Influence of Intraoperative Nociception during Hip or Knee Arthroplasty with Supplementary Regional Anaesthesia on Postoperative Pain and Opioid Consumption
Abstract
1. Introduction
2. Materials and Methods
- -
- Relationship between NOL values at skin incision as well as during surgery and postoperative opioid consumption at 24 and 48 h after surgery.
- -
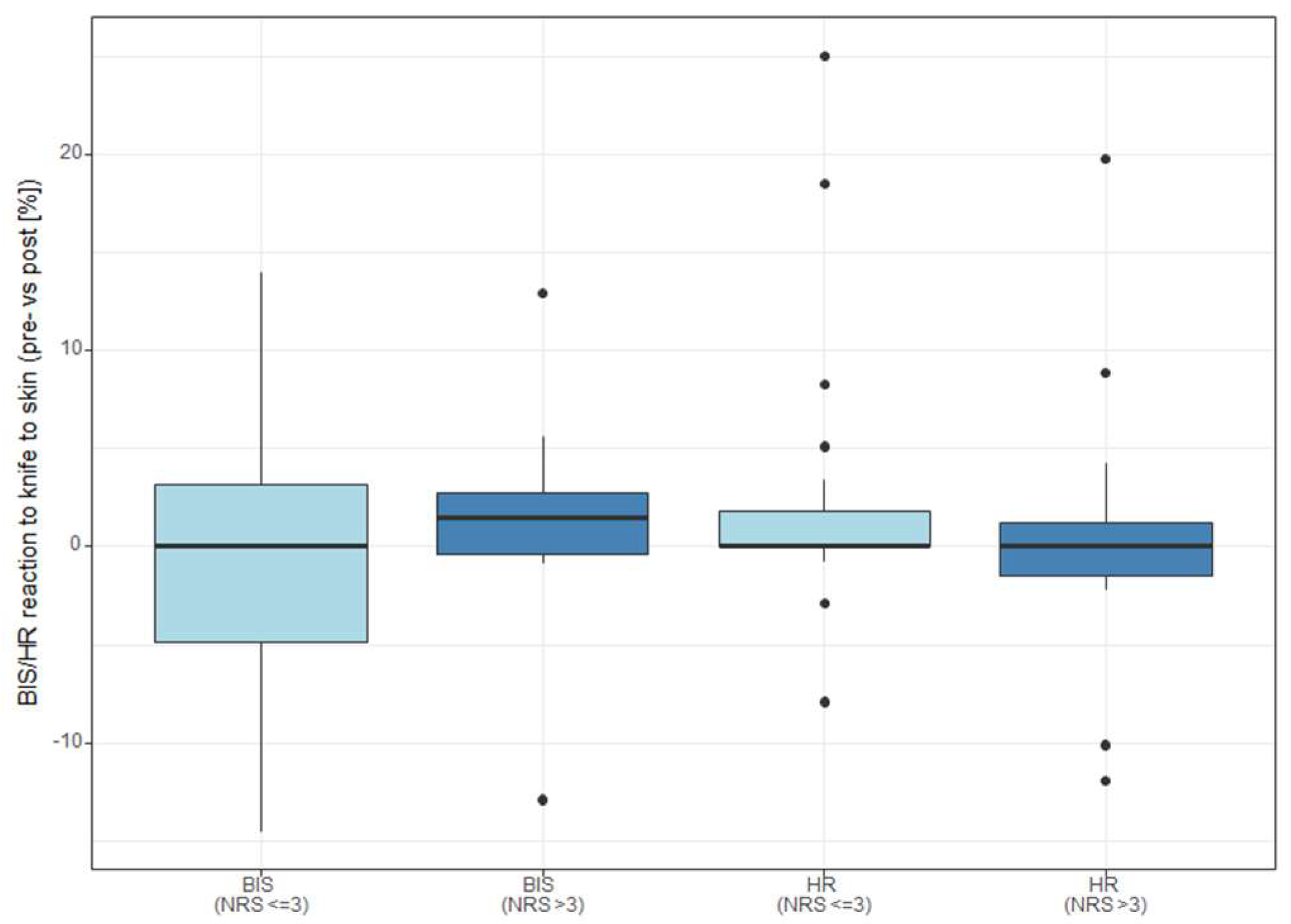
- Relationship between change in secondary parameters (BIS, HR) at skin incision and postoperative pain at 24 and 48 h after surgery.
2.1. Statistical Methods
2.2. Sample Size Calculation
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barrington, J.W.; Halaszynski, T.M.; Sinatra, R.S.; Expert Working Group on Anesthesia and Orthopaedics Critical Issues in Hip and Knee Replacement Arthroplasty. Perioperative pain management in hip and knee replacement surgery. Am. J. Orthop. 2014, 43 (Suppl. S4), S1–S16. [Google Scholar] [PubMed]
- Meijer, F.S.; Niesters, M.; van Velzen, M.; Martini, C.H.; Olofsen, E.; Edry, R.; Sessler, D.I.; van Dorp, E.L.A.; Dahan, A.; Boon, M. Does nociception monitor-guided anesthesia affect opioid consumption? A systematic review of randomized controlled trials. J. Clin. Monit. Comput. 2020, 34, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Beverly, A.; Kaye, A.D.; Ljungqvist, O.; Urman, R.D. Essential Elements of Multimodal Analgesia in Enhanced Recovery After Surgery (ERAS) Guidelines. Anesthesiol. Clin. 2017, 35, e115–e143. [Google Scholar] [CrossRef] [PubMed]
- Benyamin, R.; Trescot, A.M.; Datta, S.; Buenaventura, R.; Adlaka, R.; Sehgal, N.; Glaser, S.E.; Vallejo, R. Opioid complications and side effects. Pain Physician 2008, 11 (Suppl. S2), S105–S120. [Google Scholar] [CrossRef] [PubMed]
- Glasser, J.L.; Patel, S.A.; Li, N.Y.; Patel, R.A.; Daniels, A.H.; Antoci, V. Understanding Health Economics in Joint Replacement Surgery. Orthopedics 2022, 45, e174–e182. [Google Scholar] [CrossRef] [PubMed]
- Statista. Anzahl der Implantationen Künstlicher Kniegelenke in Ausgewählten OECD-Ländern in den Jahren 2011 bis 2015 (je 100.000 Einwohner). Available online: https://de.statista.com/statistik/daten/studie/182672/umfrage/kniegelenksoperationen-anzahl-in-ausgewählten-oecd-ländern/ (accessed on 11 January 2023).
- Wengler, A.; Nimptsch, U.; Mansky, T. Hip and knee replacement in Germany and the USA: Analysis of individual inpatient data from German and US hospitals for the years 2005 to 2011. Dtsch. Arztebl. Int. 2014, 111, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Weißer, M.; Rosery, H.; Schönfelder, T. White Paper on Joint Replacement: Status of Hip and Knee Arthroplasty Care in Germany. In Health Economic Aspects; Bleß, H.-H., Kip, M., Eds.; Springer: Berlin, Germany, 2018. [Google Scholar]
- Piscitelli, P.; Iolascon, G.; Di Tanna, G.; Bizzi, E.; Chitano, G.; Argentiero, A.; Neglia, C.; Giolli, L.; Distante, A.; Gimigliano, R.; et al. Socioeconomic burden of total joint arthroplasty for symptomatic hip and knee osteoarthritis in the Italian population: A 5-year analysis based on hospitalization records. Arthritis Care Res. 2012, 64, 1320–1327. [Google Scholar] [CrossRef] [PubMed]
- Judge, A.; Carr, A.; Price, A.; Garriga-Fuentes, C.; Cooper, C.; Prieto Alhambra, D.; Old, F.; Peat, G.; Murphy, J.; Leal, J.; et al. The Impact of the Enhanced Recovery Pathway and Other Factors on Outcomes and Costs Following Hip and Knee Replacement: Routine Data Study. Health Serv Deliv Res. 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Guerra, M.L.; Singh, P.J.; Taylor, N.F. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: A systematic review. Clin. Rehabil. 2015, 29, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Masaracchio, M.; Hanney, W.J.; Liu, X.; Kolber, M.; Kirker, K. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: A systematic review with meta-analysis. PLoS ONE 2017, 12, e0178295. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, A.J.; Arun Prasad, G.; Chan, V.W.; Brull, R. Does regional anesthesia improve outcome after total knee arthroplasty? Clin. Orthop. Relat. Res. 2009, 467, 2379–2402. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, T.W.; Gill, M.; McDonald, D.A.; Middleton, R.G.; Reed, M.; Sahota, O.; Yates, P. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2019, 91, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Clarke, H.; Soneji, N.; Ko, D.T.; Yun, L.; Wijeysundera, D.N. Rates and risk factors for prolonged opioid use after major surgery: Population based cohort study. BMJ 2014, 348, g1251. [Google Scholar] [CrossRef] [PubMed]
- Nitzschke, R.; Fischer, M.; Funcke, S. Nozizeptionsmonitoring: Methode zur intraoperativen Opioidsteuerung? Anaesthesist 2021, 70, 735–752. [Google Scholar] [CrossRef] [PubMed]
- Bollag, L.; Jelacic, S.; Upegui, C.D.; Wu, C.; Richebe, P. The nociception level index (NOL) response to intubation and incision in patients undergoing video-assisted thoracoscopic surgery (VATS) with and without thoracic epidural analgesia. A pilot study. F1000Research 2018, 7, 875. [Google Scholar] [CrossRef] [PubMed]
- Balan, C.; Tomescu, D.R.; Valeanu, L.; Morosanu, B.; Stanculea, I.; Coman, A.; Stoian, A.; Bubenek-Turconi, S.I. Nociception Level Index-Directed Erector Spinae Plane Block in Open Heart Surgery: A Randomized Controlled Clinical Trial. Medicina 2022, 58, 1462. [Google Scholar] [CrossRef] [PubMed]
- Ledowski, T.; Albus, S.; Stein, J.; MacDonald, B. Skin conductance for monitoring of acute pain in adult postoperative patients: Influence of electrode surface area and sampling time. J. Clin. Monit. Comput. 2011, 25, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Meijer, F.S.; Martini, C.H.; Broens, S.; Boon, M.; Niesters, M.; Aarts, L.; Olofsen, E.; van Velzen, M.; Dahan, A. Nociception-guided versus Standard Care during Remifentanil-Propofol Anesthesia: A Randomized Controlled Trial. Anesthesiology 2019, 130, 745–755. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Mean (SD)/ Median [Range] |
|---|---|
| Age (years) | 68.6 (13.7) |
| Height (m) | 172.3 (10.2) |
| Weight (kg) | 85.7 (19.0) |
| BMI (kg/m2) | 28.9 (6.1) |
| Duration anaesthesia (min) | 220.6 (56.1) |
| Duration surgery (min) | 134.5 (91.4) |
| NRS d1-Rest | 1 [0–7] |
| NRS d1-Movement | 3 [0–8] |
| NRS d2-Rest | 1 [0–8] |
| NRS d2-Movement | 2 [0–8] |
| NRS 0–3 (Median (Quartiles)) (n = 21) | NRS 4–10 (Median (Quartiles)) (n = 14) | p-Value | |
|---|---|---|---|
| NOL post knife to skin | 4.5 (3/24.8) | 16 (3/29) | 0.376 |
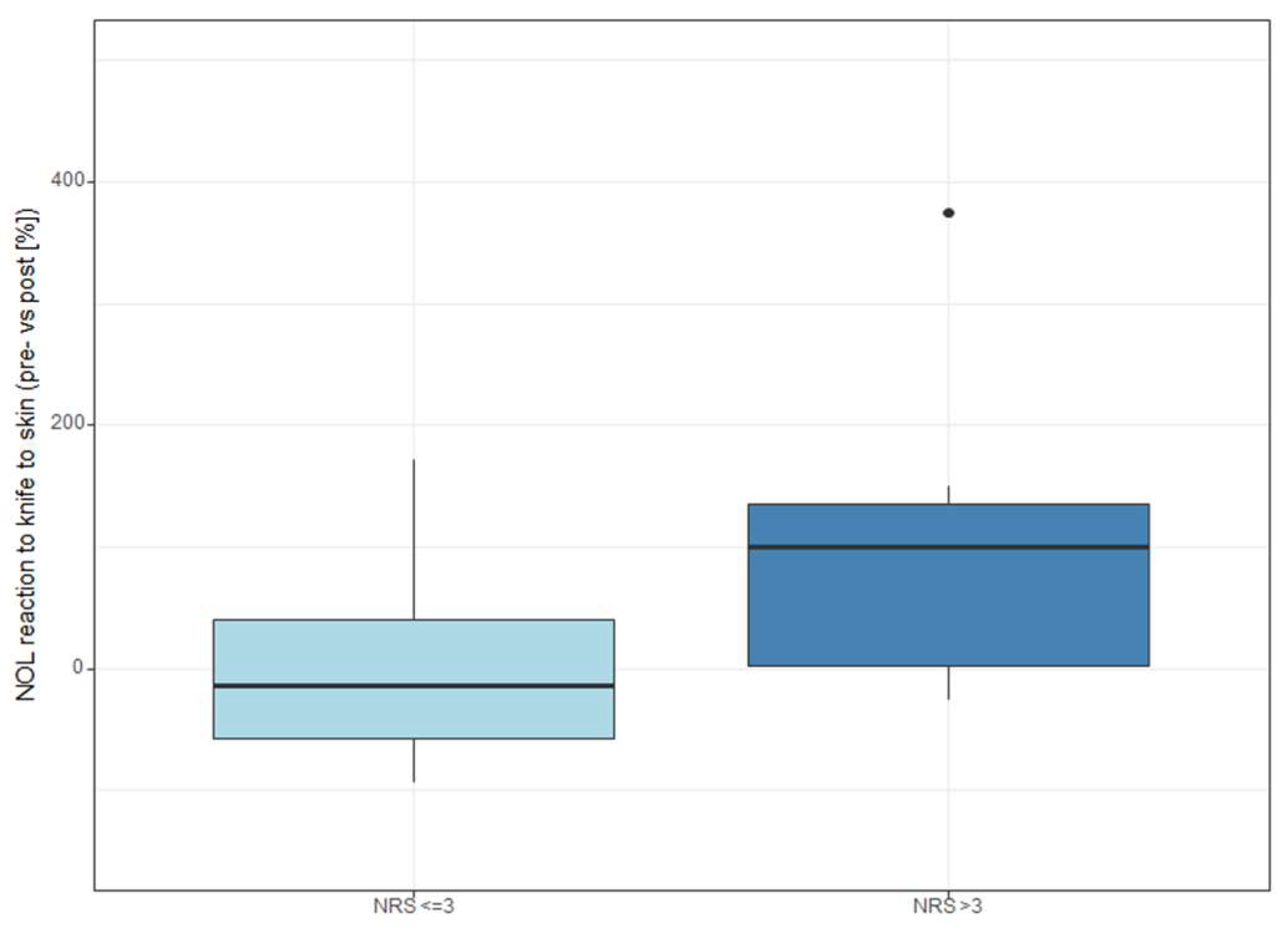
| NOL reaction to knife to skin (pre vs. Post [%]) | −12.3 (−54.6/53.6) | 119 (51.1/262.5) | 0.005 |
| NOL during surgery (median) | 7 (4/15) | 5.5 (3/12) | 0.268 |
| HR post knife to skin | 64 (54/71) | 54 (48.2/62.8) | 0.113 |
| HR reaction to knife to skin (pre vs. Post [%]) | 0 (0/1.8) | 0 (−1.5/1.2) | 0.368 |
| BIS post knife to skin | 43.2 (38.8/51) | 44.1 (39.6/44.5) | 0.533 |
| BIS reaction to knife to skin (pre vs. Post [%]) | 0 (−4.8/3.2) | 1.5 (−0.3/2.7) | 0.682 |
| NOL TWA > 25 | 0.32 (0.2/0.6) | 0.23 (0.2/0.3) | 0.127 |
| NOL TWA > 30 | 0.2 (0.1/0.4) | 0.16 (0.1/0.2) | 0.162 |
| NOL TWA > 35 | 0.13 (0.1/0.3) | 0.09 (0.1/0.1) | 0.162 |
| NOL TWA > 40 | 0.08 (0/0.2) | 0.06 (0/0.1) | 0.175 |
| NOL TWA > 45 | 0.04 (0/0.1) | 0.03 (0/0) | 0.175 |
| NOL TWA < 10 | 0.61 (0.4/0.8) | 0.77 (0.7/1) | 0.055 |
| Surgery type | 8 vs. 13 (knee vs. hip) | 9 vs. 5 (knee vs. hip) | 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neumann, C.; Gehlen, L.; Weinhold, L.; Straßberger-Nerschbach, N.; Soehle, M.; Kornilov, E.; Thudium, M. Influence of Intraoperative Nociception during Hip or Knee Arthroplasty with Supplementary Regional Anaesthesia on Postoperative Pain and Opioid Consumption. Medicina 2023, 59, 1166. https://doi.org/10.3390/medicina59061166
Neumann C, Gehlen L, Weinhold L, Straßberger-Nerschbach N, Soehle M, Kornilov E, Thudium M. Influence of Intraoperative Nociception during Hip or Knee Arthroplasty with Supplementary Regional Anaesthesia on Postoperative Pain and Opioid Consumption. Medicina. 2023; 59(6):1166. https://doi.org/10.3390/medicina59061166
Chicago/Turabian StyleNeumann, Claudia, Lena Gehlen, Leonie Weinhold, Nadine Straßberger-Nerschbach, Martin Soehle, Evgeniya Kornilov, and Marcus Thudium. 2023. "Influence of Intraoperative Nociception during Hip or Knee Arthroplasty with Supplementary Regional Anaesthesia on Postoperative Pain and Opioid Consumption" Medicina 59, no. 6: 1166. https://doi.org/10.3390/medicina59061166
APA StyleNeumann, C., Gehlen, L., Weinhold, L., Straßberger-Nerschbach, N., Soehle, M., Kornilov, E., & Thudium, M. (2023). Influence of Intraoperative Nociception during Hip or Knee Arthroplasty with Supplementary Regional Anaesthesia on Postoperative Pain and Opioid Consumption. Medicina, 59(6), 1166. https://doi.org/10.3390/medicina59061166







