Risk Factors for Anaphylaxis in Children Allergic to Peanuts
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Methods
2.3. Ethical Approval
2.4. Statistical Analysis
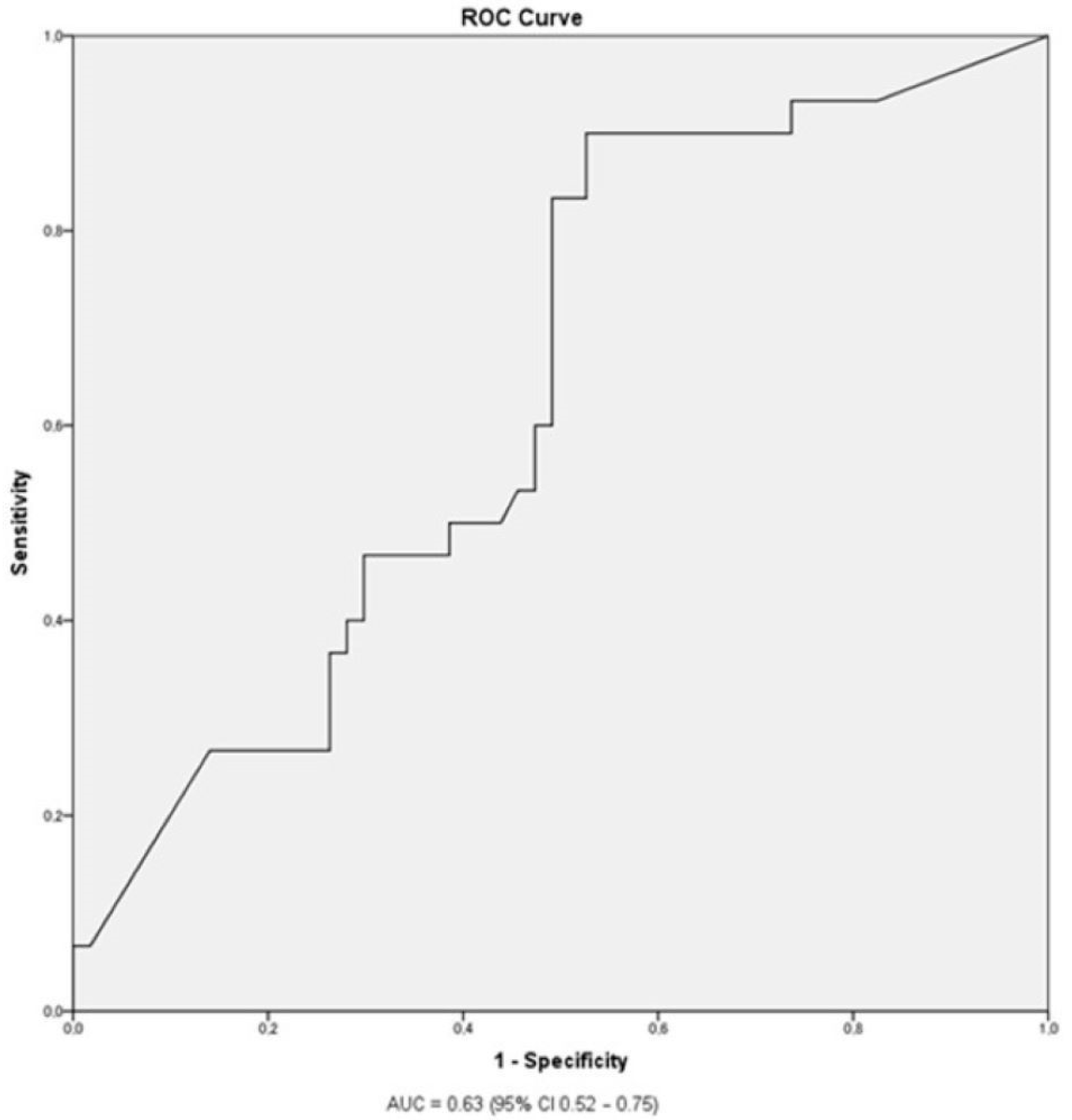
3. Results
Epidemiological, Clinical, and Laboratory Characteristics and the Severity of Allergic Reaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sicherer, S.H.; Sampson, H.A. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J. Allergy Clin. Immunol. 2018, 141, 41–58. [Google Scholar] [CrossRef]
- Al-Muhsen, S.; Clarke, A.E.; Kagan, R.S. Peanut allergy: An overview. CMAJ 2003, 168, 1279–1285. [Google Scholar]
- Lieberman, J.A.; Gupta, R.S.; Knibb, R.C.; Haselkorn, T.; Tilles, S.; Mack, D.P.; Pouessel, G. The global burden of illness of peanut allergy: A comprehensive literature review. Allergy 2021, 76, 1367–1384. [Google Scholar] [CrossRef]
- Abrams, E.M.; Chan, E.S.; Sicherer, S. Peanut allergy: New advances and ongoing controversies. Pediatrics 2020, 145, e20192102. [Google Scholar] [CrossRef]
- Bégin, P.; Graham, F.; Killer, K.; Paradis, J.; Paradis, L.; Des Roches, A. Introduction of peanuts in younger siblings of children with peanut allergy: A prospective, double-blinded assessment of risk, of diagnostic tests, and an analysis of patient preferences. Allergy 2016, 71, 1762–1771. [Google Scholar] [CrossRef]
- Allen, K.J.; Koplin, J.J.; Ponsonby, A.L.; Gurrin, L.C.; Wake, M.; Vuillermin, P.; Martin, P.; Matheson, M.; Lowe, A.; Robinson, M.; et al. Vitamin D insufficiency is associated with challenge-proven food allergy in infants. J. Allergy Clin. Immunol. 2013, 131, 1109–1116. [Google Scholar] [CrossRef]
- Abrams, E.M.; Sicherer, S. Cutaneous sensitization to peanut in children with atopic dermatitis: A window to prevention of peanut allergy. JAMA Dermatol. 2019, 155, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Halken, S.; Muraro, A.; de Silva, D.; Khaleva, E.; Angier, E.; Arasi, S.; Arshad, H.; Bahnson, H.T.; Beyer, K.; Boyle, R.; et al. EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Pediatr. Allergy Immunol. 2021, 32, 843–858. [Google Scholar] [CrossRef] [PubMed]
- Kotsapas, C.; Nicolaou, N.; Haider, S.; Kerry, G.; Turner, P.J.; Murray, C.S.; Simpson, A.; Custovic, A. Early-life predictors and risk factors of peanut allergy, and its association with asthma in later-life: Population-based birth cohort study. Clin. Exp. Allergy 2022, 52, 646–657. [Google Scholar] [CrossRef] [PubMed]
- Sikić Pogačar, M.; Mičetić-Turk, D. Vitamin D in human health. Acta Med.-Biotech. 2017, 10, 12–24. [Google Scholar] [CrossRef]
- Johnson, J.; Malinovschi, A.; Lidholm, J.; Petersson, C.J.; Nordvall, L.; Janson, C.; Alving, K.; Borres, M.P. Sensitization to storage proteins in peanut and hazelnut is associated with higher levels of inflammatory markers in asthma. Clin. Mol. Allergy 2020, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Čelakovská, J.; Bukač, J.; Vaňková, R.; Krejsek, J.; Andrýs, C. Peanuts allergy in atopic dermatitis patients, analysis of sensitization to molecular components. Agric. Immunol. 2021, 32, 221–236. [Google Scholar] [CrossRef]
- Sampson, H.A. Clinical practice. Peanut allergy. N. Engl. J. Med. 2002, 346, 1294–1299. [Google Scholar] [CrossRef]
- Datema, M.R.; Lyons, S.A.; Fernández-Rivas, M.; Ballmer-Weber, B.; Knulst, A.C.; Asero, R.; Barreales, L.; Belohlavkova, S.; de Blay, F.; Clausen, M.; et al. Estimating the risk of severe peanut allergy using clinical background and IgE sensitization profiles. Front. Allergy 2021, 2, 670789. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, M.E.; Koppelman, G.H.; Flokstra-de Blok, B.M.J.; Kollen, B.J.; Dubois, A.E.J. Prediction of the severity of allergic reactions to foods. Allergy 2018, 73, 1532. [Google Scholar] [CrossRef]
- Foong, R.X.; du Toit, G.; Fox, A.T. Asthma, food allergy, and how they relate to each other. Front. Pediatr. 2017, 5, 89. [Google Scholar] [CrossRef]
- Abrams, E.M.; Sicherer, S.H. Diagnosis and management of food allergy. CMAJ 2016, 188, 1087–1093. [Google Scholar] [CrossRef]
- Koplin, J.J.; Perrett, K.P.; Sampson, H.A. Diagnosing peanut allergy with fewer oral food challenges. J. Allergy Clin. Immunol. Pract. 2019, 7, 375–380. [Google Scholar] [CrossRef]
- Keet, C.; Plesa, M.; Szelag, D.; Shreffler, W.; Wood, R.; Dunlop, J.; Peng, R.; Dantzer, J.; Hamilton, R.G.; Togias, A.; et al. Ara h 2–specific IgE is superior to whole peanut extract–based serology or skin prick test for diagnosis of peanut allergy in infancy. J. Allergy Clin. Immunol. 2021, 147, 977–983. [Google Scholar] [CrossRef]
- Hemmings, O.; Du Toit, G.; Radulovic, S.; Lack, G.; Santos, A.F. Ara h 2 is the dominant peanut allergen despite similarities with Ara h 6. J. Allergy Clin. Immunol. 2020, 146, 621–630. [Google Scholar] [CrossRef]
- Ruinemans-Koerts, J.; Brouwer, M.L.; Schmidt-Hieltjes, Y.; Stevens, P.; Merkus, P.J.F.M.; Doggen, C.M.J.; Savelkoul, H.F.; van Setten, P.A. The indirect basophil activation test is a safe, reliable, and accessible tool to diagnose a peanut allergy in children. J. Allergy Clin. Immunol. Pract. 2022, 10, 1305–1311.e3. [Google Scholar] [CrossRef]
- Santos, A.F.; Du Toit, G.; O’Rourke, C.; Becares, N.; Couto-Francisco, N.; Radulovic, S.; Khaleva, E.; Basting, M.; Harris, K.M.; Larson, D.; et al. Biomarkers of severity and threshold of allergic reactions during oral peanut challenges. J. Allergy Clin. Immunol. 2020, 146, 344. [Google Scholar] [CrossRef] [PubMed]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Bahnson, H.T.; Radulovic, S.; Santos, A.F.; Brough, H.A.; Phippard, D.; Basting, M.; Feeney, M.; et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 2015, 372, 803–813. [Google Scholar] [CrossRef]
- Keet, C.A.; Johnson, K.; Savage, J.H.; Hamilton, R.G.; Wood, R.A. Evaluation of Ara h2 IgE thresholds in the diagnosis of peanut allergy in a clinical population. J. Allergy Clin. Immunol. Pract. 2013, 1, 101–103. [Google Scholar] [CrossRef] [PubMed]
- Ring, J.; Messmer, K. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet 1977, 309, 466–469. [Google Scholar] [CrossRef]
- Roberts, G.; Lack, G. Diagnosing peanut allergy with skin prick and specific IgE testing. J. Allergy Clin. Immunol. 2005, 115, 1291–1296. [Google Scholar] [CrossRef]
- Baseggio Conrado, A.; Patel, N.; Turner, P.J. Global patterns in anaphylaxis due to specific foods: A systematic review. J. Allergy Clin. Immunol. 2021, 148, 1515. [Google Scholar] [CrossRef] [PubMed]
- Joseph, C.L.M.; Zoratti, E.M.; Ownby, D.R.; Havstad, S.; Nicholas, C.; Nageotte, C.; Misiak, R.; Enberg, R.; Ezell, J.; Johnson, C.C.; et al. Exploring racial differences in IgE-mediated food allergy in the WHEALS birth cohort. Ann. Allergy Asthma Immunol. 2016, 116, 219–224. [Google Scholar] [CrossRef]
- Nicolaou, N.; Custovic, A. Molecular diagnosis of peanut and legume allergy. Curr. Opin. Allergy Clin. Immunol. 2011, 11, 222–228. [Google Scholar] [CrossRef]
- Martinet, J.; Couderc, L.; Renosi, F.; Bobée, V.; Marguet, C.; Boyer, O. Diagnostic value of antigen-specific immunoglobulin E immunoassays against Ara h 2 and Ara h 8 peanut components in child food allergy. Int. Arch. Allergy Immunol. 2016, 169, 216–222. [Google Scholar] [CrossRef]
- Muraro, A.; Worm, M.; Alviani, C.; Cardona, V.; Dunn Galvin, A.; Garvey, L.H.; Riggioni, C.; de Silva, D.; Angier, E.; Arasi, S.; et al. EAACI guidelines: Anaphylaxis (2021 update). Allergy 2022, 77, 357–377. [Google Scholar] [CrossRef] [PubMed]
| Grade | Skin | Abdomen | Respiratory Tract | Cardiovascular System |
|---|---|---|---|---|
| I | Itch Flushing Urticaria Angioedema | No symptoms | No symptoms | No symptoms |
| II | Itch Flushing Urticaria Angioedema | Nausea Cramps | Rhinorrhea Hoarseness Dyspnea | Tachycardia (≥20 bpm rise in heart frequency) Hypotension (≥20 mm Hg fall of SBP) Arrythmia |
| III | Itch Flushing Urticaria Angioedema | Vomiting Defecation | Laryngeal edema (stridor) Bronchospasm Cyanosis | Circulatory shock |
| IV | Itch Flushing Urticaria Angioedema | Vomiting Defecation | Respiratory arrest | Circulatory arrest |
| Characteristic | Frequency (n) | Percentage (%) |
|---|---|---|
| Female sex | 30 | 31.9 |
| Breastfeeding * | 62 | 67.4 |
| Family history of food allergy | 23 | 25 |
| of peanut allergyFamily history of allergy to airborne allergens | 15 57 | 16.3 60.6 |
| Atopic dermatitis | 69 | 75 |
| Asthma/viral induced wheeze | 33 | 35.9 |
| Allergic rhinitis | 33 | 35.9 |
| Allergy to other foods | 64 | 69.6 |
| to other nuts | 44 | 47.8 |
| Allergy to airborne allergens | 53 | 57.6 |
| Anaphylaxis to peanuts (total) | 33 | 35.1 |
| grade 2 ** | 21 | 33.3 |
| grade 3 ** | 11 | 17.5 |
| grade 4 ** | 1 | 1.6 |
| Characteristic | Median | IQR |
| Age at first introduction of peanuts (months) | 12 | 12 |
| Age at first reaction to peanuts (months) | 30 | 33 |
| Amount of peanuts (g) *** | 1 | 2.6 |
| Number of allergic reactions to peanuts | 1 | 1 |
| Number of food allergens **** | 1.5 | 4 |
| Skin test to peanuts (mm) | 6 | 9 |
| Serum total IgE levels (IU/mL) | 328 | 729 |
| Serum specific IgE levels to peanuts (IU/mL) | 8.4 | 90.8 |
| Serum specific IgE levels to Ara h2 (IU/mL) | 4.9 | 82.7 |
| Characteristic [n (%)] * | Mild Allergy ** (n = 31) | Urticaria/Angioedema (n = 30) | Anaphylaxis (n = 33) | p-Value | p-Value for Anaphylaxis (Yes/No) *** |
|---|---|---|---|---|---|
| Female sex | 11 (35.5) | 11 (36.7) | 8 (24.2) | 0.77 | 0.25 |
| Breastfeeding ◊ Family history of allergy to airborne allergens | 18 (58.1) 15 (48.4) | 20 (66.7) 22 (73.3) | 24 (72.7) 20 (60.6) | 0.62 0.51 | 0.65 1.00 |
| Family history of food allergy to peanuts | 6 (19.4) 6 (19.4) | 8 (26.7) 4 (13.3) | 9 (27.3) 5 (15.1) | 0.70 0.64 | 0.81 1.00 |
| Atopic dermatitis | 21 (67.7) | 22 (73.3) | 26 (78.8) | 0.90 | 0.62 |
| Asthma/viral induced wheeze | 8 (25.8) | 14 (46.7) | 11 (33.3) | 0.37 | 0.66 |
| Allergic rhinitis | 10 (32.3) | 11 (36.7) | 12 (36.4) | 0.96 | 1.00 |
| Allergy to other foods to other nuts | 20 (64.5) 13 (41.9) | 18 (60) 12 (40) | 26 (78.8) 19 (57.6) | 0.87 0.87 | 0.16 0.16 |
| Allergy to airborne allergens | 13 (41.9) | 19 (63.3) | 21 (63.6) | 0.14 | 0.66 |
| Characteristic [median (IQR)] | |||||
| Age at first introduction of peanuts (months) | 12 (0) | 13 (6) | 13 (23) | 0.06 | 0.53 |
| Age at first reaction to peanuts (months) | 24 (29) | 18 (22) | 36 (30) | 0.60 | 0.53 |
| Amount of peanuts (g) ◊◊ | 2.5 (7.1) | 0.3 (0.6) | 1 (1.9) | 0.03 | 0.40 |
| Number of allergic reactions to peanuts | 1 (0) | 1 (1) | 2 (2) | 0.43 | 0.05 |
| Number of food allergens ◊◊◊ | 1 (4) | 1 (5) | 2 (4) | 0.28 | 0.22 |
| Skin test to peanuts (mm) | 5 (9) | 5 (8) | 7 (10) | 0.47 | 0.52 |
| Serum total IgE levels (IU/mL) | 441 (1005) | 347 (1463) | 482 (1209) | 0.97 | 0.54 |
| Serum specific IgE levels to peanuts (IU/mL) | 2.5 (20.6) | 15.7 (98.4) | 9.4 (96.9) | 0.13 | 0.10 |
| Serum specific IgE levels to Ara h2 (IU/mL) | 0.6 (8.1) | 10.7 (89.1) | 5.3 (98.3) | 0.06 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petek, T.; Lajhar, M.; Krašovec, B.; Homšak, M.; Kavalar, M.; Korošec, P.; Koren, B.; Tomazin, M.; Hojnik, T.; Berce, V. Risk Factors for Anaphylaxis in Children Allergic to Peanuts. Medicina 2023, 59, 1037. https://doi.org/10.3390/medicina59061037
Petek T, Lajhar M, Krašovec B, Homšak M, Kavalar M, Korošec P, Koren B, Tomazin M, Hojnik T, Berce V. Risk Factors for Anaphylaxis in Children Allergic to Peanuts. Medicina. 2023; 59(6):1037. https://doi.org/10.3390/medicina59061037
Chicago/Turabian StylePetek, Tadej, Mija Lajhar, Blažka Krašovec, Matjaž Homšak, Maja Kavalar, Peter Korošec, Brigita Koren, Maja Tomazin, Tina Hojnik, and Vojko Berce. 2023. "Risk Factors for Anaphylaxis in Children Allergic to Peanuts" Medicina 59, no. 6: 1037. https://doi.org/10.3390/medicina59061037
APA StylePetek, T., Lajhar, M., Krašovec, B., Homšak, M., Kavalar, M., Korošec, P., Koren, B., Tomazin, M., Hojnik, T., & Berce, V. (2023). Risk Factors for Anaphylaxis in Children Allergic to Peanuts. Medicina, 59(6), 1037. https://doi.org/10.3390/medicina59061037






