Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis
Abstract
:1. Introduction
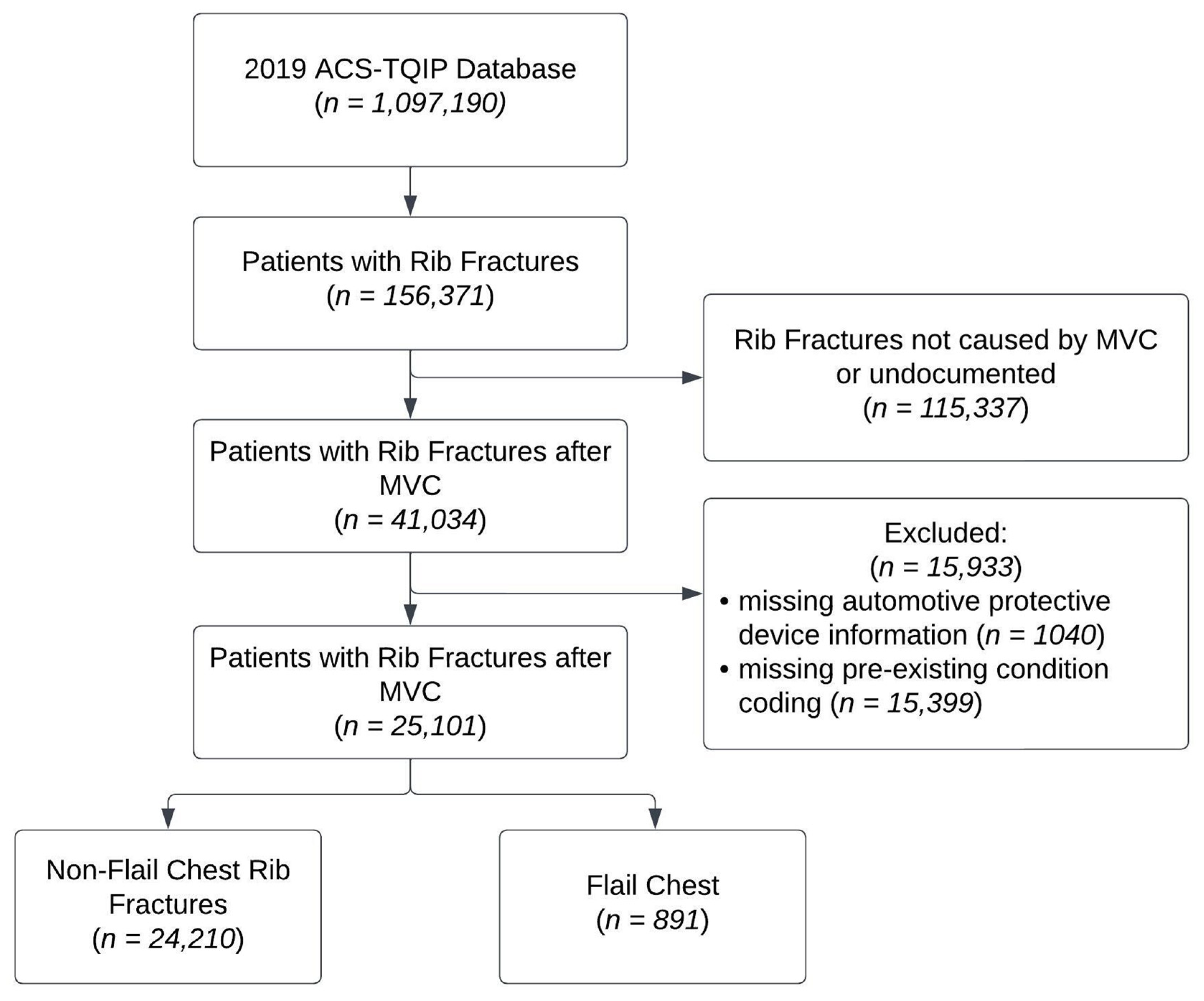
2. Materials and Methods
3. Results
3.1. Patient Characteristics
3.2. Seatbelt Use and Airbag Deployment
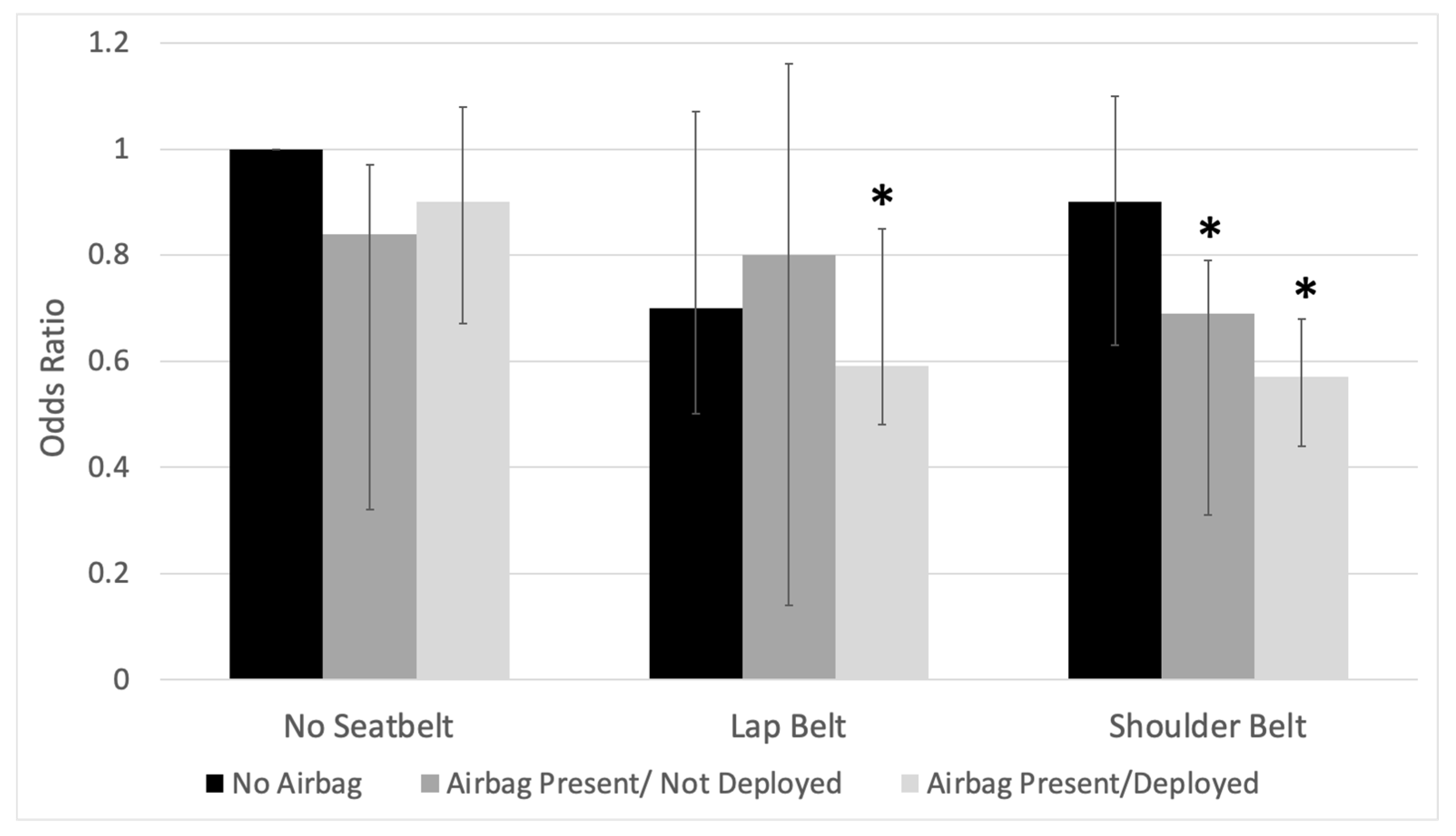
3.3. Synergistic Effects of Seatbelts and Airbags
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). Global Status Report on Road Safety 2018; The World Health Organization (WHO): Geneva, Switzerland, 2018. [Google Scholar]
- Parreira, J.G.; Rondini, G.Z.; Below, C.; Tanaka, G.O.; Pelluchi, J.N.; Arantes-Perlingeiro, J.; Soldá, S.C.; Assef, J.C. Trauma mechanism predicts the frequency and the severity of injuries in blunt trauma patients. Rev. Col. Bras. Cir. 2017, 44, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Murray, J.; Charalambides, K.; Alo, K.; Velmahos, G.; Rhee, P.; Chan, L. Trauma fatalities: Time and location of hospital deaths. J. Am. Coll. Surg. 2004, 198, 20–26. [Google Scholar] [CrossRef]
- Sirmali, M.; Turut, H.; Topcu, S.; Gulhan, E.; Yazici, U.; Kaya, S.; Taştepe, I. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur. J. Cardio-Thorac. Surg. 2003, 24, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Lafferty, P.M.; Anavian, J.; Will, R.E.; Cole, P.A. Operative Treatment of Chest Wall Injuries: Indications, Technique, and Outcomes. JBJS 2011, 93, 97. [Google Scholar] [CrossRef]
- Dehghan, N.; de Mestral, C.; McKee, M.D.; Schemitsch, E.H.; Nathens, A. Flail chest injuries: A review of outcomes and treatment practices from the National Trauma Data Bank. J. Trauma Acute Care Surg. 2014, 76, 462. [Google Scholar] [CrossRef] [PubMed]
- Flagel, B.T.; Luchette, F.A.; Reed, R.L.; Esposito, T.J.; Davis, K.A.; Santaniello, J.M.; Gamelli, R.L. Half-a-dozen ribs: The breakpoint for mortality. Surgery 2005, 138, 717–723; discussion 723–725. [Google Scholar] [CrossRef] [PubMed]
- National Highway Traffic Safety Administration. Lives Saved in 2017 by Restraint Use and Minimum-Drinking-Age Laws; National Highway Traffic Safety Administration: Washington, DC, USA, 2016; DOT HS 812. Available online: https://crashstats.nhtsa.dot.gov/Api/Public/Publication/812683 (accessed on 20 March 2023).
- Layrisse, V.; García-Rodríguez, O.; Ramos-Meléndez, E.; Rodríguez-Ortiz, P. A Comparative Analysis of the Injury Patterns and In-Hospital Mortality Rates of Belted and Unbelted Motor-Vehicle Occupants—Puerto Rico, January 2000 to December 2014. Puerto Rico Health Sci. J. 2018, 37, 213–219. [Google Scholar]
- Elkbuli, A.; Dowd, B.; Spano, P.J.; Hai, S.; Boneva, D.; McKenney, M. The association between seatbelt use and trauma outcomes: Does body mass index matter? Am. J. Emerg. Med. 2019, 37, 1716–1719. [Google Scholar] [CrossRef]
- Boserup, B.; Sutherland, M.; Paloka, R.; McKenney, M.; Elkbuli, A. The Impact of Seatbelt Use on Trauma Outcomes in Adult Motor Vehicle Collision Patients With Rib Fractures: A National ACS-TQPs-PUF Database Analysis. J. Surg. Res. 2022, 270, 376–385. [Google Scholar] [CrossRef]
- Nash, N.A.; Okoye, O.; Albuz, O.; Vogt, K.N.; Karamanos, E.; Inaba, K.; Demetriades, D. Seat Belt Use and its Effect on Abdominal Trauma: A National Trauma Databank Study. Am. Surg. 2016, 82, 134–139. [Google Scholar] [CrossRef]
- Abu-Zidan, F.M.; Abbas, A.K.; Hefny, A.F.; Eid, H.O.; Grivna, M. Effects of Seat Belt Usage on Injury Pattern and Outcome of Vehicle Occupants After Road Traffic Collisions: Prospective Study. World J. Surg. 2012, 36, 255–259. [Google Scholar] [CrossRef]
- Williams, R.F.; Fabian, T.C.; Fischer, P.E.; Zarzaur, B.L.; Magnotti, L.J.; Croce, M.A. Impact of Airbags on a Level I Trauma Center: Injury Patterns, Infectious Morbidity, and Hospital Costs. J. Am. Coll. Surg. 2008, 206, 962. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons. Trauma Quality Programs (TQP) Participant Use File (PUF) User Manual, Admission Year 2020. Available online: https://www.facs.org/media/3zjdbmxz/tqp-puf-user-manual-2020.pdf (accessed on 1 December 2022).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Clinical Classifications Software Refined (CCSR); Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. October 2021. Available online: www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp (accessed on 1 December 2022).
- Clark, D.E.; Osler, T.M.; Hahn, D.R. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores; Statistical Software Components S457028; Boston College Department of Economics: Boston, MA, USA, 2009; revised 29 October 2010. [Google Scholar]
- Clark, D.E.; Black, A.W.; Skavdahl, D.H.; Hallagan, L.D. Open-access programs for injury categorization using ICD-9 or ICD-10. Inj. Epidemiol. 2018, 5, 11. [Google Scholar] [CrossRef]
- ACS NTDS National Trauma Data Standard: Data Dictionary 2019. Available online: https://www.facs.org/quality-programs/trauma/quality/national-trauma-data-bank/national-trauma-data-standard/data-dictionary/ (accessed on 1 March 2022).
- Engel, C.; Krieg, J.C.; Madey, S.M.; Long, W.B.; Bottlang, M. Operative Chest Wall Fixation with Osteosynthesis Plates. J. Trauma Acute Care Surg. 2005, 58, 181. [Google Scholar] [CrossRef] [PubMed]
- Simon, B.; Ebert, J.; Bokhari, F.; Capella, J.; Emhoff, T.; Hayward, T.; Rodriguez, A.; Smith, L. Management of pulmonary contusion and flail chest: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2012, 73, S351. [Google Scholar] [CrossRef]
- Nirula, R.; Diaz, J.J.; Trunkey, D.D.; Mayberry, J.C. Rib Fracture Repair: Indications, Technical Issues, and Future Directions. World J. Surg. 2009, 33, 14–22. [Google Scholar] [CrossRef]
- Siegel, J.H.; Mason-Gonzalez, S.; Dischinger, P.; Cushing, B.; Read, K.; Robinson, R.; Smialek, J.; Heatfield, B.; Hill, W.; Bents, W.; et al. Safety Belt Restraints And Compartment Intrusions In Frontal And Lateral Motor Vehicle Crashes: Mechanisms Of Injuries, Complications, And Acute Care Costs. J. Trauma Acute Care Surg. 1993, 34, 736. [Google Scholar] [CrossRef] [PubMed]
- NIH Consensus Development Panel on Osteoporosis Prevention D and Therapy. Osteoporosis Prevention, Diagnosis, and Therapy. JAMA 2001, 285, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Prins, J.T.H.; Van Lieshout, E.M.M.; Reijnders, M.R.L.; Verhofstad, M.H.J.; Wijffels, M.M.E. Rib fractures after blunt thoracic trauma in patients with normal versus diminished bone mineral density: A retrospective cohort study. Osteoporos. Int. 2020, 31, 225–231. [Google Scholar] [CrossRef]
- Kim, W.; Gong, H.S.; Lee, S.H.; Park, J.W.; Kim, K.; Baek, G.H. Low evaluation rate for osteoporosis among patients presenting with a rib fracture. Arch. Osteoporos. 2017, 12, 61. [Google Scholar] [CrossRef]
- Yuan, S.; Michaëlsson, K.; Wan, Z.; Larsson, S.C. Associations of Smoking and Alcohol and Coffee Intake with Fracture and Bone Mineral Density: A Mendelian Randomization Study. Calcif. Tissue Int. 2019, 105, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Beaupre, G.S.; Lew, H.L. Bone-Density Changes After Stroke. Am. J. Phys. Med. Rehabil. 2006, 85, 464. [Google Scholar] [CrossRef] [PubMed]
- Myint, P.K.; Clark, A.B.; Kwok, C.S.; Loke, Y.K.; Yeong, J.K.-Y.; Luben, R.N.; Wareham, N.J.; Khaw, K.-T. Bone Mineral Density and Incidence of Stroke. Stroke 2014, 45, 373–382. [Google Scholar] [CrossRef] [PubMed]
| Variable | Non-Flail Chest Rib Fractures (n = 24,210) | Flail Chest (n = 891) | p Value |
|---|---|---|---|
| Age (Median) | 58 (40–71) | 59 (44–71) | 0.0368 |
| Sex | 0.481 | ||
| Female | 10,994 (45.4%) | 394 (44.22%) | |
| Male | 12,213 (54.6%) | 497 (55.8%) | |
| Race | |||
| White | 18,653 (77.0%) | 703 (78.9%) | 0.196 |
| Black | 3174 (13.1%) | 111 (12.5%) | 0.571 |
| Asian | 423 (1.7%) | 15 (1.7%) | 0.887 |
| Ethnicity | 0.221 | ||
| Hispanic or Latino | 2167 (9.3%) | 69 (8.1%) | |
| Not Hispanic or Latino | 21,121 (90.7%) | 786 (91.9%) | |
| Seatbelt Type | <0.001 | ||
| No seatbelt | 7304 (30.2%) | 350 (39.3%) | |
| Lap belt only | 3366 (13.9%) | 106 (11.9%) | |
| Shoulder belt | 13,540 (55.9%) | 435 (48.8%) | |
| Airbag Status | <0.001 | ||
| No airbag present | 6254 (25.8%) | 296 (33.2%) | |
| Airbag present not deployed | 2683 (11.1%) | 94 (10.6%) | |
| Airbag deployed | 15,273 (63.1%) | 501 (56.2%) | |
| Body region maximum AIS (median IQR) | |||
| Head/Neck | 1 (0–1) | 1 (0–3) | <0.001 |
| General | 0 (0–0) | 0 (0–0) | 0.0753 |
| Face | 0 (0–0) | 0 (0–1) | 0.003 |
| Extremities | 1 (0–1) | 1 (1–2) | <0.001 |
| Abdomen | 1 (0–1) | 1 (0–2) | <0.001 |
| History of Smoking | 1017 (4.2%) | 50 (5.61%) | 0.040 |
| History of CVA | 147 (0.61%) | 13 (1.46%) | 0.002 |
| Variable | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Age | 1.01 | 1.01–1.02 | <0.001 |
| Male sex | 1.03 | 0.89–1.18 | 0.701 |
| Seatbelt Type | |||
| No seatbelt | reference | ||
| Lap belt only | 0.72 | 0.57–0.90 | 0.004 |
| Shoulder belt | 0.73 | 0.63–0.86 | <0.001 |
| Airbag | |||
| No airbag present | reference | ||
| Airbag present not deployed | 0.86 | 0.67–1.09 | 0.208 |
| Airbag deployed | 0.76 | 0.65–0.89 | 0.001 |
| Body region maximum AIS | |||
| Head/Neck | 1.13 | 1.07–1.18 | <0.001 |
| General | 1.04 | 0.93–1.16 | 0.500 |
| Face | 1.07 | 0.95–1.20 | 0.255 |
| Extremities | 1.22 | 1.15–1.30 | <0.001 |
| Abdomen | 1.38 | 1.31–1.45 | <0.001 |
| History of Smoking | 1.29 | 0.96–1.73 | 0.096 |
| History of CVA | 2.17 | 1.21–3.88 | 0.009 |
| Variable | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Age | 1.01 | 1.01–1.02 | <0.001 |
| Male sex | 1.03 | 0.89–1.18 | 0.720 |
| Seatbelt Type and airbag status (Interaction variable) | |||
| No seatbelt/no airbag | reference | ||
| No seatbelt/airbag present, not deployed | 0.84 | 0.57–1.22 | 0.358 |
| No seatbelt/airbag deployed | 0.90 | 0.72–1.13 | 0.377 |
| Lap belt/no airbag | 0.70 | 0.47–1.04 | 0.079 |
| Lap belt/airbag present, not deployed | 0.80 | 0.44–1.46 | 0.468 |
| Lap belt/airbag deployed | 0.59 | 0.43–0.80 | 0.001 |
| Shoulder belt/no airbag | 0.90 | 0.70–1.17 | 0.448 |
| Shoulder belt/airbag present, not deployed | 0.69 | 0.49–0.97 | 0.030 |
| Shoulder belt/airbag deployed | 0.57 | 0.46–0.70 | <0.001 |
| Body region maximum AIS | |||
| Head/Neck | 1.13 | 1.07–1.18 | <0.001 |
| General | 1.04 | 0.93–1.16 | 0.519 |
| Face | 1.07 | 0.95–1.20 | 0.257 |
| Extremities | 1.22 | 1.15–1.30 | <0.001 |
| Abdomen | 1.38 | 1.30–1.45 | <0.001 |
| History of Smoking | 1.28 | 0.95–1.73 | 0.103 |
| History of CVA | 2.16 | 1.21–3.87 | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassiri, A.; Badrinathan, A.; Kishawi, S.; Sinopoli, J.; Linden, P.A.; Ho, V.P.; Towe, C.W. Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis. Medicina 2023, 59, 2046. https://doi.org/10.3390/medicina59112046
Bassiri A, Badrinathan A, Kishawi S, Sinopoli J, Linden PA, Ho VP, Towe CW. Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis. Medicina. 2023; 59(11):2046. https://doi.org/10.3390/medicina59112046
Chicago/Turabian StyleBassiri, Aria, Avanti Badrinathan, Sami Kishawi, Jillian Sinopoli, Philip A. Linden, Vanessa P. Ho, and Christopher W. Towe. 2023. "Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis" Medicina 59, no. 11: 2046. https://doi.org/10.3390/medicina59112046
APA StyleBassiri, A., Badrinathan, A., Kishawi, S., Sinopoli, J., Linden, P. A., Ho, V. P., & Towe, C. W. (2023). Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis. Medicina, 59(11), 2046. https://doi.org/10.3390/medicina59112046