Outcomes after Percutaneous Coronary Intervention in Patients with Extremely Calcified Left Main Lesions
Abstract
1. Introduction
2. Methods
2.1. Design and Patients
2.2. Data Collection
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Baseline Population Characteristics
3.2. Procedural Details
3.3. In-Hospital Events
3.4. Follow-Up Clinical Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soleimani, A.; Abbasi, A.; Kazzazi, E.H.; Hosseini, K.; Salirifar, M.; Darabian, S.; Sadeghian, S.; Sheikhfathol-Lahi, M. Prevalence of left main coronary artery disease among patients with ischemic heart disease: Insights from the Tehran Angiography Registry. Minerva Cardioangiol. 2009, 57, 175–183. [Google Scholar] [PubMed]
- D’Ascenzo, F.; Presutti, D.G.; Picardi, E.; Moretti, C.; Omede, P.; Sciuto, F.; Novara, M.; Yan, A.T.; Goodman, S.; Mahajan, N.; et al. Prevalence and non-invasive predictors of left main or three-vessel coronary disease: Evidence from a collaborative international meta-analysis including 22 740 patients. Heart 2012, 98, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Ahn, J.M.; Chang, M.; Baek, S.; Yoon, S.H.; Kang, S.J.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; Park, S.W.; et al. Left Main Coronary Artery Disease: Secular Trends in Patient Characteristics, Treatments, and Outcomes. J. Am. Coll. Cardiol. 2016, 68, 1233–1246. [Google Scholar] [CrossRef] [PubMed]
- Levine, G.N.; Bates, E.R.; Blankenship, J.C.; Bailey, S.R.; Bittl, J.A.; Cercek, B.; Chambers, C.E.; Ellis, S.G.; Guyton, R.A.; Hollenberg, S.M.; et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J. Am. Coll. Cardiol. 2011, 58, e44–e122. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Genereux, P.; Redfors, B.; Witzenbichler, B.; Arsenault, M.P.; Weisz, G.; Stuckey, T.D.; Rinaldi, M.J.; Neumann, F.J.; Christopher Metzger, D.; Henry, T.D.; et al. Two-year outcomes after percutaneous coronary intervention of calcified lesions with drug-eluting stents. Int. J. Cardiol. 2017, 231, 61–67. [Google Scholar] [CrossRef]
- Madhavan, M.V.; Tarigopula, M.; Mintz, G.S.; Maehara, A.; Stone, G.W.; Genereux, P. Coronary artery calcification: Pathogenesis and prognostic implications. J. Am. Coll. Cardiol. 2014, 63, 1703–1714. [Google Scholar] [CrossRef]
- Bourantas, C.V.; Zhang, Y.J.; Garg, S.; Iqbal, J.; Valgimigli, M.; Windecker, S.; Mohr, F.W.; Silber, S.; Vries, T.; Onuma, Y.; et al. Prognostic implications of coronary calcification in patients with obstructive coronary artery disease treated by percutaneous coronary intervention: A patient-level pooled analysis of 7 contemporary stent trials. Heart 2014, 100, 1158–1164. [Google Scholar] [CrossRef]
- Wang, X.; Matsumura, M.; Mintz, G.S.; Lee, T.; Zhang, W.; Cao, Y.; Fujino, A.; Lin, Y.; Usui, E.; Kanaji, Y.; et al. In Vivo Calcium Detection by Comparing Optical Coherence Tomography, Intravascular Ultrasound, and Angiography. JACC Cardiovasc. Imaging 2017, 10, 869–879. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology/American College of Cardiology/American Heart Association/World Heart Federation Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Glob. Heart 2018, 13, 305–338. [Google Scholar] [CrossRef]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef] [PubMed]
- Schulman, S.; Angeras, U.; Bergqvist, D.; Eriksson, B.; Lassen, M.R.; Fisher, W.; Subcommittee on Control of Anticoagulation of the Scientific; Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J. Thromb. Haemost. 2010, 8, 202–204. [Google Scholar] [CrossRef] [PubMed]
- Genereux, P.; Palmerini, T.; Caixeta, A.; Cristea, E.; Mehran, R.; Sanchez, R.; Lazar, D.; Jankovic, I.; Corral, M.D.; Dressler, O.; et al. SYNTAX score reproducibility and variability between interventional cardiologists, core laboratory technicians, and quantitative coronary measurements. Circ. Cardiovasc. Interv. 2011, 4, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Medina, A.; Suarez de Lezo, J.; Pan, M. A new classification of coronary bifurcation lesions. Rev. Esp. Cardiol. 2006, 59, 183. [Google Scholar] [CrossRef] [PubMed]
- Ungureanu, C.; Gasparini, G.L.; Aminian, A.; Blaimont, M.; Dumitrascu, S.; Lepiece, C.; Colletti, G. RailTracking: A Novel Technique to Overcome Difficult Anatomy During Transradial Approach. J. Invasive Cardiol. 2022, 34, E757–E762. [Google Scholar] [PubMed]
- Darabian, S.; Blaha, M.; Whelton, S.; Homat, A.; Vahoumeni, R.; Nozari, Y.; Li, D.; Nakanishi, R.; Hamal, S.; Budoff, M.J. Abstract 15181: Left Main Calcified Lesions as a Strong Predictor of All-Cause Death. Circulation 2013, 128, A15181. [Google Scholar] [CrossRef]
- Kang, S.J.; Ahn, J.M.; Song, H.; Kim, W.J.; Lee, J.Y.; Park, D.W.; Yun, S.C.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; et al. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ. Cardiovasc. Interv. 2011, 4, 562–569. [Google Scholar] [CrossRef]
- Ielasi, A.; Kawamoto, H.; Latib, A.; Boccuzzi, G.G.; Sardella, G.; Garbo, R.; Meliga, E.; D’Ascenzo, F.; Presbitero, P.; Nakamura, S.; et al. In-Hospital and 1-Year Outcomes of Rotational Atherectomy and Stent Implantation in Patients With Severely Calcified Unprotected Left Main Narrowings (from the Multicenter ROTATE Registry). Am. J. Cardiol. 2017, 119, 1331–1337. [Google Scholar] [CrossRef]
- Chiang, M.H.; Yi, H.T.; Tsao, C.R.; Chang, W.C.; Su, C.S.; Liu, T.J.; Liang, K.W.; Ting, C.T.; Lee, W.L. Rotablation in the treatment of high-risk patients with heavily calcified left-main coronary lesions. J. Geriatr. Cardiol. 2013, 10, 217–225. [Google Scholar] [CrossRef]
- Garcia-Lara, J.; Pinar, E.; Valdesuso, R.; Lacunza, J.; Gimeno, J.R.; Hurtado, J.A.; Valdes-Chavarri, M. Percutaneous coronary intervention with rotational atherectomy for severely calcified unprotected left main: Immediate and two-years follow-up results. Catheter. Cardiovasc. Interv. 2012, 80, 215–220. [Google Scholar] [CrossRef]
- Yabushita, H.; Takagi, K.; Tahara, S.; Fujino, Y.; Warisawa, T.; Kawamoto, H.; Watanabe, Y.; Mitomo, S.; Karube, K.; Matsumoto, T.; et al. Impact of rotational atherectomy on heavily calcified, unprotected left main disease. Circ. J. 2014, 78, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, A.S.; Narayanan, M.R.; Tun, H.; Hindoyan, A.; Matthews, R.; Mehra, A.; Shavelle, D.M.; Clavijo, L.C. In-Hospital Outcomes of Rotational Atherectomy in High-Risk Patients With Severely Calcified Left Main Coronary Artery Disease: A Single-Center Experience. J. Invasive Cardiol. 2019, 31, 101–106. [Google Scholar] [PubMed]
- Abdel-Wahab, M.; Baev, R.; Dieker, P.; Kassner, G.; Khattab, A.A.; Toelg, R.; Sulimov, D.; Geist, V.; Richardt, G. Long-term clinical outcome of rotational atherectomy followed by drug-eluting stent implantation in complex calcified coronary lesions. Catheter. Cardiovasc. Interv. 2013, 81, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Dahdouh, Z.; Roule, V.; Dugue, A.E.; Sabatier, R.; Lognone, T.; Grollier, G. Rotational atherectomy for left main coronary artery disease in octogenarians: Transradial approach in a tertiary center and literature review. J. Interv. Cardiol. 2013, 26, 173–182. [Google Scholar] [CrossRef]
- Sulimov, D.S.; Abdel-Wahab, M.; Toelg, R.; Kassner, G.; Geist, V.; Richardt, G. High-speed rotational atherectomy of the left main coronary artery: A single-center experience in 50 high-risk patients. Cardiovasc. Revasc. Med. 2015, 16, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Beohar, N.; Chen, S.; Lembo, N.J.; Banning, A.P.; Serruys, P.W.; Leon, M.B.; Morice, M.C.; Genereux, P.; Kandzari, D.E.; Kappetein, A.P.; et al. Impact of lesion preparation strategies on outcomes of left main PCI: The EXCEL trial. Catheter. Cardiovasc. Interv. 2021, 98, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Hansen, S.; Meincke, F.; Frerker, C.; Kuck, K.H.; Bergmann, M.W. Safety and efficacy of lesion preparation with the AngioSculpt Scoring Balloon in left main interventions: The ALSTER Left Main registry. EuroIntervention 2016, 11, 1346–1354. [Google Scholar] [CrossRef]
- Nassar, H.; Gotsman, I.; Gerganski, P.; Moseri, M.; Lotan, C.; Gotsman, M. Cutting balloon angioplasty and stent implantation for aorto-ostial lesions: Clinical outcome and 1-year follow-up. Clin. Cardiol. 2009, 32, 183–186. [Google Scholar] [CrossRef]
- Cimci, M.; Iglesias, J.F.; Huber, C.; Mach, F.; Roffi, M. Intravascular lithotripsy to treat an ostial left main coronary artery stenosis due to porcelain aorta in a patient with congenital high-density lipoprotein deficiency. Anatol. J. Cardiol. 2020, 24, 345–346. [Google Scholar] [CrossRef]
- Agrawal, Y.; Zoltowska, D.; Nazroo, J.R.; Halabi, A.R. Impella-Assisted Intracoronary Lithotripsy of Severely Calcified Left Main Coronary Artery Bifurcation for NSTEMI With Cardiogenic Shock. Cureus 2021, 13, e14772. [Google Scholar] [CrossRef]
- Rola, P.; Wlodarczak, A.; Kulczycki, J.J.; Barycki, M.; Furtan, L.; Pecherzewski, M.; Szudrowicz, M.; Wlodarczak, S.; Doroszko, A.; Lesiak, M. Efficacy and safety of shockwave intravascular lithotripsy (S-IVL) in calcified unprotected left main percutaneous coronary intervention—Short-term outcomes. Postepy Kardiol. Interwencyjnej 2021, 17, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, C.S.; Wilson, S.J.; Bogle, R.; Hanratty, C.G.; Williams, R.; Walsh, S.J.; McEntegart, M.; Spratt, J.C. Intravascular lithotripsy for lesion preparation in patients with calcific distal left main disease. EuroIntervention 2020, 16, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Rola, P.; Kulczycki, J.J.; Wlodarczak, A.; Barycki, M.; Wlodarczak, S.; Szudrowicz, M.; Furtan, L.; Jastrzebski, A.; Pecherzewski, M.; Lesiak, M.; et al. Intravascular Lithotripsy as a Novel Treatment Method for Calcified Unprotected Left Main Diseases-Comparison to Rotational Atherectomy-Short-Term Outcomes. Int. J. Environ. Res. Public Health 2022, 19, 9011. [Google Scholar] [CrossRef] [PubMed]
- Buono, A.; Basavarajaiah, S.; Choudhury, A.; Lee, L.; Bhatia, G.; Hailan, A.; Sharma, V.; Upadhyaya, S.; Naneishvili, T.; Ielasi, A. “RotaTripsy” for Severe Calcified Coronary Artery Lesions: Insights From a Real-World Multicenter Cohort. Cardiovasc. Revasc Med. 2022, 37, 78–81. [Google Scholar] [CrossRef]
- Tamburino, C.; Capranzano, P.; Capodanno, D.; Tagliareni, F.; Biondi-Zoccai, G.; Sanfilippo, A.; Caggegi, A.; Barrano, G.; Monaco, S.; Tomasello, S.D.; et al. Plaque distribution patterns in distal left main coronary artery to predict outcomes after stent implantation. JACC Cardiovasc. Interv. 2010, 3, 624–631. [Google Scholar] [CrossRef]
- Stone, G.W.; Kappetein, A.P.; Sabik, J.F.; Pocock, S.J.; Morice, M.C.; Puskas, J.; Kandzari, D.E.; Karmpaliotis, D.; Brown, W.M., 3rd; Lembo, N.J.; et al. Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N. Engl. J. Med. 2019, 381, 1820–1830. [Google Scholar] [CrossRef]
- Holm, N.R.; Makikallio, T.; Lindsay, M.M.; Spence, M.S.; Erglis, A.; Menown, I.B.A.; Trovik, T.; Kellerth, T.; Kalinauskas, G.; Mogensen, L.J.H.; et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: Updated 5-year outcomes from the randomised, non-inferiority NOBLE trial. Lancet 2020, 395, 191–199. [Google Scholar] [CrossRef]
- D’Ascenzo, F.; De Filippo, O.; Elia, E.; Doronzo, M.P.; Omede, P.; Montefusco, A.; Pennone, M.; Salizzoni, S.; Conrotto, F.; Gallone, G.; et al. Percutaneous vs. surgical revascularization for patients with unprotected left main stenosis: A meta-analysis of 5-year follow-up randomized controlled trials. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 476–485. [Google Scholar] [CrossRef]
- Park, S.; Park, S.-J.; Park, D.-W. Percutaneous Coronary Intervention for Left Main Coronary Artery Disease. JACC Asia 2022, 2, 119–138. [Google Scholar] [CrossRef]
- Park, S.J.; Kim, Y.H.; Park, D.W.; Lee, S.W.; Kim, W.J.; Suh, J.; Yun, S.C.; Lee, C.W.; Hong, M.K.; Lee, J.H.; et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ. Cardiovasc. Interv. 2009, 2, 167–177. [Google Scholar] [CrossRef]
- De la Torre Hernandez, J.M.; Baz Alonso, J.A.; Gomez Hospital, J.A.; Alfonso Manterola, F.; Garcia Camarero, T.; Gimeno de Carlos, F.; Roura Ferrer, G.; Recalde, A.S.; Martinez-Luengas, I.L.; Gomez Lara, J.; et al. Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: Pooled analysis at the patient-level of 4 registries. JACC Cardiovasc. Interv. 2014, 7, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.J.; Pang, S.; Chen, X.Y.; Bourantas, C.V.; Pan, D.R.; Dong, S.J.; Wu, W.; Ren, X.M.; Zhu, H.; Shi, S.Y.; et al. Comparison of intravascular ultrasound guided versus angiography guided drug eluting stent implantation: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2015, 15, 153. [Google Scholar] [CrossRef]
- Andell, P.; Karlsson, S.; Mohammad, M.A.; Gotberg, M.; James, S.; Jensen, J.; Frobert, O.; Angeras, O.; Nilsson, J.; Omerovic, E.; et al. Intravascular Ultrasound Guidance Is Associated With Better Outcome in Patients Undergoing Unprotected Left Main Coronary Artery Stenting Compared With Angiography Guidance Alone. Circ. Cardiovasc. Interv. 2017, 10, e004813. [Google Scholar] [CrossRef] [PubMed]
- Finet, G.; Gilard, M.; Perrenot, B.; Rioufol, G.; Motreff, P.; Gavit, L.; Prost, R. Fractal geometry of arterial coronary bifurcations: A quantitative coronary angiography and intravascular ultrasound analysis. EuroIntervention 2008, 3, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Genereux, P.; Palmerini, T.; Caixeta, A.; Rosner, G.; Green, P.; Dressler, O.; Xu, K.; Parise, H.; Mehran, R.; Serruys, P.W.; et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: The residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J. Am. Coll. Cardiol. 2012, 59, 2165–2174. [Google Scholar] [CrossRef] [PubMed]
- Farooq, V.; Serruys, P.W.; Bourantas, C.V.; Zhang, Y.; Muramatsu, T.; Feldman, T.; Holmes, D.R.; Mack, M.; Morice, M.C.; Stahle, E.; et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 2013, 128, 141–151. [Google Scholar] [CrossRef] [PubMed]
| Total n = 70 | CdD n = 22 | rLM n = 48 | p-Value | |
|---|---|---|---|---|
| Age | 66.54 ± 10.32 | 68.64 ± 7.63 | 65.58 ± 11.29 | 0.28 |
| Male sex | 50 (71.4%) | 16 (72.7%) | 34 (70.8%) | 0.87 |
| Diabetes | 26 (37.1%) | 8 (36.4%) | 18 (37.5%) | 0.92 |
| Insulin | 8 (11.4%) | 2 (9.1%) | 6 (12.5%) | 0.67 |
| BMI | 29.27 ± 5.22 | 30.68 ± 5.14 | 28.63 ± 5.19 | 0.13 |
| Hypercholesterolemia | 69 (98.6) | 21 (95.5%) | 48 (100%) | 0.13 |
| Arterial hypertension | 63 (90%) | 20 (90.9%) | 43 (89.6%) | 0.86 |
| Peripheral Arterial Disease | 9 (12.9%) | 4 (18.2%) | 5 (10.4%) | 0.36 |
| Malignancy | 8 (11.4%) | 3 (13.6%) | 5 (10.4%) | 0.69 |
| Active smoker | 16 (22.9%) | 3 (13.6%) | 13 (27.1%) | 0.21 |
| CrCl < 60 mL/min/1.73 m2 | 6 (8.6%) | 2 (9.1%) | 4 (8.3%) | 0.91 |
| Dialysis | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Previous PCI | 22 (31.4%) | 10 (45.4%) | 12 (25%) | 0.30 |
| Previous CABG | 0 | 0 | 0 | |
| LVEF (%) | 49 ±7.1 | 48.41 ± 6.43 | 49.38 ± 7.55 | 0.34 |
| Clinical Presentation | 0.49 | |||
| Stable angina | 41 (58.6%) | 15 (68.2%) | 26 (54.2%) | |
| Non-STE ACS | 17 (24.3%) | 4 (18.2%) | 13 (27.1%) | |
| STEMI | 3 (4.3%) | 0 | 3 (6.3%) | |
| Silent ischemia | 9 (12.9%) | 3 (13.6%) | 6 (12.5%) | |
| PCI in previous 30 days | 7 (10%) | 3 (13.6%) | 4 (8.3%) | 0.98 |
| Total n = 70 | CdD n = 22 | rLM n = 48 | p-Value | |
|---|---|---|---|---|
| Timing | 0.03 | |||
| Ad-hoc | 19 (27.1%) | 3 (13.6%) | 16 (33.3%) | |
| Elective | 51 (72.9%) | 19 (86.4%) | 32 (66.7%) | |
| SYNTAX Score | 28.45 ± 8.89 | 29.18 ± 9.92 | 28.11 ± 8.47 | 0.84 |
| SYNTAX Score >32 | 22 (31.4%) | 8 (36.3%) | 14 (29.1%) | 0.17 |
| Pharmacological support before procedure | 2 (2.9%) | 0 | 2 (4.2%) | 0.49 |
| MCS before procedure | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Type of MCS | ECMO | n/a | ECMO | |
| Transradial | 61 (87.1%) | 19 (86.3%) | 42 (87.5%) | 0.52 |
| Distal radial | 45 (64.2%) | 16 (72.7%) | 29 (60.4%) | 0.42 |
| Sheathless system | 0.34 | |||
| Total | 47 (67.1%) | 16 (72.7%) | 31 (64.5%) | |
| 7F | 36 (51.4%) | 14 (63.6%) | 22 (45.8%) | |
| 6F | 11 (15.7%) | 2 (9.1%) | 9 (18.8%) | |
| Catheter size | 0.19 | |||
| 7F | 59 (84.3%) | 19 (86.3%) | 40 (83.3%) | |
| 8F | 1 (1.4%) | 1 (4.5%) | 0 | |
| Branching | 0.87 | |||
| Bifurcation | 67 (95.7%) | 22 (100%) | 45 (93.8%) | |
| Trifurcation | 3 (4.3%) | 0 | 3 (6.3%) | |
| LM stenosis ≥70% | 36 (51.4%) | 13 (59.1%) | 23 (47.9%) | 0.38 |
| Three-vessel disease | 25 (35.7%) | 8 (36.3%) | 17 (35.4%) | 0.94 |
| Distal bifurcation angle | 0.48 | |||
| <45° | 3 (4.3%) | 0 | 3 (6.3%) | |
| 45–70° | 27 (38.6%) | 9 (40.9%) | 18 (37.5%) | |
| >70° | 40 (57.1%) | 13 (59.1%) | 27 (56.3%) | |
| LM ostial involved | 6 (8.6%) | 2 (9.1%) | 4 (8.3%) | 0.91 |
| LM body shaft only | 5 (7.1%) | 1 (4.5%) | 4 (8.3%) | 0.56 |
| Medina Classification | 0.61 | |||
| 1,1,0 | 39 (55.7%) | 10 (45.5%) | 29 (60.4%) | |
| 1,1,1 | 17 (24.3%) | 6 (27.3%) | 11 (22.9%) | |
| 1,0,1 | 6 (8.6%) | 3 (13.6%) | 3 (6.3%) | |
| 1,0,0 | 6 (8.6%) | 3 (13.6%) | 3 (6.3%) | |
| 0,0,1 | 1 (1.4%) | 0 | 1 (2.1%) | |
| Angiographic LM calcification | 0.02 | |||
| No/mild | 30 (42.8%) | 2 (9.1%) | 28 (58.3%) | |
| Moderate | 23 (32.9%) | 7 (31.8%) | 16 (33.3%) | |
| Severe | 17 (24.2%) | 13 (59.1%) | 4 (8.3%) | |
| Eccentric calcification | 19 (27.1%) | 7 (31.8%) | 12 (25%) | 0.55 |
| Lesion thrombus | 3 (4.3%) | 0 | 3 (6.3%) | 0.23 |
| LM in-stent restenosis | 1 (4.3%) | 0 | 1 (2.1%) | 0.49 |
| Total n = 70 | CdD n = 22 | rLM n = 48 | p-Value | |
|---|---|---|---|---|
| LM only PCI | 29 (41.4%) | 9 (40.9%) | 20 (41.7%) | 0.95 |
| Stent LM towards | 0.14 | |||
| CX | 6 (8.6%) | 3 (13.6%) | 3 (6.3%) | |
| LAD | 64 (91.4%) | 19 (86.4%) | 45 (93.8%) | |
| LM pharmacological balloon | 1 (1.4%) | 0 | 1 (2.1%) | |
| LM non-bifurcation stenting | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Bifurcation 1-stent | 51 (72.9%) | 16 (72.7%) | 35 (72.9%) | 0.98 |
| Bifurcation 2-stents | 17 (24.3%) | 6 (27.3%) | 11 (22.9%) | 0.69 |
| 2-stent technique | 0.54 | |||
| DK-Crush | 11 (15.7%) | 4 (18.2%) | 7 (14.6%) | |
| TAP | 3 (4.3%) | 1 (4.5%) | 2 (4.2%) | |
| Culotte | 1 (1.4%) | 0 | 1 (2.1%) | |
| Nano-Crush | 2 (2.9%) | 1 (4.5%) | 1 (2.1%) | |
| LM pre-dilation | 70 (100%) | 22 (100%) | 48 (100%) | |
| Pre-dilation balloon size | 3.19 ± 0.35 | 3.09 ± 0.33 | 3.24 ± 0.35 | 0.13 |
| Pre-dilation pressure | 20.1 ± 2.2 | 21.2 ± 2.5 | 18.8 ± 1.9 | 0.08 |
| Pre-dilation SB | 17 (24.3%) | 6 (27.3%) | 11 (22.9%) | 0.74 |
| LM stent diameter | 3.58 ± 0.24 | 3.55 ± 0.21 | 3.59 ± 0.26 | 0.4 |
| SB stent diameter | 3.01 ± 0.32 | 2.96 ± 0.33 | 3.05 ± 0.33 | 0.66 |
| LM stent length | 36.48 ± 16.25 | 37.27 ± 17.54 | 36.11 ± 15.79 | 0.86 |
| POT balloon diameter | 5.25 ± 0.43 | 5.41 ± 0.36 | 5.18 ± 0.44 | 0.03 |
| Tri-kissing | 2 (2.9%) | 0 | 2 (4.2%) | 0.28 |
| SB stenting required | 1 (1.4%) | 0 | 1 (2.1%) | 0.56 |
| SB bailout stenting technique | T-stenting | n/a | T-stenting | |
| Covered LM ostium | 67 (95.7%) | 21 (95.5%) | 46 (95.8%) | 0.94 |
| Final KBD | 67 (95.7%) | 22 (100%) | 45 (93.8%) | 0.23 |
| MB KBD diameter | 3.70 ± 0.24 | 3.7 ± 0.27 | 3.70 ± 0.23 | 0.93 |
| SB KBD diameter | 3.02 ± 0.36 | 2.99 ± 0.43 | 3.04 ± 0.32 | 0.35 |
| Re-POT | 17 (24.3%) | 6 (27.3%) | 11 (22.9%) | 0.69 |
| Stent Name | 0.02 | |||
| Synergy MegatronTM (Boston Sci.) | 39 (55.7%) | 18 (81.8%) | 21 (43.8%) | |
| XienceTM (Abbott) | 29 (41.4%) | 4 (18.2%) | 25 (52.1%) | |
| Promus EliteTM (Boston Sci.) | 1 (1.4%) | 0 | 1 (2.1%) | |
| Angiographic success | 70 (100%) | 22 (100%) | 48 (100%) | |
| Complications during LM PCI | 1 (1.4%) | 0 | 1 (2.1%) | 0.56 |
| Type of complication | Stent longitudinal compression—1 (1.4%) | n/a | Stent longitudinal compression—1 (2.1%) | |
| Treatment of complication | Re-POT—1 (1.4%) | n/a | Re-POT—1 (2.1%) | |
| Pharm. support initiated during procedure | 0 | 0 | 0 | |
| MCS initiated during procedure | 0 | 0 | 0 | |
| Procedure time (s) | 76.54 ± 36.5 | 93.18 ± 42.29 | 69.92 ± 31.15 | 0.02 |
| Fluoroscopy time (s) | 1579 ± 686.9 | 1865.18 ± 699.8 | 1448.19 ± 646.65 | 0.16 |
| Total dose area product (mGy.m2) | 8.73 ± 6.32 | 8.83 ± 5.8 | 8.69 ± 6.24 | 0.5 |
| Contrast amount (mL) | 168.57 ± 60.56 | 170.14 ± 69.88 | 167.85 ± 56.57 | 0.89 |
| Guide extension | 7 (10%) | 6 (27.3%) | 1 (2.1%) | <0.001 |
| Microcatheter | 5 (7.1%) | 3 (13.6%) | 2 (4.2%) | 0.31 |
| Intravascular imaging | ||||
| Total | 14 (20%) | 5 (22.7%) | 9 (18.8%) | 0.69 |
| IVUS | 10 (14.3%) | 4 (18.2%) | 6 (12.5%) | |
| OCT | 4 (5.7%) | 1 (4.5%) | 3 (6.3%) | |
| LM MSA (mm2) | 12.4 ± 2.1 | 12.8 ± 1.7 | 11.5 ± 2.8 | 0.24 |
| Complete revascularization | 53 (75.7%) | 17 (77.3%) | 36 (75%) | 0.83 |
| No. of other significant lesions | 2 (1–2.25) | 2 (1–2) | 2 (1–3) | 0.4 |
| Any CTO | 9 (12.9%) | 4 (18.2%) | 5 (10.4%) | 0.36 |
| Planned PCI for residual lesions | 14 (20%) | 6 (27.2%) | 8 (16.6%) | 0.21 |
| Residual SYNTAX Score ≥8 | 6 (8.5%) | 1 (4.5%) | 5 (10.4%) | 0.15 |
| Total n = 70 | CdD n = 22 | rLM n = 48 | |
|---|---|---|---|
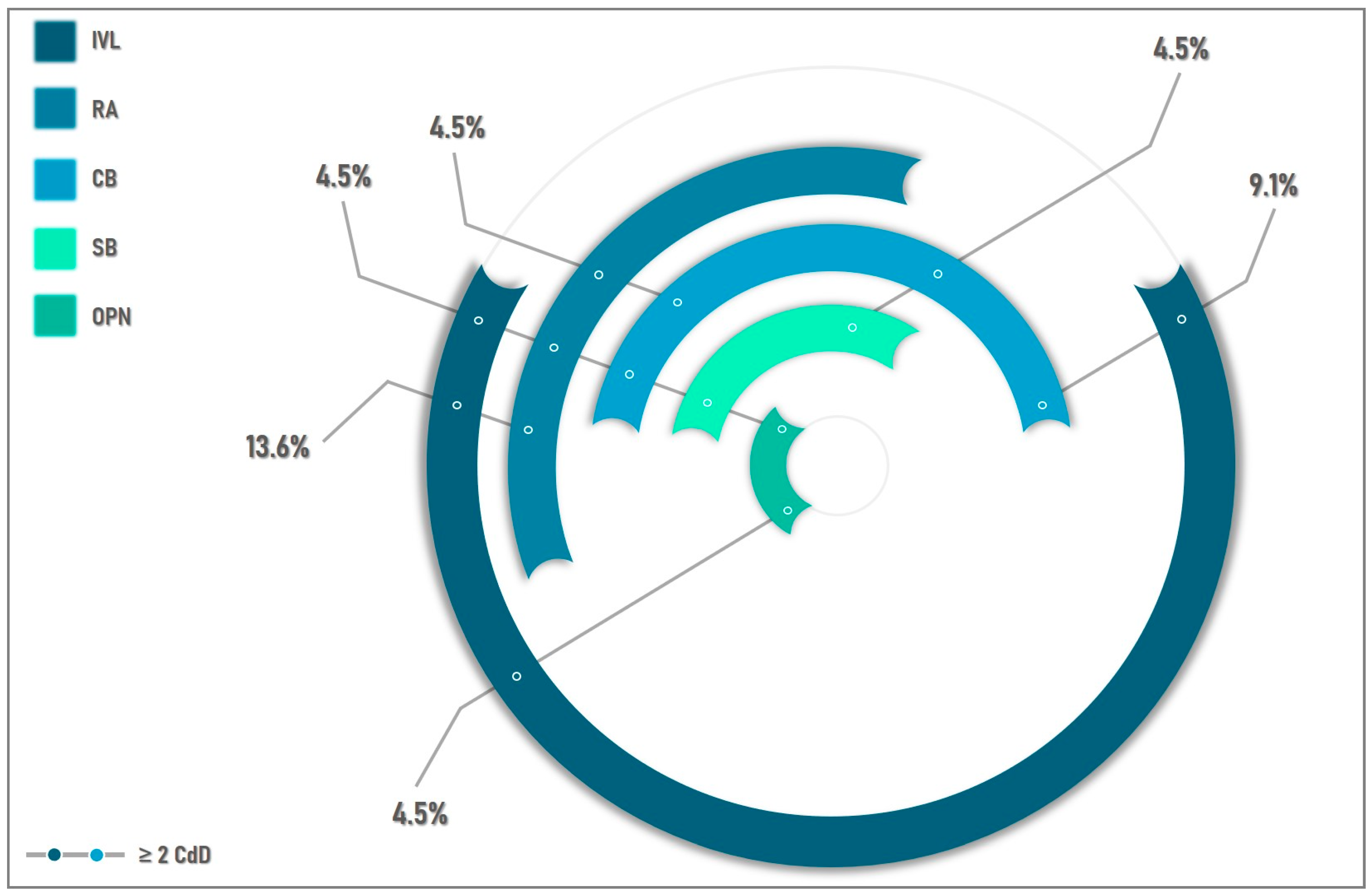
| Ca-dedicated devices | 22 (31.4%) | 22 (100%) | n/a |
| Rotational atherectomy | 9 (12.9%) | 9 (40.9%) | n/a |
| Bailout RA | 5 (7.1%) | 5 (22.7%) | n/a |
| Max. burr size | 1.75 (1.5–2) | 1.75 (1.5–2) | n/a |
| No. of burrs | |||
| 1 burr | 8 (11.4%) | 8 (36.3%) | n/a |
| 2 burrs | 1 (1.4%) | 1 (4.5%) | n/a |
| Burring LM towards | |||
| LAD | 8 (11.4%) | 8 (11.4%) | n/a |
| CX | 1 (1.4%) | 1 (1.4%) | n/a |
| IVL | 13 (18.5%) | 13 (59.1%) | n/a |
| IVL balloon size | 3.41 ± 0.49 | 3.41 ± 0.49 | n/a |
| No. of pulses on LM | 56.92 (30–80) | 56.92 (30–80) | n/a |
| IVL device crossing success | n/a | 100% | n/a |
| IVL used in >1 segment | 10 (14.2%) | 10 (45.4%) | n/a |
| Cutting Balloons | 7 (10%) | 7 (31.8%) | n/a |
| Scoring Balloon | 2 (2.8%) | 2 (9%) | n/a |
| OPN Balloon | 2 (2.8%) | 2 (9%) | n/a |
| OPN/IVL for stent under-expansion | 0 | 0 | n/a |
| Total n = 70 | CdD n = 22 | rLM n = 48 | p-Value | |
|---|---|---|---|---|
| In-hospital | ||||
| Procedural success | 70 (100%) | 22 (100%) | 48 (100%) | n/a |
| Clinical success | 70 (100%) | 22 (100%) | 48 (100%) | n/a |
| Death before discharge | 0 | 0 | 0 | n/a |
| Peri-procedural MI | 0 | 0 | 0 | n/a |
| In-hospital morbidity | 2 (2.8%) | 1 (4.5%) | 1 (2.1%) | 0.87 |
| Bleeding | 1 (1.4%) | 1 (4.5%) | 0 | |
| Access site related complication | 0 | 0 | 0 | |
| Contrast induced-nephropathy | 1 (1.4%) | 0 | 1 (2.1%) | 0.566 |
| Complication treatment | Conservative | Conservative | Conservative | |
| MACCE | 0 | 0 | 0 | n/a |
| At-discharge | ||||
| Aspirin | 70 (100%) | 22 (100%) | 48 (100%) | n/a |
| Thienopyridine | 70 (100%) | 22 (100%) | 48 (100%) | n/a |
| Clopidogrel | 42 (60%) | 14 (63.6%) | 28 (58.3%) | |
| Ticagrelor | 27 (38.6%) | 8 (36.4%) | 19 (39.6%) | |
| Prasugrel | 1 (1.4%) | 0 | 1 (2.1%) | |
| Beta-blocker | 45 (64.3%) | 10 (45.5%) | 35 (72.9%) | 0.02 |
| ACEi | 58 (82.9%) | 17 (77.3%) | 41 (85.4%) | 0.40 |
| Statins | 67 (95.7%) | 20 (90.9%) | 47 (97.9%) | 0.17 |
| Total n = 70 | CdD n = 22 | rLM n = 48 | p-Value | |
|---|---|---|---|---|
| MACCE | 3 (4.2%) | 0 | 3 (6.2%) | 0.23 |
| Cardiac death | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Non-procedural MI | 0 | 0 | 0 | n/a |
| TLR | 2 (2.8%) | 0 | 2 (4.1%) | 0.33 |
| Stroke | 0 | 0 | 0 | n/a |
| All-cause death | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Survival at 1-year | 69 (98.5%) | 22 (100%) | 47 (97.9%) | 0.49 |
| MB in-stent restenosis | 0 | 0 | 0 | n/a |
| SB restenosis | 2 (2.8%) | 0 | 2 (4.1%) | 0.33 |
| Possible ST | 1 (1.4%) | 0 | 1 (2.1%) | 0.49 |
| Hospitalization for HF | 1 (1.4%) | 0 | 1 (1.4%) | 0.49 |
| Bleeding | 4 (5.7%) | 2 (9%) | 2 (4.1%) | 0.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dumitrascu, S.; Bartos, D.; Ungureanu, C. Outcomes after Percutaneous Coronary Intervention in Patients with Extremely Calcified Left Main Lesions. Medicina 2023, 59, 825. https://doi.org/10.3390/medicina59050825
Dumitrascu S, Bartos D, Ungureanu C. Outcomes after Percutaneous Coronary Intervention in Patients with Extremely Calcified Left Main Lesions. Medicina. 2023; 59(5):825. https://doi.org/10.3390/medicina59050825
Chicago/Turabian StyleDumitrascu, Silviu, Daniela Bartos, and Claudiu Ungureanu. 2023. "Outcomes after Percutaneous Coronary Intervention in Patients with Extremely Calcified Left Main Lesions" Medicina 59, no. 5: 825. https://doi.org/10.3390/medicina59050825
APA StyleDumitrascu, S., Bartos, D., & Ungureanu, C. (2023). Outcomes after Percutaneous Coronary Intervention in Patients with Extremely Calcified Left Main Lesions. Medicina, 59(5), 825. https://doi.org/10.3390/medicina59050825







