; Kushner, B.J.; Moshkovitz, A.; Belkin, M.; Yehezkel, O.; CureSight Pivotal Trial Group. An Eye-Tracking-Based Dichoptic Home Treatment for Amblyopia: A Multicenter Randomized Clinical Trial. Ophthalmology 2023, 130, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Abdal, M.O.; Bhombal, F.; Nankani, G.J.; Nankani, S.G.; Lad, S.; Dholam, A.; Kumari, R.; Mahajan, J.; Piñero, D.P. Evaluation of the Efficacy of a New Dichoptic Digital Platform to Treat the Anisometropic and Isometropic Amblyopia. Brain Sci. 2022, 12, 815. [Google Scholar] [CrossRef] [PubMed]
- Murali, K.; Ramesh, A.; Murthy, S.R.; Goyal, A. Binocular therapy as primary intervention in adults with anisometropic amblyopia. Taiwan J. Ophthalmol. 2021, 12, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Picotti, C.; Fernández Irigaray, L.; Del Rivero, A.; Fariñalas, M.; Piñero, D.P. Treatment of Anisometropic Amblyopia with a Dichoptic Digital Platform in Argentinian Children and Adults. Semin. Ophthalmol. 2023, 2, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bhombal, F.; Kothari, M.; Abdal, M.O.; Lad, S.; Nankani, G. Effectiveness of combined dichoptic therapy, binocular vision therapy, and part-time patching for the management of amblyopia in adults. Indian J. Ophthalmol. 2020, 68, 257–258. [Google Scholar] [CrossRef]
- Shah, S.; Shah, M.; Purohit, A.; Khanguda, V. Perceptual learning with hand—Eye coordination as an effective tool for managing amblyopia: A prospective study. Indian J. Ophthalmol. 2022, 70, 3630–3633. [Google Scholar] [CrossRef]
- Poltavski, D.; Adams, R.J.; Biberdorf, D.; Patrie, J.T. Effectiveness of a Novel Video Game Platform in the Treatment of Pediatric Amblyopia. J. Pediatr. Ophthalmol. Strabismus. 2023, 1–10. [Google Scholar] [CrossRef]
- Lan, F.F.; Zhao, W.X.; Gan, L. Evaluation of visual plasticity in patients with refractive amblyopia treated using a visual perceptual learning system. Technol. Health Care 2023. [Google Scholar] [CrossRef]
- Zhu, W.; Tian, T.; Yehezkel, O.; Wygnanski-Jaffe, T.; Moshkovitz, A.; Lin, J.; Hu, C.; Liu, R. A Prospective Trial to Assess the Efficacy of Eye-Tracking-Based Binocular Treatment versus Patching for Children’s Amblyopia: A Pilot Study. Semin. Ophthalmol. 2023, 38, 761–767. [Google Scholar] [CrossRef]
- Hsieh, Y.C.; Liao, W.L.; Tsai, Y.Y.; Lin, H.J. Efficacy of vision therapy for unilateral refractive amblyopia in children aged 7-10 years. BMC Ophthalmol. 2022, 22, 44. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Ye, Q.; Zhang, S.; Feng, L.; Liu, J.; Xu, Z.; Zhuang, Y.; He, Y.; Zhou, Y.; Chen, X.; et al. Contrast Sensitivity and Stereoacuity in Successfully Treated Refractive Amblyopia. Investig. Ophthalmol. Vis. Sci. 2022, 63, 6. [Google Scholar] [CrossRef] [PubMed]
- Arnold, R.W. The impact of autostereoscopic screens on assessing depth perception. Ann. Transl. Med. 2022, 10, 653. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.M.; Manh, V.M.; Lazar, E.L.; Beck, R.W.; Birch, E.E.; Kraker, R.T.; Crouch, E.R.; Erzurum, S.A.; Khuddus, N.; Summers, A.I.; et al. Effect of a Binocular iPad Game vs Part-time Patching in Children Aged 5 to 12 Years With Amblyopia: A Randomized Clinical Trial. JAMA Ophthalmol. 2016, 134, 1391–1400. [Google Scholar] [CrossRef] [PubMed]
- Portela-Camino, J.A.; Martín-González, S.; Ruiz-Alcocer, J.; Illarramendi-Mendicute, I.; Piñero, D.P.; Garrido-Mercado, R. Predictive factors for the perceptual learning in stereodeficient subjects. J. Optom. 2021, 14, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Maniglia, M. Perspectives on the Combined Use of Electric Brain Stimulation and Perceptual Learning in Vision. Vision 2022, 6, 33. [Google Scholar] [CrossRef]
- Jin, L.; Fang, Y.; Jin, C. Binocular treatment for individual with amblyopia: A systematic review and meta-analysis. Medicine 2022, 101, e28975. [Google Scholar] [CrossRef]
- Jost, R.M.; Kelly, K.R.; Birch, E.E. Risk of recurrence after cessation of dichoptic, binocular treatment of amblyopia. J. AAPOS 2023, 27, 298–300. [Google Scholar] [CrossRef]
| Article | Publication Year | Geographical Region | Treatment Type | Age Ranges | Type of Amblyopia |
|---|---|---|---|---|---|
| Leal Vega et al. [27] | 2022 | Valladolid and Alicante, Spain | Dichoptic virtual reality (VR) video game | 5–17 yo | Anisometropic |
| Zheng et al. [28] | 2022 | Shangai, China | Online PL platform versus patching | 4–12 yo | Anisometropic and strabismic |
| Dahlmann-Noor et al. [29] | 2022 | London, UK | Dichoptic movie viewing versus patching | 3–8 yo | Anisometropic, strabismic, and combined |
| Hsieh et al. [30] | 2022 | Taiwan | Combined vision therapy and patching versus patching alone | 7–10 yo | Anisometropic |
| Zhong et al. [5] | 2022 | China | Combined PL and patching and patching alone | >7 yo | Deprivation amblyopia |
| Godinez et al. [12] | 2021 | California, USA | Dichoptic VR video game | 18–62 yo | Mainly strabismic |
| Hou et al. [25] | 2022 | San Fransico, USA | Dichoptic PL video game | 22–62 yo | Anisometropic, strabismic, and combined |
| Hou C. [31] | 2022 | USA | Perceptual learning with dichoptic training | 22–62 yo | Anisometropic, strabismic, and combined |
| Milla et al. [32] | 2022 | Alicante, Spain | Combined vision therapy and occlusion | 7–18 yo | Anisometropic and strabismic |
| Handa et al. [33] | 2022 | Japan, India | Dichoptic video game versus patching | 3–12 yo | Anisometropic |
| Ojiabo et al. [34] | 2022 | South Africa | Dichoptic video game | 19–29 yo | Anisometropic |
| Du et al. [26] | 2023 | Beijing, China | Augmented reality (AR) | >18 yo | |
| Huang et al. [30] | 2022 | China | PL Vision therapy | 7–10 yo | Bilateral amblyopia |
| Tan et al. [35] | 2022 | China | VR versus AR video game | 4–10 yo | Refractive unilateral and bilateral amblyopia |
| Mirmohammadsadeghi et al. [36] | 2022 | Tehran, India | Dichoptic movie viewing | 17–37 yo | Anisometropic, strabismic, and combined |
| Hernández-Rodríguez et al. [37] | 2021 | Alicante, Spain | Monocular PL therapy versus patching | 5–11 yo | Anisometropic and strabismic |
| He et al. [38] | 2023 | China | Monocular PL | 10–24 yo | Anisometropic and strabismic |
| Pang et al. [39] | 2020 | Hong Kong | Dichoptic video game | >7 yo | Anisometrpic, strabismic, and combined |
| Jost et al. [40] | 2022 | Texas, USA | Dichoptic movie viewing versus patching | 3–7 yo | Anisometropic, strabismic, and combined |
| Iwata et al. [41] | 2022 | Japan | Dichoptic movie viewing versus patching | 4–6 yo | Anisometropic |
| Manny et al. [42] | 2022 | USA | Dichoptic video game versus spectacle correction | 4–6 yo | Anisometropic, strabismic, and combined |
| Lee et al. [43] | 2020 | USA | Dichoptic video game versus monocular PL versus combination with patching, Crossover | 8–18 yo | Anisometropic and strabismic |
| Roy et al. [44] | 2022 | India | Dichoptic video game versus occlusion | 5–15 yo | Anisometropic |
| Martín-González et al. [45] | 2020 | Spain | Dichoptic video game | 7–14 yo | Anisometropic and strabismic |
| Liu et al. [46] | 2021 | China | Dichoptic video game | 6–17 yo | Anisometropic, strabismic, and combined |
| Kadhum et al. [47] | 2021 | The Netherlands | Dichoptic VR video game | 4–12 yo | Anisometropic, strabismic, and combined |
| Molina-Martín et al. [48] | 2023 | Spain | Dichoptic VR video game | 8–14 yo | Anisometropic |
| Xiao et al. [49] | 2021 | USA | Dichoptic movie viewing | 4–12 yo | Anisometropic, strabismic, and combined |
| Kadhum et al. [50] | 2023 | The Netherlands | Dichoptic video game versus occlusion | 4–12 yo | Anisometropic, strabismic, and combined |
| Banko et al. [51] | 2023 | Hungary | Dichoptic video game | 6–43 yo | Anisometropic, strabismic, and combined |
| Wygnanski-Jaffe et al. [52] | 2023 | Israel | Dichoptic movie viewing | 4–9 yo | Anisometropic, strabismic, and combined |
| Abdal et al. [53] | 2022 | India | Dichoptic online platform | 4–13 yo | Anisometropic and isometropic |
| Murali et al. [54] | 2021 | India | Dichoptic video game | 18–40 yo | anisometropic |
| Picotti et al. [55] | 2023 | Argentina | Dichoptic online platform | 6–60 yo | anisometropic |
| Bhombal et al. [56] | 2020 | India | Combined dichoptic therapy, vision therapy and part time patching | 20–35 yo | Bilateral refractive and anisometropic |
| Shah et al. [57] | 2022 | India | Dichoptic online platform | 7–21 yo | Anisometropic and strabismic |
| Poltavski et al. [58] | 2023 | USA | Dichoptic video game versus patching | 4–18 yo | Anisometropic |
| Lan et al. [59] | 2023 | China | Vision therapy | 5–8 yo | Refractive |
| Zhu et al. [60] | 2023 | China | Dichoptic movie viewing versus full-time and part-time patching | 4–9 yo | Anisometropic |
| Factor | Correlation with Post-Treatment Visual Outcomes |
|---|---|
| Type of amblyopia | Strabismic amblyopia patients exhibit slower recovery and inferior final binocular functions compared to anisometropic amblyopia [32]. |
| Age | No effect in restoration of stereopsis [51,65]. |
| Astigmatism | The presence of astigmatism is a significant limiting factor for both near and distant VA recovery in children. Conversely, astigmatism has no such influence in adult patients [32]. |
| Baseline stereoacuity | Strongly correlated with the improvement of stereoacuity [51,65]. Patients with poor initial stereopsis seem to require longer treatment to achieve certain degree of improvement [65]. Children with no measurable stereopsis have a >2-fold increased risk for persistent amblyopia [16]. |
| Baseline fixation stability | Poor fixation stability is related to poor monocular and binocular functions in individuals with amblyopia. Recovery of stereopsis is only possible with stable fixation, regardless of age, etiology, or depth of amblyopia [51]. The presence of fixation eye movements (FEMs) and their amplitude, fusion maldevelopment nystagmus syndrome (FMNS), or nystagmus without FMNS in amblyopic patients are associated with weaker response to treatment and limited improvement in stereoacuity [20,51]. |
| Baseline contrast sensitivity (CS) | Initial CS scores have the strongest effect on the final CS gain [51]. Non-measurable baseline stereoacuity and poor final distant VA were found to be restricting factors for CS improvement [51]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsaousis, K.T.; Mousteris, G.; Diakonis, V.; Chaloulis, S. Current Developments in the Management of Amblyopia with the Use of Perceptual Learning Techniques. Medicina 2024, 60, 48. https://doi.org/10.3390/medicina60010048
Tsaousis KT, Mousteris G, Diakonis V, Chaloulis S. Current Developments in the Management of Amblyopia with the Use of Perceptual Learning Techniques. Medicina. 2024; 60(1):48. https://doi.org/10.3390/medicina60010048
Chicago/Turabian StyleTsaousis, Konstantinos T, Georgios Mousteris, Vasilios Diakonis, and Stergios Chaloulis. 2024. "Current Developments in the Management of Amblyopia with the Use of Perceptual Learning Techniques" Medicina 60, no. 1: 48. https://doi.org/10.3390/medicina60010048
APA StyleTsaousis, K. T., Mousteris, G., Diakonis, V., & Chaloulis, S. (2024). Current Developments in the Management of Amblyopia with the Use of Perceptual Learning Techniques. Medicina, 60(1), 48. https://doi.org/10.3390/medicina60010048






