Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
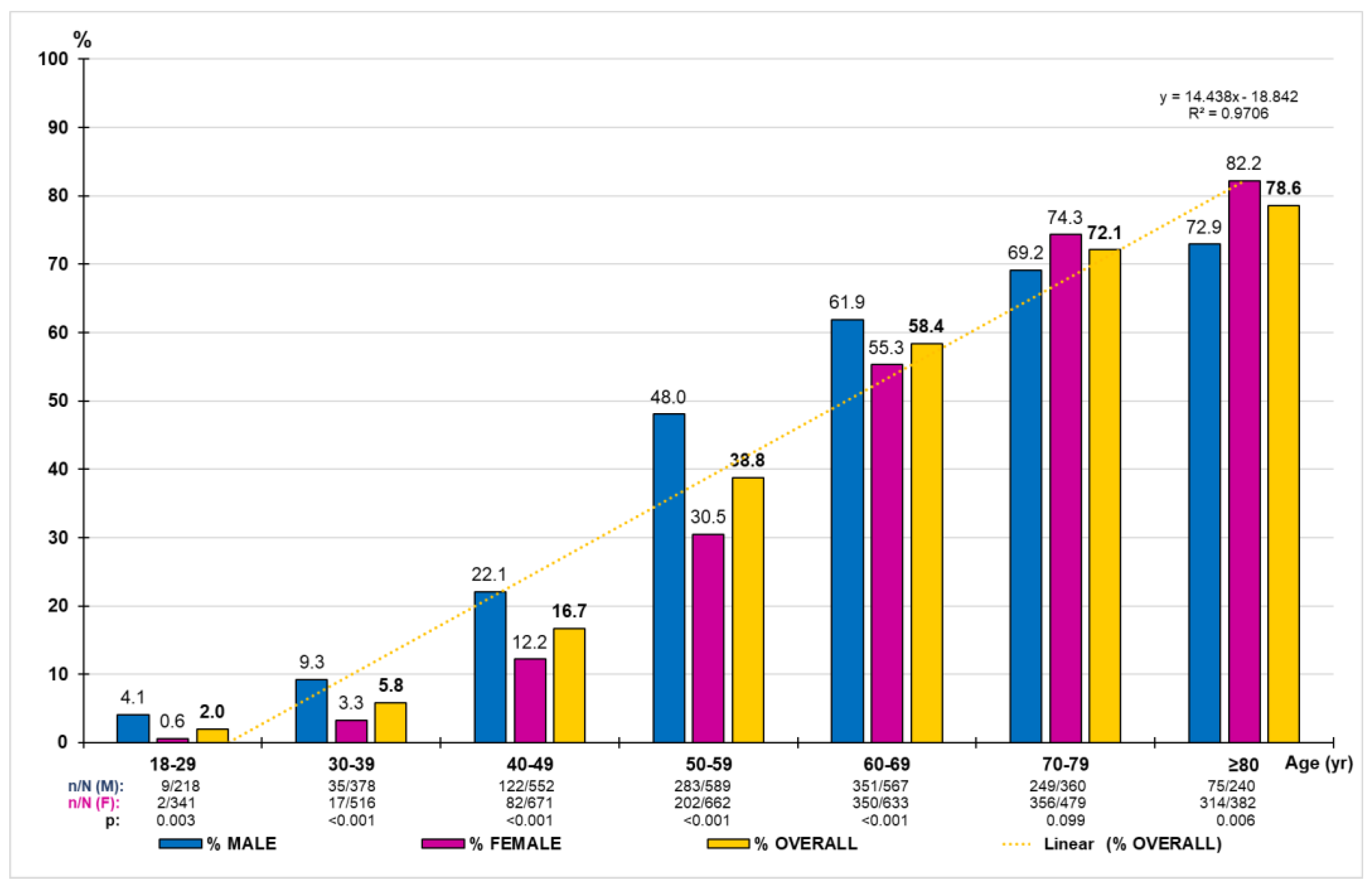
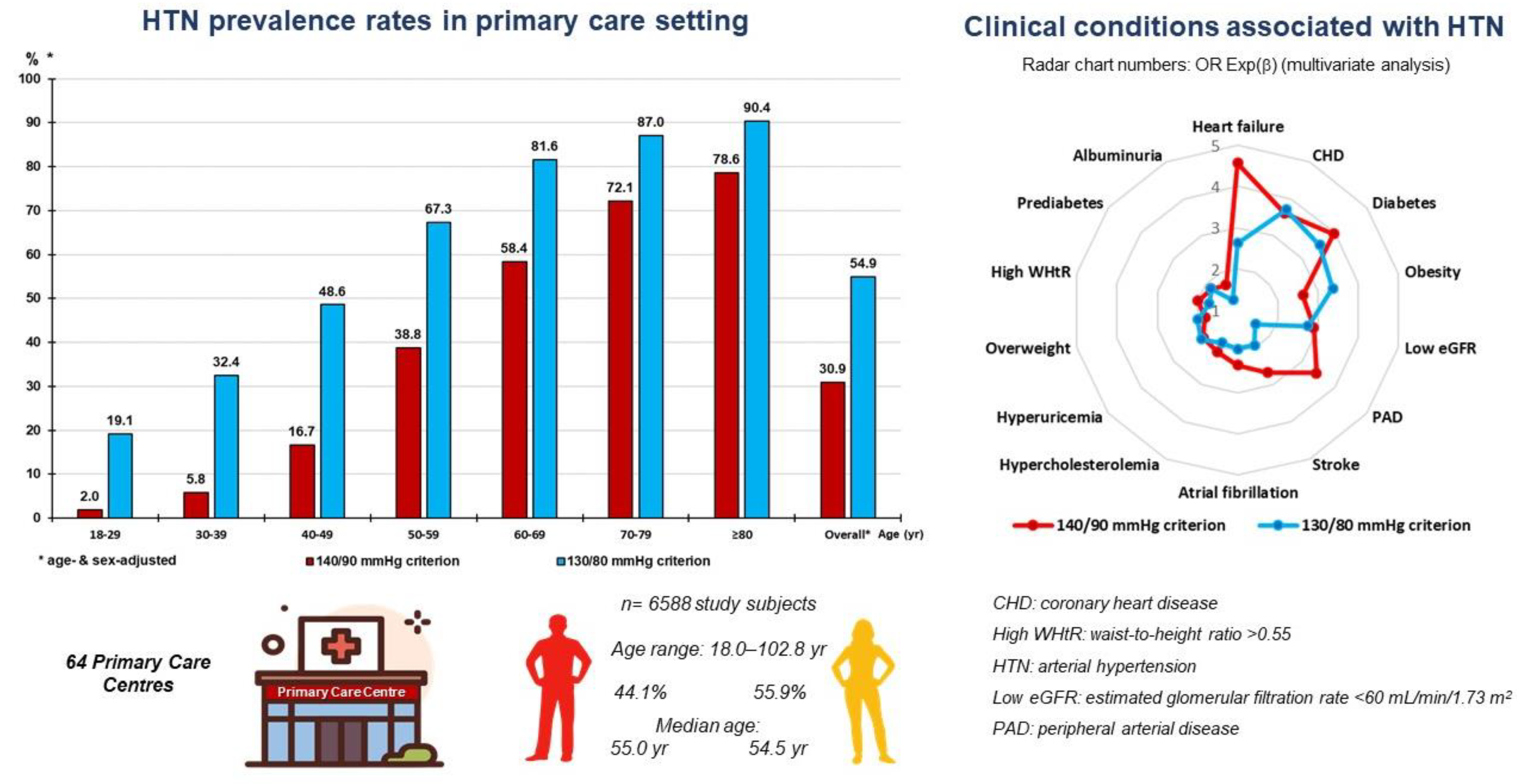
3.1. HTN Prevalence Rates According to 140/90 Criterion
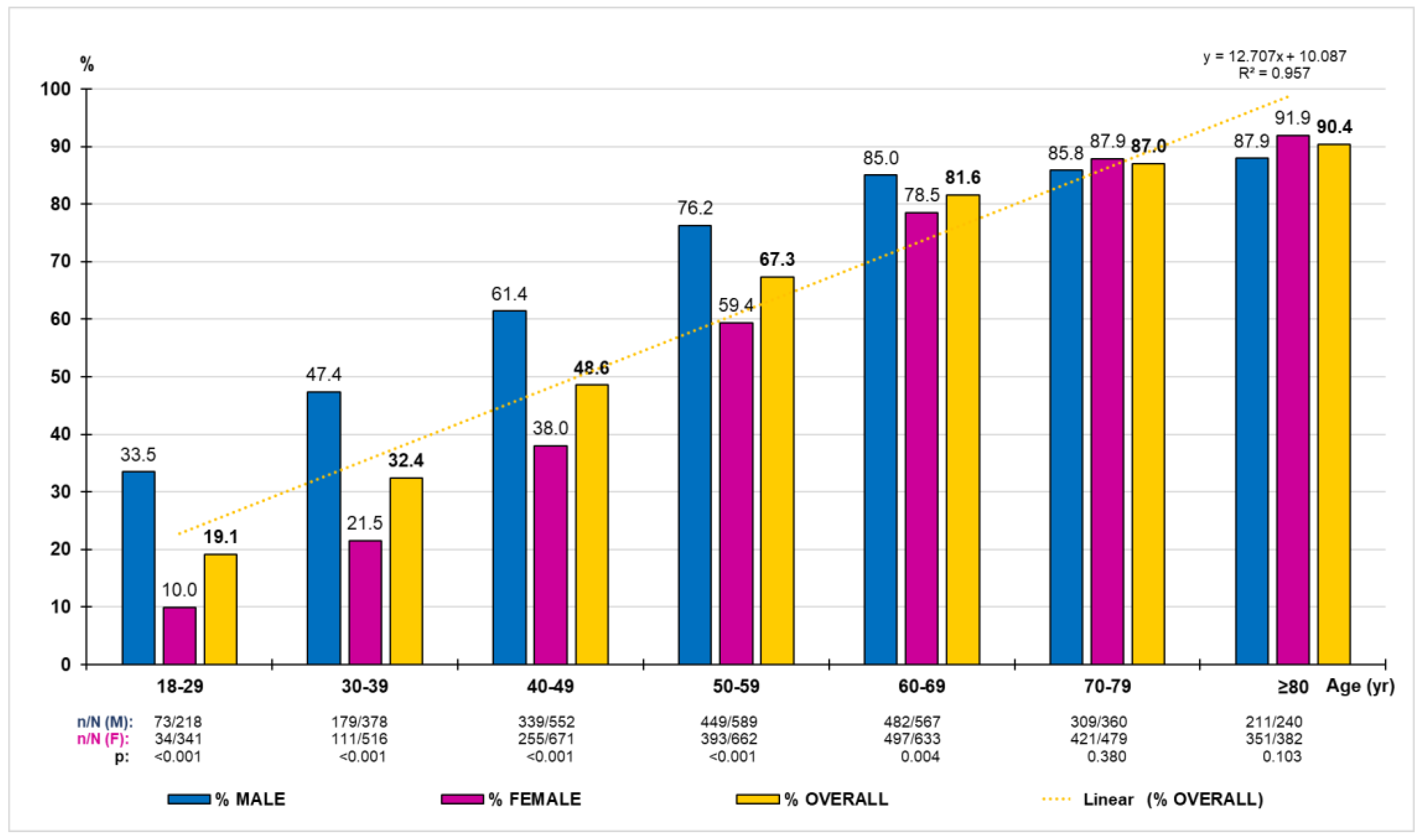
3.2. HTN Prevalence Rates According to 130/80 Criterion
3.3. Comparisons between Populations with and without HTN According to 140/90 Criterion
3.4. Comparisons between Populations with and without HTN According to 130/80 Criterion
3.5. Associations between HTN and CVRF, Renal and Cardiometabolic Diseases
3.6. Effect of Associated Comorbidities on HTN According to 140/90 or 130/80 Criteria
3.7. BP Control Targets in Patients with HTN Diagnosed According to Both Criteria
4. Discussion
4.1. HTN Prevalence Rates
4.2. Clinical Conditions and Factors Associated with HTN
4.3. Comparison of BP Control Targets in Patients with HTN Diagnosed according to Both Criteria
4.4. Strengths and Limitations
4.5. Clinical Implications
5. Conclusions
Key Points
- The proportion of adults with HTN doubled between 1990 and 2019 worldwide.
- Primary health care is the setting where HTN is usually detected.
- There is a continuous relationship between BP and cardiovascular or renal morbid or fatal events starting from SBP/DBP values >115/75 mmHg.
- The American guidelines recommend that the threshold values for SBP/DBP to consider HTN should be 130/80 mmHg, which are different from the classic threshold values (140/90 mmHg) recommended according to other international guidelines for the HTN management.
- The discrepancy with these threshold levels raises differences, not only diagnostic, but also in the determination of the HTN prevalence and in the assessment of the clinical conditions and comorbidities that can be associated with HTN.
- Early initiation of antihypertensive treatment can effectively control hypertension and prevent its progression and associated cardiovascular, metabolic, and renal complications.
- The mean age of the HTN patients diagnosed according to the 140/90 criterion was 5.7 years older than those diagnosed according to the 130/80 criterion (61.5 years).
- The age- and sex-adjusted prevalence rate of HTN was 30.9% according to the 140/90 criterion and was 54.9% according to the 130/80 criterion.
- The proportion of HTN patients with high or very high CVR was higher in those diagnosed according to the 140/90 criterion (80.1%) than in those diagnosed according to the 130/80 criterion (62.8%).
- The proportion of HTN patients without ASCVD or CKD who achieved the BP control goal < 130/80 mmHg was 60.5% in those diagnosed according to the 140/90 criterion and 65.5% according to the 130/80 criterion.
- The proportion of HTN patients according to both diagnostic criteria who achieved the BP control target < 130/80 mmHg was similar in patients with ASCVD (70%) and in patients with CKD (71%).
- The intensity of treatment with BP-lowering drugs in HTN patients without ASCVD or CKD decreased by half when using the 130/80 diagnostic criterion than when using the 140/90 criterion, and instead, it was similar for both HTN patients with ASCVD and with CKD.
- The following comorbidities and clinical conditions showed, from greater to lesser intensity, an independent association with HTN according to both criteria: HF, DM, CHD, low eGFR, obesity, stroke, AF, hypercholesterolemia, hyperuricemia, high WHtR, prediabetes, and overweight. Albuminuria and PAD showed an independent association only with HTN according to the 140/90 criterion.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AF | atrial fibrillation |
| ASCVD | atherosclerotic cardiovascular diseases |
| AST | aspartate aminotransferase |
| BP | blood pressure |
| CHD | coronary heart disease |
| CKD | chronic kidney disease |
| CVR | cardiovascular risk |
| CVRF | cardiovascular risk factors |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| eGFR | estimated glomerular filtration rate |
| HDL-C | high-density lipoprotein cholesterol |
| HF | heart failure |
| HTN | arterial hypertension |
| LDL-C | low-density lipoprotein cholesterol |
| MetS | metabolic syndrome |
| PAD | peripheral arterial disease |
| SBP | systolic blood pressure |
| WHtR | waist-to-height ratio |
References
- Al-Makki, A.; DiPette, D.; Whelton, P.K.; Murad, M.H.; Mustafa, R.A.; Acharya, S.; Beheiry, H.M.; Champagne, B.; Connell, K.; Cooney, M.T.; et al. Hypertension pharmacological treatment in adults: A World Health Organization guideline executive summary. Hypertension 2022, 79, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Danaei, G.; Lu, Y.; Singh, G.M.; Carnahan, E.; Stevens, G.A.; Cowan, M.J.; Farzadfar, F.; Lin, J.K.; Finucane, M.M.; Rao, M.; et al. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular Disease, Chronic Kidney Disease, and Diabetes Mortality Burden of Cardiometabolic Risk Factors from 1980 to 2010: A Comparative Risk Assessment. Lancet Diabetes Endocrinol. 2014, 2, 634–647. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Liu, P.; Roth, G.A.; Ng, M.; Biryukov, S.; Marczak, L.; Alexander, L.; Estep, K.; Abate, K.H.; Akinyemiju, T.F.; et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017, 317, 165–182. [Google Scholar] [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef]
- Zhou, B.; Bentham, J.; Di Cesare, M.; Bixby, H.; Danaei, G.; Cowan, M.J.; Paciorek, C.J.; Singh, G.; Hajifathalian, K.; Bennett, J.E.; et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef]
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Ford, E.S. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the united states. Circulation 2011, 123, 1737–1744. [Google Scholar] [CrossRef]
- Cinza-Sanjurjo, S.; Micó-Pérez, R.; Velilla-Zancada, S.; Prieto-Díaz, M.; Rodríguez-Roca, G.; García, A.B.; García, J.P.; Sánchez, V.M.; Caro, J.L. Factors associated with cardiovascular risk and cardiovascular and renal disease in the IBERICAN study: Final results. Semergen 2020, 46, 368–378. [Google Scholar] [CrossRef]
- Saez, M.; Barceló, M. Coste de la hipertensión arterial en España. Hipertens. Riesgo Vasc. 2012, 29, 145–151. [Google Scholar] [CrossRef]
- Banegas, J.R.; Navarro-Vidal, B.; Ruilope, L.M.; de la Cruz, J.J.; López-García, E.; Rodríguez-Artalejo, F.; Graciani, A. Trends in hypertension control among the older population of spain from 2000 to 2001 to 2008 to 2010: Role of frequency and intensity of drug treatment. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 67–76. [Google Scholar] [CrossRef]
- Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [CrossRef]
- Mancia(Chairperson), G.; Kreutz(Co-Chair), R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension. Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J. Hypertens. 2023; 41, ahead of print. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [CrossRef]
- Pallarés-Carratalá, V.; Garrote, J.D.; Díaz, M.P.; Matarín, L.G.; Vicente, M.S.; Escribano, F.M.; Aldana, D.R.; Sanjurjo, S.C.; Altozano, C.S.; Górriz, J.; et al. SEMERGEN Hypertension and Cardiovascular Disease Working Group. Positioning for the management of arterial hypertension in Primary Care from the critical analysis of the American (2017) and European (2018) guidelines. Spanish Society of Primary Care Physicians (SEMERGEN). Semergen 2019, 45, 251–272. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan for the prevention And Control of Noncommunicable Diseases 2013–2020. 2013. Available online: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1 (accessed on 31 August 2023).
- Ruiz-García, A.; Arranz-Martínez, E.; García-Álvarez, J.C.; Morales-Cobos, L.E.; García-Fernández, M.E.; de la Peña-Antón, N.; Calle, M.C.M.; Costa, A.M.; Martínez, D.P.; Villasur, M.P.G.; et al. Population and methodology of the SIMETAP study: Prevalence of cardiovascular risk factors, cardiovascular diseases, and related metabolic diseases. Clin. Investig. Arterioscler. 2018, 30, 197–208. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef] [PubMed]
- Wolf-Maier, K.; Cooper, R.S.; Banegas, J.R.; Giampaoli, S.; Hense, H.-W.; Joffres, M.; Kastarinen, M.; Poulter, N.; Primatesta, P.; Rodríguez-Artalejo, F.; et al. Hypertension Prevalence and Blood Pressure Levels in 6 European Countries, Canada, and the United States. JAMA 2003, 289, 2363–2369. [Google Scholar] [CrossRef] [PubMed]
- Gurven, M.; Blackwell, A.D.; Rodríguez, D.E.; Stieglitz, J.; Kaplan, H. Does Blood Pressure Inevitably Rise With Age? Longitudinal Evidence Among Forager-Horticulturalists. Hypertension 2012, 60, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023, 147, E93–E621. [Google Scholar] [CrossRef] [PubMed]
- Chobufo, M.D.; Gayam, V.; Soluny, J.; Rahman, E.U.; Enoru, S.; Foryoung, J.B.; Agbor, V.N.; Dufresne, A.; Nfor, T. Prevalence and control rates of hypertension in the USA: 2017–2018. Int. J. Cardiol. Hypertens. 2020, 6, 100044. [Google Scholar] [CrossRef]
- Banegas, J.R.; Graciani, A.; de la Cruz-Troca, J.J.; León-Muñoz, L.M.; Guallar-Castillón, P.; Coca, A.; Ruilope, L.M.; Rodríguez-Artalejo, F. Achievement of Cardiometabolic Goals in Aware Hypertensive Patients in Spain: A nationwide population-based study. Hypertension 2012, 60, 898–905. [Google Scholar] [CrossRef]
- Gabriel, R.; Alonso, M.; Segura, A.; Tormo, M.J.; Artigao, L.M.; Banegas, J.R.; Brotons, C.; Elosua, R.; Fernández-Cruz, A.; Muñiz, J.; et al. Prevalencia, distribución y variabilidad geográfica de los principales factores de riesgo cardiovascular en España. Análisis agrupado de datos individuales de estudios epidemiológicos poblacionales: Estudio ERICE. Rev. Esp. Cardiol. 2008, 61, 1030–1040. [Google Scholar] [CrossRef]
- Grau, M.; Elosua, R.; de León, A.C.; Guembe, M.J.; Baena-Díez, J.M.; Alonso, T.V.; Félix, F.J.; Zorrilla, B.; Rigo, F.; Lapetra, J.; et al. Cardiovascular risk factors in Spain in the first decade of the 21st Century, a pooled analysis with individual data from 11 population-based studies: The DARIOS study. Rev. Esp. Cardiol. 2011, 64, 295–304. [Google Scholar] [CrossRef]
- Menéndez, E.; Delgado, E.; Fernández-Vega, F.; Prieto, M.A.; Bordiú, E.; Calle, A.; Carmena, R.; Castaño, L.; Catalá, M.; Franch, J.; et al. Prevalencia, diagnóstico, tratamiento y control de la hipertensión arterial en España. Resultados del estudio Di@bet.es. Rev. Española Cardiol. 2016, 69, 572–578. [Google Scholar] [CrossRef]
- Alonso, A.T.V.; Alonso, J.E.L.; Sanz, R.; Muñoz, S.L. Prevalencia de la hipertensión arterial en la población de Castilla y León. Gac. Sanit. 2008, 22, 330–336. [Google Scholar] [CrossRef][Green Version]
- Gil Montalbán, E.; Torras, B.Z.; Marrón, H.O.; Cortés, M.M.; Navarro, E.D.; Aguado, P.N.; Blasco, H.d.l.C.; Albero, M.J.M.; Gamarra, I.C. Prevalencia de diabetes mellitus y factores de riesgo cardiovascular en la población adulta de la Comunidad de Madrid: Estudio PREDIMERC. Gac. Sanit. 2010, 24, 233–240. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. La Salud de la Población en España. Resultados de la Encuesta Europea de Salud en España EESE 2014. Madrid 2017. Available online: http://www.mscbs.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2014.html (accessed on 31 August 2023).
- Ministerio de Sanidad. Sanidad en datos. Encuesta Nacional de Salud de España 2017. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.html (accessed on 31 August 2023).
- Subdirección General de Información Sanitaria. Indicadores Clínicos en Atención Primaria 2016. BDCAP. Madrid: Ministerio de Sanidad, Consumo y Bienestar Social. 2019. Available online: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/home.html (accessed on 31 August 2023).
- Foti, K.; Hardy, S.T.; Chang, A.R.; Selvin, E.; Coresh, J.; Muntner, P. BMI and blood pressure control among United States adults with hypertension. J. Hypertens. 2022, 40, 741–748. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Atasoy, S.; Middeke, M.; Johar, H.; Peters, A.; Heier, M.; Ladwig, K.-H. Cardiovascular mortality risk in young adults with isolated systolic hypertension: Findings from population-based MONICA/KORA cohort study. J. Hum. Hypertens. 2022, 36, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Sundstrom, J.; Arima, H.; Woodward, M.; A Jackson, R.; Karmali, K.N.; Jones, D.L.; Baigent, C.; Emberson, J.; Rahimi, K.; Mcmahon, S.J.; et al. Blood pressure-lowering treatment based on cardiovascular risk: A meta-analysis of individual patient data. Lancet 2014, 384, 591–598. [Google Scholar] [CrossRef]
- Karmali, K.N.; Ning, H.; Goff, D.C., Jr.; Lloyd-Jones, D.M. Identifying Individuals at Risk for Cardiovascular Events Across the Spectrum of Blood Pressure Levels. J. Am. Heart Assoc. 2015, 4, e002126. [Google Scholar] [CrossRef]
- Del Pinto, R.; Giua, C.; Keber, E.; Grippa, E.; Tilotta, M.; Ferri, C. Impact of 2021 ESC Guidelines for Cardiovascular Disease Prevention on Hypertensive Patients Risk: Secondary Analysis of Save Your Heart Study. High Blood Press. Cardiovasc. Prev. 2023, 30, 167–173. [Google Scholar] [CrossRef]
- Divison-Garrote, J.A.; Carbayo-Herencia, J.A.; Simarro-Rueda, M.; Molina-Escribano, F.; Escobar-Cervantes, C.; Artigao-Rodenas, L.M.; Gil-Guillén, V.; Banegas, J.R. Prognosis of Systolic Pressure 130 to 139 According to Risk. A Prospective Cohort Study Between 1992 and 2019. Hypertension, 2023; ahead of print. [Google Scholar] [CrossRef]
- WHO Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. (2000). Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. WHO Technical Report Series; 894. Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 31 August 2023).
- Romero-Saldaña, M.; Fuentes-Jiménez, F.J.; Vaquero-Abellán, M.; Álvarez-Fernández, C.; Aguilera-López, M.D.; Molina-Recio, G. Predictive capacity and cutoff value of waist-to-height ratio in the incidence of metabolic syndrome. Clin. Nurs. Res 2019, 28, 676–691. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Gaglia, J.L.; Hilliard, M.E.; Isaacs, D.; et al. 2. Classification and diagnosis of diabetes: Standards of care in diabetes—2023. Diabetes Care 2023, 46 (Suppl. 1), S19–S40. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann. Intern Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 5–14. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Cooney, M.T.; Selmer, R.; Lindman, A.; Tverdal, A.; Menotti, A.; Thomsen, T.; DeBacker, G.; De Bacquer, D.; Tell, G.S.; Njolstad, I.; et al. Cardiovascular disease risk estimation in older persons: SCORE O.P. Eur. J. Prev. Cardiol. 2016, 23, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
| with Hypertension | without Hypertension | Difference in Means | p | |||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | |||
| Age (year) | 2547 | 67.2 (13.3) | 4041 | 47.5 (15.5) | 19.7 | <0.001 |
| Body mass index (kg/m2) | 2547 | 29.8 (5.0) | 4041 | 26.1 (4.7) | 3.7 | <0.001 |
| Abdominal circumference (cm) | 2547 | 99.9 (13.0) | 4041 | 89.2 (13.1) | 10.7 | <0.001 |
| WHtR | 2547 | 0.62 (0.08) | 4041 | 0.54 (0.08) | 0.08 | <0.001 |
| SDB (mmHg) | 2547 | 130.8 (15.3) | 4041 | 116.4 (12.7) | 14.4 | <0.001 |
| DBP (mmHg) | 2547 | 76.6 (9.8) | 4041 | 71.3 (9.2) | 5.3 | <0.001 |
| Pulse pressure (mmHg) | 2547 | 54.2 (13.1) | 4041 | 45.0 (9.6) | 9.2 | <0.001 |
| FPG (mg/dL) a | 2547 | 105.8 (30.8) | 4041 | 89.8 (20.0) | 16.0 | <0.001 |
| HbA1c (%) b | 2192 | 6.0 (1.0) | 3041 | 5.4 (0.7) | 0.6 | <0.001 |
| Total cholesterol (mg/dL) c | 2547 | 190.3 (38.9) | 4041 | 194.3 (39.6) | −4.0 | <0.001 |
| HDL-C (mg/dL) c | 2547 | 53.2 (14.8) | 4041 | 55.8 (14.5) | −2.6 | <0.001 |
| Non-HDL-C (mg/dL) c | 2547 | 137.1 (37.1) | 4041 | 138.5 (41.4) | −1.4 | 0.157 |
| LDL-C (mg/dL) c | 2530 | 110.9 (34.3) | 3996 | 116.2 (34.5) | −5.3 | <0.001 |
| VLDL-C (mg/dL) c | 2530 | 25.6 (12.8) | 3996 | 21.2 (11.7) | 4.4 | <0.001 |
| Triglycerides (mg/dL) d | 2547 | 132.0 (73.2) | 4041 | 113.3 (88.2) | 18.7 | <0.001 |
| Non-HDL-C / HDL-C | 2547 | 2.8 (1.1) | 4041 | 2.7 (1.2) | 0.1 | 0.001 |
| Triglycerides / HDL-C | 2547 | 2.8 (2.2) | 4041 | 2.3 (2.7) | 0.5 | <0.001 |
| TyG index | 2547 | 8.7 (0.6) | 4041 | 8.4 (0.6) | 0.3 | <0.001 |
| Uric acid (mg/dL) e | 2435 | 5,4 (1.5) | 3733 | 4.6 (1.4) | 0.8 | <0.001 |
| AST (U/L) | 1913 | 24.4 (49.1) | 2899 | 22.1 (38.7) | 2.3 | 0.073 |
| ALT (U/L) | 2470 | 25.7 (17.5) | 3943 | 24.3 (16.5) | 1.4 | 0.001 |
| GGT (U/L) | 2352 | 39.0 (52.0) | 3723 | 29.8 (49.8) | 9.2 | <0.001 |
| Creatinine (mg/dL) f | 2547 | 0.90 (0.38) | 4041 | 0.80 (0.22) | 0.10 | <0.001 |
| eGFR (mL/min/1.73 m2) | 2547 | 79.6 (19.8) | 4041 | 97.5 (17.8) | −17.9 | <0.001 |
| uACR (mg/g) g | 2547 | 26.9 (88.8) | 4041 | 9.8 (29.6) | 17.1 | <0.001 |
| with Hypertension | without Hypertension | Difference in Means | p | |||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | |||
| Age (year) | 4104 | 61.5 (15.7) | 2484 | 44.5 (15.1) | 17.0 | <0.001 |
| Body mass index (kg/m2) | 4104 | 29.0 (5.0) | 2484 | 25.0 (4.3) | 4.0 | <0.001 |
| Abdominal circumference (cm) | 4104 | 97.8 (13.2) | 2484 | 86.1 (12.4) | 11.7 | <0.001 |
| WHtR | 4104 | 0.60 (0.08) | 2484 | 0.52 (0.08) | 0.08 | <0.001 |
| SDB (mmHg) | 4104 | 129.2 (13.4) | 2484 | 109.9 (10.2) | 19.3 | <0.001 |
| DBP (mmHg) | 4104 | 76.6 (9.8) | 2484 | 71.3 (9.2) | 5.3 | <0.001 |
| Pulse pressure (mmHg) | 4104 | 51.5 (12.8) | 2484 | 43.8 (8.5) | 7.7 | <0.001 |
| FPG (mg/dL) a | 4104 | 101.3 (29.2) | 2484 | 87.3 (16.1) | 14.0 | <0.001 |
| HbA1c (%) b | 3403 | 5.8 (1.0) | 1830 | 5.3 (0.6) | 0.5 | <0.001 |
| Total cholesterol (mg/dL) c | 4104 | 193.4 (38.6) | 2484 | 191.7 (40.5) | 1.7 | 0.082 |
| HDL-C (mg/dL) c | 4104 | 53.4 (14.5) | 2484 | 57.1 (14.7) | −3.7 | <0.001 |
| Non-HDL-C (mg/dL) c | 4104 | 140.0 (37.3) | 2484 | 134.5 (40.0) | 5.5 | <0.001 |
| LDL-C (mg/dL) c | 4066 | 114.4 (34.0) | 2460 | 113.6 (35.4) | 0.8 | 0.388 |
| VLDL-C (mg/dL) c | 4066 | 24.8 (12.7) | 2460 | 19.8 (10.9) | 5.0 | <0.001 |
| Triglycerides (mg/dL) d | 4104 | 129.9 (83.7) | 2484 | 105.1 (80.0) | 24.8 | <0.001 |
| Non-HDL-C / HDL-C | 4104 | 2.8 (1.1) | 2484 | 2.5 (1.1) | 0.3 | <0.001 |
| Triglycerides / HDL-C | 4104 | 2.8 (2.6) | 2484 | 2.1 (2.5) | 0.7 | <0.001 |
| TyG index | 4104 | 8.6 (0.6) | 2484 | 8.2 (0.6) | 0.4 | <0.001 |
| Uric acid (mg/dL) e | 3870 | 5.2 (1.5) | 2298 | 4.4 (1.4) | 0.8 | <0.001 |
| AST (U/L) | 3030 | 23.9 (39.9) | 2899 | 21.6 (48.1) | 2.3 | 0.072 |
| ALT (U/L) | 3998 | 26.4 (18.6) | 3943 | 22.4 (13.3) | 4.0 | <0.001 |
| GGT (U/L) | 3782 | 37.9 (59.4) | 2293 | 26.0 (30.6) | 11.9 | <0.001 |
| Creatinine (mg/dL) f | 4104 | 0.88 (0.32) | 2484 | 0.78 (0.22) | 0.10 | <0.001 |
| eGFR (mL/min/1.73 m2) | 4104 | 84.8 (20.0) | 2484 | 99.9 (17.7) | −15.1 | <0.001 |
| uACR (mg/g) g | 4104 | 20.9 (74.8) | 2484 | 9.0 (18.8) | 11.9 | <0.001 |
| with HTN 140/90 (%) N = 2547 | without HTN 140/90 (%) N = 4041 | OR (95% CI) | with HTN 130/80 (%) N = 4104 | without HTN 130/80 (%) N = 2484 | OR (95% CI) | |
|---|---|---|---|---|---|---|
| Male | 1224 (48.1) | 1680 (41.6) | 1.3 (1.2–1.4) | 2042 (49.8) | 862 (34.7) | 1.9 (1.7–2.1) |
| Current smoking | 395 (15.5) | 1031 (25.5) | 0.5 (0.5–0.6) | 811 (19.8) | 615 (24.8) | 0.7 (0.7–0.8) |
| Physical inactivity | 1281 (50.3) | 1798 (44.5) | 1.3 (1.1–1.4) | 2007 (48.9) | 1072 (43.2) | 1.3 (1.1–1.4) |
| Overweight | 1053 (41.3) | 1463 (36.2) | 1.2 (1.1–1.4) | 1708 (41.6) | 808 (32.5) | 1.5 (1.3–1.6) |
| Obesity | 1104 (43.4) | 729 (18.0) | 3.5 (3.1–3.9) | 1531 (37.3) | 302 (12.2) | 4.3 (3.8–4.9) |
| Abdominal obesity | 1614 (63.4) | 1308 (32.4) | 3.6 (3.3–4.0) | 2293 (55.9) | 629 (25.3) | 3.7 (3.4–4.2) |
| High WHtR | 2018 (79.2) | 1678 (41.5) | 5.4 (4.8–6.0) | 2889 (70.4) | 807 (32.5) | 4.9 (4.4–5,5) |
| Prediabetes | 754 (29.6) | 695 (17.2) | 2.0 (1.8–2.3) | 1112 (27.1) | 337 (13.6) | 2.4 (2.1–2.7) |
| Diabetes | 771 (30.3) | 264 (6.5) | 6.2 (5.3–7.2) | 917 (22.3) | 118 (4.8) | 5.8 (4.7–7.0) |
| Hypercholesterolemia | 2002 (78.6) | 2099 (51.9) | 3.4 (3.0–3.8) | 2942 (71.7) | 1159 (446.7) | 2.9 (2.6–3.2) |
| Low HDL-C | 856 (33.6) | 963 (23.8) | 1.6 (1.5–1.8) | 1272 (31.0) | 547 (22.0) | 1.6 (1.4–1.8) |
| Hypertriglyceridemia | 1008 (39.6) | 939 (23.2) | 2.2 (1.9–2.4) | 1469 (35.8) | 478 (19.2) | 2.3 (2.1–2.6) |
| Atherogenic dyslipidaemia | 522 (20.5) | 419 (10.4) | 2.2 (2.0–2.6) | 737 (18.0) | 204 (8.2) | 2.4 (2.1–2.9) |
| Hyperuricemia | 562 (21.6) | 257 (6.9) | 3.7 (3.2–4.7) | 670 (17.3) | 113 (4.9) | 4.0 (3.3–5.0) |
| Metabolic syndrome | 1941 (76.2) | 910 (22.5) | 11.0 (9.8–12.4) | 2541 (61.9) | 310 (12.5) | 11.4 (10.0–13.0) |
| CHD | 269 (10.6) | 52 (1.3) | 9.1 (6.7–12.2) | 299 (7.3) | 22 (0.9) | 8.8 (5.7–13.6) |
| Stroke | 196 (7.7) | 54 (1.3) | 6.2 (4.5–8.4) | 219 (5.3) | 31 (1.2) | 4.5 (3.1–6.5) |
| PAD | 126 (4.9) | 24 (0.6) | 8.7 (5.6–13.5) | 133 (3.2) | 17 (0.7) | 4.9 (2.9–8.1) |
| ASCVD | 493 (19.4) | 122 (3.0) | 7.7 (6.3–9.5) | 549 (13.4) | 66 (2.7) | 5.7 (4.4–7.3) |
| Heart failure | 166 (6.5) | 18 (0.4) | 15.6 (9.6–25.4) | 172 (4.2) | 12 (0.5) | 9.0 (5.0–16.2) |
| Atrial fibrillation | 202 (7.9) | 48 (1.2) | 7.2 (5.2–9.9) | 225 (5.5) | 25 (1.0) | 5.7 (3.8–8.7) |
| Erectile dysfunction a | 363 (29.7) | 141 (8.4) | 3.5 (3.0–4.2) | 433 (21.2) | 71 (8.2) | 3.0 (2.3–3.9) |
| Albuminuria | 291 (11.4) | 103 (2.6) | 4.9 (3.9–6.2) | 336 (8.2) | 58 (2.3) | 3.7 (2.8–5.0) |
| Low eGFR | 426 (16.7) | 97 (2.4) | 8.2 (6.5–10.2) | 479 (11.7) | 44 (1.8) | 7.3 (5.4–10.0) |
| CKD | 581 (22.8) | 175 (4.3) | 6.5 (5.5–7.8) | 668 (16.3) | 88 (3.5) | 5.3 (4.2–6.6) |
| Low CVR | 104 (4.1) | 2041 (50.5) | 0.04 (0.03–0.05) | 607 (14.8) | 1538 (61.9) | 0.11 (0.09–0.12) |
| Moderate CVR | 404 (15.9) | 975 (24.1) | 0.6 (0.5–0.7) | 921 (22.4) | 458 (18.4) | 1.2 (1.1–1.4) |
| High CVR | 550 (21.6) | 473 (11.7) | 2.1 (1.8–2.4) | 798 (19.4) | 225 (9.1) | 2.4 (2.1–2.8) |
| Very high CVR | 1489 (58.5) | 552 (13.7) | 8.9 (7.9–10.0) | 1778 (43.3) | 263 (10.6) | 6.5 (5.6–7.4) |
| HTN 140/90 | β a | OR Exp(β) b | pc | HTN 130/80 | β a | OR Exp(β) b | pc |
|---|---|---|---|---|---|---|---|
| Heart failure | 1.52 (0.31) | 4.57 (2.52–8.30) | <0.001 | CHD | 1.31 (0.26) | 3.71 (2.23–6.17) | <0.001 |
| Diabetes | 1.38 (0.09) | 3.97 (3.31–4.77) | <0.001 | Diabetes | 1.26 (0.12) | 3.54 (2.83–4.44) | <0.001 |
| CHD | 1.28 (0.18) | 3.61 (2.51–5.17) | <0.001 | Obesity | 1.21 (0.11) | 3.36 (2.72–4.15) | <0.001 |
| PAD | 1.24 (0.27) | 3.44 (2.04–5.81) | <0.001 | Low eGFR | 1.01 (0.18) | 2.75 (1.95–3.88) | <0.001 |
| Low eGFR | 1.06 (0.14) | 2.89 (2.20–3.78) | <0.001 | Heart failure | 0.96 (0.36) | 2.62 (1.29–5.33) | 0.008 |
| Stroke | 0.99 (0.19) | 2.68 (1.85–3.89) | <0.001 | Hyperuricemia | 0.76 (0.12) | 2.13 (1.70–2.68) | <0.001 |
| Obesity | 0.96 (0.11) | 2.62 (2.11–3.26) | <0.001 | Overweight | 0.69 (0.08) | 2.00 (1.72–2.33) | <0.001 |
| Atrial fibrillation | 0.85 (0.20) | 2.34 (1.58–3.49) | <0.001 | Atrial fibrillation | 0.67 (0.25) | 1.94 (1.19–3.18) | 0.008 |
| Hypercholesterolemia | 0.77 (0.07) | 2.16 (1.89–2.48) | <0.001 | Stroke | 0.66 (0.22) | 1.94 (1.25–3.00) | 0.003 |
| Hyperuricemia | 0.73 (0.10) | 2.07 (1.71–2.50) | <0.001 | Hypercholesterolemia | 0.63 (0.06) | 1.88 (1.66–2.12) | <0.001 |
| High WHtR | 0.69 (0.09) | 1.99 (1.68–2.36) | <0.001 | Prediabetes | 0.61 (0.08) | 1.83 (1.57–2.14) | <0.001 |
| Prediabetes | 0.60 (0.08) | 1.83 (1.58–2.11) | <0.001 | High WHtR | 0.54 (0.08) | 1.71 (1.46–2.00) | <0.001 |
| Overweight | 0.60 (0.09) | 1.82 (1.51–2.18) | <0.001 | PAD * | 0.43 (0.29) | 1.54 (0.87–2.73) | 0.136 |
| Albuminuria | 0.51 (0.15) | 1.67 (1.25–2.24) | 0.001 | Albuminuria * | 0.24 (0.17) | 1.27 (0.90–1.78) | 0.169 |
| without ASCVD or CKD | with ASCVD | with CKD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 140/90 Criterion | 130/80 Criterion | p | 140/90 Criterion | 130/80 Criterion | p | 140/90 Criterion | 130/80 Criterion | p | |
| HTN patients * | 1652 (30.5) | 3074 (56.8) | <0.001 | 493 (80.2) | 549 (89.3) | <0.001 | 581 (76.9) | 668 (88.4) | <0.001 |
| With BP < 140/90 mmHg * | 1472 (89.1) | 2846 (92.6) | <0.001 | 455 (92.3) | 509 (92.7) | 0.797 | 535 (92.1) | 618 (92.5) | 0.776 |
| With BP < 130/80 mmHg * | 999 (60.5) | 2013 (65.5) | <0.001 | 343 (69.6) | 386 (70.3) | 0.795 | 412 (70.9) | 472 (70.7) | 0.923 |
| On BP-lowering drugs * | 1380 (83.5) | 1420 (46.2) | <0.001 | 459 (93.1) | 493 (89.8) | 0.058 | 532 (91.6) | 581 (87.0) | 0.009 |
| Daily BP-lowering drugs § | 1.40 (0.93) | 0.77 (0.97) | <0.001 | 2.19 (1.15) | 2.01 (1.23) | 0.015 | 1.96 (1.10) | 1.73 (1.20) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pallarés-Carratalá, V.; Ruiz-García, A.; Serrano-Cumplido, A.; Arranz-Martínez, E.; Divisón-Garrote, J.A.; Moyá-Amengual, A.; Escobar-Cervantes, C.; Barrios, V. Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study. Medicina 2023, 59, 1846. https://doi.org/10.3390/medicina59101846
Pallarés-Carratalá V, Ruiz-García A, Serrano-Cumplido A, Arranz-Martínez E, Divisón-Garrote JA, Moyá-Amengual A, Escobar-Cervantes C, Barrios V. Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study. Medicina. 2023; 59(10):1846. https://doi.org/10.3390/medicina59101846
Chicago/Turabian StylePallarés-Carratalá, Vicente, Antonio Ruiz-García, Adalberto Serrano-Cumplido, Ezequiel Arranz-Martínez, Juan Antonio Divisón-Garrote, Ana Moyá-Amengual, Carlos Escobar-Cervantes, and Vivencio Barrios. 2023. "Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study" Medicina 59, no. 10: 1846. https://doi.org/10.3390/medicina59101846
APA StylePallarés-Carratalá, V., Ruiz-García, A., Serrano-Cumplido, A., Arranz-Martínez, E., Divisón-Garrote, J. A., Moyá-Amengual, A., Escobar-Cervantes, C., & Barrios, V. (2023). Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study. Medicina, 59(10), 1846. https://doi.org/10.3390/medicina59101846








