Unraveling the Efficacy of Therapeutic Interventions for Short Cervix: Insights from a Retrospective Study for Improved Clinical Management
Abstract
1. Introduction
2. Materials and Methods
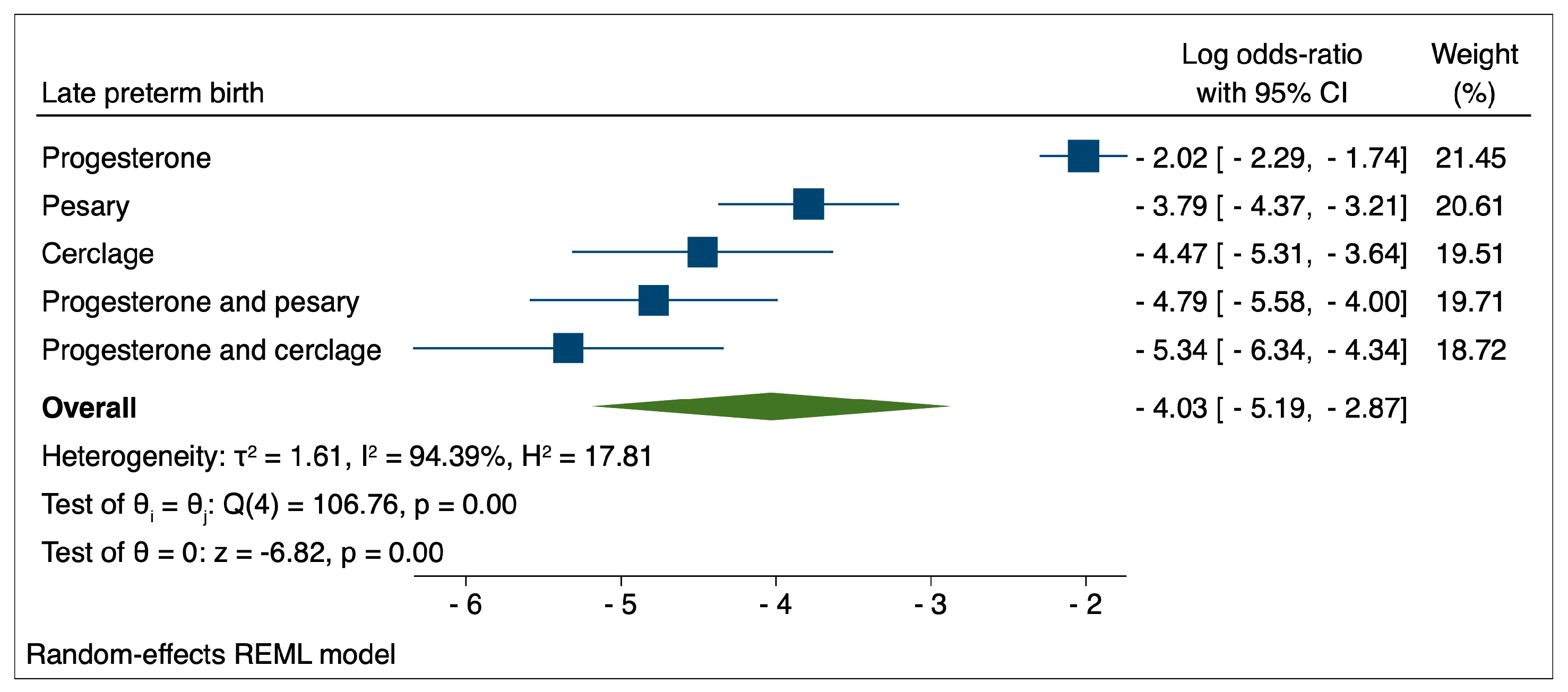
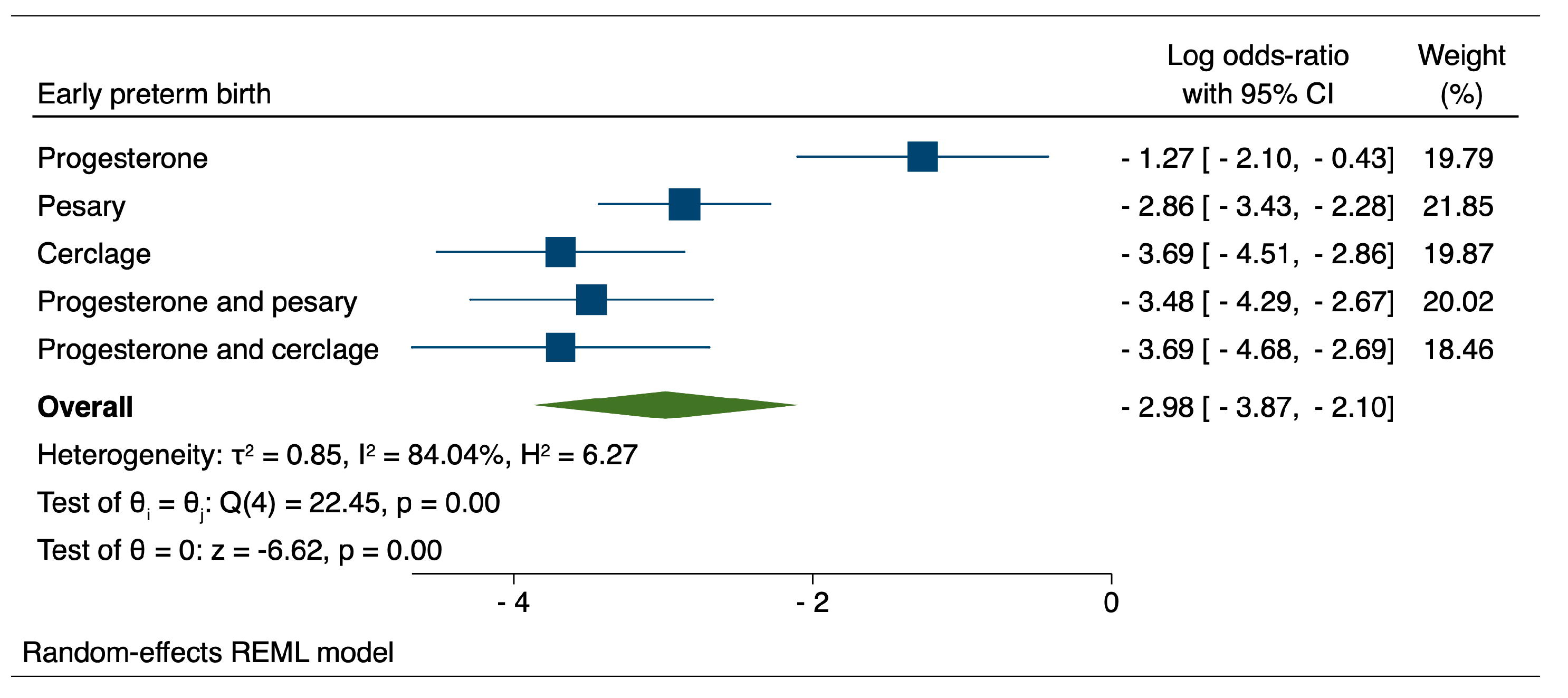
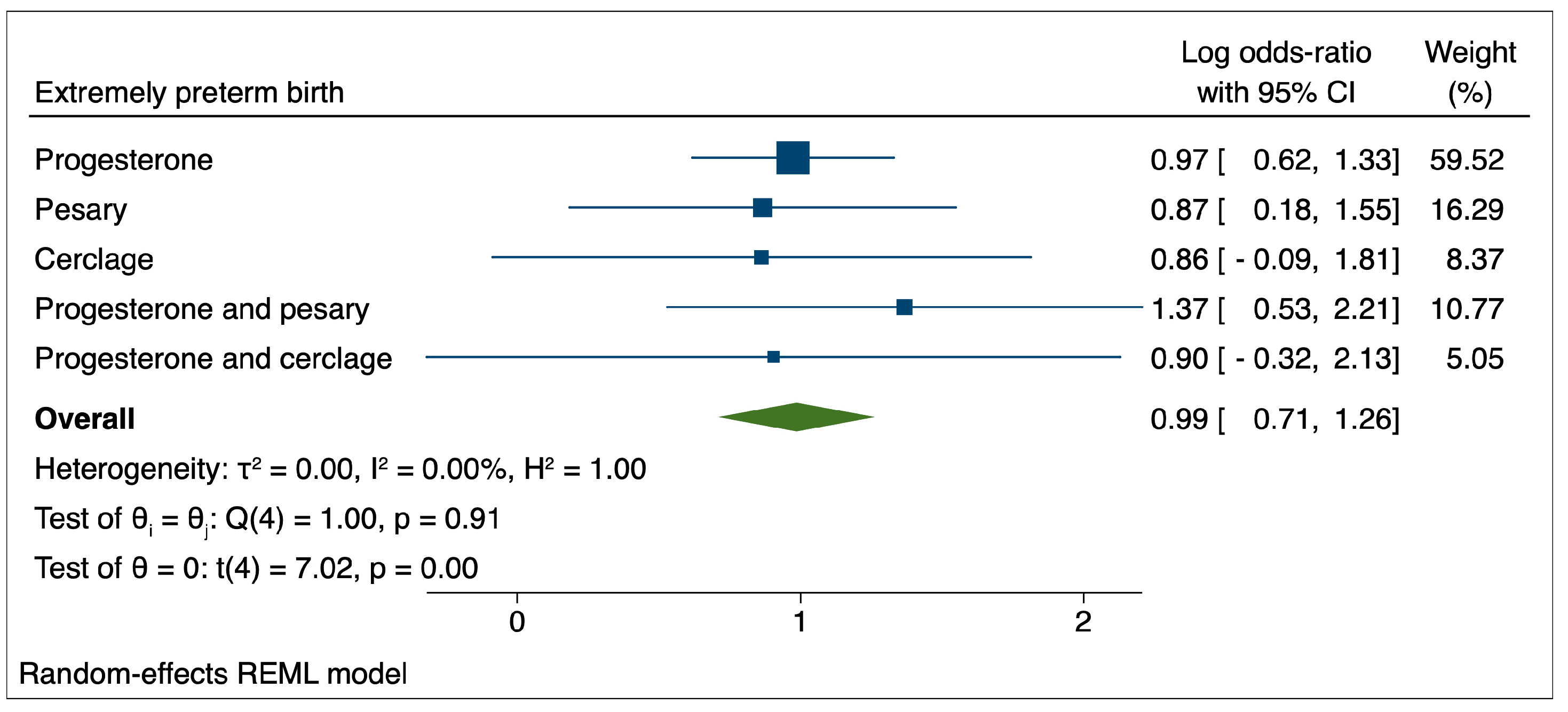
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosa-Mangeret, F.; Benski, A.-C.; Golaz, A.; Zala, P.Z.; Kyokan, M.; Wagner, N.; Muhe, L.M.; Pfister, R.E. 2.5 Million Annual Deaths—Are Neonates in Low- and Middle-Income Countries Too Small to Be Seen? A Bottom-Up Overview on Neonatal Morbi-Mortality. Trop. Med. Infect. Dis. 2022, 7, 64. [Google Scholar] [CrossRef]
- Kramer, M.S.; Papageorghiou, A.; Culhane, J.; Bhutta, Z.; Goldenberg, R.L.; Gravett, M.; Iams, J.D.; Conde-Agudelo, A.; Waller, S.; Barros, F.; et al. Challenges in defining and classifying the preterm birth syndrome. Am. J. Obstet. Gynecol. 2012, 206, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Delnord, M.; Zeitlin, J. Epidemiology of late preterm and early term births—An international perspective. Semin. Fetal Neonatal Med. 2019, 24, 3–10. [Google Scholar] [CrossRef] [PubMed]
- De Luca, D. Respiratory distress syndrome in preterm neonates in the era of precision medicine: A modern critical care-based approach. Pediatr. Neonatol. 2021, 62, S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Duchon, J.; Barbian, M.E.; Denning, P.W. Necrotizing Enterocolitis. Clin. Perinatol. 2021, 48, 229–250. [Google Scholar] [CrossRef] [PubMed]
- Ophelders, D.R.M.G.; Gussenhoven, R.; Klein, L.; Jellema, R.K.; Westerlaken, R.J.; Hütten, M.C.; Vermeulen, J.; Wassink, G.; Gunn, A.J.; Wolfs, T.G. Preterm brain injury, antenatal triggers, and therapeutics: Timing is key. Cells 2020, 9, 1871. [Google Scholar] [CrossRef]
- Luu, T.M.; Rehman Mian, M.O.; Nuyt, A.M. Long-Term Impact of Preterm Birth: Neurodevelopmental and Physical Health Outcomes. Clin. Perinatol. 2017, 44, 305–314. [Google Scholar] [CrossRef]
- Carmo, A.L.S.D.; Fredo, F.W.; Bruck, I.; de Lima, J.D.R.M.; Janke, R.N.R.G.H.; Fogaça, T.d.G.M.; Glaser, J.A.; Riechi, T.I.J.d.S.; Antoniuk, S.A. Neurological, cognitive and learning evaluation of students who were born preterm. Rev. Paul. Pediatr. 2021, 40, e2020252. [Google Scholar] [CrossRef]
- Hoffman, M.K. Prediction and Prevention of Spontaneous Preterm Birth: ACOG Practice Bulletin, Number 234. Obstet. Gynecol. 2021, 138, 945–946. [Google Scholar] [CrossRef]
- Filip, C.; Socolov, D.G.; Albu, E.; Filip, C.; Serban, R.; Popa, R.F. Serological Parameters and Vascular Investigation for a Better Assessment in DVT during Pregnancy—A Systematic Review. Medicina 2021, 57, 160. [Google Scholar] [CrossRef]
- Albu, D.F.; Albu, C.C.; Gogănău, A.M.; Albu, Ş.D.; Mogoantă, L.; Edu, A.; Ditescu, D.; Vaduva, C.C. Borderline Brenner tumors associated with ovarian cyst—Case presentation. Rom. J. Morphol. Embryol. 2016, 57, 893–898. [Google Scholar] [PubMed]
- Săndulescu, M.S.; Văduva, C.-C.; Siminel, M.A.; Dijmărescu, A.L.; Vrabie, S.C.; Camen, I.V.; Tache, D.E.; Neamţu, S.D.; Nagy, R.D.; Carp-Velişcu, A.; et al. Impact of COVID-19 on fertility and assisted reproductive technology (ART): A systematic review. Rom. J. Morphol. Embryol. 2022, 63, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Vicoveanu, P.; Vasilache, I.A.; Scripcariu, I.S.; Nemescu, D.; Carauleanu, A.; Vicoveanu, D.; Covali, A.R.; Filip, C.; Socolov, D. Use of a Feed-Forward Back Propagation Network for the Prediction of Small for Gestational Age Newborns in a Cohort of Pregnant Patients with Thrombophilia. Diagnostics 2022, 12, 1009. [Google Scholar] [CrossRef] [PubMed]
- Vicoveanu, P.; Vasilache, I.-A.; Nemescu, D.; Carauleanu, A.; Scripcariu, I.-S.; Rudisteanu, D.; Burlui, A.; Rezus, E.; Socolov, D. Predictors Associated with Adverse Pregnancy Outcomes in a Cohort of Women with Systematic Lupus Erythematosus from Romania—An Observational Study (Stage 2). J. Clin. Med. 2022, 11, 1964. [Google Scholar] [CrossRef]
- Cobo, T.; Kacerovsky, M.; Jacobsson, B. Risk factors for spontaneous preterm delivery. Int. J. Gynecol. Obstet. 2020, 150, 17–23. [Google Scholar] [CrossRef]
- Liu, B.; Xu, G.; Sun, Y.; Du, Y.; Gao, R.; Snetselaar, L.G.; Santillan, M.K.; Bao, W. Association between maternal pre-pregnancy obesity and preterm birth according to maternal age and race or ethnicity: A population-based study. Lancet Diabetes Endocrinol. 2019, 7, 707–714. [Google Scholar] [CrossRef]
- Fanni, D.; Gerosa, C.; Nurchi, V.M.; Manchia, M.; Saba, L.; Coghe, F.; Crisponi, G.; Gibo, Y.; Van Eyken, P.; Fanos, V.; et al. The Role of Magnesium in Pregnancy and in Fetal Programming of Adult Diseases. Biol. Trace Element Res. 2021, 199, 3647–3657. [Google Scholar] [CrossRef]
- Bezerra Espinola, M.S.; Laganà, A.S.; Bilotta, G.; Gullo, G.; Aragona, C.; Unfer, V. D-chiro-inositol Induces Ovulation in Non-Polycystic Ovary Syndrome (PCOS), Non-Insulin-Resistant Young Women, Likely by Modulating Aromatase Expression: A Report of 2 Cases. Am. J. Case Rep. 2021, 22, e932722. [Google Scholar] [CrossRef]
- Gullo, G.; Carlomagno, G.; Unfer, V.; D′Anna, R. Myo-inositol: From induction of ovulation to menopausal disorder management. Minerva Ginecol. 2015, 67, 485–486. [Google Scholar]
- Vahanian, S.A.; Lavery, J.A.; Ananth, C.V.; Vintzileos, A. Placental implantation abnormalities and risk of preterm delivery: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2015, 213, S78–S90. [Google Scholar] [CrossRef]
- Berger, V.; Moghadassi, M.; Gosnell, K.; Sparks, T.; Velez, J.G.; Norton, M. The Risk of Preterm Birth in Pregnancies with Fetal Anomalies [11Q]. Obstet. Gynecol. 2017, 129, 176S. [Google Scholar] [CrossRef]
- Herkert, D.; Wheeler, S.M.; Weaver, K.; Grace, M.; Dotters-Katz, S. The risk for recurrent preterm birth after prior preterm birth complicated by major fetal anomaly. J. Matern. Neonatal Med. 2022, 35, 8147–8149. [Google Scholar] [CrossRef] [PubMed]
- Bernad, S.I.B.E.; Barbat, T.; Barbu, D.; Albulescu, V. Assessment of the placental blood flow in the normally developing and growth-restricted fetus. In Proceedings of 22nd European Congress of Perinatal Medicine, Granada, Spain, 26–20 May 2010; Monduzzi Editore SPA: Bologna, Italy, 2010; pp. 127–130. [Google Scholar]
- Noventa, M.; Spagnol, G.; Marchetti, M.; Saccardi, C.; Bonaldo, G.; Laganà, A.S.; Cavallin, F.; Andrisani, A.; Ambrosini, G.; Vitale, S.G.; et al. Uterine Septum with or without Hysteroscopic Metroplasty: Impact on Fertility and Obstetrical Outcomes—A Systematic Review and Meta-Analysis of Observational Research. J. Clin. Med. 2022, 11, 3290. [Google Scholar] [CrossRef] [PubMed]
- Lemmers, M.; Verschoor, M.; Hooker, A.; Opmeer, B.; Limpens, J.; Huirne, J.; Ankum, W.; Mol, B. Dilatation and curettage increases the risk of subsequent preterm birth: A systematic review and meta-analysis. Hum. Reprod. 2016, 31, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Rault, E.; Delorme, P.; Goffinet, F.; Girault, A. Impact of history of myomectomy on preterm birth risk in women with a leiomyomatous uterus: A propensity score analysis. BMC Pregnancy Childbirth 2020, 20, 720. [Google Scholar] [CrossRef]
- Gedikbasi, A.; Akyol, A.; Bingol, B.; Cakmak, D.; Sargin, M.A.; Uncu, R.; Ceylan, Y. Multiple Repeated Cesarean Deliveries: Operative Complications in the Fourth and Fifth Surgeries in Urgent and Elective Cases. Taiwan. J. Obstet. Gynecol. 2010, 49, 425–431. [Google Scholar] [CrossRef]
- NICE. NIoHaCE. Preterm Labour and Birth (NICE Guideline 25). Available online: https://www.ncbi.nlm.nih.gov/books/NBK553008/ (accessed on 16 March 2023).
- Norman, J.E.; Marlow, N.; McConnachie, A.; Petrou, S.; Sebire, N.J.; Lavender, T.; Whyte, S.; Norrie, J.; Messow, C.-M.; Shennan, A.; et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM study): A multicentre, randomised, double-blind trial. Lancet 2016, 387, 2106–2116. [Google Scholar] [CrossRef]
- Crowther, C.A.; Ashwood, P.; McPhee, A.J.; Flenady, V.; Tran, T.; Dodd, J.M.; Robinson, J.S. For the PROGRESS Study Group Vaginal progesterone pessaries for pregnant women with a previous preterm birth to prevent neonatal respiratory distress syndrome (the PROGRESS Study): A multicentre, randomised, placebo-controlled trial. PLoS Med. 2017, 14, e1002390. [Google Scholar] [CrossRef]
- Care, A.; Nevitt, S.J.; Medley, N.; Donegan, S.; Good, L.; Hampson, L.; Smith, C.T. Interventions to prevent spontaneous preterm birth in women with singleton pregnancy who are at high risk: Systematic review and network meta-analysis. BMJ 2022, 376, e064547. [Google Scholar] [CrossRef]
- Pacagnella, R.C.; Silva, T.V.; Cecatti, J.G.; Passini, R., Jr.; Fanton, T.F.; Borovac-Pinheiro, A.; Pereira, C.M.; Fernandes, K.; Franca, M.S.; Li, W.; et al. Pessary Plus Progesterone to Prevent Preterm Birth in Women With Short Cervixes: A Randomized Controlled Trial. Obstet. Gynecol. 2022, 139, 41–51. [Google Scholar] [CrossRef]
- Alizadeh, F.; Mahmoudinia, M.; Mirteimoori, M.; Pourali, L.; Niroumand, S. Comparison of oral Dydrogesterone and 17-α hydroxyprogesterone caprate in the prevention of preterm birth. BMC Pregnancy Childbirth 2022, 22, 167. [Google Scholar] [CrossRef] [PubMed]
- Kagan, K.O.; Sonek, J. How to measure cervical length. Ultrasound Obstet. Gynecol. 2015, 45, 358–362. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists′ Committee on Practice Bulletins—Obstetrics. Prediction and Prevention of Spontaneous Preterm Birth: ACOG Practice Bulletin Summary, Number 234. Obstet. Gynecol. 2021, 138, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Sentilhes, L.; Sénat, M.-V.; Ancel, P.-Y.; Azria, E.; Benoist, G.; Blanc, J.; Brabant, G.; Bretelle, F.; Brun, S.; Doret, M.; et al. Prevention of spontaneous preterm birth: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF). Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 210, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.; Abele, H.; Bahlmann, F.; Bedei, I.; Doubek, K.; Felderhoff-Müser, U. Prevention and Therapy of Preterm Birth. Guideline of the DGGG, OEGGG and SGGG (S2k Level, AWMF Registry Number 015/025, February 2019)—Part 2 with Recommendations on the Tertiary Prevention of Preterm Birth and the Management of Preterm Premature Rupture of Membranes. Geburtshilfe Frauenheilkd 2019, 79, 813–833. [Google Scholar]
- Berger, R.; Abele, H.; Bahlmann, F.; Bedei, I.; Doubek, K.; Felderhoff-Müser, U. Prevention and Therapy of Preterm Birth. Guideline of the DGGG, OEGGG and SGGG (S2k Level, AWMF Registry Number 015/025, February 2019)—Part 1 with Recommendations on the Epidemiology, Etiology, Prediction, Primary and Secondary Prevention of Preterm Birth. Geburtshilfe Frauenheilkd 2019, 79, 800–812. [Google Scholar] [CrossRef]
- Chatzakis, C.; Efthymiou, A.; Sotiriadis, A.; Makrydimas, G. Emergency cerclage in singleton pregnancies with painless cervical dilatation: A meta-analysis. Acta Obstet. Gynecol. Scand. 2020, 99, 1444–1457. [Google Scholar] [CrossRef]
- Mönckeberg, M.; Valdés, R.; Kusanovic, J.P.; Schepeler, M.; Nien, J.K.; Pertossi, E.; Silva, P.; Silva, K.; Venegas, P.; Guajardo, U.; et al. Patients with acute cervical insufficiency without intra-amniotic infection/inflammation treated with cerclage have a good prognosis. J. Périnat. Med. 2019, 47, 500–509. [Google Scholar] [CrossRef]
- Stupin, J.H.; David, M.; Siedentopf, J.-P.; Dudenhausen, J.W. Emergency cerclage versus bed rest for amniotic sac prolapse before 27 gestational weeks. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 139, 32–37. [Google Scholar] [CrossRef]
- Ito, A.; Maseki, Y.; Ikeda, S.; Tezuka, A.; Kuribayashi, M.; Furuhashi, M. Factors associated with delivery at or after 28 weeks gestation in women with bulging fetal membranes before 26 weeks gestation. J. Matern. Neonatal Med. 2017, 30, 2046–2050. [Google Scholar] [CrossRef]
- Abdel-Aleem, H.; Shaaban, O.M.; Abdel-Aleem, A.M.; Mohamed, A.A. Cervical pessary for preventing preterm birth in singleton pregnancies. Cochrane Database Syst. Rev. 2022, 2022, Cd014508. [Google Scholar]
- Alfirevic, Z.; Stampalija, T.; Medley, N. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst. Rev. 2017, 6, Cd008991. [Google Scholar] [CrossRef]
- Conde-Agudelo, A.; Romero, R.; Da Fonseca, E.; O’brien, J.M.; Cetingoz, E.; Creasy, G.W.; Hassan, S.S.; Erez, O.; Pacora, P.; Nicolaides, K.H. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: Updated indirect comparison meta-analysis. Am. J. Obstet. Gynecol. 2018, 219, 10–25. [Google Scholar] [CrossRef] [PubMed]
- Ragab, A.; Mesbah, Y. To do or not to do emergency cervical cerclage (a rescue stitch) at 24–28 weeks gestation in addition to progesterone for patients coming early in labor? A prospective randomized trial for efficacy and safety. Arch. Gynecol. Obstet. 2015, 292, 1255–1260. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Melguizo, S.; San-Frutos, L.; Martínez-Payo, C.; Ruiz-Antorán, B.; Adiego-Burgos, B.; Campillos-Maza, J.M.; Garcia-Gonzalez, C.; Martinez-Guisasola, M.; Perez-Carbajo, E.; Teulon-Gonzalez, M.; et al. Cervical Pessary Compared with Vaginal Progesterone for Preventing Early Preterm Birth: A Randomized Controlled Trial. Obstet. Gynecol. 2018, 132, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Enakpene, C.A.; DiGiovanni, L.; Jones, T.N.; Marshalla, M.; Mastrogiannis, D.; Della Torre, M. Cervical cerclage for singleton pregnant patients on vaginal progesterone with progressive cervical shortening. Am. J. Obstet. Gynecol. 2018, 219, 397.e1–397.e10. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Vogel, J.P.; Chawanpaiboon, S.; Moller, A.-B.; Watananirun, K.; Bonet, M.; Lumbiganon, P. The global epidemiology of preterm birth. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 52, 3–12. [Google Scholar] [CrossRef]
- da Fonseca, E.B.; Damião, R.; Moreira, D.A. Preterm birth prevention. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 69, 40–49. [Google Scholar] [CrossRef]
- Petre Izabella, C.M.; Bernad, E.; DOrneanu, F.; Citu, I.; Citu, C.; Stelea, L.; Iacob, D.; Boglut, A.; Moleriu, R.M. Procalcitonin—Neonatal Sepsis Biomarker. In Proceedings of the 13th Conference of the Romanian-German Society of Obstetrics and Gynecology, Timisoara, Romania, 14–16 September 2017; pp. 232–236. [Google Scholar]
| Patient’s Data | Group 1 (n = 562 Patients) | Group 2 (n = 286 Patients) | Group 3 (n = 128 Patients) | Group 4 (n = 101 Patients) | Group 5 (n = 69 Patients) | p-Value |
|---|---|---|---|---|---|---|
| Maternal age, years (mean and standard deviation) | 29.46 ± 6.59 | 30.34 ± 6.54 | 29.98 ± 6.60 | 29.83 ± 6.85 | 30.67 ± 6.19 | 0.31 |
| Medium (n/%) | Rural = 291 (51.9%) Urban = 270 (48.1%) | Rural = 138 (48.1%) Urban = 149 (51.9%) | Rural = 68 (53.1%) Urban = 60 (46.9%) | Rural = 52 (51.5%) Urban = 49 (48.5%) | Rural = 42 (60.9%) Urban = 39.1 (47%) | 0.41 |
| Smoking (n/%) | Yes = 13 (2.3%) | Yes = 10 (3.49%) | Yes = 7 (5.5%) | Yes = 5 (5.0%) | Yes = 4 (5.8%) | 0.19 |
| Personal history of preterm birth (n/%) | Yes = 34 (6.04%) | Yes = 47 (16.43%) | Yes = 50 (39.06%) | Yes = 31 (30.69%) | Yes = 18 (26.08%) | <0.001 |
| Personal history of thrombosis (n/%) | Yes = 2 (0.35%) | Yes = 1 (0.34%) | Yes = 0 (0%) | Yes = 0 (0%) | Yes = 0 (0%) | 0.47 |
| Diabetes (n/%) | Yes = 6 (1.1%) | Yes = 2 (0.7%) | Yes = 1 (0.8%) | Yes = 1 (1%) | Yes = 0 (0%) | 0.91 |
| Thrombophilia (n/%) | Yes = 5 (0.88%) | Yes = 2 (0.69%) | Yes = 1 (0.8%) | Yes = 0 (0%) | Yes = 0 (0%) | 0.98 |
| Personal history of autoimmune disorders (n/%) | Yes = 18 (3.2%) | Yes = 14 (4.89%) | Yes = 8 (6.25%) | Yes = 5 (4.95%) | Yes = 0 (0%) | 0.33 |
| Personal history of ischemic placental disease (n/%) | Yes = 7 (1.24%) | Yes = 4 (1.39%) | Yes = 2 (1.56%) | Yes = 1 (1%) | Yes = 0 (0%) | 0.98 |
| Cervical length, mm (mean and standard deviation) | 22.1 ± 2.16 | 20.25 ± 2.21 | 19.75 ± 1.70 | 18.75 ± 3.59 | 16.5 ± 3.87 | 0.14 |
| Treatment | Late Preterm Birth | Early Preterm Birth | Extremely Preterm Birth | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ATT | 95%CI Lower Bound | 95%CI Upper Bound | p-Value | ATT | 95%CI Lower Bound | 95%CI Upper Bound | p-Value | ATT | 95%CI Lower Bound | 95%CI Upper Bound | p-Value | |
| Progesterone | −0.14 | −0.19 | −0.09 | <0.001 | −0.07 | −0.13 | 0.11 | <0.001 | −0.07 | −0.13 | 0.10 | <0.001 |
| Pessary | −0.16 | −0.28 | −0.05 | <0.001 | −0.10 | −0.17 | 0.21 | 0.03 | 0.06 | −0.01 | 0.13 | 0.09 |
| Cerclage | −0.14 | −0.31 | −0.01 | 0.01 | −0.08 | −0.19 | 0.23 | 0.02 | 0.06 | −0.04 | 0.17 | 0.255 |
| Progesterone and pessary | −0.18 | −0.35 | −0.01 | 0.03 | −0.07 | −0.21 | 0.16 | 0.01 | 0.16 | −0.03 | 0.35 | 0.09 |
| Progesterone and cerclage | −0.28 | −0.48 | −0.08 | 0.006 | −0.21 | −0.35 | 0.37 | 0.009 | 0.09 | −0.09 | 0.29 | 0.306 |
| Therapeutic Intervention | Late Preterm Birth | Early Preterm Birth | Extremely Preterm Birth | |||
|---|---|---|---|---|---|---|
| RR and 95% CI | p-Value | RR and 95% CI | p-Value | RR and 95% CI | p-Value | |
| Progesterone vs. pessary | 3.13 (2.42–4.04) | <0.001 | 3.73 (2.37–5.88) | <0.001 | 4.81 (2.49–9.26) | <0.001 |
| Progesterone vs cerclage | 2.73 (1.93–3.86) | <0.001 | 3.57 (1.87–6.83) | <0.001 | 4.16 (1.71–10.12) | 0.001 |
| Cerclage vs. pessary | 0.87 (0.57–1.32) | 0.52 | 1.04 (0.49–2.20) | 0.11 | 1.15 (0.40–3.28) | 0.78 |
| Progesterone + pessary vs progesterone alone | 0.36 (0.24–0.54) | <0.001 | 0.44 (0.24–0.78) | 0.005 | 0.59 (0.28–1.23) | 0.15 |
| Progesterone + pessary vs. cerclage | 0.79 (0.47–1.32) | 0.37 | 1.58 (0.69–3.61) | 0.27 | 2.45 (0.82–7.35) | 0.10 |
| Progesterone + pessary vs. pessary | 1.14 (0.72–1.82) | 0.55 | 1.65 (0.82–3.28) | 0.15 | 2.83 (1.13–7.11) | 0.05 |
| Progesterone + cerclage vs. progesterone alone | 0.30 (0.18–0.52) | <0.001 | 0.49 (0.26–0.91) | 0.02 | 0.27 (0.08–0.84) | 0.02 |
| Progesterone + cerclage vs. pessary | 0.96 (0.53–1.73) | 0.91 | 1.84 (0.88–3.81) | 0.10 | 1.31 (0.37–4.60) | 0.66 |
| Progesterone + cerclage vs. cerclage | 0.84 (0.45–1.58) | 0.60 | 1.76 (0.74–4.17) | 0.19 | 1.13 (0.28–4.56) | 0.85 |
| Progesterone + pessary vs. progesterone +cerclage | 1.18 (0.61–2.29) | 0.61 | 0.89 (0.39–2.01) | 0.79 | 1.61 (0.43–5.92) | 0.47 |
| Outcome | Late Preterm Birth | Early Preterm Birth | Extremely Preterm Birth | |||
|---|---|---|---|---|---|---|
| aOR and 95% CI | p-Value | aOR and 95% CI | p-Value | aOR and 95% CI | p-Value | |
| Cesarean delivery | 2.11 (0.35–5.41) | <0.001 | 0.95 (0.70–1.29) | 0.78 | 0.88 (0.49–1.57) | 0.68 |
| Apgar score at 1 min < 7 | 1.82 (1.42–2.31) | <0.001 | 1.79 (0.68–4.41) | 0.007 | 1.83 (0.19–4.51) | 0.008 |
| Apgar score at 5 min < 7 | 1. 21 (0.45–3.58) | <0.001 | 2.65 (1.55–4.55) | <0.001 | 1.28 (0.45–3.44) | 0.03 |
| NICU admission | 0.96 (0.67–1.38) | 0.84 | 1.26 (0.17–4.21) | <0.001 | 0.72 (0.18–2.87) | <0.001 |
| Necrotizing enterocolitis | 0.44 (0.16–1.85) | 0.79 | 1.04 (0.55–2.65) | <0.001 | 1.97 (0.49–3.35) | <0.001 |
| Invasive ventilation | 1.39 (0.54–3.09) | <0.001 | 1.42 (0.73–2.10) | <0.001 | 1.47 (0.25–2.75) | <0.001 |
| ARDS | 1.56 (0.37–3.32) | <0.001 | 1.38 (0.38–2.44) | <0.001 | 2.32 (0.92–3.37) | <0.001 |
| Cerebral palsy | 0.96 (0.08–4.83) | 0.67 | 0.20 (−0.30–0.72) | 0.42 | 1.99 (0.26–4.04) | 0.035 |
| Visual or hearing impairment | 0.48 (0.02–2.52) | 0.43 | 0.90 (−0.86–2.68) | 0.31 | 1.67 (0.08–4.68) | 0.003 |
| Intraventricular hemorrhage | 0.56 (0.37–1.32) | 0.06 | 0.38 (−0.38–1.14) | 0.32 | 2.32 (0.92–3.37) | <0.001 |
| Neonatal death | 0.68 (0.36–1.82) | 0.79 | 1.04 (−0.55–2.65) | <0.001 | 1.97 (0.49–3.35) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luca, A.-M.; Bernad, E.; Nemescu, D.; Vaduva, C.; Harabor, A.; Adam, A.-M.; Harabor, V.; Nechita, A.; Strobescu, C.; Mogos, R.; et al. Unraveling the Efficacy of Therapeutic Interventions for Short Cervix: Insights from a Retrospective Study for Improved Clinical Management. Medicina 2023, 59, 1018. https://doi.org/10.3390/medicina59061018
Luca A-M, Bernad E, Nemescu D, Vaduva C, Harabor A, Adam A-M, Harabor V, Nechita A, Strobescu C, Mogos R, et al. Unraveling the Efficacy of Therapeutic Interventions for Short Cervix: Insights from a Retrospective Study for Improved Clinical Management. Medicina. 2023; 59(6):1018. https://doi.org/10.3390/medicina59061018
Chicago/Turabian StyleLuca, Alina-Madalina, Elena Bernad, Dragos Nemescu, Cristian Vaduva, Anamaria Harabor, Ana-Maria Adam, Valeriu Harabor, Aurel Nechita, Cristina Strobescu, Raluca Mogos, and et al. 2023. "Unraveling the Efficacy of Therapeutic Interventions for Short Cervix: Insights from a Retrospective Study for Improved Clinical Management" Medicina 59, no. 6: 1018. https://doi.org/10.3390/medicina59061018
APA StyleLuca, A.-M., Bernad, E., Nemescu, D., Vaduva, C., Harabor, A., Adam, A.-M., Harabor, V., Nechita, A., Strobescu, C., Mogos, R., Carauleanu, A., Vasilache, I.-A., & Socolov, D. (2023). Unraveling the Efficacy of Therapeutic Interventions for Short Cervix: Insights from a Retrospective Study for Improved Clinical Management. Medicina, 59(6), 1018. https://doi.org/10.3390/medicina59061018







