Efficacy of Music Intervention for Dental Anxiety Disorders: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
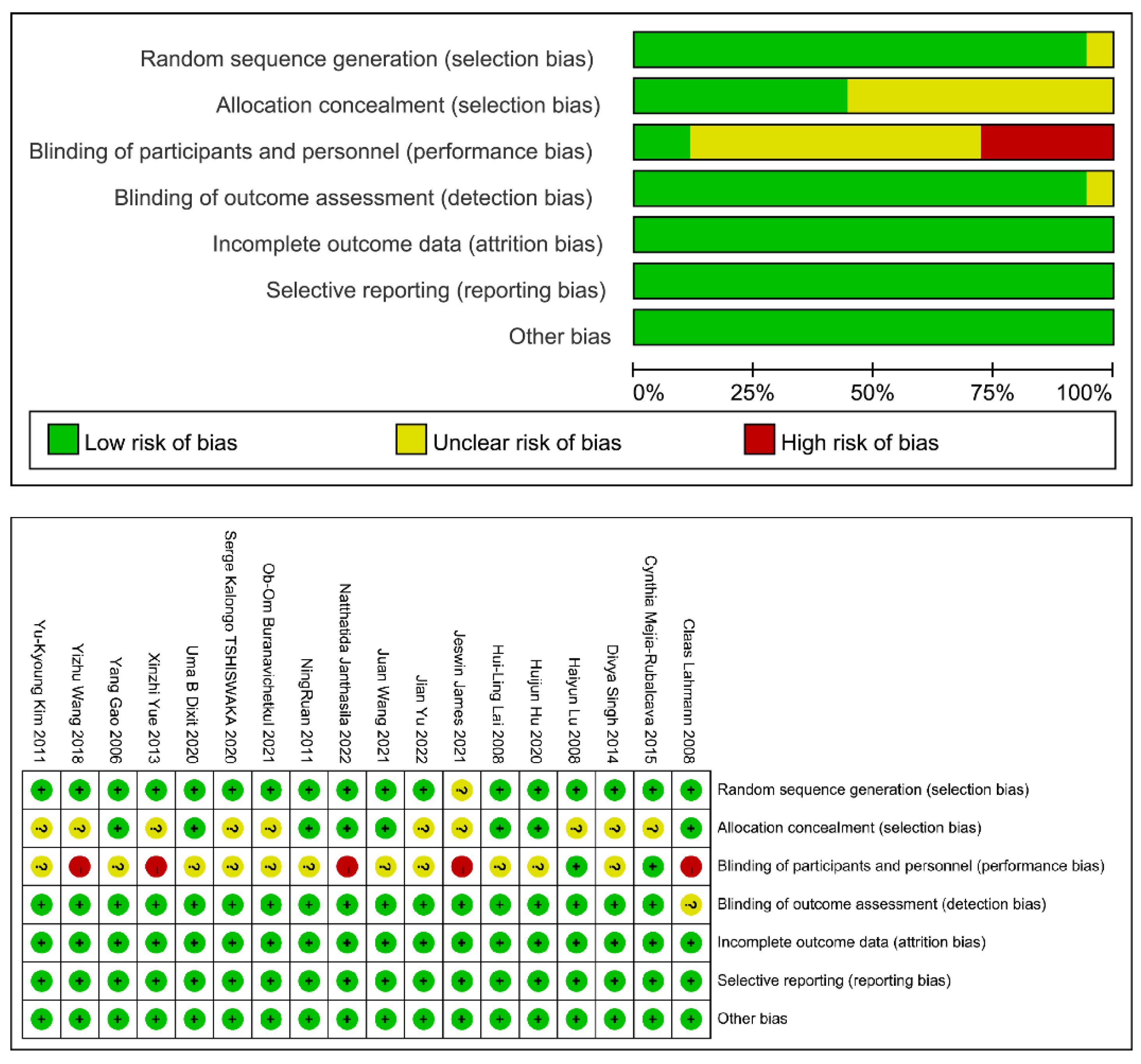
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analyses
2.5. Statement
3. Results
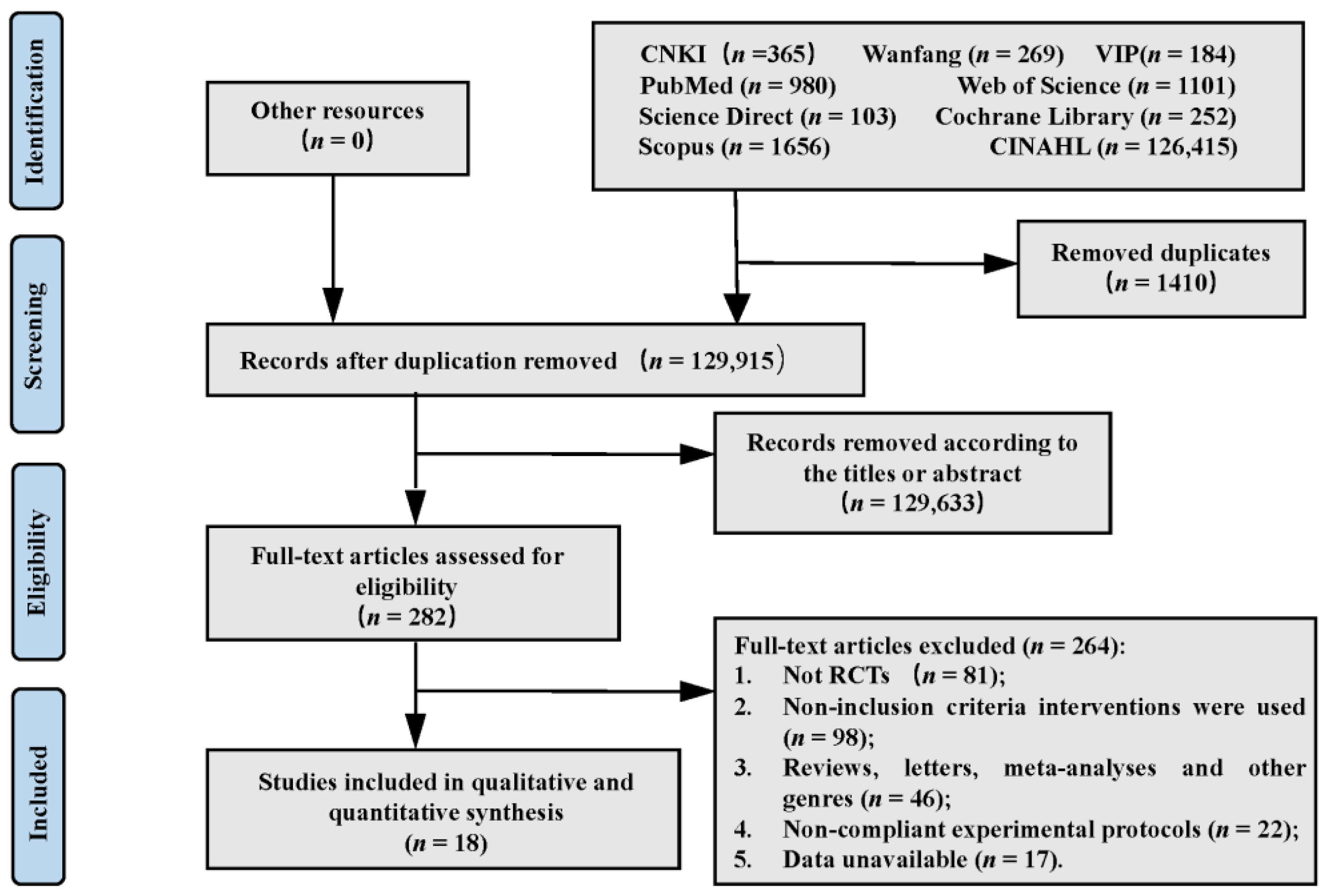
3.1. Identification of Studies
3.2. Study Outcome
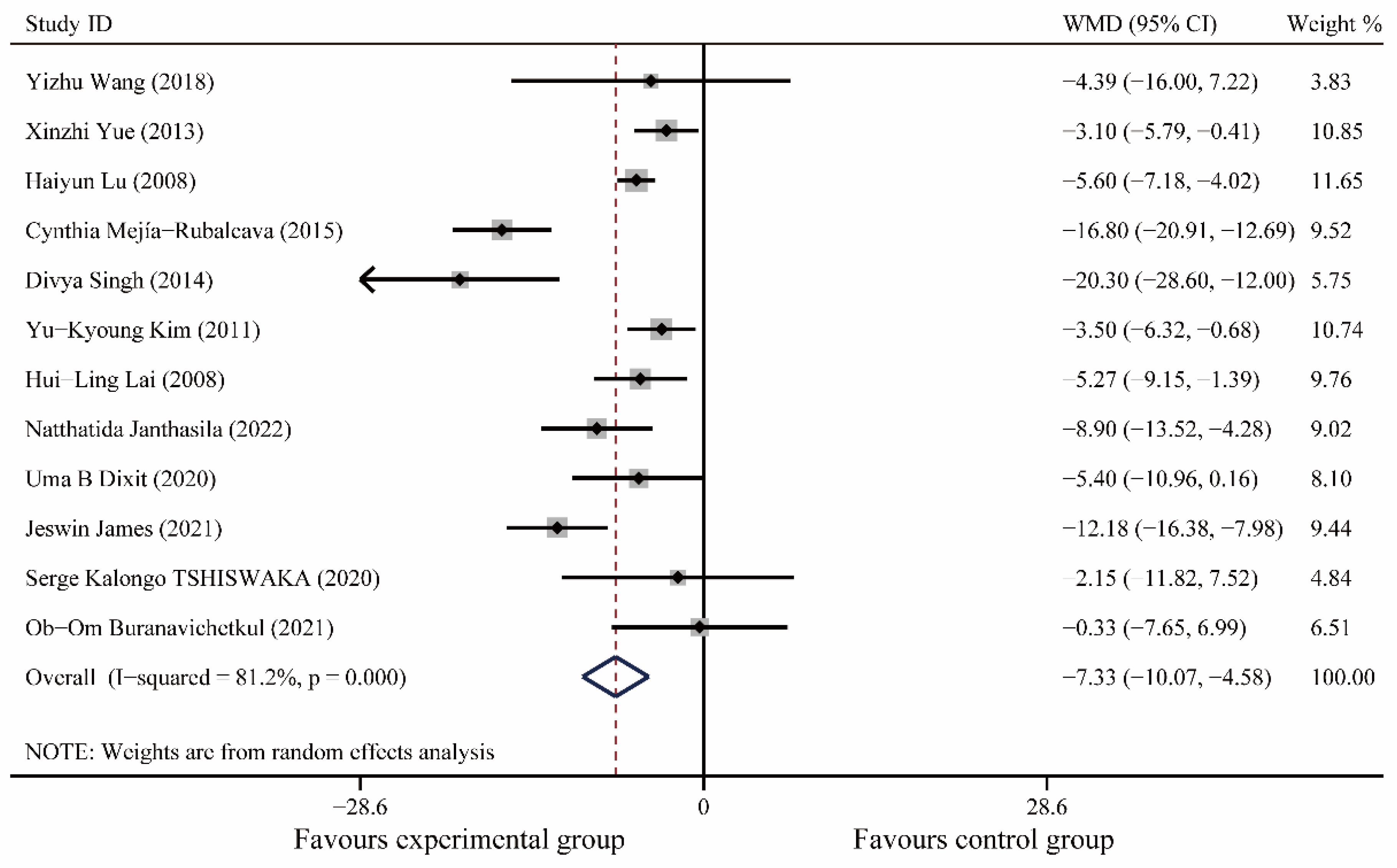
3.2.1. Heart Rate
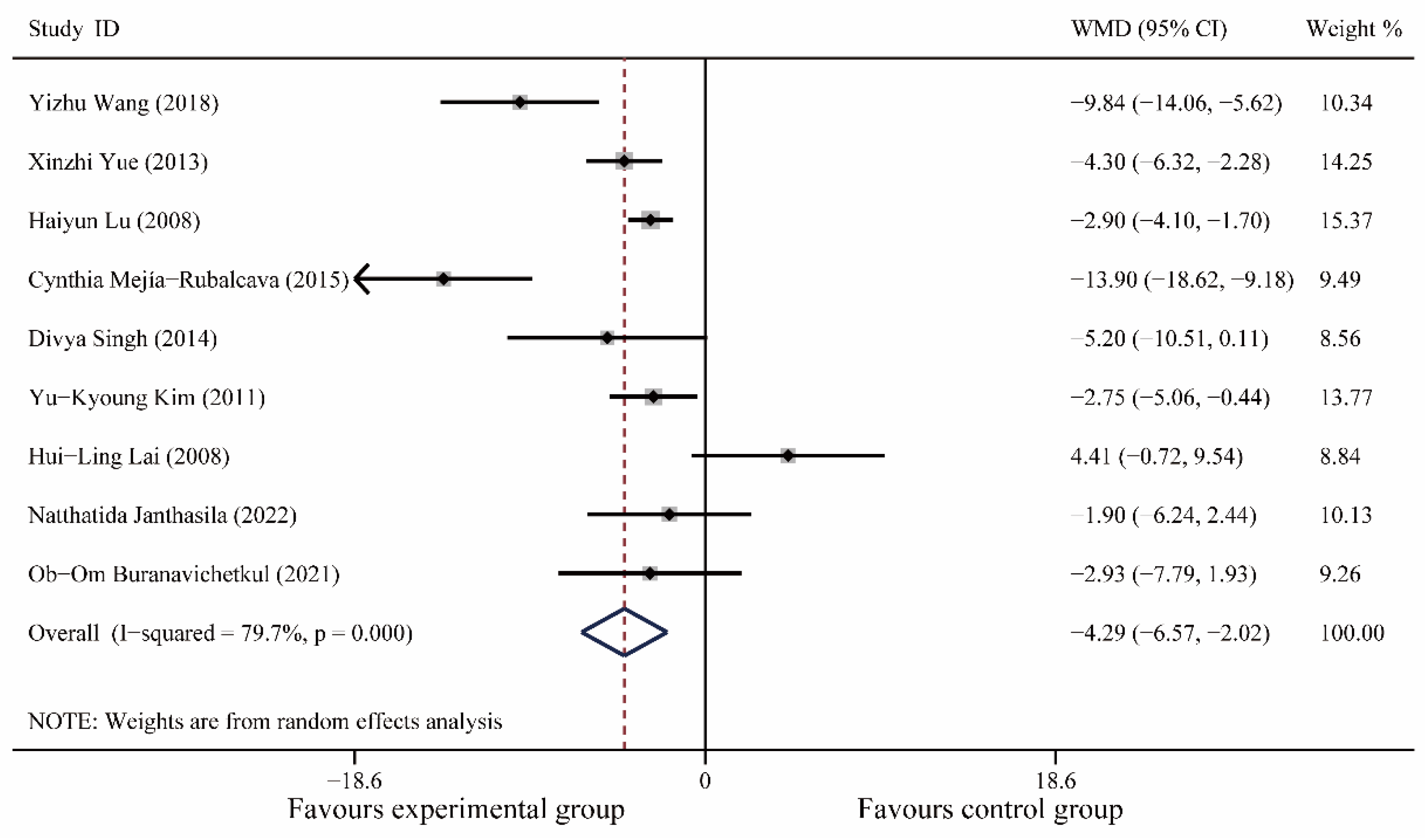
3.2.2. Systolic Blood Pressure
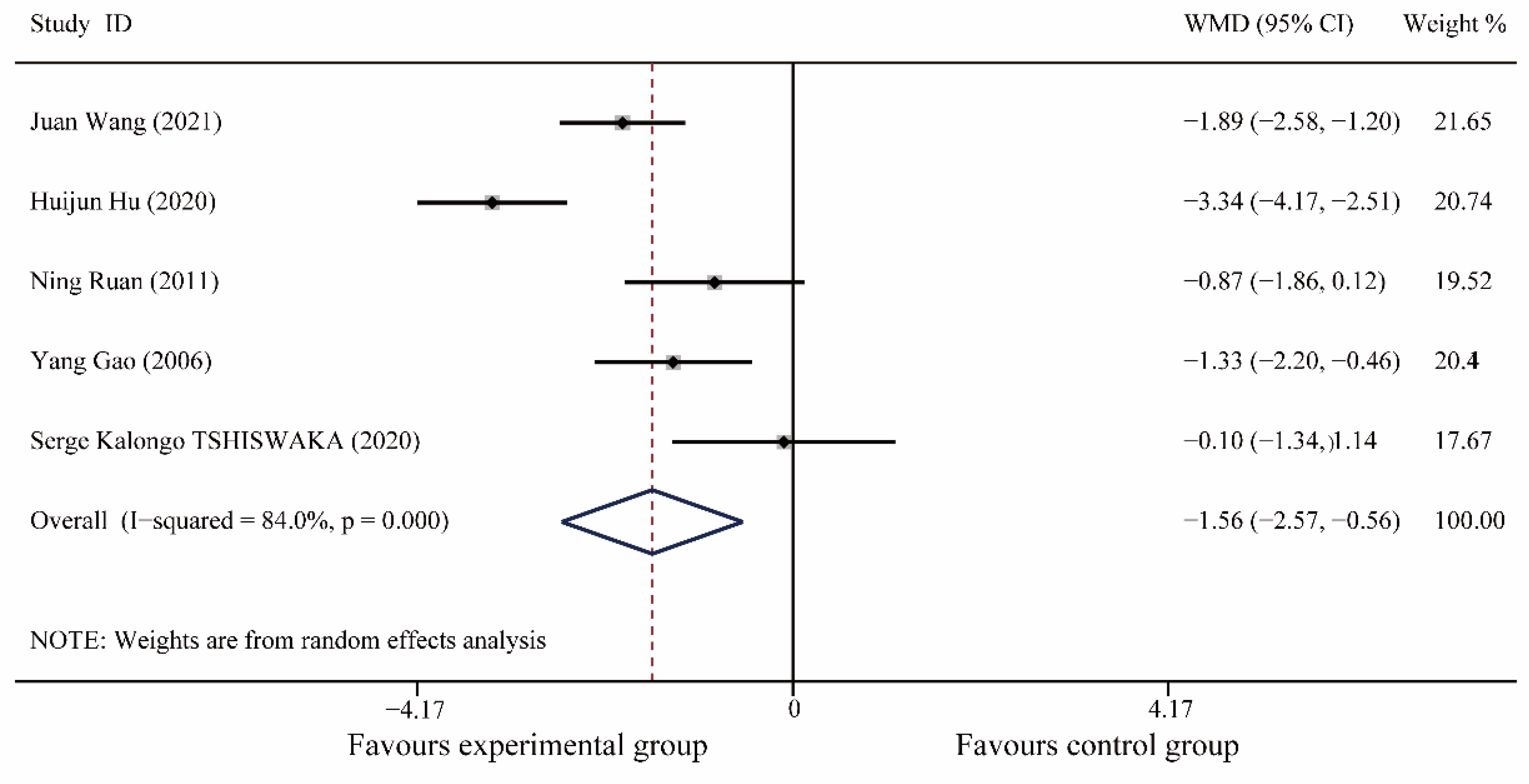
3.2.3. Diastolic Blood Pressure
3.2.4. Pain Scores
3.2.5. MDAS
3.2.6. CFSS-DS
3.2.7. S-AI
3.2.8. Cooperation Rate
3.2.9. Sensitivity Analysis and Publication Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murad, M.H.; Ingle, N.A.; Assery, M.K. Evaluating factors associated with fear and anxiety to dental treatment-A systematic review. J. Fam. Med. Prim. Care 2020, 9, 4530–4535. [Google Scholar] [CrossRef]
- Saatchi, M.; Abtahi, M.; Mohammadi, G.; Mirdamadi, M.; Binandeh, E.S. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent. Res. J. 2015, 12, 248–253. [Google Scholar]
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Armfield, J.A.; Demarco, F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021, 108, 103632. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, B.M.; Dos, S.A.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Guentsch, A.; Stier, C.; Raschke, G.F.; Peisker, A.; Fahmy, M.D.; Kuepper, H.; Schueler, I. Oral health and dental anxiety in a German practice-based sample. Clin. Oral Investig. 2017, 21, 1675–1680. [Google Scholar] [CrossRef]
- Lin, C.S.; Wu, S.Y.; Yi, C.A. Association between Anxiety and Pain in Dental Treatment: A Systematic Review and Meta-analysis. J. Dent. Res. 2017, 96, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Ketting, M. Predictors of dental avoidance among Australian adults with different levels of dental anxiety. Health Psychol. 2015, 34, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Hannibal, N.; Pedersen, I.N.; Hestbæk, T.; Sørensen, T.E.; Munk-Jørgensen, P. Schizophrenia and personality disorder patients’ adherence to music therapy. Nord. J. Psychiatry 2012, 66, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Kobus, S.; Bologna, F.; Maucher, I.; Gruenen, D.; Brandt, R.; Dercks, M.; Debus, O.; Jouini, E. Music Therapy Supports Children with Neurological Diseases during Physical Therapy Interventions. Int. J. Environ. Res. Public Health 2022, 19, 1492. [Google Scholar] [CrossRef]
- Lu, G.; Jia, R.; Liang, D.; Yu, J.; Wu, Z.; Chen, C. Effects of music therapy on anxiety: A meta-analysis of randomized controlled trials. Psychiatry Res. 2021, 304, 114137. [Google Scholar] [CrossRef]
- Jia, R.; Liang, D.; Yu, J.; Lu, G.; Wang, Z.; Wu, Z.; Huang, H.; Chen, C. The effectiveness of adjunct music therapy for patients with schizophrenia: A meta-analysis. Psychiatry Res. 2020, 293, 113464. [Google Scholar] [CrossRef] [PubMed]
- Messika, J.; Kalfon, P.; Ricard, J.D. Adjuvant therapies in critical care: Music therapy. Intensive Care Med. 2018, 44, 1929–1931. [Google Scholar] [CrossRef]
- Geretsegger, M.; Mössler, K.A.; Bieleninik, A.; Chen, X.J.; Heldal, T.O.; Gold, C. Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst. Rev. 2017, 5, D4025. [Google Scholar] [CrossRef]
- Aalbers, S.; Fusar-Poli, L.; Freeman, R.E.; Spreen, M.; Ket, J.C.; Vink, A.C.; Maratos, A.; Crawford, M.; Chen, X.J.; Gold, C. Music therapy for depression. Cochrane Database Syst. Rev. 2017, 11, D4517. [Google Scholar] [CrossRef] [PubMed]
- Broder-Fingert, S.; Feinberg, E.; Silverstein, M. Music Therapy for Children with Autism Spectrum Disorder. JAMA 2017, 318, 523–524. [Google Scholar] [CrossRef]
- Page, M.J.; Mckenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Xu, L.Q.; Zhao, Y.Y.; E, R.X.; Hu, X.; Song, G.T. Study on the effectiveness of comfort treatment strategy based on environmental auditory management in pediatric dental phobia. Chin. J. Pract. Dent. 2022, 15, 93–96. [Google Scholar] [CrossRef]
- Wang, J. Study on the Factors Influencing Dental Anxiety and Measures to Alleviate it in Patients with Obstructed Wisdom Teeth Extraction. Master’s Thesis, Zhengzhou University, Zhengzhou, China, 2021. [Google Scholar]
- Hu, H.; Chang, Z.; Han, Y.; Li, X.; Miao, C.; Jing, Q. Factors influencing dental extraction anxiety and the clinical efficacy of Chinese medicine five elements music therapy in intervening dental extraction anxiety. J. Clin. Dent. 2020, 36, 482–486. [Google Scholar]
- Wang, Y.Z.; Li, R.; Chang, P.; Lv, Y.; Li, X.G.; Wen, L.; Liang, Y.R.; Yuan, Y.I.; Guo, B. Study on the application of music therapy in the clinical treatment of dental phobia in children. Chin. J. Pract. Dent. 2017, 10, 274–278. [Google Scholar] [CrossRef]
- Yue, X.Z. Effects of music therapy on dental anxiety disorders. Clin. Med. Eng. 2013, 20, 1017–1018. [Google Scholar]
- Ruan, N. Investigation of Dental Anxiety and Psychological Intervention in Patients with Extracted Obstructed Wisdom Teeth. Master’s Thesis, Shihezi University, Shihezi, China, 2011. [Google Scholar]
- Gao, Y.; Wang, Z.; Wang, X. A clinical study on the effect of music on relieving anxiety symptoms in patients with dental treatment phobia. Nurs. Res. 2006, 30, 2784–2785. [Google Scholar]
- Lu, H.Y.; Feng, L.R. Psychological intervention of individualized “music therapy” for dental anxiety patients. Mod. Hosp. 2008, 8, 77–78. [Google Scholar]
- Mejía-Rubalcava, C.; Alanís-Tavira, J.; Mendieta-Zerón, H.; Sánchez-Pérez, L. Changes induced by music therapy to physiologic parameters in patients with dental anxiety. Complement. Ther. Clin. Pract. 2015, 21, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Samadi, F.; Jaiswal, J.; Tripathi, A.M. Stress Reduction through Audio Distraction in Anxious Pediatric Dental Patients: An Adjunctive Clinical Study. Int. J. Clin. Pediatr. Dent. 2014, 7, 149–152. [Google Scholar] [CrossRef]
- Kim, Y.K.; Kim, S.M.; Myoung, H. Musical intervention reduces patients’ anxiety in surgical extraction of an impacted mandibular third molar. J. Oral Maxillofac. Surg. 2011, 69, 1036–1045. [Google Scholar] [CrossRef]
- Lahmann, C.; Schoen, R.; Henningsen, P.; Ronel, J.; Muehlbacher, M.; Loew, T.; Tritt, K.; Nickel, M.; Doering, S. Brief relaxation versus music distraction in the treatment of dental anxiety: A randomized controlled clinical trial. J. Am. Dent. Assoc. 2008, 139, 317–324. [Google Scholar] [CrossRef]
- Lai, H.L.; Hwang, M.J.; Chen, C.J.; Chang, K.F.; Peng, T.C.; Chang, F.M. Randomised controlled trial of music on state anxiety and physiological indices in patients undergoing root canal treatment. J. Clin. Nurs. 2008, 17, 2654–2660. [Google Scholar] [CrossRef]
- Janthasila, N.K.O. Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. J. Dent. Sci. 2022, 18, 203–210. [Google Scholar] [CrossRef]
- Dixit, U.B.; Jasani, R.R. Comparison of the effectiveness of Bach flower therapy and music therapy on dental anxiety in pediatric patients: A randomized controlled study. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 71–78. [Google Scholar] [CrossRef]
- James, J.; Retnakumari, N.; Vadakkepurayil, K.; Thekkeveetil, A.K.; Tom, A. Effectiveness of Aromatherapy and Music Distraction in Managing Pediatric Dental Anxiety: A Comparative Study. Int. J. Clin. Pediatr. Dent. 2021, 14, 249–253. [Google Scholar] [CrossRef]
- Tshiswaka, S.K.; Pinheiro, S.L. Effect of music on reducing anxiety in children during dental treatment. RGO Rev. Gaúcha Odontol. 2020, 68, e20200033. [Google Scholar] [CrossRef]
- Burana, T.T. Effect of Music Intervention on Anxiety in Patients Undergoing Periodontal Surgery: A Pilot Study. SOJ Dent. Oral Disord. 2021, 1. [Google Scholar] [CrossRef]
- Khan, J.; Zusman, T.; Wang, Q.; Eliav, E. Acute and chronic pain in orofacial trauma patients. Dent. Traumatol. 2019, 35, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S.; Salvato, R. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Altenmüller, E.; Schlaug, G. Music, brain, and health: Exploring biological foundations of music’s health effects. Music. Health Wellbeing 2012, 2, 12–24. [Google Scholar]
- O’Callaghan, C. Bringing music to life: A study of music therapy and palliative care experiences in a cancer hospital. J. Palliat. Care 2001, 17, 155–160. [Google Scholar]
- Bradt, J.; Teague, A. Music interventions for dental anxiety. Oral Dis. 2018, 24, 300–306. [Google Scholar] [CrossRef]
- Sihvonen, A.J.; Särkämö, T.; Leo, V.; Tervaniemi, M.; Altenmüller, E.; Soinila, S. Music-based interventions in neurological rehabilitation. Lancet Neurol. 2017, 16, 648–660. [Google Scholar] [CrossRef]

| Inclusion criteria |
|
| Exclusion criteria |
|
| No. | Study | Country | Population | Operation | Number of Patients | Age | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | Jian Yu, 2022 [17] | China | Child | Children’s Oral Treatment | 60 | T: 5.65 ± 1.19 C: 5.83 ± 1.12 | CFSS-DS; Cooperation Rate |
| 2 | Juan Wang, 2021 [18] | China | Adult | Tooth Extraction | 60 | NA | Pain Score; MDAS |
| 3 | Huijun Hu, 2020 [19] | China | Adult | Tooth Extraction | 58 | NA | Pain Score; MDAS |
| 4 | Yizhu Wang, 2018 [20] | China | Child | Children’s Oral Treatment | 128 | NA | HR; SBP; DBP; Cooperation Rate |
| 5 | Xinzhi Yue, 2013 [21] | China | Adult | Oral Treatment | 98 | T: 32.9 ± 7.9 C: 33.1 ± 8.3 | HR; SBP; DBP; Pain Score |
| 6 | Ning Ruan, 2011 [22] | China | Adult | Tooth Extraction | 80 | NA | Pain Score; MDAS; S-AI |
| 7 | Yang Gao, 2006 [23] | China | NA | Root Canal Treatment | 42 | T: 31.7 ± 8.3 C: 30.7 ± 8.3 | Pain Score; S-AI |
| 8 | Haiyun Lu, 2008 [24] | China | Adult | Oral Treatment | 100 | NA | HR; SBP; DBP |
| 9 | Cynthia Mejía-Rubalcava, 2015 [25] | Mexico | Adult | Oral Treatment | 34 | NA | HR; SBP; DBP |
| 10 | Divya Singh, 2014 [26] | India | Child | Tooth Extraction | 60 | NA | HR; SBP; DBP |
| 11 | Yu-Kyoung Kim, 2011 [27] | Korea | Adult | Tooth Extraction | 219 | T: 35.1 ± 15.6 C: 38.6 ± 12.9 | HR; SBP; DBP |
| 12 | Claas Lahmann, 2008 [28] | Germany | Adult | Oral Treatment | 58 | T: 32.7 ± 12.2 C: 43.7 ± 13.0 | S-AI |
| 13 | Hui-Ling Lai, 2008 [29] | China | Adult | Root Canal Treatment | 44 | NA | HR; SBP; DBP; S-AI |
| 14 | Natthatida Janthasila, 2022 [30] | Thailand | Child | Children’s Oral Treatment | 65 | T: 11.00 ± 0.83 C: 11.00 ± 0.88 | HR; SBP; DBP; CFSS-DS |
| 15 | Uma B Dixit, 2020 [31] | India | Child | Children’s Oral Treatment | 80 | T: 5.23 ± 0.11 C: 5.25 ± 0.12 | HR; SBP; DBP |
| 16 | Jeswin James, 2021 [32] | India | Child | Children’s Oral Treatment | 100 | NA | HR |
| 17 | Serge Kalongo Tshiswaka, 2020 [33] | Brazil | Child | Children’s Oral Treatment | 40 | NA | HR; Pain Score |
| 18 | Ob-Om Buranavichetkul, 2021 [34] | Thailand | Adult | Periodontal Surgery | 60 | T: 48.03 ± 14.02 C: 52.53 ± 12.18 | HR; SBP; DBP |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, K.; Liu, H.; Huang, S.; Li, C. Efficacy of Music Intervention for Dental Anxiety Disorders: A Systematic Review and Meta-Analysis. Medicina 2023, 59, 209. https://doi.org/10.3390/medicina59020209
Tan K, Liu H, Huang S, Li C. Efficacy of Music Intervention for Dental Anxiety Disorders: A Systematic Review and Meta-Analysis. Medicina. 2023; 59(2):209. https://doi.org/10.3390/medicina59020209
Chicago/Turabian StyleTan, Kui, Hao Liu, Shuang Huang, and Conghua Li. 2023. "Efficacy of Music Intervention for Dental Anxiety Disorders: A Systematic Review and Meta-Analysis" Medicina 59, no. 2: 209. https://doi.org/10.3390/medicina59020209
APA StyleTan, K., Liu, H., Huang, S., & Li, C. (2023). Efficacy of Music Intervention for Dental Anxiety Disorders: A Systematic Review and Meta-Analysis. Medicina, 59(2), 209. https://doi.org/10.3390/medicina59020209