A Retrospective Analysis of the Association of Neutrophil–Lymphocyte Ratio (NLR) with Anemia in the Saudi Population
Abstract
:1. Introduction
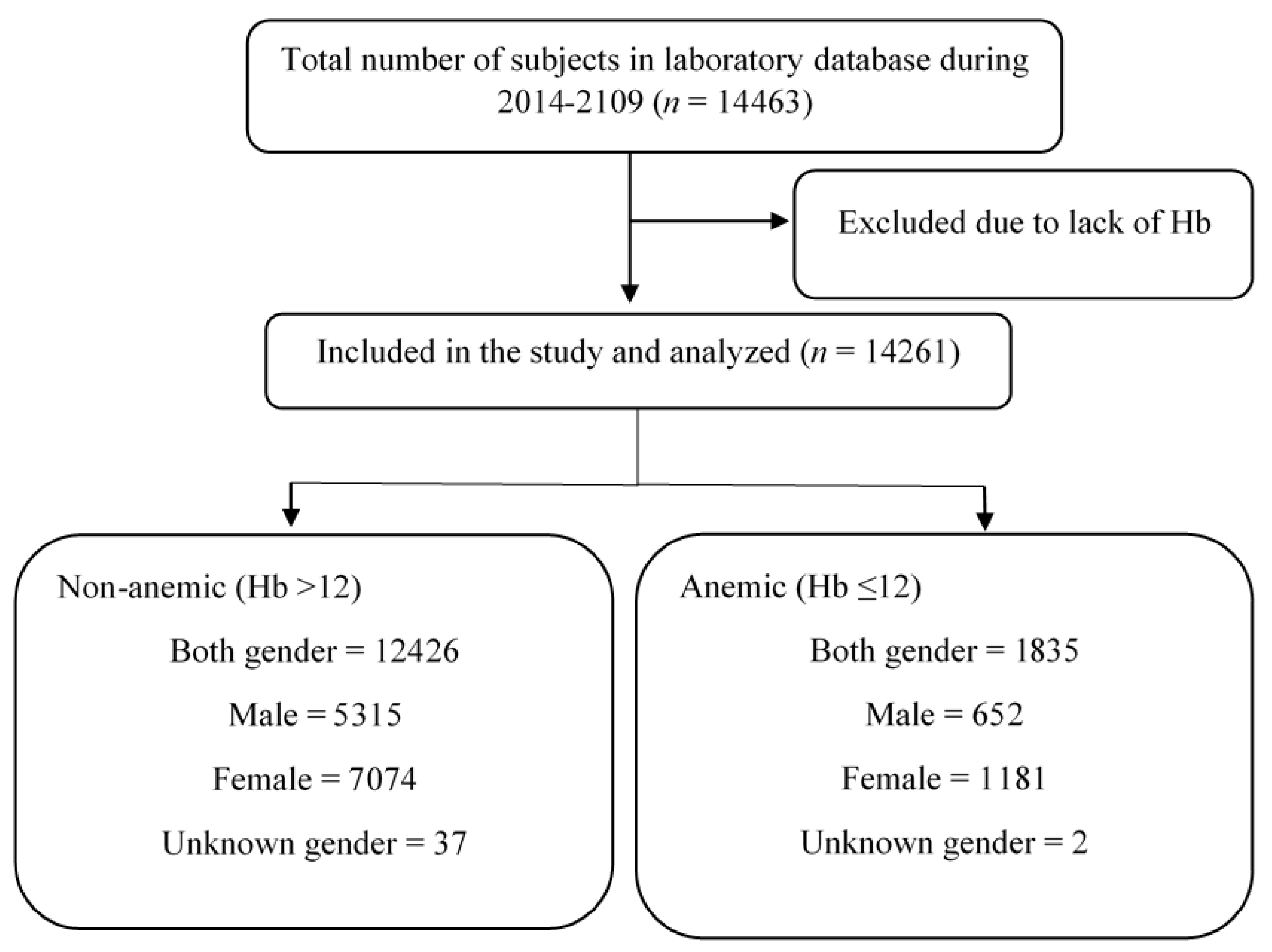
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Statistics
3. Results
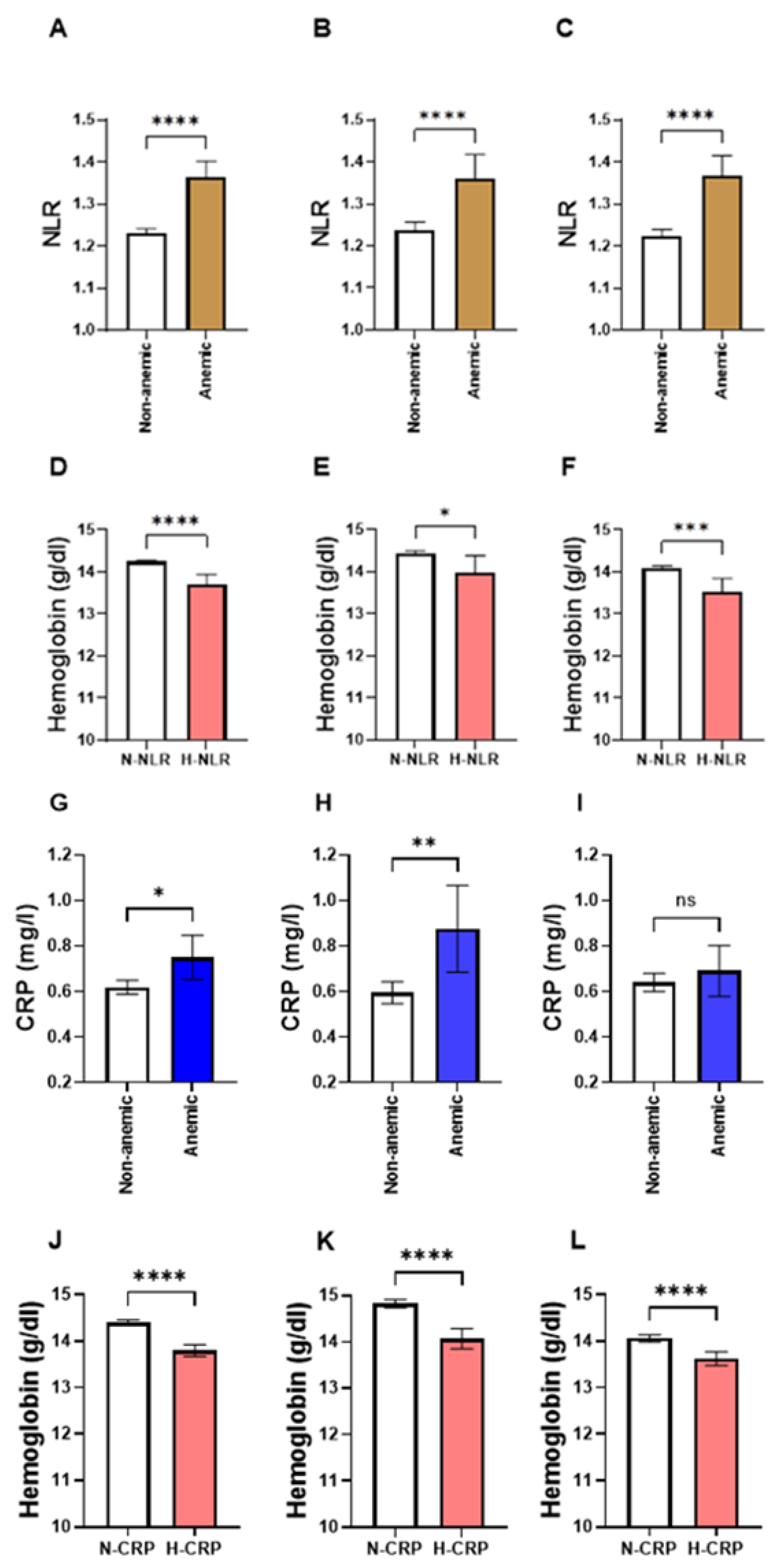
3.1. NLR Is Significantly Elevated in Anemic Individuals
3.2. Subjects with High NLR Have a Lower Hb Concentration
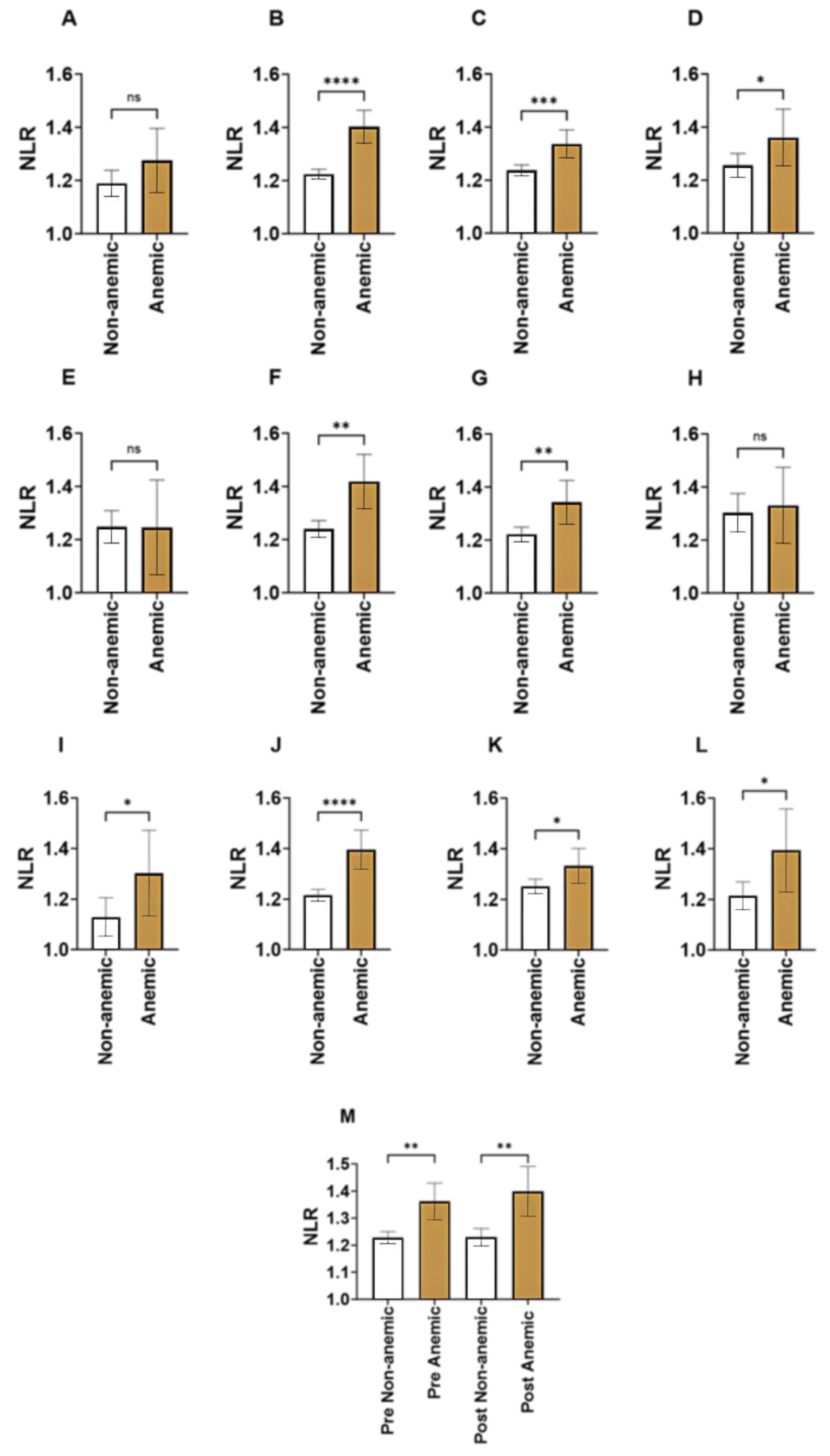
3.3. Age-Specific Comparisons of NLR in Anemia
3.4. Gender-Wise Comparisons of NLR in Anemia
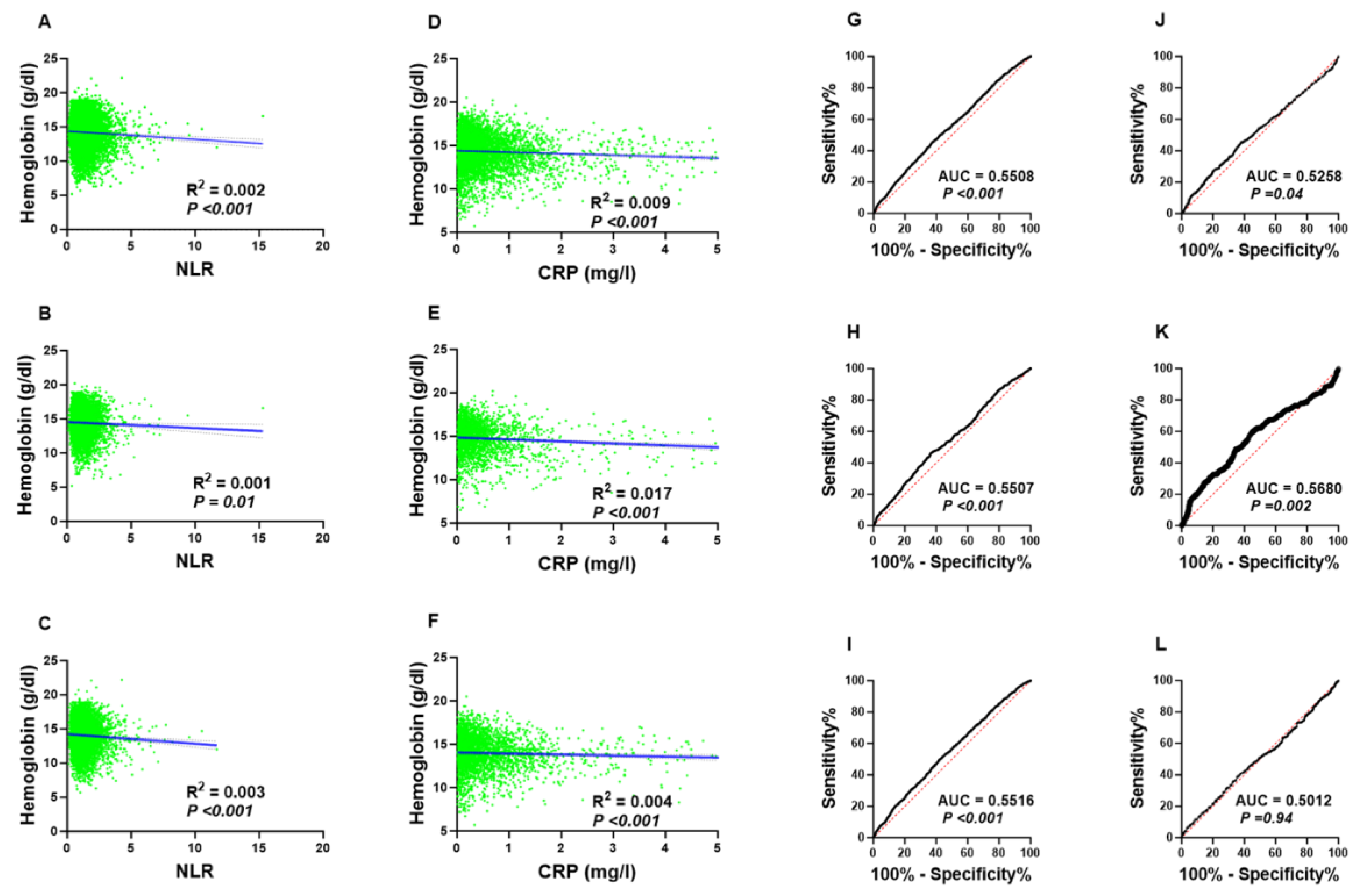
3.5. Elevated NLR Is More Prevalent in Anemic Subjects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Turner, J.; Parsi, M.; Badireddy, M. Anemia. In Handbook of Outpatient Medicine, 2nd ed.; Springer: Cham, Switzerland, 2023; pp. 355–389. [Google Scholar] [CrossRef]
- Chaparro, C.M.; Suchdev, P.S. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Jasrasaria, R.; Naghavi, M.; Wulf, S.K.; Johns, N.; Lozano, R.; Regan, M.; Weatherall, D.; Chou, D.P.; Eisele, T.P.; et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 2014, 123, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.A.; Noori, M.; Nejadghaderi, S.A.; Karamzad, N.; Bragazzi, N.L.; Sullman, M.J.M.; Abdollahi, M.; Collins, G.S.; Kaufman, J.S.; et al. Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: Results from the Global Burden of Disease Study 2019. J. Hematol. Oncol. 2021, 14, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Paciorek, C.J.; Flores-Urrutia, M.C.; Borghi, E.; Namaste, S.; Wirth, J.P.; Suchdev, P.S.; Ezzati, M.; Rohner, F.; Flaxman, S.R.; et al. National, regional, and global estimates of anaemia by severity in women and children for 2000–19: A pooled analysis of population-representative data. Lancet Glob. Health 2022, 10, e627–e639. [Google Scholar] [CrossRef] [PubMed]
- Alquaiz, A.M.; Gad Mohamed, A.; Khoja, T.A.M.; Alsharif, A.; Shaikh, S.A.; Al Mane, H.; Aldiris, A.; Kazi, A.; Hammad, D. Prevalence of anemia and associated factors in child bearing age women in Riyadh, Saudi Arabia. J. Nutr. Metab. 2013, 2013, 636585. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Ganz, T.; Goodnough, L.T. Anemia of inflammation. Blood 2019, 133, 40–50. [Google Scholar] [CrossRef]
- Piccin, A.; O’Connor-Byrne, N.; Daves, M.; Lynch, K.; Farshbaf, A.D.; Martin-Loeches, I. Autoimmune disease and sickle cell anaemia: ‘Intersecting pathways and differential diagnosis’. Br. J. Haematol. 2022, 197, 518–528. [Google Scholar] [CrossRef]
- Santos, E.J.F.; Dias, R.S.C.; Lima, J.F.d.B.; Filho, N.S.; Dos Santos, A.M. Erythropoietin resistance in patients with chronic kidney disease: Current perspectives. Int. J. Nephrol. Renov. Dis. 2020, 13, 231–237. [Google Scholar] [CrossRef]
- Binnetoğlu, E.; Şengül, E.; Halhallı, G.; Dindar, S.; Şen, H. Is Neutrophil Lymphocyte Ratio an Indicator for Proteinuria in Chronic Kidney Disease? J. Clin. Lab. Anal. 2014, 28, 487–492. [Google Scholar] [CrossRef]
- Prasetya, D.; Rochadi; Gunadi. Accuracy of neutrophil lymphocyte ratio for diagnosis of acute appendicitis in children: A diagnostic study. Ann. Med. Surg. 2019, 48, 35–38. [Google Scholar] [CrossRef]
- Sayed, A.A.; Allam, A.A.; Sayed, A.I.; Alraey, M.A.; Joseph, M.V. The use of neutrophil-to-lymphocyte ratio (NLR) as a marker for COVID-19 infection in Saudi Arabia: A case-control retrospective multicenter study. Saudi Med. J. 2021, 42, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Curran, F.M.; Bhalraam, U.; Mohan, M.; Singh, J.S.; Anker, S.D.; Dickstein, K.; Doney, A.S.; Filippatos, G.; George, J.; Metra, M.; et al. Neutrophil-to-lymphocyte ratio and outcomes in patients with new-onset or worsening heart failure with reduced and preserved ejection fraction. ESC Hear. Fail. 2021, 8, 3168–3179. [Google Scholar] [CrossRef]
- Sharma, D.J.; Nath, H.J.; Batta, A.; Goala, A.K. Neutrophil-to-Lymphocyte Ratio (NLR) Useful as a Cost-Effective Preliminary Prognostic Marker in ST-Elevation Myocardial Infarction (STEMI): An Observational Study from a Tertiary Care Hospital in Northeast India. Cureus 2023, 15, e36885. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Q.; Wu, H.; Du, H.; Liu, L.; Shi, H.; Wang, C.; Xia, Y.; Guo, X.; Li, C.; et al. Blood neutrophil to lymphocyte ratio as a predictor of hypertension. Am. J. Hypertens. 2015, 28, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Mertoglu, C.; Gunay, M. Neutrophil-Lymphocyte ratio and Platelet-Lymphocyte ratio as useful predictive markers of prediabetes and diabetes mellitus. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, S127–S131. [Google Scholar] [CrossRef] [PubMed]
- Alfhili, M.A.; Alsughayyir, J.; Basudan, A.; Ghneim, H.K.; Aboul-Soud, M.A.M.; Marie, M.; Dera, A.; Alfaifi, M.; Alkhathami, A.G.; Awan, Z.A.; et al. Isolated and Combined Effect of Age and Gender on Neutrophil–Lymphocyte Ratio in the Hyperglycemic Saudi Population. Medicina 2022, 58, 1040. [Google Scholar] [CrossRef]
- Alfhili, M.A.; Alsughayyir, J.; Basudan, A.M.; Alsubki, R.; Alqahtani, S.; Awan, Z.A.; Algethami, M.R.; Al-Sheikh, Y.A. Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population. Healthcare 2022, 10, 2289. [Google Scholar] [CrossRef]
- Zahorec, R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl. Med. J. 2021, 122, 474–488. [Google Scholar] [CrossRef]
- Singh, K. Leucocyte counts in anaemia. Indian J. Physiol. Pharmacol. 2010, 54, 85–88. [Google Scholar]
- Owen, W.F.; Lowrie, E.G. C-reactive protein as an outcome predictor for maintenance hemodialysis patients. Kidney Int. 1998, 54, 627–636. [Google Scholar] [CrossRef]
- Zhang, P.; Tong, Y.; Yuan, D.; Li, Y.; Jin, Y.; Bai, L.; Gao, P.; Wang, W.; Hu, J.; Duan, X.; et al. Association of high-sensitivity C-reactive protein and anemia with acute kidney injury in neonates. Front. Pediatr. 2022, 10, 882739. [Google Scholar] [CrossRef]
- Ziv-Baran, T.; Wasserman, A.; Goldiner, I.; Stark, M.; Shenhar-Tsarfaty, S.; Shapira, I.; Zeltser, D.; Mailis, I.; Berliner, S.; Rogowski, O. The association between C-reactive protein and common blood tests in apparently healthy individuals undergoing a routine health examination. Clin. Chim. Acta 2020, 501, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Heidari, B.; Fazli, M.R.; Misaeid, M.A.G.; Heidari, P.; Hakimi, N.; Zeraati, A.A. A linear relationship between serum high-sensitive C-reactive protein and hemoglobin in hemodialysis patients. Clin. Exp. Nephrol. 2015, 19, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Guralnik, J.M.; Bandinelli, S.; Semba, R.D.; Lauretani, F.; Corsi, A.; Ruggiero, C.; Ershler, W.B.; Longo, D.L. Unexplained anaemia in older persons is characterised by low erythropoietin and low levels of pro-inflammatory markers. Br. J. Haematol. 2007, 136, 849–855. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Ortona, E.; Pierdominici, M.; Rider, V. Editorial: Sex hormones and gender differences in immune responses. Front. Immunol. 2019, 10, 1076. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Rahman, M.S.; Aziz Rahman, M.; Szymlek-Gay, E.A.; Uddin, R.; Islam, S.M.S. Prevalence of and factors associated with anaemia in women of reproductive age in Bangladesh, Maldives and Nepal: Evidence from nationally-representative survey data. PLoS ONE 2021, 16, e0245335. [Google Scholar] [CrossRef]
- Emokpae, M.; Aruomaren, A.; Osime, E. Relationship between Neutrophil-to-Lymphocyte Ratio and Inflammatory Markers in Sickle Cell Anaemia Patients with Proteinuria. Med. Sci. 2016, 4, 11. [Google Scholar] [CrossRef]
- Jadoon, S.K.; Soomro, R.; Ahsan, M.N.; Khan, R.M.I.; Iqbal, S.; Yasmin, F.; Najeeb, H.; Saleem, N.; Cho, N.; Shaikh, T.G.; et al. Association of neutrophil-to-lymphocyte ratio with clinical, pathological, radiological, laboratory features and disease outcomes of invasive breast cancer patients A retrospective observational cohort study. Medicine 2023, 102, e33811. [Google Scholar] [CrossRef]
- Sahin, B.E.; Celikbilek, A.; Kocak, Y.; Koysuren, A.; Hizmali, L. Associations of the neutrophil/lymphocyte ratio, monocyte/lymphocyte ratio, and platelet/lymphocyte ratio with COVID-19 disease severity in patients with neurological symptoms: A cross-sectional monocentric study. J. Neurosci. Rural. Pract. 2022, 14, 224–229. [Google Scholar] [CrossRef]
- Ning, P.; Yang, F.; Kang, J.; Yang, J.; Zhang, J.; Tang, Y.; Ou, Y.; Wan, H.; Cao, H. Predictive value of novel inflammatory markers platelet-to-lymphocyte ratio, neutrophil-to-lymphocyte ratio, and monocyte-to-lymphocyte ratio in arterial stiffness in patients with diabetes: A propensity score–matched analysis. Front. Endocrinol. 2022, 13, 1039700. [Google Scholar] [CrossRef] [PubMed]
- Dharmapuri, S.; Özbek, U.; Lin, J.Y.; Sung, M.; Schwartz, M.; Branch, A.D.; Ang, C. Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in advanced hepatocellular carcinoma patients treated with anti–PD-1 therapy. Cancer Med. 2020, 9, 4962–4970. [Google Scholar] [CrossRef]
- Szilasi, Z.; Jósa, V.; Zrubka, Z.; Mezei, T.; Vass, T.; Merkel, K.; Helfferich, F.; Baranyai, Z. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as prognostic markers of survival in patients with head and neck tumours—Results of a retrospective multicentric study. Int. J. Environ. Res. Public Health 2020, 17, 1742. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Wei, D.; Sun, C.; Yang, Y.; Wei, Y.; Liu, X. Prognostic value of the combination of neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio and platelet-to-lymphocyte ratio on mortality in patients on maintenance hemodialysis. BMC Nephrol. 2022, 23, 393. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Ivanescu, A.D.; Fodor, P.; Moldovan, L.; Bataga, T. Correlation between Inflammatory Systemic Biomarkers and Surgical Trauma in Elderly Patients with Hip Fractures. J. Clin. Med. 2023, 12, 5147. [Google Scholar] [CrossRef]
- Begum, S.; Latunde-Dada, G.O. Anemia of inflammation with an emphasis on chronic kidney disease. Nutrients 2019, 11, 2424. [Google Scholar] [CrossRef] [PubMed]
- Ganz, T.; Nemeth, E. Iron homeostasis in host defence and inflammation. Nat. Rev. Immunol. 2015, 15, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Kowdley, K.V.; Gochanour, E.M.; Sundaram, V.; Shah, R.A.; Handa, P. Hepcidin Signaling in Health and Disease: Ironing Out the Details. Hepatol. Commun. 2021, 5, 723–735. [Google Scholar] [CrossRef]
- Nemeth, E.; Rivera, S.; Gabayan, V.; Keller, C.; Taudorf, S.; Pedersen, B.K.; Ganz, T. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J. Clin. Investig. 2004, 113, 1271–1276. [Google Scholar] [CrossRef]
| Number of Subjects (%) | Mean WBC Count (×106/mL) (95% CI) | Mean NLR (95%CI) | |
|---|---|---|---|
| Male | |||
| Young | 3.05 | 6.17 (5.99–6.35) | 1.25 (1.19–1.31) |
| Young Adult | 16.65 | 6.06 (5.99–6.14) | 1.26 (1.23–1.29) |
| Adult | 18.21 | 6.01 (5.94–6.08) | 1.23 (1.21–1.26) |
| Elderlies | 3.93 | 6.17 (6.01–6.32) | 1.31 (1.12–1.37) |
| Female | |||
| Young | 3.02 | 5.93 (5.74–6.12) | 1.15 (1.08–1.22) |
| Young Adult | 30.36 | 5.98 (5.93–6.04) | 1.24 (1.22–1.26) |
| Adult | 20.12 | 6.04 (5.97–6.11) | 1.26 (1.24–1.29) |
| Elderlies | 4.39 | 6.02 (5.87–6.18) | 1.24 (1.18–1.29) |
| Unknown gender | 0.27 | 6.11 (5.46–6.76) | 1.26 (1.10–1.41) |
| Parameter | Non-Anemic | Anemic |
|---|---|---|
| Both genders | ||
| N-NLR | 97.33 | 95.02 |
| H-NLR | 2.67 | 4.98 |
| N-CRP | 85.05 | 79.08 |
| H-CRP | 14.95 | 20.92 |
| Male | ||
| N-NLR | 97.63 | 95.54 |
| H-NLR | 2.37 | 4.46 |
| N-CRP | 86.73 | 75.38 |
| H-CRP | 13.27 | 24.62 |
| Female | ||
| N-NLR | 97.09 | 94.72 |
| H-NLR | 2.91 | 5.28 |
| N-CRP | 83.24 | 80.93 |
| H-CRP | 16.76 | 19.07 |
| Score | 95% CI | z Statistic | Significance Level | |
|---|---|---|---|---|
| PR | ||||
| Both genders | 1.87 | 1.46–2.40 | 4.92 | p < 0.0001 |
| Males | 1.88 | 1.23–2.89 | 2.89 | p = 0.004 |
| Females | 1.81 | 1.34–2.46 | 3.83 | p = 0.0001 |
| OR | ||||
| Both genders | 1.91 | 1.47–2.48 | 4.88 | p < 0.0001 |
| Males | 1.92 | 1.23–3.01 | 2.87 | p = 0.004 |
| Females | 2.22 | 1.64–3.00 | 5.18 | p < 0.0001 |
| Score | 95% CI | z Statistic | Significance Level | |
|---|---|---|---|---|
| PR | ||||
| Both genders | 1.40 | 1.18–1.65 | 3.95 | p = 0.0001 |
| Males | 1.86 | 1.42–2.42 | 4.53 | p < 0.0001 |
| Females | 1.14 | 0.92–1.42 | 1.19 | p = 0.24 |
| OR | ||||
| Both genders | 1.51 | 1.22–1.85 | 3.85 | p = 0.0001 |
| Males | 2.13 | 1.51–3.02 | 4.28 | p < 0.0001 |
| Females | 1.17 | 0.90–1.52 | 1.18 | p = 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshuweishi, Y.; Alfaifi, M.; Almoghrabi, Y.; Al-Sheikh, Y.A.; Alfhili, M.A. A Retrospective Analysis of the Association of Neutrophil–Lymphocyte Ratio (NLR) with Anemia in the Saudi Population. Medicina 2023, 59, 1592. https://doi.org/10.3390/medicina59091592
Alshuweishi Y, Alfaifi M, Almoghrabi Y, Al-Sheikh YA, Alfhili MA. A Retrospective Analysis of the Association of Neutrophil–Lymphocyte Ratio (NLR) with Anemia in the Saudi Population. Medicina. 2023; 59(9):1592. https://doi.org/10.3390/medicina59091592
Chicago/Turabian StyleAlshuweishi, Yazeed, Mohammed Alfaifi, Yousef Almoghrabi, Yazeed A. Al-Sheikh, and Mohammad A. Alfhili. 2023. "A Retrospective Analysis of the Association of Neutrophil–Lymphocyte Ratio (NLR) with Anemia in the Saudi Population" Medicina 59, no. 9: 1592. https://doi.org/10.3390/medicina59091592
APA StyleAlshuweishi, Y., Alfaifi, M., Almoghrabi, Y., Al-Sheikh, Y. A., & Alfhili, M. A. (2023). A Retrospective Analysis of the Association of Neutrophil–Lymphocyte Ratio (NLR) with Anemia in the Saudi Population. Medicina, 59(9), 1592. https://doi.org/10.3390/medicina59091592







