Hyalofast Cartilage Repair Surgery with a Full Load-Bearing Rehabilitation Program One Day after Operation Reduces the Time for Professional Athletes to Return to Play
Abstract
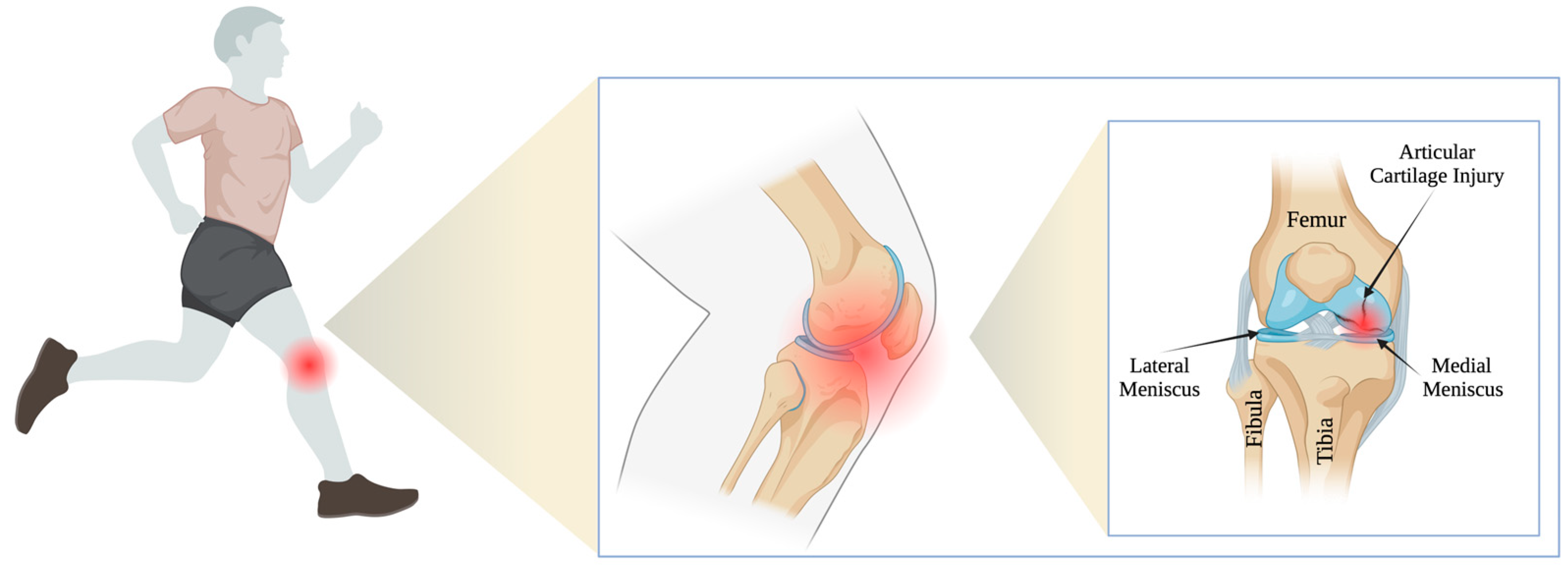
1. Introduction
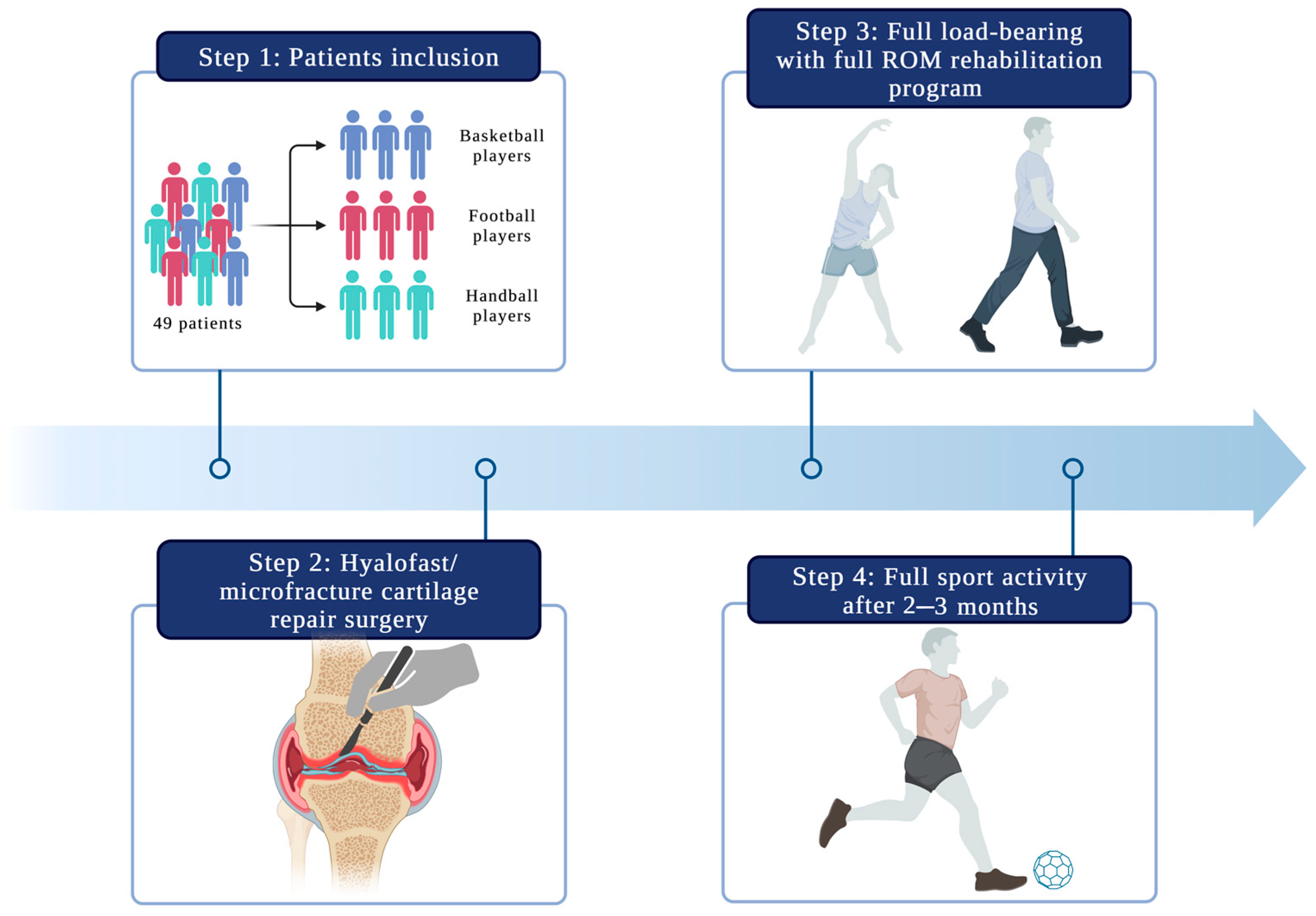
2. Materials and Methods
2.1. Patient Selection
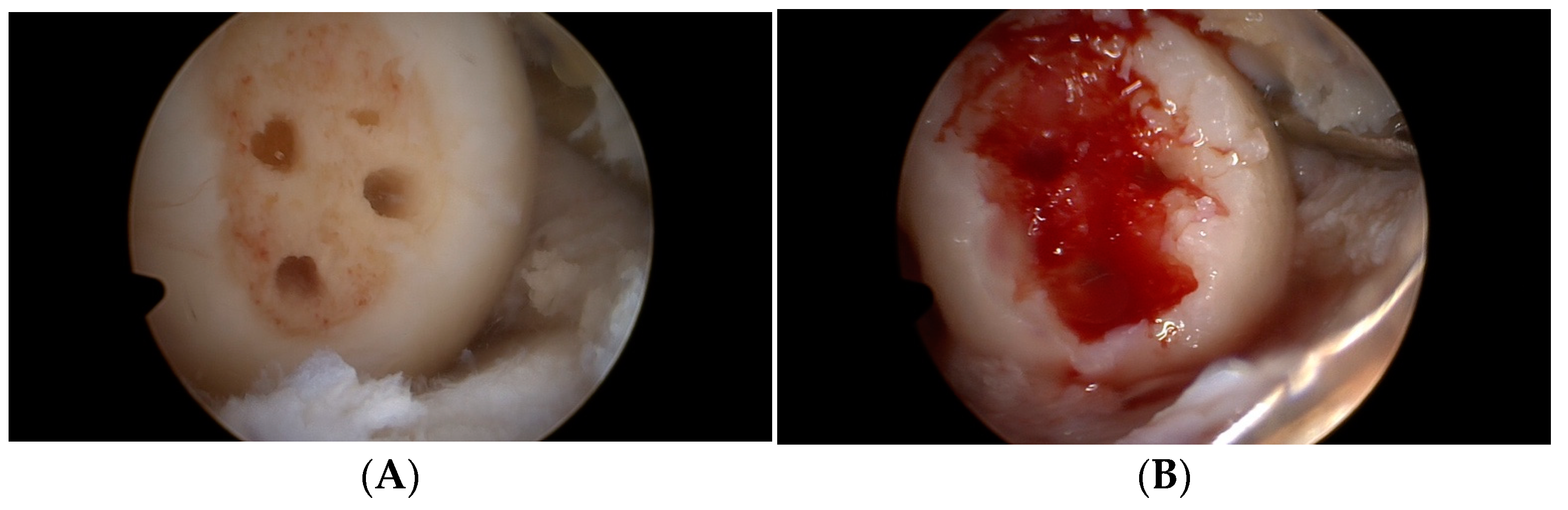
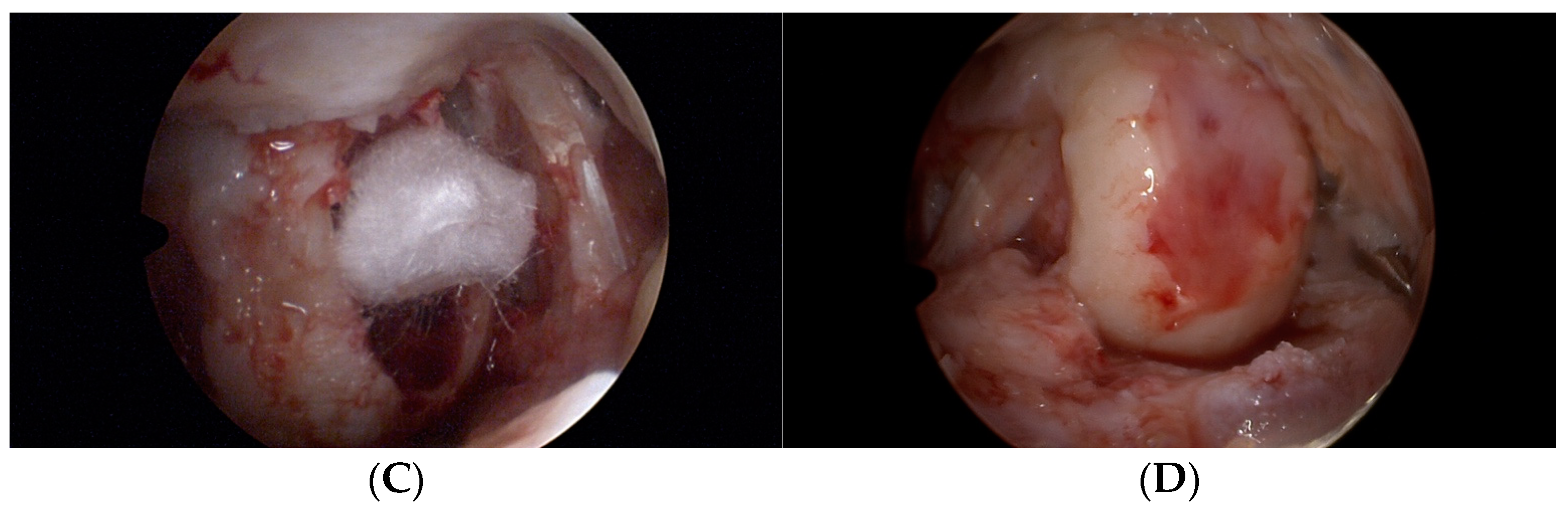
2.2. Operation Procedure
2.3. Follow-Up Evaluation
2.4. Rehabilitation Protocol
2.5. Statistics
3. Results
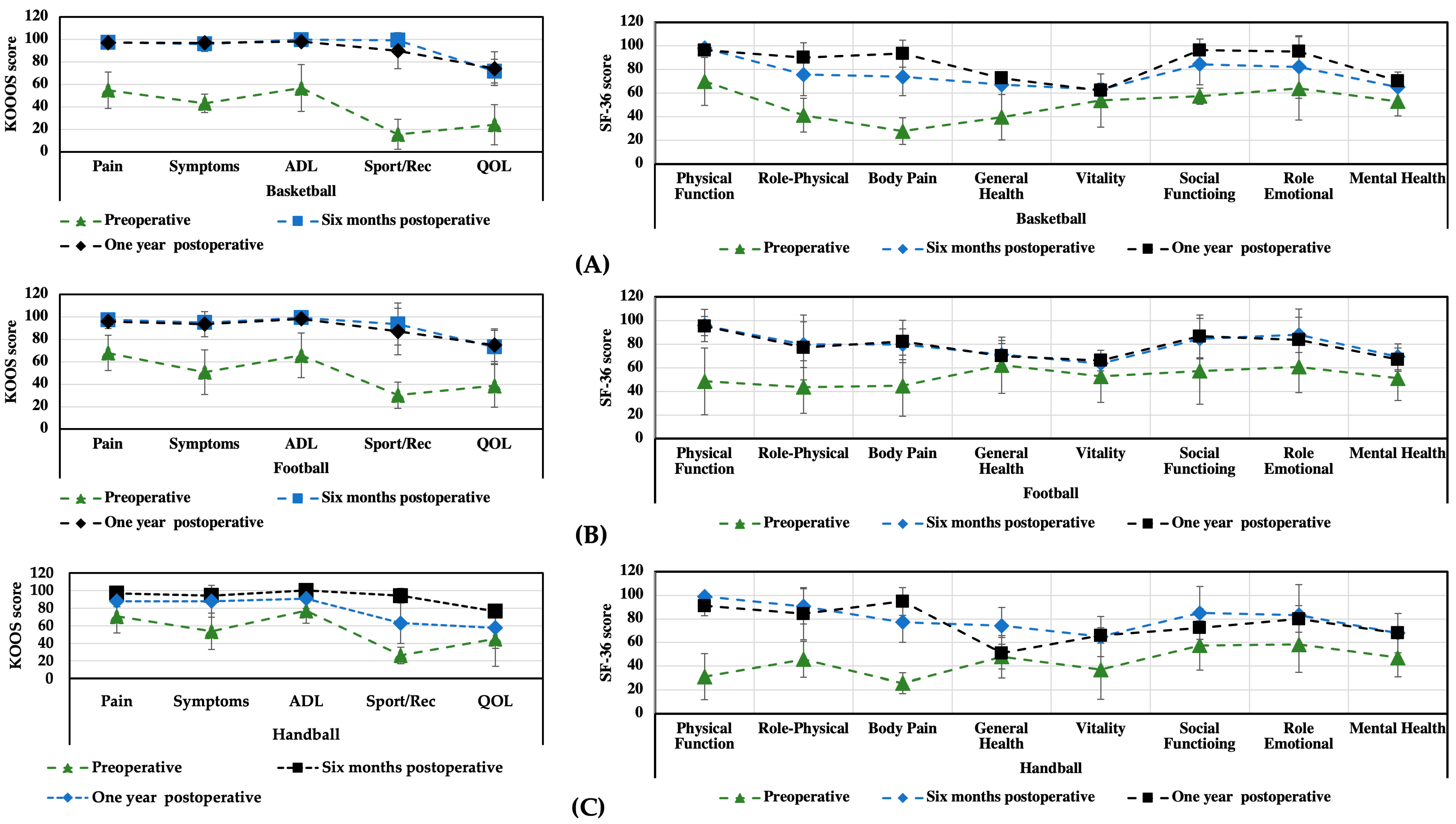
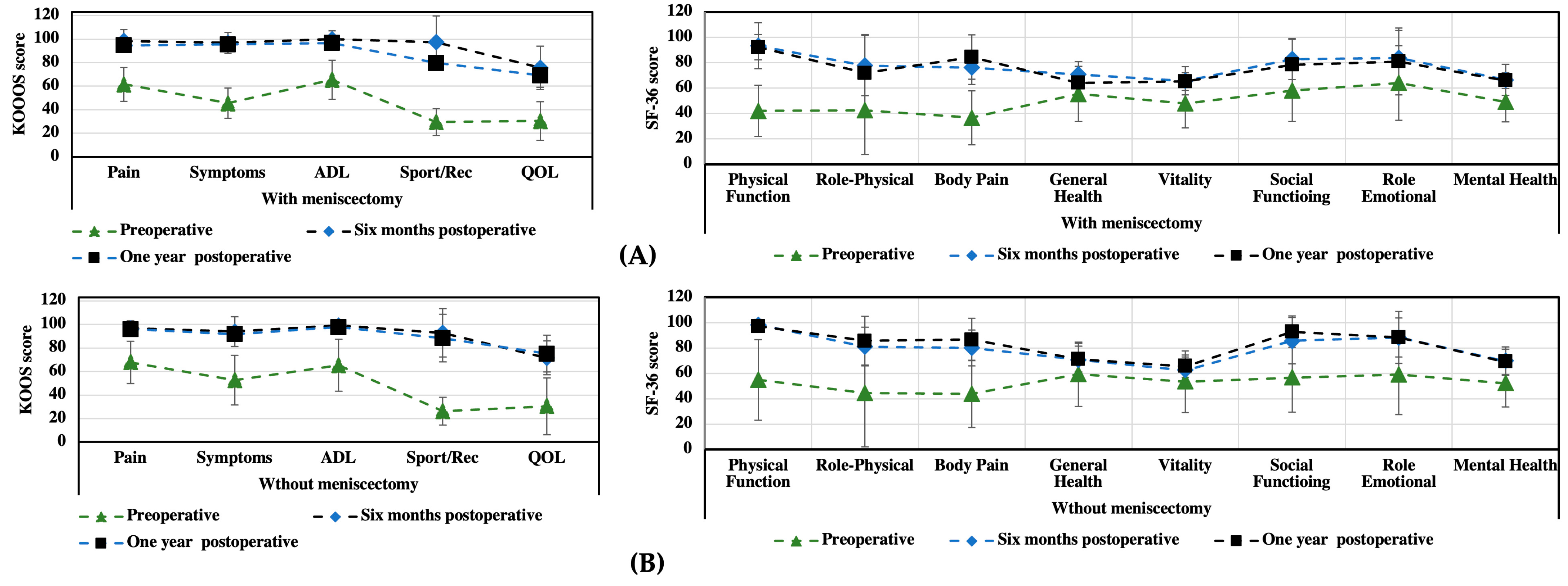
3.1. KOOS and SF-36 Scales
3.2. Functional Assessment
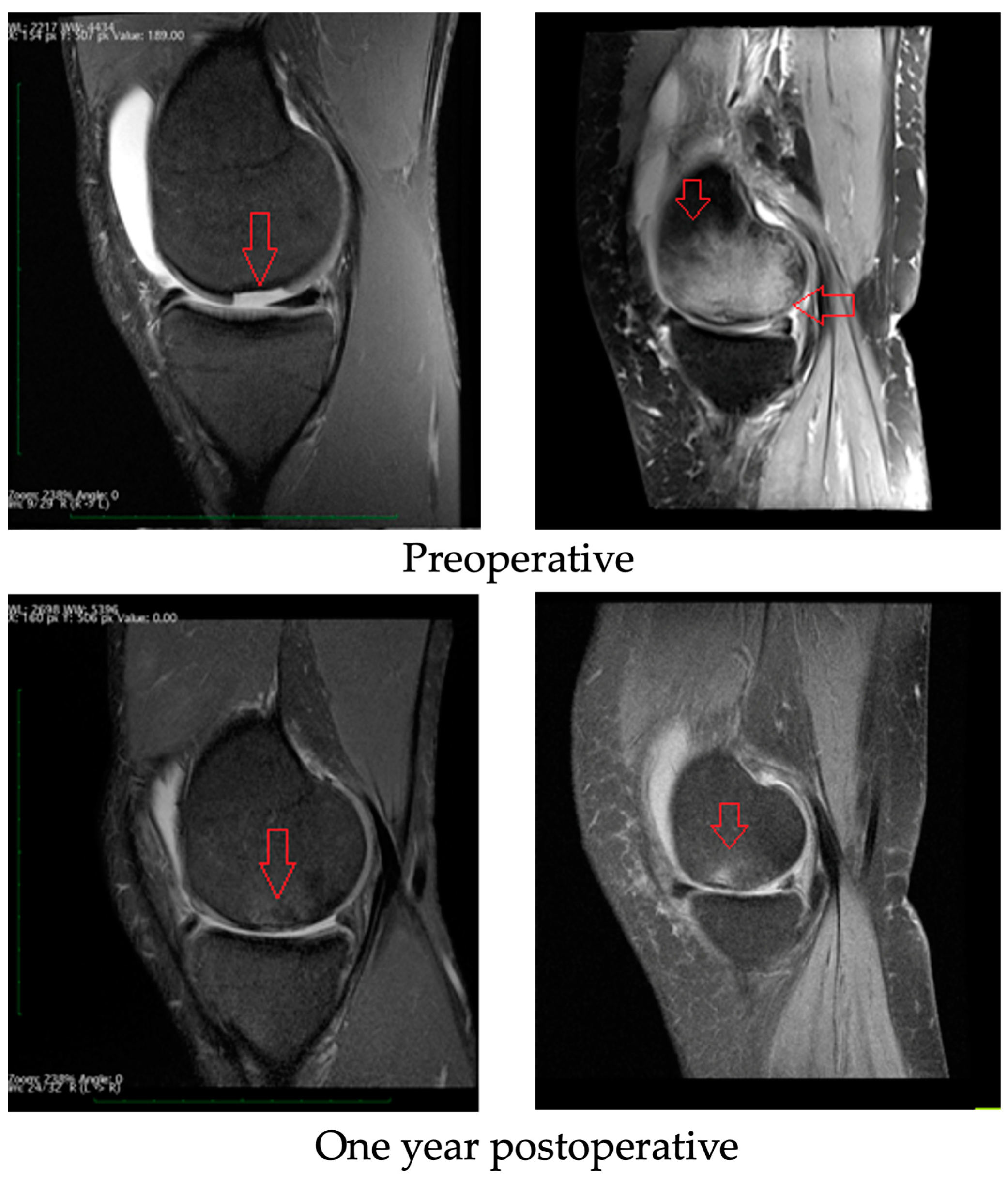
3.3. Radiological Evaluation
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steadman, J.R.; Rodkey, W.G.; Rodrigo, J.J. Microfracture: Surgical Technique and Rehabilitation to Treat Chondral Defects. Clin. Orthop. Relat. Res. 2001, 391, S362–S369. [Google Scholar] [CrossRef] [PubMed]
- Richter, D.L.; Schenck, R.C., Jr.; Wascher, D.C.; Treme, G. Knee Articular Cartilage Repair and Restoration Techniques: A Review of the Literature. Sport. Health A Multidiscip. Approach 2016, 8, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Ochi, M.; Uchio, Y.; Kawasaki, K.; Wakitani, S.; Iwasa, J. Transplantation of cartilage-like tissue made by tissue engineering in the treatment of cartilage defects of the knee. J. Bone Jt. Surg. Br. 2002, 84, 571–578. [Google Scholar] [CrossRef]
- Della Villa, S.; Kon, E.; Filardo, G.; Ricci, M.; Vincentelli, F.; Delcogliano, M.; Marcacci, M. Does Intensive Rehabilitation Permit Early Return to Sport without Compromising the Clinical Outcome after Arthroscopic Autologous Chondrocyte Implantation in Highly Competitive Athletes? Am. J. Sport. Med. 2010, 38, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zheng, J.; Meng, X.; Wang, F. Effects of Electrical Stimulation on Articular Cartilage Regeneration with a Focus on Piezoelectric Biomaterials for Articular Cartilage Tissue Repair and Engineering. Int. J. Mol. Sci. 2023, 24, 1836. [Google Scholar] [CrossRef] [PubMed]
- Barbour, K.E.; Helmick, C.G.; Theis, K.A.; Murphy, L.B.; Hootman, J.M.; Brady, T.J.; Cheng, Y.J. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2010–2012. Morb. Mortal. Wkly. Rep. 2013, 62, 869. [Google Scholar]
- Hootman, J.M.; Helmick, C.G. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006, 54, 226–229. [Google Scholar] [CrossRef]
- Kujala, U.M.; Kettunen, J.; Paananen, H.; Aalto, T.; Battié, M.C.; Impivaara, O.; Videman, T.; Sarna, S. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arthritis Rheum. 1995, 38, 539–546. [Google Scholar] [CrossRef]
- Drawer, S.; Fuller, C.W. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br. J. Sport. Med. 2001, 35, 402–408. [Google Scholar] [CrossRef]
- Roos, H. ARE THERE LONG-TERM SEQUELAE FROM SOCCER? Clin. Sport. Med. 1998, 17, 819–831. [Google Scholar] [CrossRef]
- Hori, M.; Terada, M.; Suga, T.; Isaka, T. Changes in anterior femoral articular cartilage structure in collegiate rugby athletes with and without a history of traumatic knee joint injury following a five-month competitive season. Sci. Rep. 2021, 11, 15186. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.D.; Rejeski, W.; Williamson, J.D.; Morgan, T.; Sevick, M.A.; Loeser, R.F.; Ettinger, W.H.; Messier, S.P. The Arthritis, Diet and Activity Promotion Trial (ADAPT): Design, rationale, and baseline results. Control. Clin. Trials 2003, 24, 462–480. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of Exercise Is a Major Cause of Chronic Diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed]
- Tran, G.; Smith, T.; Grice, A.; Kingsbury, S.R.; McCrory, P.; Conaghan, P.G. Does sports participation (including level of performance and previous injury) increase risk of osteoarthritis? A systematic review and meta-analysis. Br. J. Sport. Med. 2016, 50, 1459–1466. [Google Scholar] [CrossRef]
- Driban, J.B.; Hootman, J.M.; Sitler, M.R.; Harris, K.; Cattano, N.M. Is Participation in Certain Sports Associated With Knee Osteoarthritis? A Systematic Review. J. Athl. Train. 2017, 52, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Lefèvre-Colau, M.M.; Nguyen, C.; Haddad, R.; Delamarche, P.; Paris, G.; Palazzo, C.; Poiraudeau, S.; Rannou, F.; Roren, A. Is Physical Activity, Practiced as Recommended for Health Benefit, a Risk Factor for Osteoarthritis? Ann. Phys. Rehabil. Med. 2016, 59, 196–206. [Google Scholar] [CrossRef]
- Davies, M.; Judge, A.; Stokes, K.; Delmestri, A.; Kemp, S.; Arden, N.K.; Newton, J.L. Is rugby playing load predictive of lower limb osteoarthritis in former international rugby players? Osteoarthr. Cartil. 2016, 24, S533–S534. [Google Scholar] [CrossRef]
- Cavalcanti, F.M.M.D.C.; Doca, D.; Cohen, M.; Ferretti, M. UPDATING ON DIAGNOSIS AND TREATMENT OF CHONDRAL LESION OF THE KNEE. Rev. Bras. Ortop. 2012, 47, 12–20. [Google Scholar] [CrossRef]
- Talesa, G.R.; Manfreda, F.; Ceccarini, P.; Pace, V.; Antinolfi, P.; Rinonapoli, G.; Caraffa, A. The treatment of knee cartilaginous injuries: State of the art. Acta Bio Med. Atenei Parmensis. 2022, 93, 11740. [Google Scholar]
- Swan, E.R.; Lynch, T.B.; Sheean, A.J. Treatment of Cartilage Defects of the Knee in Military Tactical Athletes: An Overview of Management and Clinical Outcomes. J. Knee Surg. 2022, 35, 1165–1174. [Google Scholar] [CrossRef]
- Yang, B.W.; Brusalis, C.M.; Fabricant, P.D.; Greditzer, H.G., IV. Articular Cartilage Repair in the Knee: Postoperative Imaging. J. Knee Surg. 2021, 34, 2–10. [Google Scholar] [CrossRef]
- Dekker, T.J.; Aman, Z.S.; DePhillipo, N.N.; Dickens, J.F.; Anz, A.W.; LaPrade, R.F. Chondral Lesions of the Knee: An Evidence-Based Approach. J. Bone Jt. Surg. Am. 2021, 103, 629–645. [Google Scholar] [CrossRef] [PubMed]
- Rosneck, J.; A Higuera, C.; Tadross, N.; Krebs, V.; Barsoum, W.K. Managing knee osteoarthritis before and after arthroplasty. Clevel. Clin. J. Med. 2007, 74, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Epanomeritakis, I.E.; Lee, E.; Lu, V.; Khan, W. The Use of Autologous Chondrocyte and Mesenchymal Stem Cell Implants for the Treatment of Focal Chondral Defects in Human Knee Joints—A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2022, 23, 4065. [Google Scholar] [CrossRef]
- Cerynik, D.L.; Lewullis, G.E.; Joves, B.C.; Palmer, M.P.; Tom, J.A. Outcomes of microfracture in professional basketball players. Knee Surg. Sport. Traumatol. Arthrosc. 2009, 17, 1135–1139. [Google Scholar] [CrossRef] [PubMed]
- Namdari, S.; Baldwin, K.; Anakwenze, O.; Park, M.-J.; Huffman, G.R.; Sennett, B.J. Results and Performance after Microfracture in National Basketball Association Athletes. Am. J. Sport. Med. 2009, 37, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Gudas, R.; Gudaitė, A.; Mickevičius, T.; Masiulis, N.; Simonaitytė, R.; Čekanauskas, E.; Skurvydas, A. Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: A prospective study with a 3-year follow-up. Arthroscopy 2013, 29, 89–97. [Google Scholar] [CrossRef]
- Bugbee, W.D.; Pallante-Kichura, A.L.; Görtz, S.; Amiel, D.; Sah, R. Osteochondral allograft transplantation in cartilage repair: Graft storage paradigm, translational models, and clinical applications. J. Orthop. Res. 2016, 34, 31–38. [Google Scholar] [CrossRef]
- Bistolfi, A.; Ferracini, R.; Galletta, C.; Tosto, F.; Sgarminato, V.; Digo, E.; Vernè, E.; Massè, A. Regeneration of articular cartilage: Scaffold used in orthopedic surgery. A short handbook of available products for regenerative joints surgery. Clin. Sci. Res. Rep. 2017, 1, 1–7. [Google Scholar] [CrossRef]
- Munir, N.; McDonald, A.; Callanan, A. Integrational Technologies for the Development of Three-Dimensional Scaffolds as Platforms in Cartilage Tissue Engineering. ACS Omega 2020, 5, 12623–12636. [Google Scholar] [CrossRef]
- Yu, X.; Zhang, H.; Miao, Y.; Xiong, S.; Hu, Y. Recent strategies of collagen-based biomaterials for cartilage repair: From structure cognition to function endowment. J. Leather Sci. Eng. 2022, 4, 11. [Google Scholar] [CrossRef]
- Sánchez-Téllez, D.A.; Téllez-Jurado, L.; Rodríguez-Lorenzo, L.M. Hydrogels for Cartilage Regeneration, from Polysaccharides to Hybrids. Polymers 2017, 9, 671. [Google Scholar] [CrossRef] [PubMed]
- Prakoso, A.T.; Basri, H.; Adanta, D.; Yani, I.; Ammarullah, M.I.; Akbar, I.; Ghazali, F.A.; Syahrom, A.; Kamarul, T. The Effect of Tortuosity on Permeability of Porous Scaffold. Biomedicines 2023, 11, 427. [Google Scholar] [CrossRef]
- Putra, R.U.; Basri, H.; Prakoso, A.T.; Chandra, H.; Ammarullah, M.I.; Akbar, I.; Syahrom, A.; Kamarul, T. Level of Activity Changes Increases the Fatigue Life of the Porous Magnesium Scaffold, as Observed in Dynamic Immersion Tests, over Time. Sustainability 2023, 15, 823. [Google Scholar] [CrossRef]
- Bruyas, A.; Lou, F.; Stahl, A.M.; Gardner, M.; Maloney, W.; Goodman, S.; Yang, Y.P. Systematic characterization of 3D-printed PCL/β-TCP scaffolds for biomedical devices and bone tissue engineering: Influence of composition and porosity. J. Mater. Res. 2018, 33, 1948–1959. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Nie, W.; Li, D.; Wang, W.; Zheng, L.; Zhang, J.; Zhang, J.; Peng, C.; Mo, X.; He, C. 3D printed PCL/SrHA scaffold for enhanced bone regeneration. Chem. Eng. J. 2019, 362, 269–279. [Google Scholar] [CrossRef]
- Chen, L.; Wu, Z.; Zhou, Y.; Li, L.; Wang, Y.; Wang, Z.; Chen, Y.; Zhang, P. Biomimetic porous collagen/hydroxyapatite scaffold for bone tissue engineering. J. Appl. Polym. Sci. 2017, 134, 45271. [Google Scholar] [CrossRef]
- Hoyer, B.; Bernhardt, A.; Heinemann, S.; Stachel, I.; Meyer, M.; Gelinsky, M. Biomimetically Mineralized Salmon Collagen Scaffolds for Application in Bone Tissue Engineering. Biomacromolecules 2012, 13, 1059–1066. [Google Scholar] [CrossRef]
- Mithoefer, K.; McAdams, T.; Williams, R.J.; Kreuz, P.C.; Mandelbaum, B.R. Clinical Efficacy of the Microfracture Technique for Articular Cartilage Repair in the Knee: An Evidence-Based Systematic Analysis. Am. J. Sport. Med. 2009, 37, 2053–2063. [Google Scholar] [CrossRef]
- Mithoefer, K.; Williams, R.J.; Warren, R.F.; Wickiewicz, T.L.; Marx, R.G. High-impact athletics after knee articular cartilage repair: A prospective evaluation of the microfracture technique. Am. J. Sport. Med. 2006, 34, 1413–1418. [Google Scholar] [CrossRef]
- Steadman, J.R.; Briggs, K.K.; Rodrigo, J.J.; Kocher, M.S.; Gill, T.J.; Rodkey, W.G. Outcomes of microfracture for traumatic chondral defects of the knee: Average 11-year follow-up. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Chou, A.C.C.; Lie, D.T.T. Clinical Outcomes of an All-Arthroscopic Technique for Single-Stage Autologous Matrix-Induced Chondrogenesis in the Treatment of Articular Cartilage Lesions of the Knee. Arthrosc. Sport. Med. Rehabil. 2020, 2, e353–e359. [Google Scholar] [CrossRef] [PubMed]
- Benthien, J.P.; Behrens, P. Autologous matrix-induced chondrogenesis (AMIC). A one-step procedure for retropatellar articular resurfacing. Acta Orthop. Belg. 2010, 76, 260. [Google Scholar] [PubMed]
- Zanasi, S.; Ventura, C.; Stefano, Z.P. One Step Tissue Engineering for Cartilage Reconstruction in Severe Osteoarthritis of the Knee and Ankle: A Comprehensive Review of the Technique Resorting to Isolated BMAC or ADSCS and their Last Combination. NanoWorld J. 2017, 3, 59–65. [Google Scholar] [CrossRef]
- Kon, E.; Filardo, G.; Roffi, A.; Andriolo, L.; Marcacci, M. New trends for knee cartilage regeneration: From cell-free scaffolds to mesenchymal stem cells. Curr. Rev. Musculoskelet. Med. 2012, 5, 236–243. [Google Scholar] [CrossRef]
- Buda, R.; Vannini, F.; Cavallo, M.; Grigolo, B.; Cenacchi, A.; Giannini, S. Osteochondral Lesions of the Knee: A New One-Step Repair Technique with Bone-Marrow-Derived Cells. J. Bone Jt. Surg. 2010, 92 (Suppl. 2), 2–11. [Google Scholar] [CrossRef]
- Aytekin, K.; Zeki Esenyel, C. Cite This Article as: Aytekin K, Esenyel CZ. Comparing BST-CarGel® with Hyalofast for the Treatment of Hyaline Cartilage Defects. Eur. Arch. Med. Res. 2021, 37, 217–239. [Google Scholar] [CrossRef]
- Slynarski, K.; Deszczynski, J.; Jopowicz, R.; Krzesniak, A. Use of hyaluronan scaffold in combination with fresh bone marrow transplantation or with microfractures in treatment of cartilage defects of the knee joint. Osteoarthr. Cartil. 2014, 22, S152. [Google Scholar] [CrossRef]
- Disler, D.G.; McCauley, T.R.; Kelman, C.G.; Fuchs, M.D.; Ratner, L.M.; Wirth, C.R.; Hospodar, P.P. Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: Comparison with standard MR imaging and arthroscopy. AJR Am. J. Roentgenol. 1996, 167, 127–132. [Google Scholar] [CrossRef]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D.J. Patient Satisfaction after Total Knee Arthroplasty: Who is Satisfied and Who is Not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Bajuri, M.Y.; Sabri, S.; Mazli, N.; Sarifulnizam, F.A.; Apandi, H.M. Osteochondral Injury of the Talus Treated With Cell-Free Hyaluronic Acid-Based Scaffold (Hyalofast®)—A Reliable Solution. Cureus 2021, 13, e17928. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.K.; Ackland, T.; Ebert, J.R. Clinical Rehabilitation Guidelines for Matrix-Induced Autologous Chondrocyte Implantation on the Tibiofemoral Joint. J. Orthop. Sport. Phys. Ther. 2014, 44, 102–119. [Google Scholar] [CrossRef] [PubMed]
- Dowdy, P.; Miniaci, A.; Arnoczky, S.P.; Fowler, P.J.; Boughner, D.R. The Effect of Cast Immobilization on Meniscal Healing. Am. J. Sport. Med. 1995, 23, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, M.; Srinivasan, A.; Deschner, J.; Gassner, R.; Baliko, F.; Piesco, N.; Salter, R.; Agarwal, S. Anti-inflammatory effects of continuous passive motion on meniscal fibrocartilage. J. Orthop. Res. 2005, 23, 1165–1171. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, J.; Origuchi, T.; Okita, M.; Nakano, J.; Kato, K.; Yoshimura, T.; Izumi, S.-I.; Komori, T.; Nakamura, H.; Ida, H.; et al. Immobilization-Induced Cartilage Degeneration Mediated Through Expression of Hypoxia-Inducible Factor-1α, Vascular Endothelial Growth Factor, and Chondromodulin-I. Connect. Tissue Res. 2021, 50, 37–45. [Google Scholar] [CrossRef]
- Hurley, E.T.; Davey, M.S.; Jamal, M.S.; Manjunath, A.K.; Alaia, M.J.; Strauss, E.J. Return-to-Play and Rehabilitation Protocols following Cartilage Restoration Procedures of the Knee: A Systematic Review. Cartilage 2021, 13, 907S–914S. [Google Scholar] [CrossRef]
- Wang, H.-C.; Lin, T.-H.; Chang, N.-J.; Hsu, H.-C.; Yeh, M.-L. Continuous Passive Motion Promotes and Maintains Chondrogenesis in Autologous Endothelial Progenitor Cell-Loaded Porous PLGA Scaffolds during Osteochondral Defect Repair in a Rabbit Model. Int. J. Mol. Sci. 2019, 20, 259. [Google Scholar] [CrossRef]
- Ağır, I.; Tunçer, N.; Küçükdurmaz, F.; Gümüstaş, S.; Akgül, E.D.; Akpinar, F. Functional Comparison of Immediate and Late Weight Bearing after Ankle Bimalleolar Fracture Surgery. Open Orthop. J. 2015, 9, 188–190. [Google Scholar] [CrossRef]
- Roos, E.M.; Roos, H.P.; Lohmander, S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a Self-Administered Outcome Measure. J. Orthop. Sport. Phys. Ther. 1998, 28, 88–96. [Google Scholar] [CrossRef]
- Ware, J.E., Jr. SF-36 Health Survey Update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef]
- E Brown, W.; Potter, H.G.; Marx, R.G.; Wickiewicz, T.L.; Warren, R.F. Magnetic Resonance Imaging Appearance of Cartilage Repair in the Knee. Clin. Orthop. Relat. Res. 2004, 422, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Quiceno, G.A.J.; Riveros, P.A.S.; Perea, G.A.O.; Vergara, M.G.; Muñoz, L.F.R.; Perez, R.D.A.; Piovesan, N.O.; Salamanca, J.A.M. Satisfactory clinical outcomes with autologous matrix-induced chondrogenesis in the treatment of grade IV chondral injuries of the knee. J. ISAKOS 2022. [Google Scholar] [CrossRef]
- Gobbi, A.; Scotti, C.; Karnatzikos, G.; Mudhigere, A.; Castro, M.; Peretti, G.M. One-step surgery with multipotent stem cells and Hyaluronan-based scaffold for the treatment of full-thickness chondral defects of the knee in patients older than 45 years. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 25, 2494–2501. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, A.; Whyte, G.P. Long-term Clinical Outcomes of One-Stage Cartilage Repair in the Knee With Hyaluronic Acid–Based Scaffold Embedded With Mesenchymal Stem Cells Sourced From Bone Marrow Aspirate Concentrate. Am. J. Sport. Med. 2019, 47, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.I.; Tho, S.J.W.; Tho, K.S. Biological resurfacing of grade IV articular cartilage ulcers in knee joint with Hyalofast. J. Orthop. Surg. 2020, 28, 2309499020905158. [Google Scholar] [CrossRef]
- Brophy, R.H.; Wojahn, R.D.; Lamplot, J.D. Cartilage Restoration Techniques for the Patellofemoral Joint. J. Am. Acad. Orthop. Surg. 2017, 25, 321–329. [Google Scholar] [CrossRef]
- Redondo, M.L.; Beer, A.J.; Yanke, A.B. Cartilage Restoration: Microfracture and Osteochondral Autograft Transplantation. J. Knee Surg. 2018, 31, 231–238. [Google Scholar] [CrossRef]
- Solheim, E.; Hegna, J.; Strand, T.; Harlem, T.; Inderhaug, E. Randomized Study of Long-term (15-17 Years) Outcome After Microfracture Versus Mosaicplasty in Knee Articular Cartilage Defects. Am. J. Sport. Med. 2018, 46, 826–831. [Google Scholar] [CrossRef]
- Yen, Y.-M.; Cascio, B.; O'Brien, L.; Stalzer, S.; Millett, P.J.; Steadman, J.R. Treatment of Osteoarthritis of the Knee with Microfracture and Rehabilitation. Med. Sci. Sport. Exerc. 2008, 40, 200–205. [Google Scholar] [CrossRef]
- Mithoefer, K.; Williams, R.J.; Warren, R.F.; Potter, H.G.; Spock, C.R.; Jones, E.C.; Wickiewicz, T.L.; Marx, R.G. The Microfracture Technique for the Treatment of Articular Cartilage Lesions in the Knee. A prospective cohort study. J. Bone Jt. Surg. 2005, 87, 1911–1920. [Google Scholar] [CrossRef]
- Hambly, K.; Bobic, V.; Wondrasch, B.; Van Assche, D.; Marlovits, S. Autologous Chondrocyte Implantation Postoperative Care and Rehabilitation: Science and practice. Am. J. Sport. Med. 2006, 34, 1020–1038. [Google Scholar] [CrossRef] [PubMed]
- Mithoefer, K.; Hambly, K.; Della Villa, S.; Silvers, H.; Mandelbaum, B.R. Return to Sports Participation after Articular Cartilage Repair in the Knee. Am. J. Sport. Med. 2009, 37 (Suppl. 1), 167S–176S. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Kurdi, O.; Tauviqirrahman, M.; Winarni, T.I.; Jamari, J. Tresca stress study of CoCrMo-on-CoCrMo bearings based on body mass index using 2D computational model. J. Tribol. 2022, 33, 31–38. [Google Scholar]
| Knee Joint (n = 49) | |
|---|---|
| Age, mean ± SD | 30 ± 6.7 |
| Sporting activity | |
| Professional | 49 |
| Gender, F/M | 15/34 |
| Cause of damage | |
| Traumatic | 32 |
| Non-traumatic | 6 |
| OCD | 11 |
| Location of the lesion | |
| LFC | 29 |
| MFC | 20 |
| Size of lesion (cm2), mean ± SD | 2.96 ± 1.05 |
| Previous surgeries | 4 ACL reconstructions |
| Accompanying procedures | |
| Meniscectomy | 19 |
| Preoperative | Six Months Postoperative | One Year Postoperative | (before/after Six Months) | |
|---|---|---|---|---|
| KOOS | Mean ± SD | Mean ± SD | Mean ± SD | p |
| Patients (n) | 49 | 49 | 43 | |
| Pain intensity | 55 ± 18.2 | 96 ± 4.2 | 99.5 ± 2.3 | <0.05 |
| Symptoms | 46 ± 16.6 | 93 ± 6.5 | 98.2 ± 1.8 | <0.05 |
| Activities of daily living | 57 ± 25.5 | 99 ± 2.6 | 100 ± 0.0 | <0.05 |
| Sport/Rec | 14 ± 11.1 | 95 ± 7.7 | 99.8 ± 1.8 | <0.05 |
| Quality of life | 30 ± 18 | 76 ± 4.7 | 88 ± 8.8 | <0.05 |
| Preoperative | Six Months Postoperative | One Year Postoperative | ||
|---|---|---|---|---|
| SF-36 | Mean ± SD | Mean ± SD | Mean ± SD | (before/after Six Months) |
| Patients (n) | 49 | 49 | 43 | p |
| Physical function | 34 ± 18.5 | 95.6 ± 2.0 | 97 ± 2.5 | <0.05 |
| Role physical | 63 ± 46.5 | 76 ± 15.0 | 96 ± 3.7 | 0.345 |
| Bodily pain | 36 ± 18.7 | 78 ± 15,6 | 98 ± 2.3 | <0.05 |
| General health | 68 ± 17.1 | 70 ± 16.1 | 83 ± 15.8 | 0.401 |
| Vitality | 53 ± 20.6 | 64 ± 8.0 | 87 ± 7.1 | 0.067 |
| Social function | 64 ± 29.6 | 87 ± 13.6 | 90 ± 9.5 | 0.068 |
| Role emotional | 73 ± 42.0 | 83 ± 22.9 | 90 ± 13.3 | 0.285 |
| Mental health | 52 ± 9.8 | 68 ± 11 | 70 ± 10.8 | 0.464 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kacprzak, B.; Rosińska, K.; Siuba-Jarosz, N. Hyalofast Cartilage Repair Surgery with a Full Load-Bearing Rehabilitation Program One Day after Operation Reduces the Time for Professional Athletes to Return to Play. Medicina 2023, 59, 804. https://doi.org/10.3390/medicina59040804
Kacprzak B, Rosińska K, Siuba-Jarosz N. Hyalofast Cartilage Repair Surgery with a Full Load-Bearing Rehabilitation Program One Day after Operation Reduces the Time for Professional Athletes to Return to Play. Medicina. 2023; 59(4):804. https://doi.org/10.3390/medicina59040804
Chicago/Turabian StyleKacprzak, Bartłomiej, Karolina Rosińska, and Natalia Siuba-Jarosz. 2023. "Hyalofast Cartilage Repair Surgery with a Full Load-Bearing Rehabilitation Program One Day after Operation Reduces the Time for Professional Athletes to Return to Play" Medicina 59, no. 4: 804. https://doi.org/10.3390/medicina59040804
APA StyleKacprzak, B., Rosińska, K., & Siuba-Jarosz, N. (2023). Hyalofast Cartilage Repair Surgery with a Full Load-Bearing Rehabilitation Program One Day after Operation Reduces the Time for Professional Athletes to Return to Play. Medicina, 59(4), 804. https://doi.org/10.3390/medicina59040804







