Longitudinal Study of Bone Height Change between Two Approaches for Sinus Floor Elevation
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Operative Technique
2.2.1. The Crestal Approach
2.2.2. The Lateral Approach
2.3. Bone Augmentation Materials
2.4. Postoperative Care
2.5. Radiographic Analysis
2.6. Statistical Analysis
3. Results
3.1. Crestal and Lateral Approach Sinus Augmentation
3.2. Native Bone Height
3.3. Follow-Up Period
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bahat, O.; Fontancsi, R.V.; Preston, J. Reconstruction of the hard and soft tissue for optimal placement of osseointegrated im-plants. Int. J. Periodont. Rest. Dent. 1993, 13, 255–275. [Google Scholar]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Hirsch, J.-M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants, (II). Etiopathogenesis. Eur. J. Oral Sci. 1998, 106, 721–764. [Google Scholar] [CrossRef]
- Bryant, S.R. The effects of age, jaw site, and bone condition on oral implant outcomes. Int. J. Prosthodont. 1998, 11, 470–490. [Google Scholar]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinusfloor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar]
- Chanavaz, M. Maxillary sinus: Anatomy, physiology, surgery, and bone grafting related to implantology—Eleven years of surgical experience (1979–1990). J. Oral Implantol. 1990, 16, 199–209. [Google Scholar] [PubMed]
- Grag, A.K. Augmentation grafting of the maxillary sinus for placements of dental implants: Anatomy, physiology, and proce-dures. Implant. Dent. 1999, 8, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152–154. [Google Scholar] [PubMed]
- Tatum, H., Jr. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef]
- Misch, C.E. Maxillary sinus augmentation for endosteal implants: Organized alternative treatment plans. Int. J. Oral Implantol. 1987, 4, 49–58. [Google Scholar]
- Kim, S.M.; Park, J.W.; Suh, J.Y.; Sohn, D.S.; Lee, J.M. Bone-added osteotome technique versus lateral approach for sinus floor elevation: A comparative radiographic study. Implant. Dent. 2011, 20, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Hatano, N.; Shimizu, Y.; Ooya, K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin. Oral Implant. Res. 2004, 15, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Geurs, N.C.; Wang, I.C.; Shulman, L.B.; Jeffcoat, M.K. Retrospective radiographic analysis of sinus graft and implant placement proce-dures from the Academy of Osseointegration Consensus Conference on Sinus Grafts. Int. J. Periodont. Restor. Dent. 2001, 21, 517–523. [Google Scholar]
- Nampo, T.; Watahiki, J.; Enomoto, A.; Taguchi, T.; Ono, M.; Nakano, H.; Yamamoto, G.; Irie, T.; Tachikawa, T.; Maki, K. A New Method for Alveolar Bone Repair Using Extracted Teeth for the Graft Material. J. Periodontol. 2010, 81, 1264–1272. [Google Scholar] [CrossRef]
- Jensen, O.T.; Shulman, L.B.; Block, M.S.; Iacono, V.J. Report of the Sinus Consensus Conference of 1996. Int. J. Oral Maxillofac. Implant. 1998, 13, 11–45. [Google Scholar]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Misch, C.E.; Perel, M.L.; Wang, H.L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; et al. Implant success, survival, and failure: The International Congress of Oral Implantolo-gists (ICOI) Pisa Consensus Conference. Implant. Dent. 2008, 17, 5–15. [Google Scholar] [CrossRef]
- Cochran, D.L.; Nummikoski, P.V.; Schoolfield, J.D.; Jones, A.A.; Oates, T.W. A Prospective Multicenter 5-Year Radiographic Evaluation of Crestal Bone Levels Over Time in 596 Dental Implants Placed in 192 Patients. J. Periodontol. 2009, 80, 725–733. [Google Scholar] [CrossRef]
- Petrikowski, C.; Pharoah, M.; Schmitt, A. Presurgical radiographic assessment for implants. J. Prosthet. Dent. 1989, 61, 59–64. [Google Scholar] [CrossRef]
- Rosen, P.S.; Summers, R.; Mellado, J.R.; Salkin, L.M.; Shanaman, R.H.; Marks, M.H.; Fugazzotto, P.A. The bone-added osteotome sinus floor elevation technique: Multicenter retrospective report of consecutively treated patients. Int. J. Oral Maxillofac. Implant. 1999, 14, 853–858. [Google Scholar]
- Asai, S.; Shimizu, Y.; Ooya, K. Maxillary sinus augmentation model in rabbits: Effect of occluded nasal ostium on new bone formation. Clin. Oral Implant. Res. 2002, 13, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Oh, T.J.; Yoon, J.; Misch, C.E.; Wang, H.-L. The causes of early implant bone loss: Myth or science? J. Periodontol. 2002, 73, 322–333. [Google Scholar] [CrossRef] [PubMed]
- Jensen, O.T. Vital biomechanics of bone and bone grafts. In The Sinus Bone Graft, 2nd ed.; Jensen, O.T., Ed.; Quintessence: Seoul, Republic of Korea, 2006; Volume 3, pp. 30–31. [Google Scholar]
- Ostman, P.-O.; Hellman, M.; Sennerby, L. Direct Implant Loading in the Edentulous Maxilla Using a Bone Density–Adapted Surgical Protocol and Primary Implant Stability Criteria for Inclusion. Clin. Implant. Dent. Relat. Res. 2005, 7 (Suppl. S1), s60–s69. [Google Scholar] [CrossRef]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontol. 2000 2008, 47, 51–56. [Google Scholar] [CrossRef]
- Bornstein, M.M.; Hart, C.N.; Halbritter, S.A.; Morton, D.; Buser, D. Early loading of nonsubmerged titanium implants with a chemically modified sand-blasted and acid-etched surface: 6-month results of a prospective case series study in the posterior mandible focusing on peri-implant crestal bone changes and implant stability quotient (ISQ) values. Clin. Implant. Dent. Relat. Res. 2009, 11, 338–347. [Google Scholar]
- Balleri, P.; Cozzolino, A.; Ghelli, L.; Momicchioli, G.; Varriale, A. Stability measurements of osseointegrated implants using Osstell in partially edentulous jaws after 1 year of loading: A pilot study. Clin. Implant. Dent. Relat. Res. 2002, 4, 128–132. [Google Scholar] [CrossRef]
- Patel, S.; Lee, D.; Shiffler, K.; Aghaloo, T.; Moy, P.; Pi-Anfruns, J. Resonance Frequency Analysis of Sinus Augmentation by Osteotome Sinus Floor Elevation and Lateral Window Technique. J. Oral Maxillofac. Surg. 2015, 73, 1920–1925. [Google Scholar] [CrossRef]
- Beretta, M.; Poli, P.; Grossi, G.B.; Pieroni, S.; Maiorana, C. Long-term survival rate of implants placed in conjunction with 246 sinus floor elevation procedures: Results of a 15-year retrospective study. J. Dent. 2015, 43, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Schärer, P. Sinus elevation procedures in the resorbed posterior maxilla: Comparison of the crestal and lateral approaches. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 8–17. [Google Scholar] [CrossRef]
- Hsu, Y.; Rosen, P.S.; Choksi, K.; Shih, M.; Ninneman, S.; Lee, C. Complications of sinus floor elevation procedure and management strategies: A systematic review. Clin. Implant. Dent. Relat. Res. 2022, 24, 740–765. [Google Scholar] [CrossRef]
- Barbu, H.M.; Andreescu, C.F.; Comaneanu, M.R.; Referendaru, D.; Mijiritsky, E. Maxillary Sinus Floor Augmentation to Enable One-Stage Implant Placement by Using Bovine Bone Substitute and Platelet-Rich Fibrin. BioMed Res. Int. 2018, 2018, 6562958. [Google Scholar] [CrossRef] [PubMed]
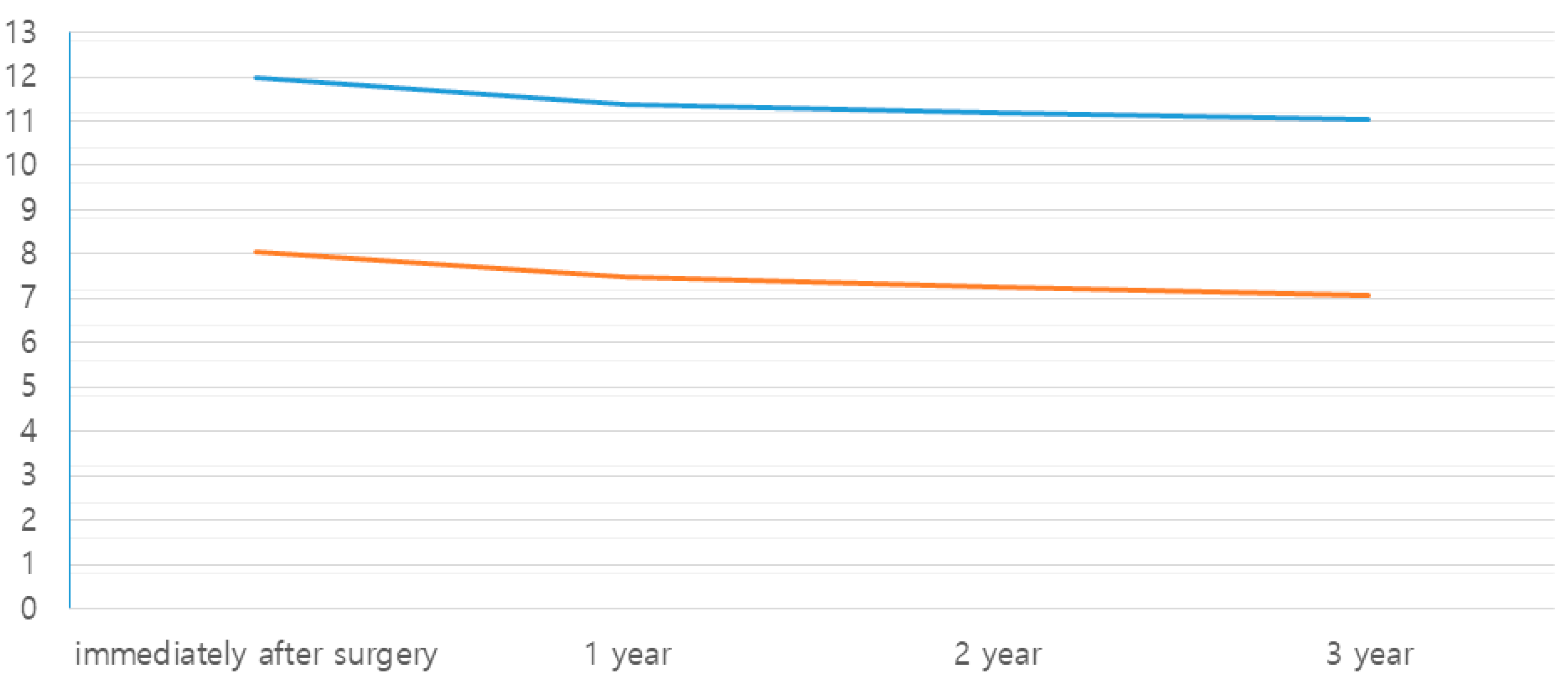
| Mean Native Bone Height (mm) | No. of Implants | Gain in Bone Height (mm) | Change in the Grafted Bone Height (mm) | |||
|---|---|---|---|---|---|---|
| 1 year | 2 year | 3 year | ||||
| Crestal | 6.55 | 40 | 8.07 | −0.58 | −0.80 (−0.22) | −0.98 (−0.18) |
| Lateral | 3.68 | 63 | 12.00 | −0.62 | −0.83 (−0.21) | −0.95 (−0.12) |
| Total | 5.12 | 103 | 10.47 | −0.60 | −0.82 (−0.22) | −0.96 (−0.14) |
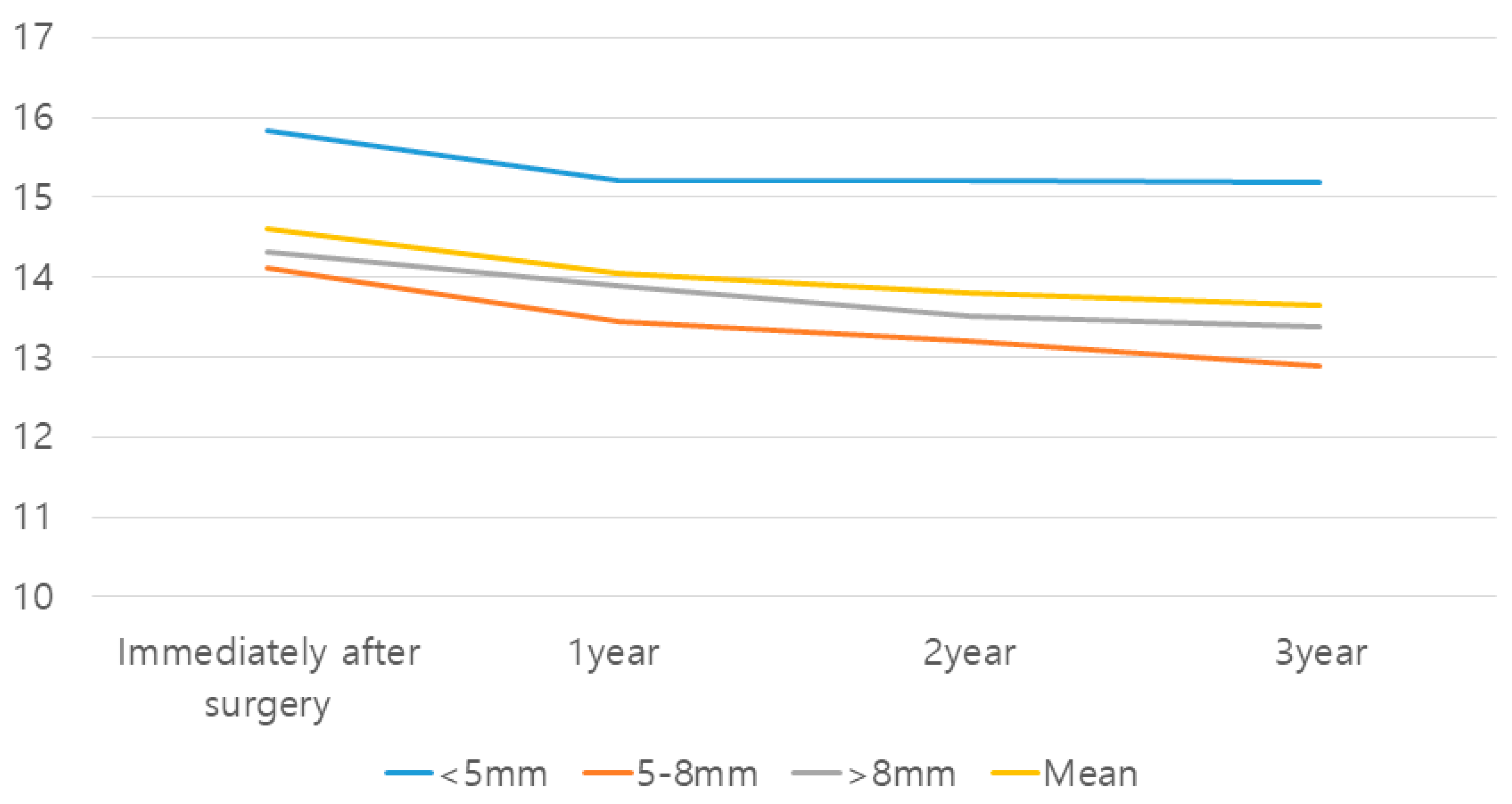
| Native Bone Height (mm) | Mean Height (mm) | No. of Implants | Gain in Bone Height (mm) | Change in the Grafted Bone Height (mm) | ||
|---|---|---|---|---|---|---|
| 1 Year | 2 Year | 3 Year | ||||
| <5 mm | 3.48 | 10 | 12.35 | −0.62 | −0.61 | −0.65 |
| 5–8 mm | 6.11 | 16 | 8.01 | −0.68 | −0.93 | −1.23 |
| >8 mm | 9.25 | 14 | 5.07 | −0.43 | −0.81 | −0.93 |
| Mean | 6.55 | 40 | 8.07 | −0.58 | −0.81 | −0.98 |
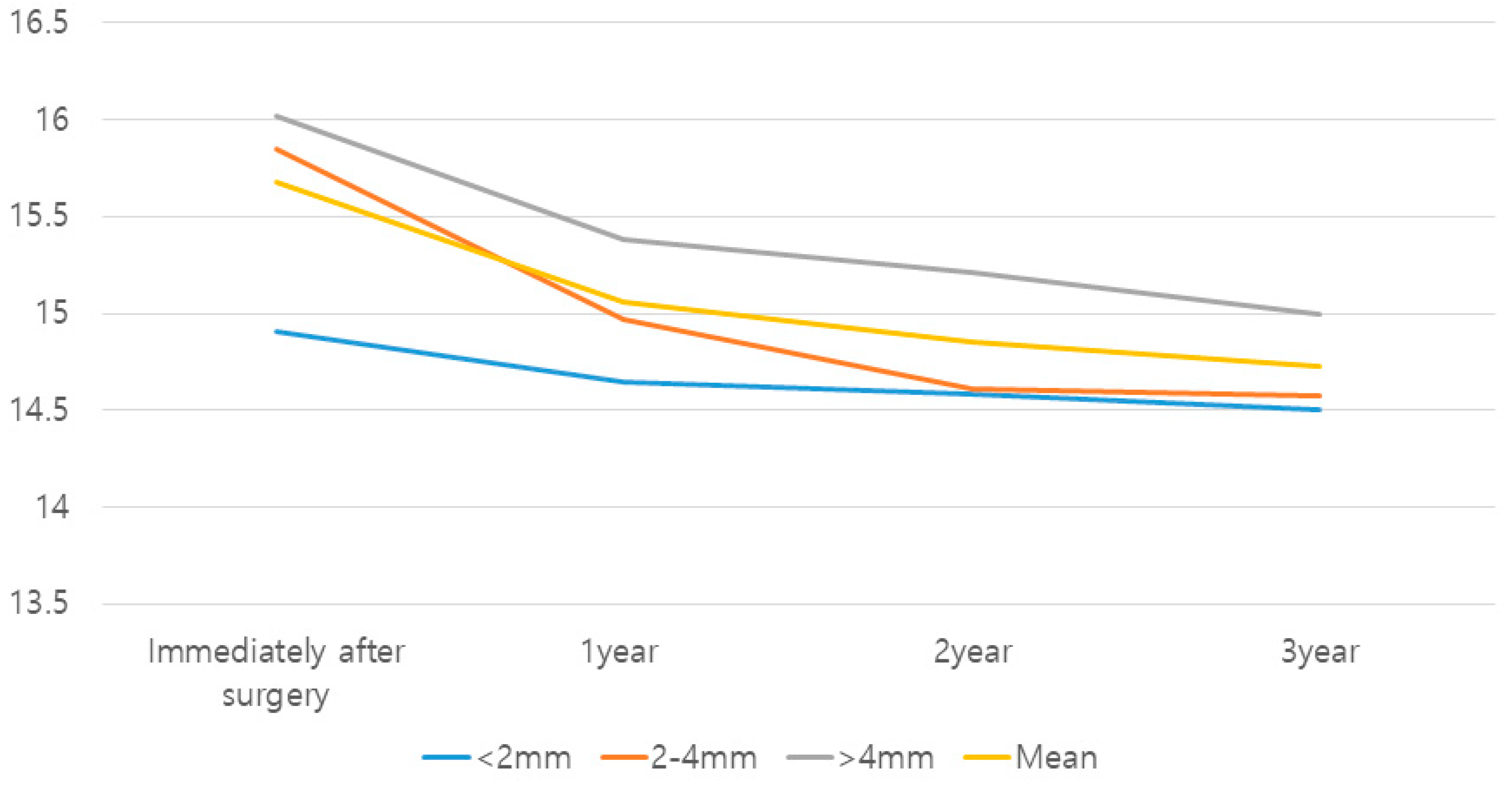
| Native Bone Height (mm) | Mean Height (mm) | No. of Implants | Gain in Bone Height (mm) | Change in the Grafted Bone Height (mm) | ||
|---|---|---|---|---|---|---|
| 1 Year | 2 Year | 3 Year | ||||
| <2 mm | 1.34 | 16 | 13.57 | −0.26 | −0.32 | −0.40 |
| 2–4 mm | 3.15 | 21 | 12.69 | −0.87 | −1.23 | −1.27 |
| >4 mm | 5.55 | 26 | 10.47 | −0.63 | −0.81 | −1.02 |
| Mean | 3.68 | 63 | 12.00 | −0.62 | −0.83 | −0.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Kim, Y.-G.; Suh, J.-Y.; Lee, D.-H.; Kim, J.-W.; Lee, J.-M. Longitudinal Study of Bone Height Change between Two Approaches for Sinus Floor Elevation. Medicina 2023, 59, 1132. https://doi.org/10.3390/medicina59061132
Park J-H, Kim Y-G, Suh J-Y, Lee D-H, Kim J-W, Lee J-M. Longitudinal Study of Bone Height Change between Two Approaches for Sinus Floor Elevation. Medicina. 2023; 59(6):1132. https://doi.org/10.3390/medicina59061132
Chicago/Turabian StylePark, Jun-Hyeong, Yong-Gun Kim, Jo-Young Suh, Du-Hyeong Lee, Jin-Wook Kim, and Jae-Mok Lee. 2023. "Longitudinal Study of Bone Height Change between Two Approaches for Sinus Floor Elevation" Medicina 59, no. 6: 1132. https://doi.org/10.3390/medicina59061132
APA StylePark, J.-H., Kim, Y.-G., Suh, J.-Y., Lee, D.-H., Kim, J.-W., & Lee, J.-M. (2023). Longitudinal Study of Bone Height Change between Two Approaches for Sinus Floor Elevation. Medicina, 59(6), 1132. https://doi.org/10.3390/medicina59061132






