Learning of Basic Life Support through the Flipped Classroom in Secondary Schoolchildren: A Quasi-Experimental Study with 12-Month Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
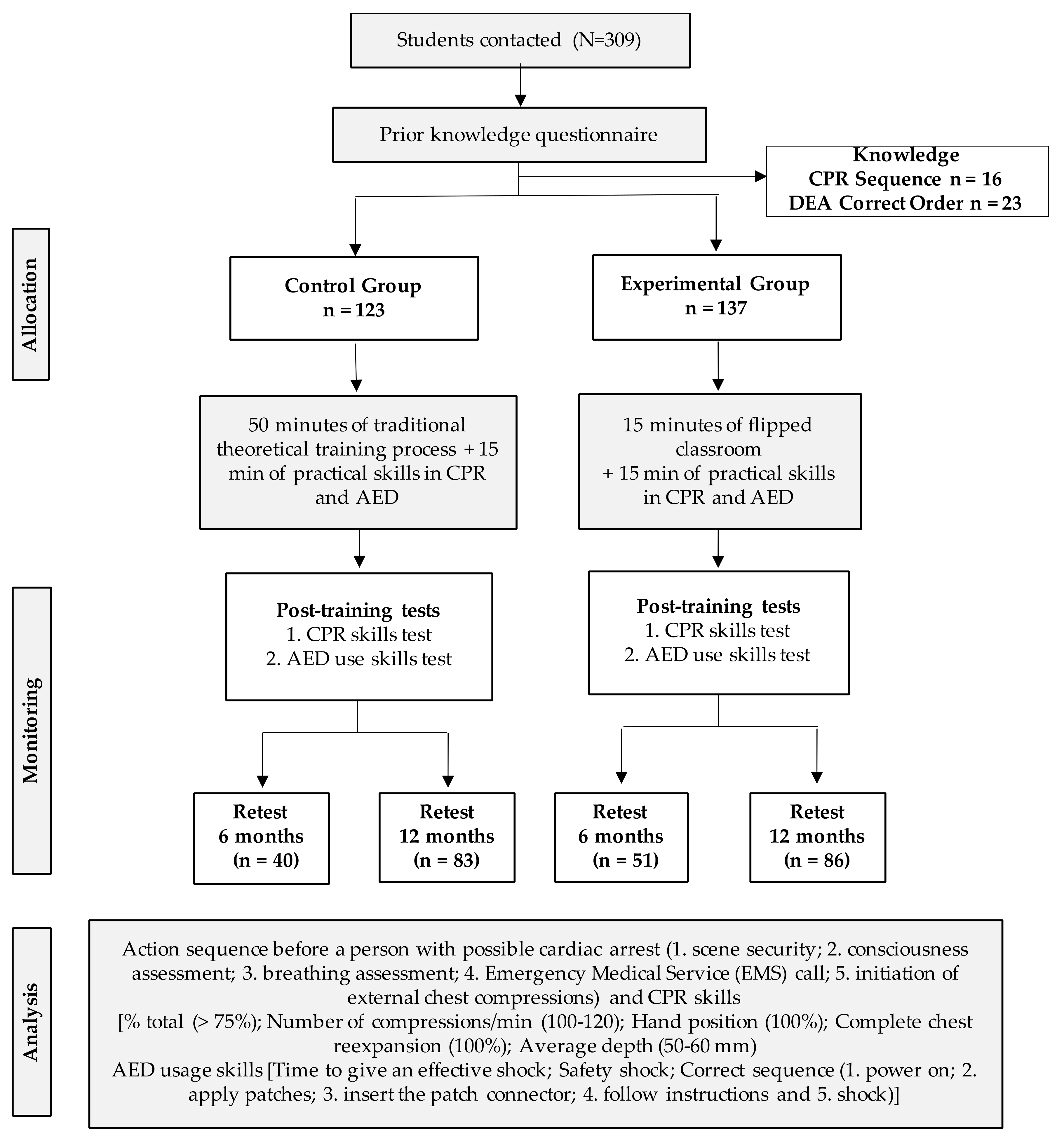
2.1. Study Design
2.2. Participants
2.3. Tools and Measurements
2.3.1. Ad Hoc Questionnaire
2.3.2. Anthropometric Data
2.3.3. CPR Data Collected
2.3.4. AED Data Collection
2.4. Procedure
2.5. Data Analysis
3. Results
3.1. Baseline Characteristics
3.2. Results Regarding the Sequence of Action in the Event of a Possible Cardiac Arrest
3.3. CPR Skills
3.4. AED Application
4. Discussion
4.1. BLS Action Sequence
4.2. Hands-Only CPR Skills
4.3. AED Application
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parnell, M.M.; Pearson, J.; Galletly, D.C.; Larsen, P.D. Knowledge of and attitudes towards resuscitation in New Zealand high-school students. Emerg. Med. J. 2006, 23, 899–902. [Google Scholar] [CrossRef]
- Riva, G.; Ringh, M.; Jonsson, M.; Svensson, L.; Herlitz, J.; Claesson, A.; Djärv, T.; Nordberg, P.; Forsberg, S.; Rubertsson, S.; et al. Survival in Out-of-Hospital Cardiac Arrest After Standard Cardiopulmonary Resuscitation or Chest Compressions Only Before Arrival of Emergency Medical Services. Circulation 2019, 139, 2600–2609. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, T.; Nishiyama, C.; Murakami, Y.; Yonezawa, T.; Nakai, S.; Hamanishi, M.; Marukawa, S.; Sakamoto, T.; Iwami, T. Compression-only CPR training in elementary schools and student attitude toward CPR. Pediatr. Int. 2016, 58, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Pivač, S.; Gradišek, P.; Skela-Savič, B. The impact of cardiopulmonary resuscitation (CPR) training on schoolchildren and their CPR knowledge, attitudes toward CPR, and willingness to help others and to perform CPR: Mixed methods research design. BMC Public Health 2020, 20, 915. [Google Scholar] [CrossRef]
- Plant, N.; Taylor, K. How best to teach CPR to schoolchildren: A systematic review. Resuscitation 2013, 84, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Bohn, A.; Van Aken, H.K.; Möllhoff, T.; Wienzek, H.; Kimmeyer, P.; Wild, E.; Döpker, S.; Lukas, R.P.; Weber, T.P. Teaching resuscitation in schools: Annual tuition by trained teachers is effective starting at age 10. A four-year prospective cohort study. Resuscitation 2012, 83, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Böttiger, B.W.; Bossaert, L.L.; Castrén, M.; Cimpoesu, D.; Georgiou, M.; Greif, R.; Grünfeld, M.; Lockey, A.; Lott, C.; Maconochie, I.; et al. Kids Save Lives—ERC position statement on school children education in CPR: “Hands that help—Training children is training for life”. Resuscitation 2016, 105, A1–A3. [Google Scholar] [CrossRef]
- Banfai, B.; Pandur, A.; Schiszler, B.; Pék, E.; Radnai, B.; Bánfai-Csonka, H.; Betlehem, J. Little lifesavers: Can we start first aid education in kindergarten?—A longitudinal cohort study. Health Educ. J. 2018, 77, 1007–1017. [Google Scholar] [CrossRef]
- Navarro-Patón, R.; Freire-Tellado, M.; Basanta-Camiño, S.; Barcala-Furelos, R.; Arufe-Giraldez, V.; Rodriguez-Fernández, J.E. Effect of 3 basic life support training programs in future primary school teachers. A quasi-experimental design. Med. Intensiv. 2018, 42, 207–215. [Google Scholar] [CrossRef]
- Stroobants, J.; Monsieurs, K.G.; Devriendt, B.; Dreezen, C.; Vets, P.; Mols, P. Schoolchildren as BLS instructors for relatives and friends: Impact on attitude towards bystander CPR. Resuscitation 2014, 85, 1769–1774. [Google Scholar] [CrossRef]
- Watanabe, K.; Lopez-Colon, D.; Shuster, J.J.; Philip, J. Efficacy and retention of Basic Life Support education including Automated External Defibrillator usage during a physical education period. Prev. Med. Rep. 2017, 5, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Borovnik Lesjak, V.; Šorgo, A.; Strnad, M. Development, validation and assessment of the test on knowledge about basic life support and use of automated external defibrillator among schoolchildren. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 114. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Padilla, J.M.; Suthers, F.; Granero-Molina, J.; Fernández-Sola, C. Effects of two retraining strategies on nursing students’ acquisition and retention of BLS/AED skills: A cluster randomised trial. Resuscitation 2015, 93, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Greif, R.; Lockey, A.S.; Conaghan, P.; Lippert, A.; De Vries, W.; Monsieurs, K.G.; Ballance, J.H.W.; Barelli, A.; Biarent, D.; Bossaert, L.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 10. Education and implementation of resuscitation. Resuscitation 2015, 95, 288–301. [Google Scholar] [CrossRef] [PubMed]
- Pavón-Prieto, M.d.P.; Navarro-Patón, R.; Basanta-Camiño, S.; Regueira-Méndez, C.; Neira-Pájaro, M.Á.; Freire-Tellado, M. Estudio cuasiexperimental para evaluar la capacidad de los escolares para utilizar un desfibrilador externo semiautomático a los 6 meses tras un proceso formativo. Emerg. Rev. Soc. Esp. Med. Urgenc. Emerg. 2016, 28, 114–116. [Google Scholar]
- Böttiger, B.W.; Van Aken, H. Training children in cardiopulmonary resuscitation worldwide. Lancet 2015, 385, 2353. [Google Scholar] [CrossRef]
- Böttiger, B.W.; Van Aken, H. Kids save lives: Training school children in cardiopulmonary resuscitation worldwide is now endorsed by the World Health Organization (WHO). Resuscitation 2015, 94, A5–A7. [Google Scholar] [CrossRef]
- Abelairas-Gómez, C.; Martinez-Isasi, S.; Barcala-Furelos, R.; Varela-Casal, C.; Carballo-Fazanes, A.; Pichel-López, M.; Fernández Méndez, F.; Otero-Agra, M.; Sanchez Santos, L.; Rodriguez-Nuñez, A. Training frequency for educating schoolchildren in basic life support: Very brief 4-month rolling-refreshers versus annual retraining—A 2-year prospective longitudinal trial. BMJ Open 2021, 11, e052478. [Google Scholar] [CrossRef]
- Lago-Ballesteros, J.; Basanta-Camiño, S.; Navarro-Paton, R. La enseñanza de los primeros auxilios en educación física: Revisión sistemática acerca de los materiales para su implementación. Retos 2018, 34, 349–355. [Google Scholar] [CrossRef]
- Schmidt, S.M.P.; Ralph, D.L. The flipped classroom: A twist on teaching. Contemp. Issues Educ. Res. 2016, 9, 1–6. [Google Scholar] [CrossRef]
- Garcia del Aguila, J.J.; López Rebollo, E.; Escamilla Pérez, R.; Luque Gutiérrez, M.; Fernández Valle, P.; García Sánchez, M.; Lucena Serrano, C.; Vivar Díaz, I.; Berbel González, F.; Pérez López, S.; et al. Formación de escolares en soporte vital básico por sus propios profesores. Emerg. Rev. Soc. Esp. Med. Urgenc. Emerg. 2019, 31, 185–188. [Google Scholar]
- Greif, R.; Lockey, A.; Breckwoldt, J.; Carmona, F.; Conaghan, P.; Kuzovlev, A.; Pflanzl-Knizacek, L.; Sari, F.; Shammet, S.; Scapigliati, A.; et al. European Resuscitation Council Guidelines 2021: Education for resuscitation. Resuscitation 2021, 161, 388–407. [Google Scholar] [CrossRef] [PubMed]
- Ato, M.; López, J.J.; Benavente, A. Un sistema de clasificación de los diseños de investigación en psicología. An. Psicol. 2013, 29, 1038–1059. [Google Scholar] [CrossRef]
- Olasveengen, T.M.; Mancini, M.E.; Perkins, G.D.; Avis, S.; Brooks, S.; Castrén, M.; Chung, S.P.; Considine, J.; Couper, K.; Escalante, R.; et al. Adult Basic Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020, 142, S41–S91. [Google Scholar] [CrossRef]
- Navarro-Patón, R.; Cons-Ferreiro, M.; Romo-Pérez, V. Schoolteacher´s theoretical and skills knowledge on cardiopulmonary resuscitation and use of the automated external defibrillator after a video-training process. Retos 2021, 42, 172–181. [Google Scholar] [CrossRef]
- Navarro-Patón, R.; Cons-Ferreiro, M.; Mecías-Calvo, M.; Romo-Pérez, V. Acquisition of knowledge and skills on cardiopulmonary resuscitation and use of the automated external defibrillator after a training process by Galician schoolteachers. J. Hum. Sport Exerc. 2022, 17, 931–941. [Google Scholar] [CrossRef]
- Böttiger, B.W.; Lockey, A.; Georgiou, M.; Greif, R.; Monsieurs, K.G.; Mpotos, N.; Nikolaou, N.; Nolan, J.; Perkins, G.; Semeraro, F.; et al. KIDS SAVE LIVES: ERC Position statement on schoolteacher´s education and qualification in resuscitation. Resuscitation 2020, 151, 87–90. [Google Scholar] [CrossRef]
- Monteiro, M.d.L.R.B.P.; Ferraz, A.I.B.; Rodrigues, F.M.P. Assessment of knowledge and self efficacy before and after teaching basic life support to schoolchildren. Rev. Paul. Pediatr. 2021, 39, e2019143. [Google Scholar] [CrossRef]
- Yeung, J.; Kovic, I.; Vidacic, M.; Skilton, E.; Higgins, D.; Melody, T.; Lockey, A. The School Lifesavers Study—A randomised controlled trial comparing the impact of Lifesaver only, Lifesaver with face-to-face training and face-to-face training only on CPR knowledge, skills and attitudes in UK school children. Resuscitation 2017, 118, e12–e13. [Google Scholar] [CrossRef]
- Weidenauer, D.; Hamp, T.; Schriefl, C.; Holaubek, C.; Gattinger, M.; Krammel, M.; Winnisch, M.; Weidenauer, A.; Mundigler, G.; Lang, I.; et al. The impact of cardiopulmonary resuscitation (CPR) manikin chest stiffness on motivation and CPR performance measures in children undergoing CPR training—A prospective, randomized, single-blind, controlled trial. PLoS ONE 2018, 13, e0202430. [Google Scholar] [CrossRef]
- Martínez-Isasi, S.; Abelairas-Gómez, C.; Pichel-López, M.; Barcala-Furelos, R.; Varela-Casal, C.; Vázquez-Santamariña, D.; Sánchez-Santos, L.; Rodríguez-Núñez, A. Learning to resuscitate at school. Study in 8-12 year-old schoolchildren. An. Pediatr. 2022, 96, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Borovnik Lesjak, V.; Šorgo, A.; Strnad, M. Retention of Knowledge and Skills After a Basic Life Support Course for Schoolchildren: A Prospective Study. Inq. J. Health Care Organ. Provis. Financ. 2022, 59, 00469580221098755. [Google Scholar] [CrossRef] [PubMed]
- AHA. American Heart Association Basic Life Support (BLS) Provider Manual; American Heart Association: Tulsa, OK, USA, 2020; ISBN 1616694742. [Google Scholar]
- Plotnikoff, R.; Moore, P.J. Retention of cardiopulmonary resuscitation knowledge and skills by 11- and 12-year-old children. Med. J. Aust. 1989, 150, 296–302. [Google Scholar] [CrossRef] [PubMed]
- González-Salvado, V.; Abelairas-Gómez, C.; Peña-Gil, C.; Neiro-Rey, C.; Barcala-Furelos, R.; González-Juanatey, J.R.; Rodríguez-Núñez, A. Basic life support training into cardiac rehabilitation programs: A chance to give back. A community intervention controlled manikin study. Resuscitation 2018, 127, 14–20. [Google Scholar] [CrossRef]
- Süss-Havemann, C.; Kosan, J.; Seibold, T.; Dibbern, N.M.; Daubmann, A.; Kubitz, J.C.; Beck, S. Implementation of Basic Life Support training in schools: A randomised controlled trial evaluating self-regulated learning as alternative training concept. BMC Public Health 2020, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Van Raemdonck, V.; Monsieurs, K.G.; Aerenhouts, D.; De Martelaer, K. Teaching basic life support: A prospective randomized study on low-cost training strategies in secondary schools. Eur. J. Emerg. Med. 2014, 21, 284–290. [Google Scholar] [CrossRef]
- Allan, K.S.; Mammarella, B.; Visanji, M.; Moglica, E.; Sadeghlo, N.; O’Neil, E.; Chan, T.T.; Kishibe, T.; Aves, T. Methods to teach schoolchildren how to perform and retain cardiopulmonary resuscitation (CPR) skills: A systematic review and meta-analysis. Resusc. Plus 2023, 15, 100439. [Google Scholar] [CrossRef]
- Meissner, T.M.; Kloppe, C.; Hanefeld, C. Basic life support skills of high school students before and after cardiopulmonary resuscitation training: A longitudinal investigation. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 31. [Google Scholar] [CrossRef]
- Mpotos, N.; Iserbyt, P. Children saving lives: Training towards CPR excellence levels in chest compression based on age and physical characteristics. Resuscitation 2017, 121, 135–140. [Google Scholar] [CrossRef]
- Contri, E.; Cornara, S.; Somaschini, A.; Dossena, C.; Tonani, M.; Epis, F.; Zambaiti, E.; Fichtner, F.; Baldi, E. Complete chest recoil during laypersons’ CPR: Is it a matter of weight? Am. J. Emerg. Med. 2017, 35, 1266–1268. [Google Scholar] [CrossRef]
- Mathew, R.; Sahu, A.K.; Thakur, N.; Katyal, A.; Bhoi, S.; Aggarwal, P. Hands-only cardiopulmonary resuscitation training for schoolchildren: A comparison study among different class groups. Turk. J. Emerg. Med. 2020, 20, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Connolly, M.; Toner, P.; Connolly, D.; McCluskey, D.R. The ‘ABC for life’ programme—Teaching basic life support in schools. Resuscitation 2007, 72, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Lester, C.A.; Weston, C.F.M.; Donnelly, P.D.; Assar, D.; Morgan, M.J. The need for wider dissemination of CPR skills: Are schools the answer? Resuscitation 1994, 28, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Greif, R.; Bhanji, F.; Bigham, B.L.; Bray, J.; Breckwoldt, J.; Cheng, A.; Duff, J.P.; Gilfoyle, E.; Hsieh, M.-J.; Iwami, T.; et al. Education, Implementation, and Teams: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020, 156, A188–A239. [Google Scholar] [CrossRef] [PubMed]
- Otero-Agra, M.; Barcala-Furelos, R.; Besada-Saavedra, I.; Peixoto-Pino, L.; Martínez-Isasi, S.; Rodríguez-Núñez, A. Let the kids play: Gamification as a CPR training methodology in secondary school students. A quasi-experimental manikin simulation study. Emerg. Med. J. 2019, 36, 653–659. [Google Scholar] [CrossRef]
- Abelairas-Gómez, C.; Rodríguez-Núñez, A.; Casillas-Cabana, M.; Romo-Pérez, V.; Barcala-Furelos, R. Schoolchildren as life savers: At what age do they become strong enough? Resuscitation 2014, 85, 814–819. [Google Scholar] [CrossRef]
- Fariduddin, M.N.; Mohamed, M.; Jaafar, M.J.; Baharin, K.; Siau, C.S.; Bashah, K. Compression-Only Cardiopulmonary Resuscitation and Automated External Defibrillator Course for Primary School Students: A Malaysian Pilot Study. Children 2023, 10, 58. [Google Scholar] [CrossRef]
- Jorge-Soto, C.; Abelairas-Gómez, C.; Barcala-Furelos, R.; Garrido-Viñas, A.; Navarro-Patón, R.; Muiño-Piñeiro, M.; Díaz-Pereira, M.P.; Rodríguez-Núñez, A. Automated external defibrillation skills by naive schoolchildren. Resuscitation 2016, 106, 37–41. [Google Scholar] [CrossRef]
- De Buck, E.; Van Remoortel, H.; Dieltjens, T.; Verstraeten, H.; Clarysse, M.; Moens, O.; Vandekerckhove, P. Evidence-based educational pathway for the integration of first aid training in school curricula. Resuscitation 2015, 94, 8–22. [Google Scholar] [CrossRef]
| Variable | Control Group (n = 123) | Experimental Group (n = 137) | p-Value |
|---|---|---|---|
| Age (years) | 12.84 ± 1.02 | 12.74 ± 1.03 | 0.364 |
| Gender (male/female) | 67/56 | 76/61 | 0.437 |
| Weight (kg) | 54.88 ± 12.44 | 55.03 ± 12.06 | 0.921 |
| Height (cm) | 162.76 ± 9.74 | 162.76 ± 9.07 | 0.995 |
| Body mass index (kg·m−2) | 20.60 ± 1.02 | 20.67 ± 1.03 | 0.880 |
| Previous training received (yes/no) | 97/26 | 107/30 | 0.882 |
| CPR action sequence (correct/incorrect) | 123/0 | 137/0 | - |
| AED action sequence (correct/incorrect) | 123/0 | 137/0 | - |
| Post-Training (n = 260) | 6 Months Post-Training (n = 91) | 12 Months Post-Training (n = 169) | |||||
|---|---|---|---|---|---|---|---|
| CG (n = 123) | EG (n = 137) | CG (n = 40) | EG (n = 51) | CG (n = 83) | EG (n = 86) | ||
| Scene security | No | 52 (42.3%) | 42 (30.7%) | 5 (12.5%) | 6 (11.8%) | 8 (9.6%) | 3 (3.5%) |
| Yes | 71 (57.7%) | 95 (69.3%) | 35 (87.5%) | 45 (88.2%) | 75 (90.4%) | 83 (96.5%) | |
| p-value | 0.052 | 0.915 | 0.105 | ||||
| Consciousness assessment | No | 10 (8.2%) | 14 (10.2%) | 1 (2.5%) | 5 (9.8%) | 1 (1.2%) | 5 (5.8%) |
| Yes | 113 (91.8%) | 123 (89.8%) | 39 (97.5%) | 46 (90.2%) | 83/98.8%) | 81 (94.2%) | |
| p-value | 0.561 | 0.163 | 0.105 | ||||
| Breathing assessment (open airway and check breathing) | No | 3 (2.4%) | 4 (2.9%) | 1 (2.5%) | 2 (3.9%) | 2 (2.4%) | 2 (2.3%) |
| Yes | 120 (97.6%) | 133 (97.28%) | 39 (97.5%) | 29 (96.1%) | 81 (97.6%) | 84 (97.7%) | |
| p-value | 0.811 | 0.706 | 0.971 | ||||
| Emergency call | No | 19 (15.4%) | 20 (14.6%) | 4 (10.0%) | 3 (5.9%) | 2 (2.4%) | 9 (10.5%) |
| Yes | 104 (84.6%) | 117 (85.4%) | 36 (90.0%) | 48 (94.1%) | 81 (97.6%) | 77 (89.5%) | |
| p-value | 0.848 | 0.464 | 0.034 | ||||
| Percentage of total compressions | 75–100 | 48 (39.0%) | 57 (41.6%) | 22 (55.0%) | 22 (43.1%) | 40 (48.2%) | 46 (53.5%) |
| Oher | 75 (61.0%) | 80 (58.4%) | 18 (45.06%) | 29 (56.9%) | 43 (51.8%) | 40 (46.5%) | |
| p-value | 0.672 | 0.296 | 0.540 | ||||
| Total compressions in 1 min | 100–120 | 24 (19.5%) | 40 (29.2%) | 12 (30.0%) | 15 (31.4%) | 36 (43.4%) | 32 (37.2%) |
| Other | 99 (80.5%) | 97 (70.8%) | 28 (70.0%) | 35 (68.6%) | 47 (56.6%) | 54 (62.8%) | |
| p-value | 0.070 | 0.888 | 0.436 | ||||
| Hand position during compression | 100% | 36 (29.3%) | 61 (44.5%) | 31 (77.5%) | 33 (64.7%) | 61 (73.5%) | 70 (81.4%) |
| Other | 87 (70.7%) | 76 (55.5%) | 9 (22.5%) | 18 (35.3%) | 22 (26.5%) | 16 (18.6%) | |
| p-value | 0.011 | 0.249 | 0.270 | ||||
| Compression depth | 50–60 mm | 63 (51.2%) | 101 (73.7%) | 24 (60.0%) | 27 (52.9%) | 46 (55.4%) | 56 (65.1%) |
| Other | 60 (48.8%) | 36 (26.3%) | 16 (40.0%) | 24 (47.1%) | 37 (44.6%) | 30 (34.9%) | |
| p-value | <0.001 | 0.530 | 0.212 | ||||
| Compressions with full re-expansion | 100% | 59 (48.0%) | 47 (34.3%) | 20 (50.0%) | 28 (54.9%) | 43 (51.8%) | 39 (45.3%) |
| Other | 64 (52.0%) | 90 (65.7%) | 20 (50.0%) | 23 (45.1%) | 40 (48.2%) | 47 (54.7%) | |
| p-value | 0.025 | 0.677 | 0.443 | ||||
| AED application with effective discharge | No | 7 (5.7%) | 5 (3.6%) | 11 (27.5%) | 11 (21.6%) | 23 (27.7%) | 27 (31.4%) |
| Yes | 116 (94.3%) | 132 (96.4%) | 39 (97.5%) | 50 (98.0%) | 60 (72.3%) | 59 (68.6%) | |
| p-value | 0.313 | 0.623 | 0.617 | ||||
| AED application safely | No | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (3.5%) |
| Yes | 122 (99.2%) | 137 (100%) | 40 (100%) | 51 (100%) | 83 (100%) | 83 (96.5%) | |
| p-value | 0.473 | - | 0.246 | ||||
| AED application without any errors | No | 47 (38.2%) | 41 (29.9%) | 23 (57.5%) | 40 (78.4%) | 62 (74.7%) | 61 (49.6%) |
| Yes | 76 (61.8%) | 96 (70.1%) | 17 (42.5%) | 11 (21.6%) | 21 (25.3%) | 25 (29.1%) | |
| p-value | 0.101 | 0.041 | 0.608 | ||||
| Average time to apply an effective shock | M (SD) | 69.19 (10.83) | 66.15 (7.62) | 57.49 (8.60) | 54.74 (9.19) | 59.08 (12.55) | 59.79 (9.26) |
| p-value | 0.013 | 0.213 | 0.725 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cons-Ferreiro, M.; Mecias-Calvo, M.; Romo-Perez, V.; Navarro-Patón, R. Learning of Basic Life Support through the Flipped Classroom in Secondary Schoolchildren: A Quasi-Experimental Study with 12-Month Follow-Up. Medicina 2023, 59, 1526. https://doi.org/10.3390/medicina59091526
Cons-Ferreiro M, Mecias-Calvo M, Romo-Perez V, Navarro-Patón R. Learning of Basic Life Support through the Flipped Classroom in Secondary Schoolchildren: A Quasi-Experimental Study with 12-Month Follow-Up. Medicina. 2023; 59(9):1526. https://doi.org/10.3390/medicina59091526
Chicago/Turabian StyleCons-Ferreiro, Miguel, Marcos Mecias-Calvo, Vicente Romo-Perez, and Rubén Navarro-Patón. 2023. "Learning of Basic Life Support through the Flipped Classroom in Secondary Schoolchildren: A Quasi-Experimental Study with 12-Month Follow-Up" Medicina 59, no. 9: 1526. https://doi.org/10.3390/medicina59091526
APA StyleCons-Ferreiro, M., Mecias-Calvo, M., Romo-Perez, V., & Navarro-Patón, R. (2023). Learning of Basic Life Support through the Flipped Classroom in Secondary Schoolchildren: A Quasi-Experimental Study with 12-Month Follow-Up. Medicina, 59(9), 1526. https://doi.org/10.3390/medicina59091526









