Takotsubo Syndrome Occurring after mRNA COVID-19 Vaccination in a Patient with Graves’ Disease
Abstract
:1. Introduction
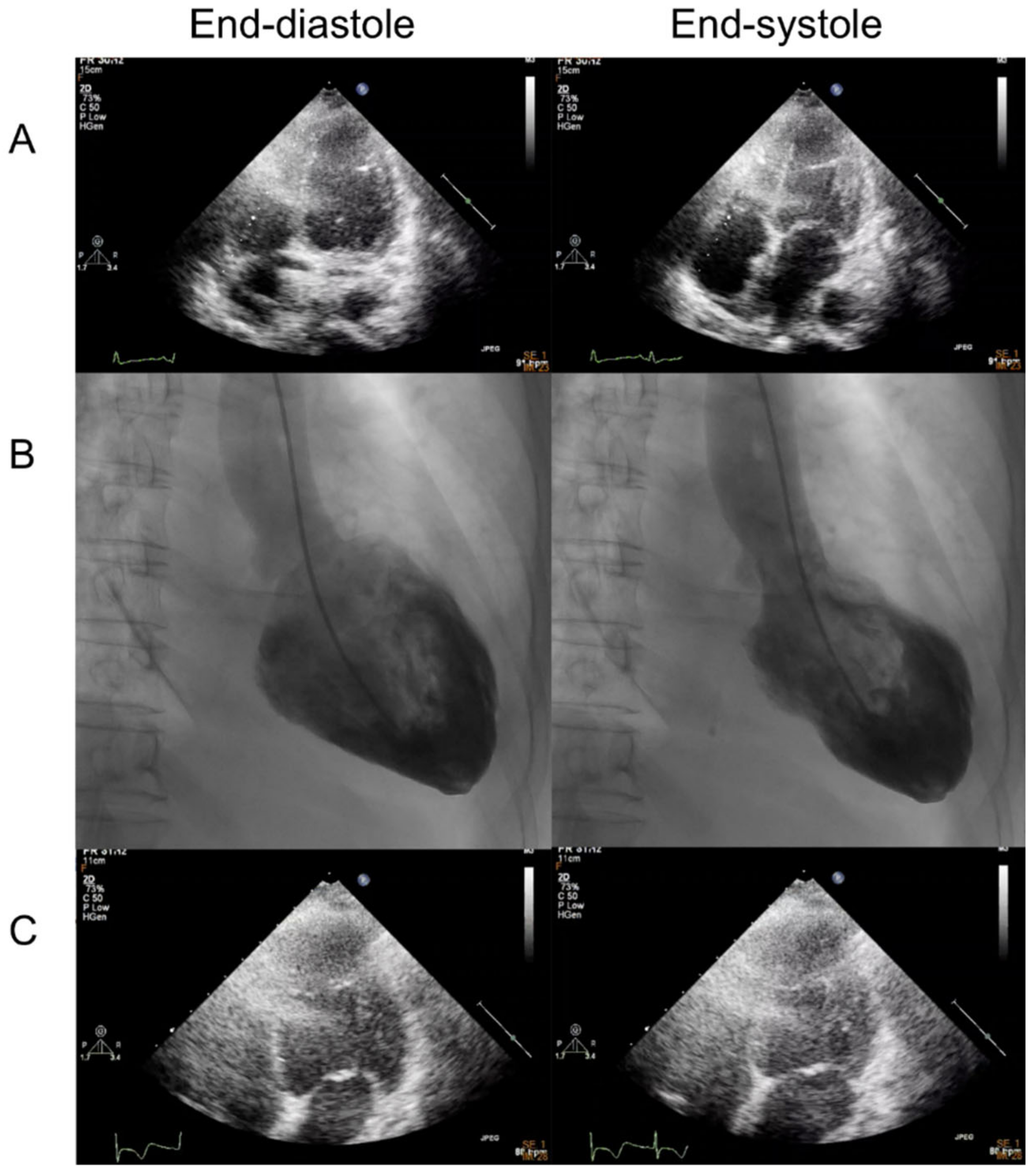
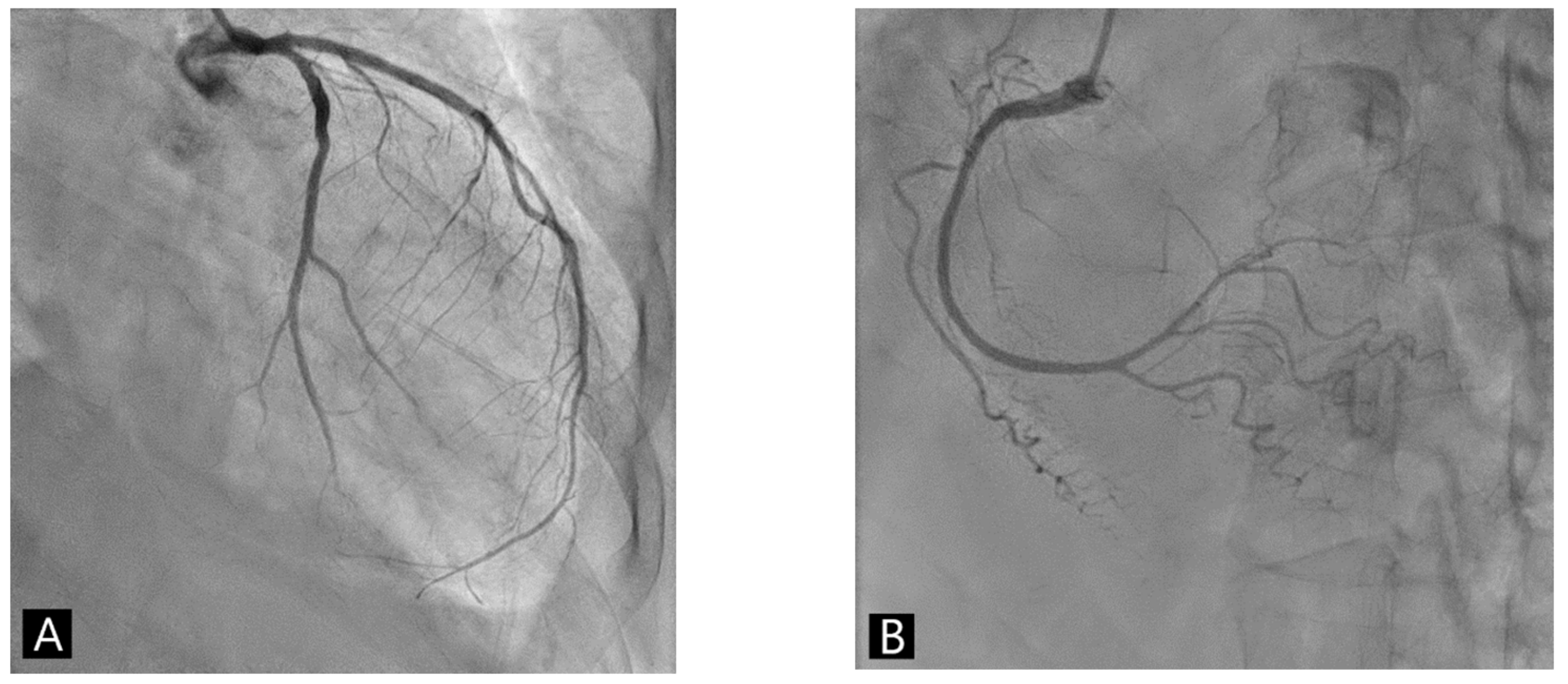
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klein, N.P.; Lewis, N.; Goddard, K.; Fireman, B.; Zerbo, O.; Hanson, K.E.; Donahue, J.G.; Kharbanda, E.O.; Naleway, A.; Nelson, J.C.; et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA 2021, 326, 1390–1399. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Ahmed, S.K.; Mohamed, M.G.; Essa, R.A.; Dabou, E.A.A.R.; Abdulqadir, S.O.; Omar, R.M. Global reports of takotsubo (stress) cardiomyopathy following COVID-19 vaccination: A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2022, 43, 101108. [Google Scholar] [CrossRef]
- Bozkurt, B.; Kamat, I.; Hotez, P.J. Myocarditis with COVID-19 mRNA vaccines. Circulation 2021, 144, 471–484. [Google Scholar] [CrossRef] [PubMed]
- Jani, C.; Leavitt, J.; Al Omari, O.; Dimaso, A.; Pond, K.; Gannon, S.; Chandran, A.K.; Dennis, C.; Colgrove, R. COVID-19 vaccine-associated takotsubo cardiomyopathy. Am. J. Ther. 2021, 28, 361–364. [Google Scholar] [CrossRef]
- Berto, M.B.; Spano, G.; Wagner, B.; Bernhard, B.; Häner, J.; Huber, A.T.; Gräni, C. Takotsubo cardiomyopathy after mRNA COVID-19 vaccination. Heart Lung Circ. 2021, 30, e119–e120. [Google Scholar] [CrossRef]
- Toida, R.; Uezono, S.; Komatsu, H.; Toida, T.; Imamura, A.; Fujimoto, S.; Kaikita, K. Takotsubo cardiomyopathy after vaccination for coronavirus disease 2019 in a patient on maintenance hemodialysis. CEN Case Rep. 2022, 11, 220–224. [Google Scholar] [CrossRef]
- Stewart, C.; Gamble, D.T.; Dawson, D. Novel case of takotsubo cardiomyopathy following COVID-19 vaccination. BMJ Case Rep. 2022, 15, e247291. [Google Scholar] [CrossRef] [PubMed]
- Fearon, C.; Parwani, P.; Gow-Lee, B.; Abramov, D. Takotsubo syndrome after receiving the COVID-19 vaccine. J. Cardiol. Cases 2021, 24, 223–226. [Google Scholar] [CrossRef]
- Crane, P.; Wong, C.; Mehta, N.; Barlis, P. Takotsubo (stress) cardiomyopathy after ChAdOx1 nCoV-19 vaccination. BMJ Case Rep. 2021, 14, e246580. [Google Scholar] [CrossRef] [PubMed]
- Vidula, M.K.; Ambrose, M.; Glassberg, H.; Chokshi, N.; Chen, T.; Ferrari, V.A.; Han, Y. Myocarditis and other cardiovascular complications of the mRNA-based COVID-19 vaccines. Cureus 2021, 13, e15576. [Google Scholar] [CrossRef]
- Yamaura, H.; Ishikawa, H.; Otsuka, K.; Kasayuki, N. Reverse takotsubo cardiomyopathy as a cause of acute chest pain in a young woman following COVID-19 vaccination. Circ. Cardiovasc. Imaging 2022, 15, e013661. [Google Scholar] [CrossRef]
- Tedeschi, A.; Camilli, M.; Ianni, U.; Tavecchia, G.; Palazzini, M.; Cartella, I.; Gentile, P.; Quattrocchi, G.; Spanò, F.M.; Cipriani, M.; et al. Takotsubo syndrome after BNT162b2 mRNA COVID-19 vaccine: Emotional or causative relationship with vaccination? Int. J. Cardiol. Heart Vasc. 2022, 40, 101002. [Google Scholar] [CrossRef]
- Ricci, G.; Citarelli, G.; De Laura, D.; Degennaro, L.; Ligurgo, L.; Sassara, M.; Corriero, F.; Musci, S.; Desario, P.; Rutigliano, D.; et al. P311 takotsubo cardiomyopathy related to MRNA SARS–CoV-2 vaccine. Eur. Heart J. Suppl. 2022, 24 (Suppl. C), suac012-298. [Google Scholar] [CrossRef]
- Vojdani, A.; Kharrazian, D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin. Immunol. 2020, 217, 108480. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Desai, R.; Gandhi, Z.; Fong, H.K.; Doreswamy, S.; Desai, V.; Chockalingam, A.; Mehta, P.K.; Sachdeva, R.; Kumar, G. Takotsubo syndrome in patients with COVID-19: A systematic review of published cases. SN Compr. Clin. Med. 2020, 2, 2102–2108. [Google Scholar] [CrossRef] [PubMed]
- Sriphrapradang, C.; Shantavasinkul, P.C. Graves’ disease following SARS-CoV-2 vaccination. Endocrine 2021, 74, 473–474. [Google Scholar] [CrossRef] [PubMed]
- Komamura, K.; Fukui, M.; Iwasaku, T.; Hirotani, S.; Masuyama, T. Takotsubo cardiomyopathy: Pathophysiology, diagnosis and treatment. World J. Cardiol. 2014, 6, 602–609. [Google Scholar] [CrossRef]
- Watad, A.; Quaresma, M.; Bragazzi, N.L.; Cervera, R.; Tervaert, J.W.C.; Amital, H.; Shoenfeld, Y. The autoimmune/inflammatory syndrome induced by adjuvants (ASIA)/Shoenfeld’s syndrome: Descriptive analysis of 300 patients from the international ASIA syndrome registry. Clin. Rheumatol. 2018, 37, 483–493. [Google Scholar] [CrossRef]
- Aweimer, A.; El-Battrawy, I.; Akin, I.; Borggrefe, M.; Mügge, A.; Patsalis, P.C.; Urban, A.; Kummer, M.; Vasileva, S.; Stachon, A.; et al. Abnormal thyroid function is common in takotsubo syndrome and depends on two distinct mechanisms: Results of a multicentre observational study. J. Intern. Med. 2021, 289, 675–687. [Google Scholar] [CrossRef]
- Rueda, D.; Aguirre, R.; Contardo, D.; Finocchietto, P.; Hernandez, S.; di Fonzo, H. Takotsubo myocardiopathy and hyperthyroidism: A case report and literature review. Am. J. Case Rep. 2017, 18, 865–870. [Google Scholar] [CrossRef]

| Author/Year of Publication | Jani et al. [5] | Boscolo Berto et al. [6] | Toida et al. [7] | Caitlin Stewart et al. 2021 [8] | Fearon et al. [9] | Crane et al. [10] | Vidula et al. [11] | Hiroki Yamaura et al. 2022 [12] | Tedeschi et al. [13] | Ricci et al. [14] | The Present Case |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | United States | Switzerland | Japan | United Kingdom | United States | Australia | United States | Japan | Italy | Italy | Taiwan |
| Age, year | 65 | 63 | 80 | 50 | 73 | 72 | 60 | 30 | 71 | 54 | 67 |
| Sex | Female | Female | Female | Female | Female | Male | Female | Female | Female | Female | Female |
| Comorbidities | Hyperlipidemia | None | Renal sclerosis on maintenance hemodialysis, hypertension | Chronic obstructive pulmonary disease | Chronic kidney disease, hypertension | Ischemic heart disease, hypertension, type 2 diabetes mellitus, ulcerative colitis | Coronary artery disease | None | Congenital Long QT Syndrome | None | Thyrotoxicosis |
| Vaccine received | mRNA-1273 | mRNA-1273 | Pfizer-BioNTech | ChadOX1 nCOV-19 | mRNA-1273 | ChadOX1 nCOV-19 | Pfizer-BioNTech | Pfizer-BioNTech | Pfizer-BioNTech | mRNA-1273 | mRNA-1273 |
| Doses received | 1 | 1 | 1 | 2 | NA | 1 | 2 | 2 | 1 | 2 | 1 |
| Interval after vaccination, days | 3 | 1 | 1 | 7 | 1 | 4 | 4 | 2 | <1 | <1 | 7 |
| Symptoms | chest pain, myalgia, nausea, headache | dyspnea and fever | general fatigue and loss of appetite | chest pain | chest pain, shortness of breath, fatigue, and nausea | chest pain, fatigue, myalgias, and fever | chest pain | chest pain and cold sweat | chest pain and shortness of breath | palpitations, asthenia, and intermittent chest tightness | chest pain, palpitation, dyspnea on exertion, nausea, and diarrhea |
| LVEF (%) | 35% | 40% | 48% | NA | 65% | 60% | 47% | NA | 38% | 40% | 45% |
| Electrocardiogram (ECG) | Evolving ST-T changes suggestive of inferolateral ischemia | TWI over the inferior/anterior leads | TWI in I, aVL, and V3-6, and a prolonged QTc | Anterior T wave inversion and a prolonged QTc | ST-T changes of inferolateral ischemia and PRWP | First-degree and RBBB without acute or dynamic ischemic changes | Inferolateral TWI | ST-segment depression on the V4-V6 leads | TWI in all leads except for aVL and aVF, and prolonged QTc | PRWP and TWI in inferior leads and from V3 to V6. | ST-T changes of inferior/anterior leads |
| Troponin (mcg/L) | 5.7 (Tn) | 3.20 (hsTnT) | 2.26 (Tn) | 1.66 (Tn) | 220 (Tn) | 1.86 (Tn) | 0.12 (Tn) | 1.00 (Tn) | 0.34 (hsTnT) | Elevated | 1298 (hsTnI) |
| NT-proBNP (ng/L) | NA | 10,180 | NA | NA | >70,000 | NA | NA | NA | 2261 | Elevated | 3872 |
| Therapy | |||||||||||
| beta-blocker | Low-dose metoprolol | NA | None | None | Metoprolol | NA | Metoprolol | None | NA | NA | Low-dose bisoprolol |
| ACEi/ARB | Lisinopril | NA | None | None | Losartan | NA | Lisinopril | None | NA | NA | None |
| Length of hospital stay (days) | NA | NA | 13 | 5 | 8 | 10 | NA | 15 | NA | NA | 6 |
| Outcome | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged | Uneventfully Discharged |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-C.; Lin, G.-M.; Takimoto, E.; Lin, C.-S.; Lin, W.-Y.; Wu, C.-H.; Huang, C.-L.; Cheng, C.-C.; Cheng, S.-M.; Lin, S.-H.; et al. Takotsubo Syndrome Occurring after mRNA COVID-19 Vaccination in a Patient with Graves’ Disease. Medicina 2023, 59, 94. https://doi.org/10.3390/medicina59010094
Chen Y-C, Lin G-M, Takimoto E, Lin C-S, Lin W-Y, Wu C-H, Huang C-L, Cheng C-C, Cheng S-M, Lin S-H, et al. Takotsubo Syndrome Occurring after mRNA COVID-19 Vaccination in a Patient with Graves’ Disease. Medicina. 2023; 59(1):94. https://doi.org/10.3390/medicina59010094
Chicago/Turabian StyleChen, Yen-Chi, Gen-Min Lin, Eiki Takimoto, Chin-Sheng Lin, Wen-Yu Lin, Chun-Hsien Wu, Chia-Luen Huang, Cheng-Chung Cheng, Shu-Meng Cheng, Shih-Hua Lin, and et al. 2023. "Takotsubo Syndrome Occurring after mRNA COVID-19 Vaccination in a Patient with Graves’ Disease" Medicina 59, no. 1: 94. https://doi.org/10.3390/medicina59010094
APA StyleChen, Y.-C., Lin, G.-M., Takimoto, E., Lin, C.-S., Lin, W.-Y., Wu, C.-H., Huang, C.-L., Cheng, C.-C., Cheng, S.-M., Lin, S.-H., Komuro, I., & Liu, P.-Y. (2023). Takotsubo Syndrome Occurring after mRNA COVID-19 Vaccination in a Patient with Graves’ Disease. Medicina, 59(1), 94. https://doi.org/10.3390/medicina59010094








