Updates on Epstein–Barr Virus (EBV)-Associated Nasopharyngeal Carcinoma: Emphasis on the Latent Gene Products of EBV
Abstract
1. Introduction
2. Definition of Nasopharyngeal Carcinoma
2.1. Staging of NPC
2.2. Diagnostic Features of NPC
2.3. Morphological Similarity of Undifferentiated Carcinomas of Nasopharyngeal Type (UCNT)
3. Symptoms and Transmission
- ➢
- Neck lymph node enlargement.
- ➢
- Bleeding from the mouth or nose.
- ➢
- Ear-related issues and hearing loss caused by the tumor’s closeness to the Eustachian tube, which causes obstruction and fluid collection in the middle ear.
- ➢
- Sore throat.
- ➢
- Difficulty breathing through the nose.
- ➢
- Headache.
- ➢
- The most common method of EBV transmission is via bodily fluids, notably saliva. EBV may, however, be spread by blood and sperm during sexual activity, blood transfusions, and organ transplants.
- ➢
- EBV may be transmitted by touching an infected individual’s recently used drinking glass or toothbrush. The virus is likely to live on a surface for as long as it stays moist.
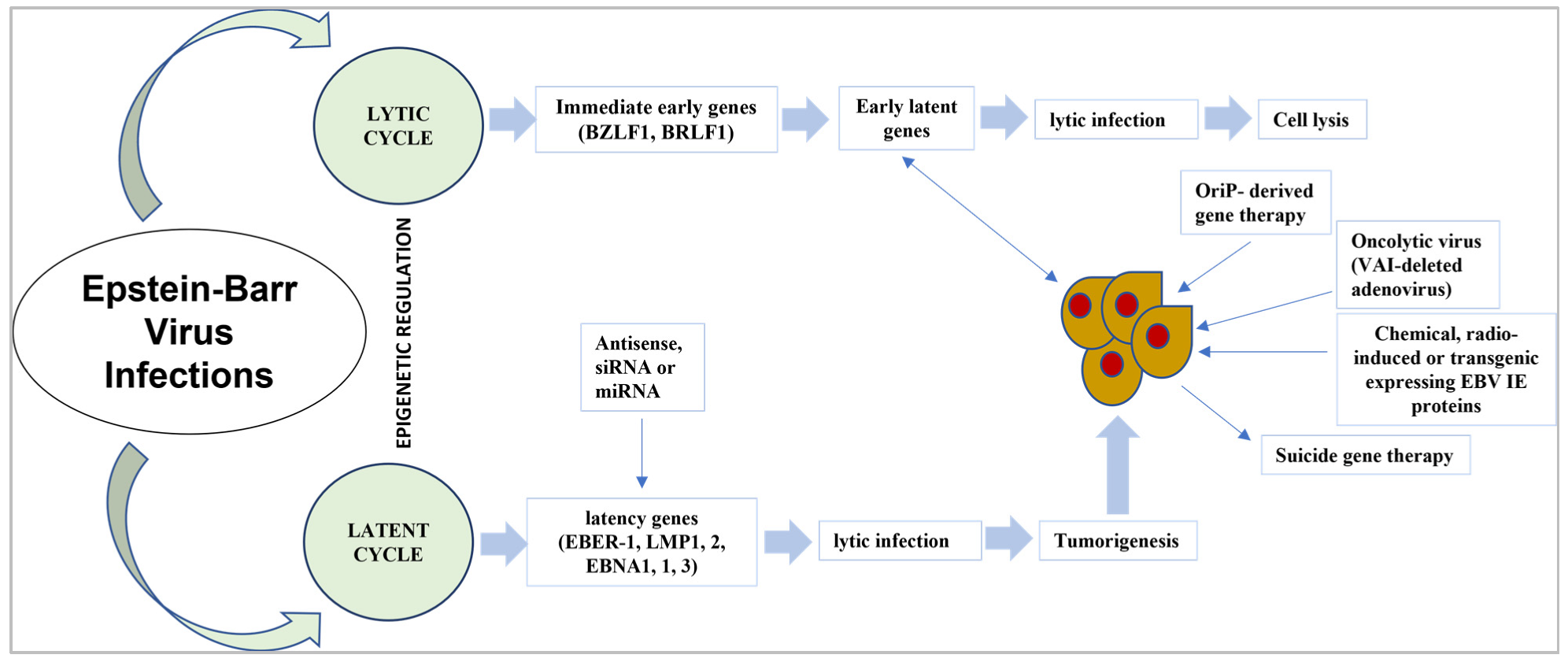
4. Latent Gene Products of EBV
4.1. Expression of EBV Latent Gene in Virus-Associated Tumors
4.2. Targeting the EBV Latent Proteins
4.3. Therapeutic Targeting of EBNA1
4.4. Latent EBV Genes’ Expression in NPC and Their Function
4.4.1. LMPs and EBNA1
4.4.2. LMP1
4.4.3. BamHI-A and EBER Regions
4.4.4. EBV Strain Variation
5. Primary Gene Product (Genetic Variability)
EBV-Related Head and Neck Cancers (Adoptive VST Therapy)
6. Risk Factors
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsang, C.M.; Yip, Y.L.; Lo, K.W.; Deng, W.; To, K.F.; Hau, P.M.; Lau, V.M.Y.; Takada, K.; Lui, V.W.Y.; Lung, M.L. Cyclin D1 overexpression supports stable EBV infection in nasopharyngeal epithelial cells. Proc. Natl. Acad. Sci. USA 2012, 109, E3473–E3482. [Google Scholar] [CrossRef] [PubMed]
- Young, L.S.; Dawson, C.W. Epstein-Barr virus and nasopharyngeal carcinoma. Chin. J. Cancer 2014, 33, 581. [Google Scholar] [CrossRef] [PubMed]
- Sousa, H.; Pinto-Correia, A.L.; Medeiros, R.; Dinis-Ribeiro, M. Epstein-Barr virus is associated with gastric carcinoma: The question is what is the significance? World J. Gastroenterol. WJG 2008, 14, 4347. [Google Scholar] [CrossRef] [PubMed]
- Albanese, M.; Tagawa, T.; Bouvet, M.; Maliqi, L.; Lutter, D.; Hoser, J.; Hastreiter, M.; Hayes, M.; Sugden, B.; Martin, L. Epstein–Barr virus microRNAs reduce immune surveillance by virus-specific CD8+ T cells. Proc. Natl. Acad. Sci. USA 2016, 113, E6467–E6475. [Google Scholar] [CrossRef] [PubMed]
- Tao, Q.; Young, L.S.; Woodman, C.B.; Murray, P.G. Epstein-Barr virus (EBV) and its associated human cancers—Genetics, epigenetics, pathobiology and novel therapeutics. Front. Biosci. Landmark 2006, 11, 2672–2713. [Google Scholar] [CrossRef]
- Brady, G.; MacArthur, G.; Farrell, P. Epstein–Barr virus and Burkitt lymphoma. Postgrad. Med. J. 2008, 84, 372–377. [Google Scholar] [CrossRef]
- Teow, S.-Y.; Yap, H.-Y.; Peh, S.-C. Epstein-barr virus as a promising immunotherapeutic target for nasopharyngeal carcinoma treatment. J. Pathog. 2017, 2017, 7349268. [Google Scholar] [CrossRef]
- Al-Mozaini, M.; Bodelon, G.; Karstegl, C.E.; Jin, B.; Al-Ahdal, M.; Farrell, P.J. Epstein–Barr virus BART gene expression. J. Gen. Virol. 2009, 90, 307–316. [Google Scholar] [CrossRef]
- Zur Hausen, A.; Van Rees, B.; Van Beek, J.; Craanen, M.; Bloemena, E.; Offerhaus, G.; Meijer, C.; van den Brule, A. Epstein-Barr virus in gastric carcinomas and gastric stump carcinomas: A late event in gastric carcinogenesis. J. Clin. Pathol. 2004, 57, 487–491. [Google Scholar] [CrossRef]
- Shannon-Lowe, C.; Rowe, M. Epstein-Barr virus infection of polarized epithelial cells via the basolateral surface by memory B cell-mediated transfer infection. PLoS Pathog. 2011, 7, e1001338. [Google Scholar] [CrossRef]
- Kennedy, G.; Komano, J.; Sugden, B. Epstein-Barr virus provides a survival factor to Burkitt’s lymphomas. Proc. Natl. Acad. Sci. USA 2003, 100, 14269–14274. [Google Scholar] [CrossRef] [PubMed]
- Tzellos, S.; Farrell, P.J. Epstein-Barr virus sequence variation—Biology and disease. Pathogens 2012, 1, 156–175. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.I. Epstein–barr virus vaccines. Clin. Transl. Immunol. 2015, 4, e32. [Google Scholar] [CrossRef]
- Lee, C.-H.; Yeh, T.-H.; Lai, H.-C.; Wu, S.-Y.; Su, I.-J.; Takada, K.; Chang, Y. Epstein-Barr virus Zta-induced immunomodulators from nasopharyngeal carcinoma cells upregulate interleukin-10 production from monocytes. J. Virol. 2011, 85, 7333–7342. [Google Scholar] [CrossRef] [PubMed]
- Young, L.S.; Rickinson, A.B. Epstein–Barr virus: 40 years on. Nat. Rev. Cancer 2004, 4, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Tierney, R.J.; Edwards, R.H.; Sitki-Green, D.; Croom-Carter, D.; Roy, S.; Yao, Q.-Y.; Raab-Traub, N.; Rickinson, A.B. Multiple Epstein-Barr virus strains in patients with infectious mononucleosis: Comparison of ex vivo samples with in vitro isolates by use of heteroduplex tracking assays. J. Infect. Dis. 2006, 193, 287–297. [Google Scholar] [CrossRef]
- Khabir, A.; Karray, H.; Rodriguez, S.; Rosé, M.; Daoud, J.; Frikha, M.; Boudawara, T.; Middeldorp, J.; Jlidi, R.; Busson, P. EBV latent membrane protein 1 abundance correlates with patient age but not with metastatic behavior in north African nasopharyngeal carcinomas. Virol. J. 2005, 2, 39. [Google Scholar] [CrossRef]
- Dawson, C.W.; Port, R.J.; Young, L.S. The role of the EBV-encoded latent membrane proteins LMP1 and LMP2 in the pathogenesis of nasopharyngeal carcinoma (NPC). Semin. Cancer Biol. 2012, 22, 144–153. [Google Scholar] [CrossRef]
- Frappier, L. Role of EBNA1 in NPC tumourigenesis. Semin. Cancer Biol. 2012, 22, 154–161. [Google Scholar] [CrossRef]
- Houali, K.; Wang, X.; Shimizu, Y.; Djennaoui, D.; Nicholls, J.; Fiorini, S.; Bouguermouh, A.; Ooka, T. A new diagnostic marker for secreted Epstein-Barr virus–encoded LMP1 and BARF1 oncoproteins in the serum and saliva of patients with nasopharyngeal carcinoma. Clin. Cancer Res. 2007, 13, 4993–5000. [Google Scholar] [CrossRef]
- Stoker, S.D.; Novalić, Z.; Wildeman, M.A.; Huitema, A.D.; Verkuijlen, S.A.; Juwana, H.; Greijer, A.E.; Tan, I.B.; Middeldorp, J.M.; de Boer, J.P. Epstein–Barr virus-targeted therapy in nasopharyngeal carcinoma. J. Cancer Res. Clin. Oncol. 2015, 141, 1845–1857. [Google Scholar] [CrossRef]
- Prabhu, S.R.; Wilson, D.F. Evidence of Epstein-Barr virus association with head and neck cancers: A review. J. Can. Dent. Assoc. 2016, 82, 1488–2159. [Google Scholar]
- Ji, X.; Zhang, W.; Xie, C.; Wang, B.; Zhang, G.; Zhou, F. Nasopharyngeal carcinoma risk by histologic type in central China: Impact of smoking, alcohol and family history. Int. J. Cancer 2011, 129, 724–732. [Google Scholar] [CrossRef]
- Wu, L.; Li, C.; Pan, L. Nasopharyngeal carcinoma: A review of current updates. Exp. Ther. Med. 2018, 15, 3687–3692. [Google Scholar] [CrossRef]
- Bossi, P.; Chan, A.; Licitra, L.; Trama, A.; Orlandi, E.; Hui, E.; Halámková, J.; Mattheis, S.; Baujat, B.; Hardillo, J. Nasopharyngeal carcinoma: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 452–465. [Google Scholar] [CrossRef]
- Chou, J.; Lin, Y.C.; Kim, J.; You, L.; Xu, Z.; He, B.; Jablons, D.M. Nasopharyngeal carcinoma—Review of the molecular mechanisms of tumorigenesis. Head Neck 2008, 30, 946–963. [Google Scholar] [CrossRef]
- Read, S.A.; Douglas, M.W. Virus induced inflammation and cancer development. Cancer Lett. 2014, 345, 174–181. [Google Scholar] [CrossRef]
- Lung, H.L.; Cheung, A.K.L.; Ko, J.M.Y.; Cheng, Y.; Stanbridge, E.J.; Lung, M.L. Deciphering the molecular genetic basis of NPC through functional approaches. Semin. Cancer Biol. 2012, 22, 87–95. [Google Scholar] [CrossRef]
- Lo, K.-W.; Chung, G.T.-Y.; To, K.-F. Deciphering the molecular genetic basis of NPC through molecular, cytogenetic, and epigenetic approaches. Semin. Cancer Biol. 2012, 22, 79–86. [Google Scholar] [CrossRef]
- Ji, M.; Sheng, W.; Cheng, W.; Ng, M.; Wu, B.; Yu, X.; Wei, K.; Li, F.; Lian, S.; Wang, P. Incidence and mortality of nasopharyngeal carcinoma: Interim analysis of a cluster randomized controlled screening trial (PRO-NPC-001) in southern China. Ann. Oncol. 2019, 30, 1630–1637. [Google Scholar] [CrossRef]
- Louis, C.U.; Straathof, K.; Bollard, C.M.; Ennamuri, S.; Gerken, C.; Lopez, T.T.; Huls, M.H.; Sheehan, A.; Wu, M.-F.; Liu, H. Adoptive transfer of EBV-specific T cells results in sustained clinical responses in patients with locoregional nasopharyngeal carcinoma. J. Immunother. 2010, 33, 983. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.-Y.; Wen, Y.-F.; Guo, L.; Liu, H.; Huang, P.-Y.; Mo, H.-Y.; Li, N.-W.; Xiang, Y.-Q.; Luo, D.-H.; Qiu, F. Concurrent chemoradiotherapy vs. radiotherapy alone in stage II nasopharyngeal carcinoma: Phase III randomized trial. J. Natl. Cancer Inst. 2011, 103, 1761–1770. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Fang, X.; Feng, Z.; Guo, Y.-M.; Peng, R.-J.; Liu, T.; Huang, Z.; Feng, Y.; Sun, X.; Xiong, Z. Direct sequencing and characterization of a clinical isolate of Epstein-Barr virus from nasopharyngeal carcinoma tissue by using next-generation sequencing technology. J. Virol. 2011, 85, 11291–11299. [Google Scholar] [CrossRef] [PubMed]
- Abdulamir, A.; Hafidh, R.; Abdulmuhaimen, N.; Abubakar, F.; Abbas, K. The distinctive profile of risk factors of nasopharyngeal carcinoma in comparison with other head and neck cancer types. BMC Public Health 2008, 8, 400. [Google Scholar] [CrossRef] [PubMed]
- Xiong, F.; Deng, S.; Huang, H.-B.; Li, X.-Y.; Zhang, W.-L.; Liao, Q.-J.; Ma, J.; Li, X.-L.; Xiong, W.; Li, G.-Y. Effects and mechanisms of innate immune molecules on inhibiting nasopharyngeal carcinoma. Chin. Med. J. 2019, 132, 749–752. [Google Scholar] [CrossRef]
- Li, J.-H.; Shi, W.; Chia, M.; Sanchez-Sweatman, O.; Siatskas, C.; Huang, D.; Busson, P.; Klamut, H.; Yeh, W.-C.; Richardson, C. Efficacy of targeted FasL in nasopharyngeal carcinoma. Mol. Ther. 2003, 8, 964–973. [Google Scholar] [CrossRef]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Anzai, Y.; Brizel, D.M.; Bruce, J.Y.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J. Head and neck cancers, version 2.2020, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 873–898. [Google Scholar] [CrossRef]
- Katzman, R.B.; Longnecker, R. Cholesterol-dependent infection of Burkitt’s lymphoma cell lines by Epstein–Barr virus. J. Gen. Virol. 2003, 84, 2987–2992. [Google Scholar] [CrossRef]
- Chan, K.A.; Hung, E.C.; Woo, J.K.; Chan, P.K.; Leung, S.F.; Lai, F.P.; Cheng, A.S.; Yeung, S.W.; Chan, Y.W.; Tsui, T.K. Early detection of nasopharyngeal carcinoma by plasma Epstein-Barr virus DNA analysis in a surveillance program. Cancer 2013, 119, 1838–1844. [Google Scholar] [CrossRef]
- Smith, C.; Tsang, J.; Beagley, L.; Chua, D.; Lee, V.; Li, V.; Moss, D.J.; Coman, W.; Chan, K.H.; Nicholls, J. Effective treatment of metastatic forms of Epstein-Barr virus–associated nasopharyngeal carcinoma with a novel adenovirus-based adoptive immunotherapy. Cancer Res. 2012, 72, 1116–1125. [Google Scholar] [CrossRef]
- Kwok, H.; Wu, C.; Palser, A.; Kellam, P.; Sham, P.; Kwong, D.; Chiang, A. Genomic diversity of Epstein-Barr virus genomes isolated from primary nasopharyngeal carcinoma biopsy samples. J. Virol. 2014, 88, 10662–10672. [Google Scholar] [CrossRef]
- Wei, K.R.; Xu, Y.; Liu, J.; Zhang, W.-J.; Liang, Z.-H. Histopathological classification of nasopharyngeal carcinoma. Asian Pac. J. Cancer Prev. 2011, 12, 1141–1147. [Google Scholar]
- Lee, H.S.; Chang, M.S.; Yang, H.-K.; Lee, B.L.; Kim, W.H. Epstein-Barr virus-positive gastric carcinoma has a distinct protein expression profile in comparison with Epstein-Barr virus-negative carcinoma. Clin. Cancer Res. 2004, 10, 1698–1705. [Google Scholar] [CrossRef]
- Sivachandran, N.; Wang, X.; Frappier, L. Functions of the Epstein-Barr virus EBNA1 protein in viral reactivation and lytic infection. J. Virol. 2012, 86, 6146–6158. [Google Scholar] [CrossRef]
- Song, H.-J.; Kim, K.-M. Pathology of epstein-barr virus-associated gastric carcinoma and its relationship to prognosis. Gut Liver 2011, 5, 143. [Google Scholar] [CrossRef]
- Hohaus, S.; Santangelo, R.; Giachelia, M.; Vannata, B.; Massini, G.; Cuccaro, A.; Martini, M.; Cesarini, V.; Cenci, T.; D’Alo, F. The viral load of Epstein–Barr virus (EBV) DNA in peripheral blood predicts for biological and clinical characteristics in Hodgkin lymphoma. Clin. Cancer Res. 2011, 17, 2885–2892. [Google Scholar] [CrossRef]
- Hochberg, D.; Souza, T.; Catalina, M.; Sullivan, J.L.; Luzuriaga, K.; Thorley-Lawson, D.A. Acute infection with Epstein-Barr virus targets and overwhelms the peripheral memory B-cell compartment with resting, latently infected cells. J. Virol. 2004, 78, 5194–5204. [Google Scholar] [CrossRef]
- Tsang, C.M.; Lui, V.W.Y.; Bruce, J.P.; Pugh, T.J.; Lo, K.W. Translational genomics of nasopharyngeal cancer. Semin. Cancer Biol. 2020, 61, 84–100. [Google Scholar] [CrossRef]
- Thompson, L.D. Update on nasopharyngeal carcinoma. Head Neck Pathol. 2007, 1, 81–86. [Google Scholar] [CrossRef]
- Seto, E.; Ooka, T.; Middeldorp, J.; Takada, K. Reconstitution of Nasopharyngeal Carcinoma–Type EBV Infection Induces Tumorigenicity. Cancer Res. 2008, 68, 1030–1036. [Google Scholar] [CrossRef]
- Peterson, B.R.; Nelson, B.L. Nonkeratinizing undifferentiated nasopharyngeal carcinoma. Head Neck Pathol. 2013, 7, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.; Lee, V.; Schuessler, A.; Beagley, L.; Rehan, S.; Tsang, J.; Li, V.; Tiu, R.; Smith, D.; Neller, M.A. Pre-emptive and therapeutic adoptive immunotherapy for nasopharyngeal carcinoma: Phenotype and effector function of T cells impact on clinical response. Oncoimmunology 2017, 6, e1273311. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Jiang, C.; Wang, L.; Yan, F.; Sun, Q.; Ye, Z.; Liu, T.; Fu, Z.; Jiang, Y. Influence of concurrent chemotherapy on locoregionally advanced nasopharyngeal carcinoma treated with neoadjuvant chemotherapy plus intensity-modulated radiotherapy: A retrospective matched analysis. Sci. Rep. 2020, 10, 2489. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, S.H.; Han, S.H.; An, J.S.; Lee, E.S.; Kim, Y.S. Clinicopathological and molecular characteristics of Epstein–Barr virus-associated gastric carcinoma: A meta-analysis. J. Gastroenterol. Hepatol. 2009, 24, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Corvalan, A.; Ding, S.; Koriyama, C.; Carrascal, E.; Carrasquilla, G.; Backhouse, C.; Urzua, L.; Argandoña, J.; Palma, M.; Eizuru, Y. Association of a distinctive strain of Epstein-Barr virus with gastric cancer. Int. J. Cancer 2006, 118, 1736–1742. [Google Scholar] [CrossRef]
- Plummer, M.; de Martel, C.; Vignat, J.; Ferlay, J.; Bray, F.; Franceschi, S. Global burden of cancers attributable to infections in 2012: A synthetic analysis. Lancet Glob. Health 2016, 4, e609–e616. [Google Scholar] [CrossRef]
- Tsao, S.W.; Tsang, C.M.; To, K.F.; Lo, K.W. The role of Epstein–Barr virus in epithelial malignancies. J. Pathol. 2015, 235, 323–333. [Google Scholar] [CrossRef]
- Ugel, S.; De Sanctis, F.; Mandruzzato, S.; Bronte, V. Tumor-induced myeloid deviation: When myeloid-derived suppressor cells meet tumor-associated macrophages. J. Clin. Investig. 2015, 125, 3365–3376. [Google Scholar] [CrossRef]
- Hamarsheh, S.A.; Zeiser, R. NLRP3 inflammasome activation in cancer: A double-edged sword. Front. Immunol. 2020, 11, 1444. [Google Scholar] [CrossRef]
- Balahura, L.R.; Selaru, A.; Dinescu, S.; Costache, M. Inflammation and inflammasomes: Pros and cons in tumorigenesis. J. Immunol. Res. 2020, 2020, 2549763. [Google Scholar] [CrossRef]
- Wang, K.; Yuen, S.T.; Xu, J.; Lee, S.P.; Yan, H.H.; Shi, S.T.; Siu, H.C.; Deng, S.; Chu, K.M.; Law, S. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat. Genet. 2014, 46, 573–582. [Google Scholar] [CrossRef]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef]
- Jochum, S.; Moosmann, A.; Lang, S.; Hammerschmidt, W.; Zeidler, R. The EBV immunoevasins vIL-10 and BNLF2a protect newly infected B cells from immune recognition and elimination. PLoS Pathog. 2012, 8, e1002704. [Google Scholar] [CrossRef]
- Abusalah, M.A.H.; Binti Hassan, S.A.; Mat Lazim, N.; Abdullah, B.; Binti Wan Sohaimi, W.F.; Husin, A.; Cheng, K.Y.; Yean, C.Y. Design of InnoPrimers-Duplex Real-Time PCR for Detection and Treatment Response Prediction of EBV-Associated Nasopharyngeal Carcinoma Circulating Genetic Biomarker. Diagnostics 2021, 11, 1761. [Google Scholar] [CrossRef]
- Dias, J.M.; Santana, I.V.; da Silva, V.D.; Carvalho, A.L.; Arantes, L.M. Analysis of Epstein–Barr Virus (EBV) and PD-L1 Expression in Nasopharyngeal Carcinoma Patients in a Non-Endemic Region. Int. J. Mol. Sci. 2022, 23, 11720. [Google Scholar] [CrossRef]
- Li, M.; Chen, W.-J.; Yang, J.; Charvat, H.; Xie, S.-H.; Li, T.; Ling, W.; Lu, Y.-Q.; Liu, Q.; Hong, M.-H. Association between solid fuel use and seropositivity against Epstein-Barr virus in a high-risk area for nasopharyngeal carcinoma. Environ. Pollut. 2022, 304, 119184. [Google Scholar] [CrossRef]
- Guan, X.; Yu, D.; HuangFu, M.; Huang, Z.; Dou, T.; Liu, Y.; Zhou, L.; Li, X.; Wang, L.; Liu, H. Curcumol inhibits EBV-positive nasopharyngeal carcinoma migration and invasion by targeting nucleolin. Biochem. Pharmacol. 2021, 192, 114742. [Google Scholar] [CrossRef]
- Nickles, E.; Dharmadhikari, B.; Yating, L.; Walsh, R.J.; Koh, L.P.; Poon, M.; Tan, L.K.; Wang, L.-Z.; Ang, Y.; Asokumaran, Y. Dendritic cell therapy with CD137L-DC-EBV-VAX in locally recurrent or metastatic nasopharyngeal carcinoma is safe and confers clinical benefit. Cancer Immunol. Immunother. 2022, 71, 1531–1543. [Google Scholar] [CrossRef]
- Zhu, G.-L.; Fang, X.-L.; Yang, K.-B.; Tang, L.-L.; Ma, J. Development and validation of a joint model for dynamic prediction of overall survival in nasopharyngeal carcinoma based on longitudinal post-treatment plasma cell-free Epstein-Barr virus DNA load. Oral Oncol. 2022, 134, 106140. [Google Scholar] [CrossRef]
- Liu, W.; Chen, G.; Gong, X.; Wang, Y.; Zheng, Y.; Liao, X.; Liao, W.; Song, L.; Xu, J.; Zhang, X. The diagnostic value of EBV-DNA and EBV-related antibodies detection for nasopharyngeal carcinoma: A meta-analysis. Cancer Cell Int. 2021, 21, 164. [Google Scholar] [CrossRef]
- Yuan, L.; Li, S.; Chen, Q.; Xia, T.; Luo, D.; Li, L.; Liu, S.; Guo, S.; Liu, L.; Du, C. EBV infection-induced GPX4 promotes chemoresistance and tumor progression in nasopharyngeal carcinoma. Cell Death Differ. 2022, 29, 1513–1527. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Xu, X.; Wang, Y.; Zeng, M.-S.; Yuan, Y. EBV latent membrane proteins promote hybrid epithelial-mesenchymal and extreme mesenchymal states of nasopharyngeal carcinoma cells for tumorigenicity. PLoS Pathog. 2021, 17, e1009873. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.K.-Y.; Chung, D.L.-S.; Tao, L.; Chan, K.F.; Tung, S.Y.; Ngan, R.K.C.; Ng, W.T.; Lee, A.W.-M.; Yau, C.C.; Kwong, D.L.-W. Epigenomic landscape study reveals molecular subtypes and EBV-associated regulatory epigenome reprogramming in nasopharyngeal carcinoma. EBioMedicine 2022, 86, 104357. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.-J.; Sui, Y.-H.; Liu, T.-T.; Tsang, N.-M.; Huang, C.-H.; Lin, T.-Y.; Chang, K.-P.; Liu, S.-C. Epstein-Barr viral product-containing exosomes promote fibrosis and nasopharyngeal carcinoma progression through activation of YAP1/FAPα signaling in fibroblasts. J. Exp. Clin. Cancer Res. 2022, 41, 254. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.C.; Lee, A.W.; Wong, C.H.; Ng, W.T.; Liu, Z.; Tay, J.K.; Loh, K.S.; Pace-Asciak, P.; Cohen, O.; Corry, J. Epstein-Barr virus directed screening for nasopharyngeal carcinoma in individuals with positive family history: A systematic review. Oral Oncol. 2022, 133, 106031. [Google Scholar] [CrossRef]
- Zhang, T.; Chen, Z.; Deng, J.; Xu, K.; Che, D.; Lin, J.; Jiang, P.; Gu, X.; Xu, B. Epstein–Barr virus-encoded microRNA BART22 serves as novel biomarkers and drives malignant transformation of nasopharyngeal carcinoma. Cell Death Dis. 2022, 13, 664. [Google Scholar] [CrossRef]
- Chang, E.T.; Ye, W.; Zeng, Y.-X.; Adami, H.-O. The evolving epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1035–1047. [Google Scholar] [CrossRef]
- Ai, J.; Tan, G.; Li, W.; Liu, H.; Li, T.; Zhang, G.; Zhou, Z.; Gan, Y. Exosomes loaded with circPARD3 promotes EBV-miR-BART4-induced stemness and cisplatin resistance in nasopharyngeal carcinoma side population cells through the miR-579-3p/SIRT1/SSRP1 axis. Cell Biol. Toxicol. 2022, 38, 1–20. [Google Scholar] [CrossRef]
- Wang, S.; Chen, S.; Zhong, Q.; Liu, Y. Immunotherapy for the treatment of advanced nasopharyngeal carcinoma: A promising new era. J. Cancer Res. Clin. Oncol. 2022, 148, 1–9. [Google Scholar] [CrossRef]
- Yi, Y.-S. Caspase-11 non-canonical inflammasome: Emerging activator and regulator of infection-mediated inflammatory responses. Int. J. Mol. Sci. 2020, 21, 2736. [Google Scholar] [CrossRef]
- Zhao, C.; Zhao, W. NLRP3 inflammasome—A key player in antiviral responses. Front. Immunol. 2020, 11, 211. [Google Scholar] [CrossRef]
- Jiang, L.; Lan, R.; Huang, T.; Chan, C.-F.; Li, H.; Lear, S.; Zong, J.; Wong, W.-Y.; Muk-Lan Lee, M.; Dow Chan, B. EBNA1-targeted probe for the imaging and growth inhibition of tumours associated with the Epstein–Barr virus. Nat. Biomed. Eng. 2017, 1, 0042. [Google Scholar] [CrossRef]
- Kantono, M.; Guo, B. Inflammasomes and cancer: The dynamic role of the inflammasome in tumor development. Front. Immunol. 2017, 8, 1132. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef]
- Moossavi, M.; Parsamanesh, N.; Bahrami, A.; Atkin, S.L.; Sahebkar, A. Role of the NLRP3 inflammasome in cancer. Mol. Cancer 2018, 17, 158. [Google Scholar] [CrossRef]
- Morrison, J.A.; Raab-Traub, N. Roles of the ITAM and PY motifs of Epstein-Barr virus latent membrane protein 2A in the inhibition of epithelial cell differentiation and activation of β-catenin signaling. J. Virol. 2005, 79, 2375–2382. [Google Scholar] [CrossRef]
- Tempera, I.; Klichinsky, M.; Lieberman, P.M. EBV latency types adopt alternative chromatin conformations. PLoS Pathog. 2011, 7, e1002180. [Google Scholar] [CrossRef]
- Bollard, C.M.; Gottschalk, S.; Torrano, V.; Diouf, O.; Ku, S.; Hazrat, Y.; Carrum, G.; Ramos, C.; Fayad, L.; Shpall, E.J. Sustained complete responses in patients with lymphoma receiving autologous cytotoxic T lymphocytes targeting Epstein-Barr virus latent membrane proteins. J. Clin. Oncol. 2014, 32, 798. [Google Scholar] [CrossRef]
- Tao, Y.; Shi, Y.; Jia, J.; Jiang, Y.; Yang, L.; Cao, Y. Novel roles and therapeutic targets of Epstein–Barr virus-encoded latent membrane protein 1-induced oncogenesis in nasopharyngeal carcinoma. Expert Rev. Mol. Med. 2015, 17, E15. [Google Scholar] [CrossRef]
- Kondo, S.; Okabe, A.; Nakagawa, T.; Matsusaka, K.; Fukuyo, M.; Rahmutulla, B.; Dochi, H.; Mizokami, H.; Kitagawa, Y.; Kurokawa, T. Repression of DERL3 via DNA methylation by Epstein-Barr virus latent membrane protein 1 in nasopharyngeal carcinoma. Biochim. Biophys. Acta 2022, 1869, 166598. [Google Scholar] [CrossRef]
- Lee, A.W.; Lee, V.H.; Ng, W.-T.; Strojan, P.; Saba, N.F.; Rinaldo, A.; Willems, S.M.; Rodrigo, J.P.; Forastiere, A.A.; Ferlito, A. A systematic review and recommendations on the use of plasma EBV DNA for nasopharyngeal carcinoma. Eur. J. Cancer 2021, 153, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.-S.; Chen, Y.-Z.; Liu, L.-T.; Liu, R.-P.; Liang, Y.-J.; Wen, D.-X.; Jin, J.; Tang, L.-Q.; Mai, H.-Q.; Chen, Q.-Y. Prognostic significance of AKR1C4 and the advantage of combining EBV DNA to stratify patients at high risk of locoregional recurrence of nasopharyngeal carcinoma. BMC Cancer 2022, 22, 880. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Zhang, X.; Liu, P.; Wei, A.; Ouyang, W.; Xiao, S. Pathogenesis and Diagnostic Significance of EBV-miR-BARTs in Nasopharyngeal Carcinoma. Oxidative Med. Cell. Longev. 2022, 2022, 4479905. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.S. Caspase-11 non-canonical inflammasome: A critical sensor of intracellular lipopolysaccharide in macrophage-mediated inflammatory responses. Immunology 2017, 152, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Thi, H.T.H.; Hong, S. Inflammasome as a therapeutic target for cancer prevention and treatment. J. Cancer Prev. 2017, 22, 62. [Google Scholar] [CrossRef]
- McLaughlin, L.P.; Bollard, C.M.; Keller, M.D. Adoptive T Cell Therapy for Epstein–Barr Virus Complications in Patients with Primary Immunodeficiency Disorders. Front. Immunol. 2018, 9, 556. [Google Scholar] [CrossRef]
- Bouvard, V.; Baan, R.; Straif, K.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Freeman, C.; Galichet, L.; et al. A review of human carcinogens—Part B: Biological agents. Lancel Oncol. 2009, 10, 321–322. [Google Scholar] [CrossRef]
- Bollard, C.M.; Rooney, C.M.; Heslop, H.E. T-cell therapy in the treatment of post-transplant lymphoproliferative disease. Nat. Rev. Clin. Oncol. 2012, 9, 510–519. [Google Scholar] [CrossRef]
- Dagenais, M.; Skeldon, A.; Saleh, M. The inflammasome: In memory of Dr. Jurg Tschopp. Cell Death Differ. 2012, 19, 5–12. [Google Scholar] [CrossRef]
- Xie, J.; Wang, Z.; Fan, W.; Liu, Y.; Liu, F.; Wan, X.; Liu, M.; Wang, X.; Zeng, D.; Wang, Y. Targeting cancer cell plasticity by HDAC inhibition to reverse EBV-induced dedifferentiation in nasopharyngeal carcinoma. Signal Transduct. Target. Ther. 2021, 6, 333. [Google Scholar] [CrossRef]
- Bian, J.; Niu, Y.; Ma, Y.; Chen, F.; Ma, N. A Review on the Application of PD-1 Blockade in EBV-Associated Nasopharyngeal Carcinoma Immunotherapy. Appl. Bionics Biomech. 2022, 2022, 8537966. [Google Scholar] [CrossRef]
- Sinha, S.; Dickey, B.L.; Coghill, A.E. Utility of Epstein-Barr virus (EBV) antibodies as screening markers for nasopharyngeal carcinoma: A narrative review. Ann. Nasopharynx Cancer 2022, 6. [Google Scholar] [CrossRef]
- Taylor, G.S.; Jia, H.; Harrington, K.; Lee, L.W.; Turner, J.; Ladell, K.; Price, D.A.; Tanday, M.; Matthews, J.; Roberts, C. A Recombinant Modified Vaccinia Ankara Vaccine Encoding Epstein–Barr Virus (EBV) Target Antigens: A Phase I Trial in UK Patients with EBV-Positive Cancer Therapeutic Vaccination to Treat EBV Malignancies. Clin. Cancer Res. 2014, 20, 5009–5022. [Google Scholar] [CrossRef]
- Paudel, S.; Warner, B.E.; Wang, R.; Adams-Haduch, J.; Reznik, A.S.; Dou, J.; Huang, Y.; Gao, Y.-T.; Koh, W.-P.; Bäckerholm, A. Serologic Profiling Using an Epstein-Barr Virus Mammalian Expression Library Identifies EBNA1 IgA as a Prediagnostic Marker for Nasopharyngeal Carcinoma. Clin. Cancer Res. 2022, 28, 5221–5230. [Google Scholar] [CrossRef]
- Xu, M.; Zhang, L.; Feng, J.; Yang, S.; Wang, Y.; Wang, Y.; Chen, M.; Zhou, L.; Zhang, J.; Qin, Q. Establishment and characterization of two Epstein-Barr virus (EBV)-positive gastric cancer cell lines with epitheliotropic M81 strain undergoing distinct viral and altered cellular expression profiles. J. Med. Virol. 2022, 95, e28387. [Google Scholar] [CrossRef]
- Miller, J.A.; Sahoo, M.K.; Yamamoto, F.; Huang, C.; Wang, H.; Zehnder, J.L.; Le, Q.-T.; Pinsky, B.A. Multiplex Epstein-Barr virus BALF2 genotyping detects high-risk variants in plasma for population screening of nasopharyngeal carcinoma. Mol. Cancer 2022, 21, 154. [Google Scholar] [CrossRef]
- Zong, J.; Ji, P.; Lin, C.; Zhang, R.; Chen, Y.; Lu, Q.; Peng, X.; Pan, J.; Lin, S. Plasma Epstein-Barr viral DNA load after completion of two cycles of induction chemotherapy predicts outcomes for patients with advanced-stage nasopharyngeal carcinoma. Oral Oncol. 2022, 131, 105972. [Google Scholar] [CrossRef]
- Peng, X.; Zhou, Y.; Tao, Y.; Liu, S. Nasopharyngeal Carcinoma: The Role of the EGFR in Epstein–Barr Virus Infection. Pathogens 2021, 10, 1113. [Google Scholar] [CrossRef]
- Chang, E.; Ye, W.; Ernberg, I.; Zeng, Y.; Adami, H. A novel causal model for nasopharyngeal carcinoma. Cancer Causes Control. 2022, 33, 1013–1018. [Google Scholar] [CrossRef]
- Huang, J.; Harris, E.; Lorch, J. Vaccination as a therapeutic strategy for Nasopharyngeal carcinoma. Oral Oncol. 2022, 135, 106083. [Google Scholar] [CrossRef]
- Karam, I.; Lee, N.Y.; Le, Q.-T.; O’Sullivan, B.; Lu, J.J.; Poon, I. Nasopharyngeal carcinoma. In Target Volume Delineation and Field Setup; Lee, N.Y., Lu, J.J., Yu, Y., Eds.; Springer: Cham, Switzerland, 2022; pp. 1–13. [Google Scholar]
- Wong, K.C.; Hui, E.P.; Lo, K.-W.; Lam, W.K.J.; Johnson, D.; Li, L.; Tao, Q.; Chan, K.C.A.; To, K.-F.; King, A.D. Nasopharyngeal carcinoma: An evolving paradigm. Nat. Rev. Clin. Oncol. 2021, 18, 679–695. [Google Scholar] [CrossRef] [PubMed]
- Xiao, R.-W.; Wang, F.; Wang, T.-M.; Zhang, J.-B.; Wu, Z.-Y.; Deng, C.-M.; Liao, Y.; Zhou, T.; Yang, D.-W.; Dong, S.-Q. Rare POLN mutations confer risk for familial nasopharyngeal carcinoma through weakened Epstein-Barr virus lytic replication. EBioMedicine 2022, 84, 104267. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, N.; Abusalah, M.A.H.A.; Farzand, A.; Absar, M.; Yusof, N.Y.; Rabaan, A.A.; AlSaihati, H.; Alshengeti, A.; Alwarthan, S.; Alsuwailem, H.S.; et al. Updates on Epstein–Barr Virus (EBV)-Associated Nasopharyngeal Carcinoma: Emphasis on the Latent Gene Products of EBV. Medicina 2023, 59, 2. https://doi.org/10.3390/medicina59010002
Ahmed N, Abusalah MAHA, Farzand A, Absar M, Yusof NY, Rabaan AA, AlSaihati H, Alshengeti A, Alwarthan S, Alsuwailem HS, et al. Updates on Epstein–Barr Virus (EBV)-Associated Nasopharyngeal Carcinoma: Emphasis on the Latent Gene Products of EBV. Medicina. 2023; 59(1):2. https://doi.org/10.3390/medicina59010002
Chicago/Turabian StyleAhmed, Naveed, Mai Abdel Haleem A. Abusalah, Anam Farzand, Muhammad Absar, Nik Yusnoraini Yusof, Ali A. Rabaan, Hajir AlSaihati, Amer Alshengeti, Sara Alwarthan, Haifa S. Alsuwailem, and et al. 2023. "Updates on Epstein–Barr Virus (EBV)-Associated Nasopharyngeal Carcinoma: Emphasis on the Latent Gene Products of EBV" Medicina 59, no. 1: 2. https://doi.org/10.3390/medicina59010002
APA StyleAhmed, N., Abusalah, M. A. H. A., Farzand, A., Absar, M., Yusof, N. Y., Rabaan, A. A., AlSaihati, H., Alshengeti, A., Alwarthan, S., Alsuwailem, H. S., Alrumaih, Z. A., Alsayyah, A., & Yean, C. Y. (2023). Updates on Epstein–Barr Virus (EBV)-Associated Nasopharyngeal Carcinoma: Emphasis on the Latent Gene Products of EBV. Medicina, 59(1), 2. https://doi.org/10.3390/medicina59010002







