Pre-Trauma Pain Is the Strongest Predictor of Persistent Enhanced Pain Patterns after Severe Trauma: Results of a Single-Centre Retrospective Study
Abstract
1. Introduction
- Chronic pain: Pain that endures beyond the normal healing period or persists for a minimum of three to six months. It may manifest as continuous or intermittent, and its intensity can range from mild to severe [28].
- Post-Traumatic Pain Syndrome (PTPS): A condition characterized by sustained pain that emerges subsequent to a traumatic injury or event. This syndrome often encompasses a combination of physical, psychological, and social factors contributing to the perception of pain [29].
- Complex Regional Pain Syndrome (CRPS): A chronic pain disorder that typically arises after an injury such as a fracture or sprain. It is characterized by enduring severe pain, alterations in skin colour and temperature, swelling, and anomalous hair or nail growth in the affected area [30].
- Neuropathic pain: Pain resulting from damage or dysfunction of the nervous system. It is frequently described as a shooting, burning, or tingling sensation, and may stem from nerve injuries associated with trauma [31].
- Central sensitization: A condition in which the central nervous system becomes hypersensitive to pain signals, intensifying the experience of pain. Central sensitization can manifest following trauma and can induce heightened pain responses even in the absence of ongoing tissue damage [32].
2. Materials and Methods
2.1. Study Design
2.2. Questionnaires
2.2.1. Trauma Outcome Profile
2.2.2. AIS—Abbreviated Injury Scale
2.2.3. ISS—Injury Severity Score
2.3. Patient Sample
2.4. Statistical Analysis
3. Results
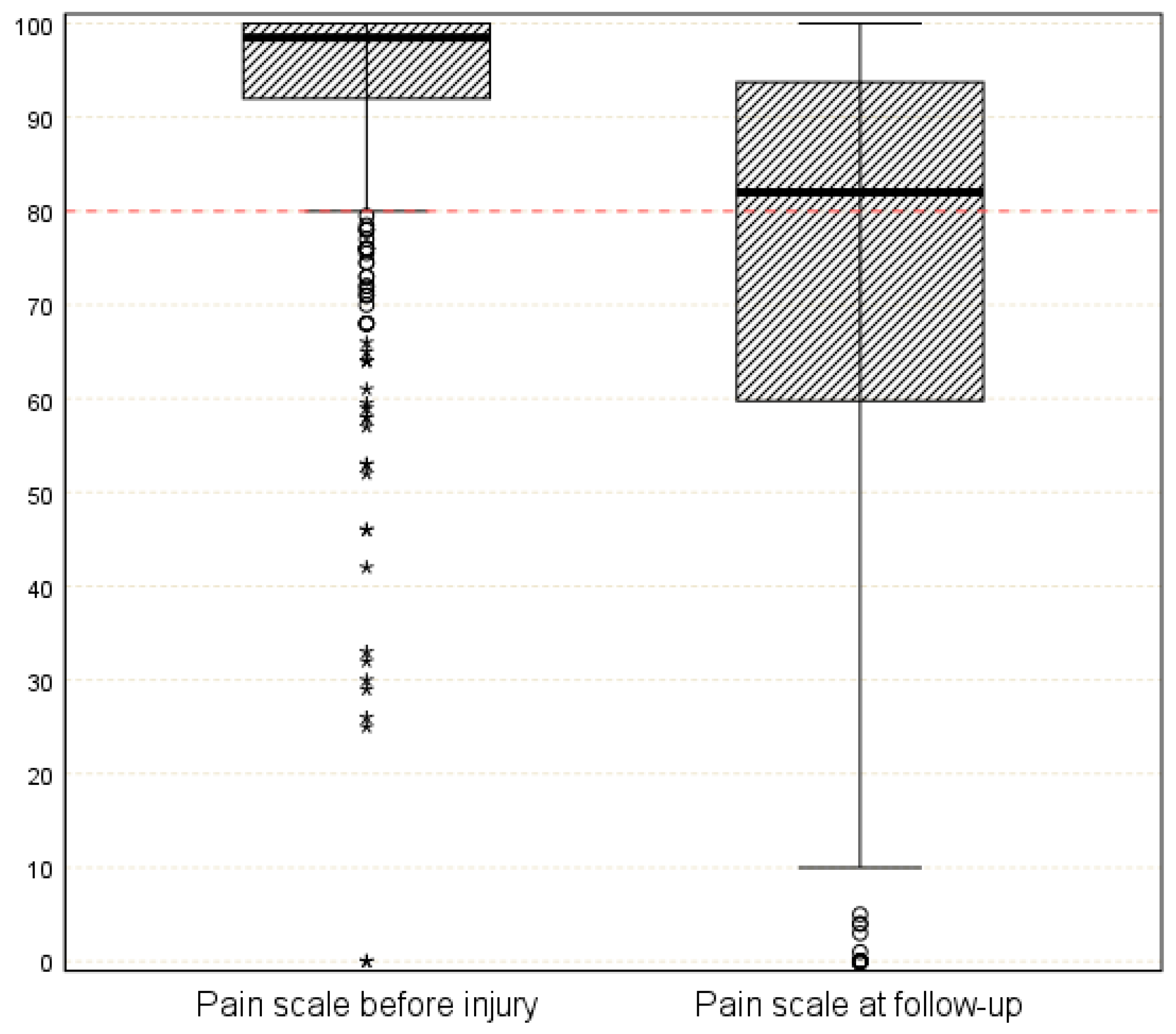
3.1. Trauma Outcome Profile Pain Scale
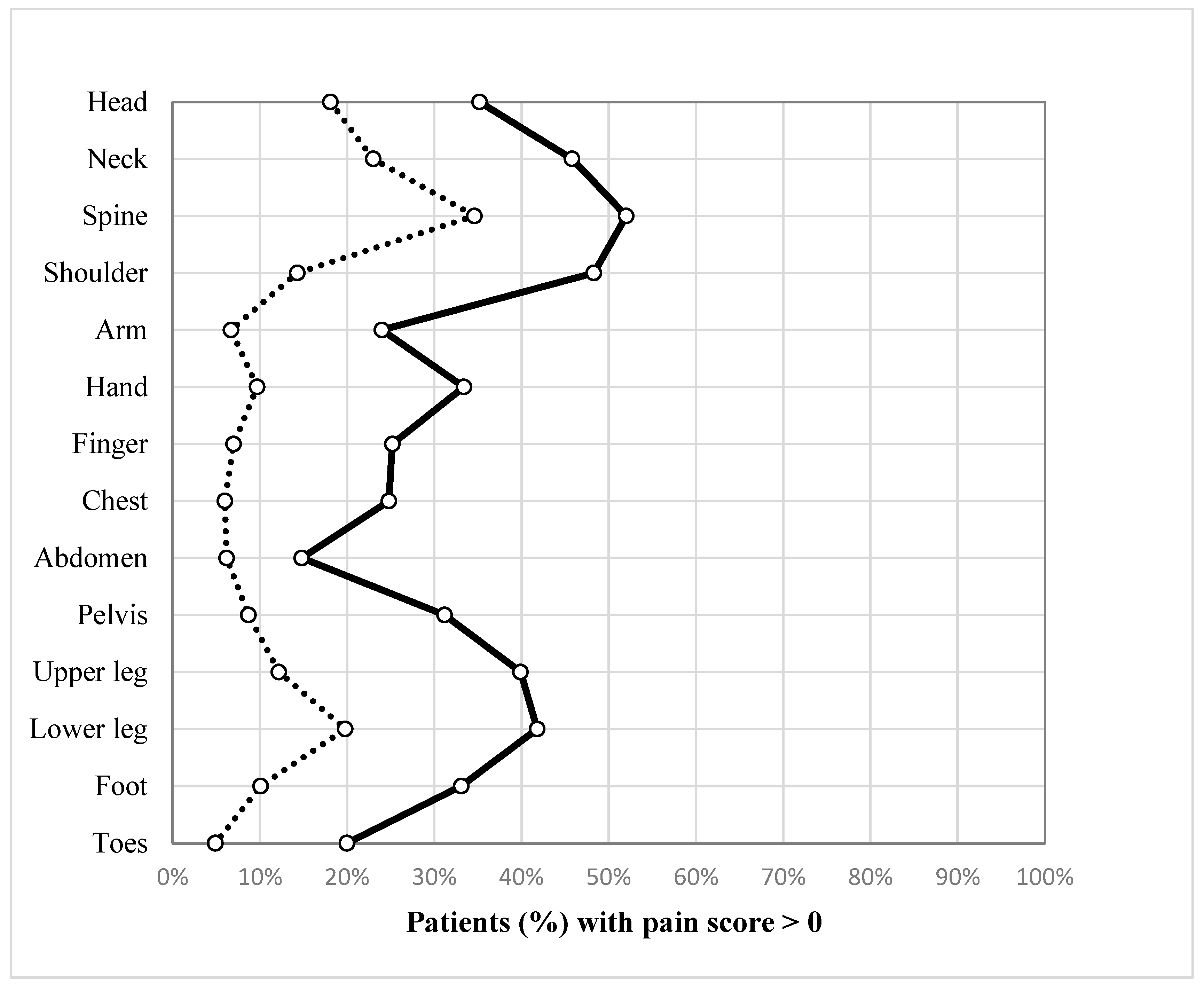
3.2. Pain Pattern before and after Trauma
3.3. Injury Severity and Pain
3.4. Predictors of Persistent Pain: Regression Analysis
4. Discussion
4.1. Pain before Trauma Is a Strong Predictor for Persistent Enhanced Pain
4.2. Body Areas of the Neck, Spine, Shoulder, Pelvis, Hip, Knee, and Feet
4.3. Even Minor Injuries (AIS = 1) Lead to Increased Pain Scores after an Accident
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krug, E.G.; Sharma, G.K.; Lozano, R. The Global Burden of Injuries. Am. J. Public Health 2000, 90, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Anke, A.G.; Stanghelle, J.K.; Finset, A.; Roaldsen, K.S.; Pillgram-Larsen, J.; Fugl-Meyer, A.R. Long-Term Prevalence of Impairments and Disabilities after Multiple Trauma. J. Trauma 1997, 42, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic Pain: A Review of Its Epidemiology and Associated Factors in Population-Based Studies. BJA Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef] [PubMed]
- van der Vlegel, M.; Haagsma, J.A.; Havermans, R.J.M.; de Munter, L.; de Jongh, M.A.C.; Polinder, S. Long-Term Medical and Productivity Costs of Severe Trauma: Results from a Prospective Cohort Study. PLoS ONE 2021, 16, e0252673. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.W.; Kellermann, A.; McGuire, L.C.; Chen, B.; Popovic, T. CDC Grand Rounds: Reducing Severe Traumatic Brain Injury in the United States. Morb. Mortal. Wkly. Rep. 2013, 62, 549–552. [Google Scholar]
- Kaske, S.; Lefering, R.; Trentzsch, H.; Driessen, A.; Bouillon, B.; Maegele, M.; Probst, C. Quality of Life Two Years after Severe Trauma: A Single Centre Evaluation. Injury 2014, 45, S100–S105. [Google Scholar] [CrossRef]
- Lotfalla, A.; Halm, J.; Schepers, T.; Giannakópoulos, G. Health-Related Quality of Life after Severe Trauma and Available PROMS: An Updated Review (Part I). Eur. J. Trauma Emerg. Surg. 2022, 49, 747–761. [Google Scholar] [CrossRef]
- Vardon-Bounes, F.; Gracia, R.; Abaziou, T.; Crognier, L.; Seguin, T.; Labaste, F.; Geeraerts, T.; Georges, B.; Conil, J.-M.; Minville, V. A Study of Patients’ Quality of Life More than 5 Years after Trauma: A Prospective Follow-Up. Health Qual. Life Outcomes 2021, 19, 18. [Google Scholar] [CrossRef]
- Zwingmann, J.; Hagelschuer, P.; Langenmair, E.; Bode, G.; Herget, G.; Südkamp, N.P.; Hammer, T. Lower Health-Related Quality of Life in Polytrauma Patients. Medicine 2016, 95, e3515. [Google Scholar] [CrossRef]
- Keene, D.D.; Rea, W.E.; Aldington, D. Acute Pain Management in Trauma. Trauma 2011, 13, 167–179. [Google Scholar] [CrossRef]
- Dueñas, M.; Ojeda, B.; Salazar, A.; Mico, J.A.; Failde, I. A Review of Chronic Pain Impact on Patients, Their Social Environment and the Health Care System. J. Pain Res. 2016, 9, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Dydyk, A.M.; Conermann, T. Chronic Pain. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Sheng, J.; Liu, S.; Wang, Y.; Cui, R.; Zhang, X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast. 2017, 2017, 9724371. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, A.; Bazargan-Hejazi, S.; Heidari Zadie, Z.; Euasobhon, P.; Ketumarn, P.; Karbasfrushan, A.; Amini-Saman, J.; Mohammadi, R. Pain Management in Trauma: A Review Study. J. Inj. Violence Res. 2016, 8, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Saranteas, T.; Kostroglou, A.; Anagnostopoulos, D.; Giannoulis, D.; Vasiliou, P.; Mavrogenis, A.F. Pain Is Vital in Resuscitation in Trauma. SICOT-J 2019, 5, 28. [Google Scholar] [CrossRef]
- Scholten, A.C.; Berben, S.A.A.; Westmaas, A.H.; van Grunsven, P.M.; de Vaal, E.T.; Rood, P.P.M.; Hoogerwerf, N.; Doggen, C.J.M.; Schoonhoven, L. Pain Management in Trauma Patients in (Pre)Hospital Based Emergency Care: Current Practice versus New Guideline. Injury 2015, 46, 798–806. [Google Scholar] [CrossRef]
- Becker, W.C.; Dorflinger, L.; Edmond, S.N.; Islam, L.; Heapy, A.A.; Fraenkel, L. Barriers and Facilitators to Use of Non-Pharmacological Treatments in Chronic Pain. BMC Fam. Pract. 2017, 18, 41. [Google Scholar] [CrossRef]
- Shafeeq, H.; DiGiacomo, J.C.; Sookraj, K.A.; Gerber, N.; Bahr, A.; Talreja, O.N.; Munnangi, S.; Cardozo-Stolberg, S.; Angus, L.D.G. Perioperative Multimodal Pain Management Approach in Older Adults With Polytrauma. J. Surg. Res. 2022, 275, 96–102. [Google Scholar] [CrossRef]
- Castillo, R.C.; MacKenzie, E.J.; Wegener, S.T.; Bosse, M.J.; Group, L.S. Prevalence of Chronic Pain Seven Years Following Limb Threatening Lower Extremity Trauma. Pain 2006, 124, 321–329. [Google Scholar] [CrossRef]
- Åkerblom, S.; Larsson, J.; Malmström, E.-M.; Persson, E.; Westergren, H. Acceptance: A Factor to Consider in Persistent Pain after Neck Trauma. Scand. J. Pain 2019, 19, 733–741. [Google Scholar] [CrossRef]
- Kaske, S.; Tjardes, T.; Lefering, R.; Bouillon, B.; Maegele, M. Frequency of Relevant Back Pain Two Years after Trauma and the Effect on Health-Related Quality of Life. J. Back Musculoskelet. Rehabil. 2022, 36, 377–385. [Google Scholar] [CrossRef]
- Ohanisian, L.; Brown, N.; White, S.D.; Rubay, D.; Schwartz, P.M. Persistent Shoulder Pain Due to a Suprascapular Nerve Injury in the Setting of Trauma. Cureus 2019, 11, e4224. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, E.J.; Bosse, M.J.; Kellam, J.F.; Pollak, A.N.; Webb, L.X.; Swiontkowski, M.F.; Smith, D.G.; Sanders, R.W.; Jones, A.L.; Starr, A.J. Early Predictors of Long-Term Work Disability after Major Limb Trauma. J. Trauma Acute Care Surg. 2006, 61, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Westergren, H.; Larsson, J.; Freeman, M.; Carlsson, A.; Jöud, A.; Malmström, E.-M. Sex-Based Differences in Pain Distribution in a Cohort of Patients with Persistent Post-Traumatic Neck Pain. Disabil. Rehabil. 2018, 40, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.P.; Brier, Z.M.; Price, M. The Association between Pain Trajectories with PTSD, Depression, and Disability During the Acute Post Trauma Period. Psychosom. Med. 2020, 82, 862. [Google Scholar] [CrossRef]
- Reddi, D.; Curran, N. Chronic Pain after Surgery: Pathophysiology, Risk Factors and Prevention. Postgrad. Med. J. 2014, 90, 222–227. [Google Scholar] [CrossRef]
- Rosenbloom, B.N.; Khan, S.; McCartney, C.; Katz, J. Systematic Review of Persistent Pain and Psychological Outcomes Following Traumatic Musculoskeletal Injury. J. Pain Res. 2013, 6, 39–51. [Google Scholar] [CrossRef]
- Chapman, C.R.; Vierck, C.J. The Transition of Acute Postoperative Pain to Chronic Pain: An Integrative Overview of Research on Mechanisms. J. Pain 2017, 18, 359.e1–359.e38. [Google Scholar] [CrossRef]
- Edwards, R.R.; Dworkin, R.H.; Sullivan, M.D.; Turk, D.C.; Wasan, A.D. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. J. Pain 2016, 17, T70–T92. [Google Scholar] [CrossRef]
- Taylor, S.-S.; Noor, N.; Urits, I.; Paladini, A.; Sadhu, M.S.; Gibb, C.; Carlson, T.; Myrcik, D.; Varrassi, G.; Viswanath, O. Complex Regional Pain Syndrome: A Comprehensive Review. Pain Ther. 2021, 10, 875–892. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Kuner, R.; Jensen, T.S. Neuropathic Pain: From Mechanisms to Treatment. Physiol. Rev. 2021, 101, 259–301. [Google Scholar] [CrossRef]
- Nijs, J.; George, S.Z.; Clauw, D.J.; Fernández-de-las-Peñas, C.; Kosek, E.; Ickmans, K.; Fernández-Carnero, J.; Polli, A.; Kapreli, E.; Huysmans, E.; et al. Central Sensitisation in Chronic Pain Conditions: Latest Discoveries and Their Potential for Precision Medicine. Lancet Rheumatol. 2021, 3, e383–e392. [Google Scholar] [CrossRef]
- Macrae, W.A. Chronic Post-Surgical Pain: 10 Years On. Br. J. Anaesth. 2008, 101, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Macrae, W.A.; Davies, H.T.O. Epidemiology of Pain. In Core Topics in Pain; Cambridge University Press: Cambridge, UK, 1999; p. 99. [Google Scholar]
- El-Tallawy, S.N.; Nalamasu, R.; Salem, G.I.; LeQuang, J.A.K.; Pergolizzi, J.V.; Christo, P.J. Management of Musculoskeletal Pain: An Update with Emphasis on Chronic Musculoskeletal Pain. Pain Ther. 2021, 10, 181–209. [Google Scholar] [CrossRef]
- MacKay, C.; Jaglal, S.B.; Sale, J.; Badley, E.M.; Davis, A.M. A Qualitative Study of the Consequences of Knee Symptoms: ‘It’s like You’re an Athlete and You Go to a Couch Potato. BMJ Open 2014, 4, e006006. [Google Scholar] [CrossRef] [PubMed]
- Haack, M.; Simpson, N.; Sethna, N.; Kaur, S.; Mullington, J. Sleep Deficiency and Chronic Pain: Potential Underlying Mechanisms and Clinical Implications. Neuropsychopharmacology 2020, 45, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Clay, F.J.; Watson, W.L.; Newstead, S.V.; McClure, R.J. A Systematic Review of Early Prognostic Factors for Persistent Pain Following Acute Orthopedic Trauma. Pain Res. Manag. 2012, 17, 35–44. [Google Scholar] [CrossRef]
- Alkassabi, O.; Voogt, L.; Andrews, P.; Alhowimel, A.; Nijs, J.; Alsobayel, H. Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review. Int. J. Environ. Res. Public. Health 2022, 19, 9318. [Google Scholar] [CrossRef] [PubMed]
- Velmahos, C.S.; Herrera-Escobar, J.P.; Al Rafai, S.S.; Fat, S.C.; Kaafarani, H.; Nehra, D.; Kasotakis, G.; Salim, A.; Haider, A.H. It Still Hurts! Persistent Pain and Use of Pain Medication One Year after Injury. Am. J. Surg. 2019, 218, 864–868. [Google Scholar] [CrossRef] [PubMed]
- Busse, J.W.; Heels-Ansdell, D.; Makosso-Kallyth, S.; Petrisor, B.; Jeray, K.; Tufescu, T.; Laflamme, Y.; McKay, P.; McCabe, R.E.; Le Manach, Y. Patient Coping and Expectations Predict Recovery after Major Orthopaedic Trauma. Br. J. Anaesth. 2019, 122, 51–59. [Google Scholar] [CrossRef]
- Pozzato, I.; Craig, A.; Gopinath, B.; Kifley, A.; Tran, Y.; Jagnoor, J.; Cameron, I.D. Outcomes after Traffic Injury: Mental Health Comorbidity and Relationship with Pain Interference. BMC Psychiatry 2020, 20, 189. [Google Scholar] [CrossRef]
- Lefering, R.; Tecic, T.; Schmidt, Y.; Pirente, N.; Bouillon, B.; Neugebauer, E.; Group, P.C.S. Quality of Life after Multiple Trauma: Validation and Population Norm of the Polytrauma Outcome (POLO) Chart. Eur. J. Trauma Emerg. Surg. 2012, 38, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Pirente, N.; Ottlik, Y.; Lefering, R.; Boullion, B.; Neugebauer, E.; Working Group “Polytrauma” of the DGU*. “Polytrauma” of the Quality of Life in Multiply Injured Patients: Development of the Trauma Outcome Profile (TOP) as Part of the Modular Polytrauma Outcome (POLO) Chart. Eur. J. Trauma 2006, 32, 44–62. [Google Scholar] [CrossRef]
- Haasper, C.; Junge, M.; Ernstberger, A.; Brehme, H.; Hannawald, L.; Langer, C.; Nehmzow, J.; Otte, D.; Sander, U.; Krettek, C. The Abbreviated Injury Scale (AIS) Options and Problems in Application. Unfallchirurg 2010, 113, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Linn, S. The Injury Severity Score—Importance and Uses. Ann. Epidemiol. 1995, 5, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, M.; Segui-Gomez, M.; Lescohier, I.; Di Scala, C.; McDonald-Smith, G. An Overview of the Injury Severity Score and the New Injury Severity Score. Inj. Prev. 2001, 7, 10–13. [Google Scholar] [CrossRef]
- Williamson, O.D.; Epi, G.D.C.; Gabbe, B.J.; Physio, B.; Cameron, P.A.; Edwards, E.R.; Richardson, M.D.; Group, V.O.T.O.R.P. Predictors of Moderate or Severe Pain 6 Months after Orthopaedic Injury: A Prospective Cohort Study. J. Orthop. Trauma 2009, 23, 139–144. [Google Scholar] [CrossRef]
- Holmes, A.; Williamson, O.; Hogg, M.; Arnold, C.; Prosser, A.; Clements, J.; Konstantatos, A.; O’Donnell, M. Predictors of Pain 12 Months after Serious Injury. Pain Med. 2010, 11, 1599–1611. [Google Scholar] [CrossRef]
- Rivara, F.P.; MacKenzie, E.J.; Jurkovich, G.J.; Nathens, A.B.; Wang, J.; Scharfstein, D.O. Prevalence of Pain in Patients 1 Year after Major Trauma. Arch. Surg. 2008, 143, 282–287. [Google Scholar] [CrossRef]
- Hoffman, J.M.; Pagulayan, K.F.; Zawaideh, N.; Dikmen, S.; Temkin, N.; Bell, K.R. Understanding Pain after Traumatic Brain Injury: Impact on Community Participation. Am. J. Phys. Med. Rehabil. 2007, 86, 962–969. [Google Scholar] [CrossRef]
- Hours, M.; Bernard, M.; Charnay, P.; Chossegros, L.; Javouhey, E.; Fort, E.; Boisson, D.; Sancho, P.-O.; Laumon, B. Functional Outcome after Road-Crash Injury: Description of the ESPARR Victims Cohort and 6-Month Follow-up Results. Accid. Anal. Prev. 2010, 42, 412–421. [Google Scholar] [CrossRef]
- Holtslag, H.R.; van Beeck, E.F.; Lindeman, E.; Leenen, L.P. Determinants of Long-Term Functional Consequences after Major Trauma. J. Trauma Acute Care Surg. 2007, 62, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Airosa, F.; Arman, M.; Sundberg, T.; Öhlén, G.; Falkenberg, T. Caring Touch as a Bodily Anchor for Patients after Sustaining a Motor Vehicle Accident with Minor or No Physical Injuries-a Mixed Methods Study. BMC Complement. Altern. Med. 2016, 16, 106. [Google Scholar] [CrossRef] [PubMed]
- Rosberg, H.-E.; Carlsson, K.S.; Dahlin, L.B. Prospective Study of Patients with Injuries to the Hand and Forearm: Costs, Function, and General Health. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2005, 39, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Kasch, H.; Qerama, E.; Bach, F.W.; Jensen, T.S. Reduced Cold Pressor Pain Tolerance in Non-Recovered Whiplash Patients: A 1-Year Prospective Study. Eur. J. Pain 2005, 9, 561–569. [Google Scholar] [CrossRef]
- Archer, K.R.; Abraham, C.M.; Obremskey, W.T. Psychosocial Factors Predict Pain and Physical Health after Lower Extremity Trauma. Clin. Orthop. Relat. Res. 2015, 473, 3519–3526. [Google Scholar] [CrossRef]
- Haagsma, J.A.; Polinder, S.; Olff, M.; Toet, H.; Bonsel, G.J.; van Beeck, E.F. Posttraumatic Stress Symptoms and Health-Related Quality of Life: A Two Year Follow up Study of Injury Treated at the Emergency Department. BMC Psychiatry 2012, 12, 1. [Google Scholar] [CrossRef]
| Injury Severity | ||||||
|---|---|---|---|---|---|---|
| Injured Body Region | Prevalence | Not Injured | AIS 1 | AIS 2 | AIS 3 | AIS 4+ |
| Head | 311 (52%) | 1.0 | 1.2 | 1.5 | 1.7 | 2.7 |
| Spinal cord | 204 (34%) | 1.9 | -/- | 3.1 | 3.1 | 3.6 |
| Thorax | 276 (46%) | 0.5 | 0.9 | 1.0 | 1.5 | 1.7 |
| Abdomen | 116 (19%) | 0.4 | -/- | 1.0 | 1.2 | 1.5 |
| Upper extremity | 248 (42%) | 2.1 | 2.6 | 3.7 | 4.1 | -/- |
| Pelvis | 98 (17%) | 1.0 | -/- | 2.2 | 3.1 | 3.6 |
| Lower extremity | 226 (38%) | 2.2 | 2.3 | 4.7 | 5.0 | -/- |
| Predictor | n | Odds Ratio (OR) | 95% CI for OR | p-Value |
|---|---|---|---|---|
| Age (reference: <30 years) | 122 | --- | --- | 0.003 |
| 30–64 years | 356 | 2.09 | 1.33–3.27 | 0.001 |
| 65 and older | 118 | 1.33 | 0.76–2.34 | 0.32 |
| Females | 168 | 1.08 | 0.73–1.59 | 0.70 |
| Relevant pain before the accident | 51 | 5.43 | 2.60–11.34 | <0.001 |
| ISS 16+ | 312 | 1.80 | 1.20–2.69 | 0.004 |
| Head injury | 334 | 0.82 | 0.57–1.18 | 0.29 |
| Thoracic injury | 276 | 0.70 | 0.47–1.05 | 0.082 |
| Injury of the abdomen | 116 | 1.09 | 0.68–1.76 | 0.72 |
| Injury of spinal cord | 204 | 1.12 | 0.77–1.63 | 0.55 |
| Injury of upper extremity | 248 | 1.22 | 0.85–1.74 | 0.28 |
| Injury of lower extremity | 226 | 1.26 | 0.88–1.82 | 0.21 |
| Pelvic injury | 98 | 1.96 | 1.20–3.21 | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fetz, K.; Lefering, R.; Kaske, S. Pre-Trauma Pain Is the Strongest Predictor of Persistent Enhanced Pain Patterns after Severe Trauma: Results of a Single-Centre Retrospective Study. Medicina 2023, 59, 1327. https://doi.org/10.3390/medicina59071327
Fetz K, Lefering R, Kaske S. Pre-Trauma Pain Is the Strongest Predictor of Persistent Enhanced Pain Patterns after Severe Trauma: Results of a Single-Centre Retrospective Study. Medicina. 2023; 59(7):1327. https://doi.org/10.3390/medicina59071327
Chicago/Turabian StyleFetz, Katharina, Rolf Lefering, and Sigune Kaske. 2023. "Pre-Trauma Pain Is the Strongest Predictor of Persistent Enhanced Pain Patterns after Severe Trauma: Results of a Single-Centre Retrospective Study" Medicina 59, no. 7: 1327. https://doi.org/10.3390/medicina59071327
APA StyleFetz, K., Lefering, R., & Kaske, S. (2023). Pre-Trauma Pain Is the Strongest Predictor of Persistent Enhanced Pain Patterns after Severe Trauma: Results of a Single-Centre Retrospective Study. Medicina, 59(7), 1327. https://doi.org/10.3390/medicina59071327






