Cocaine Abuse as an Immunological Trigger in a Case Diagnosed with Eales Disease
Abstract
1. Introduction
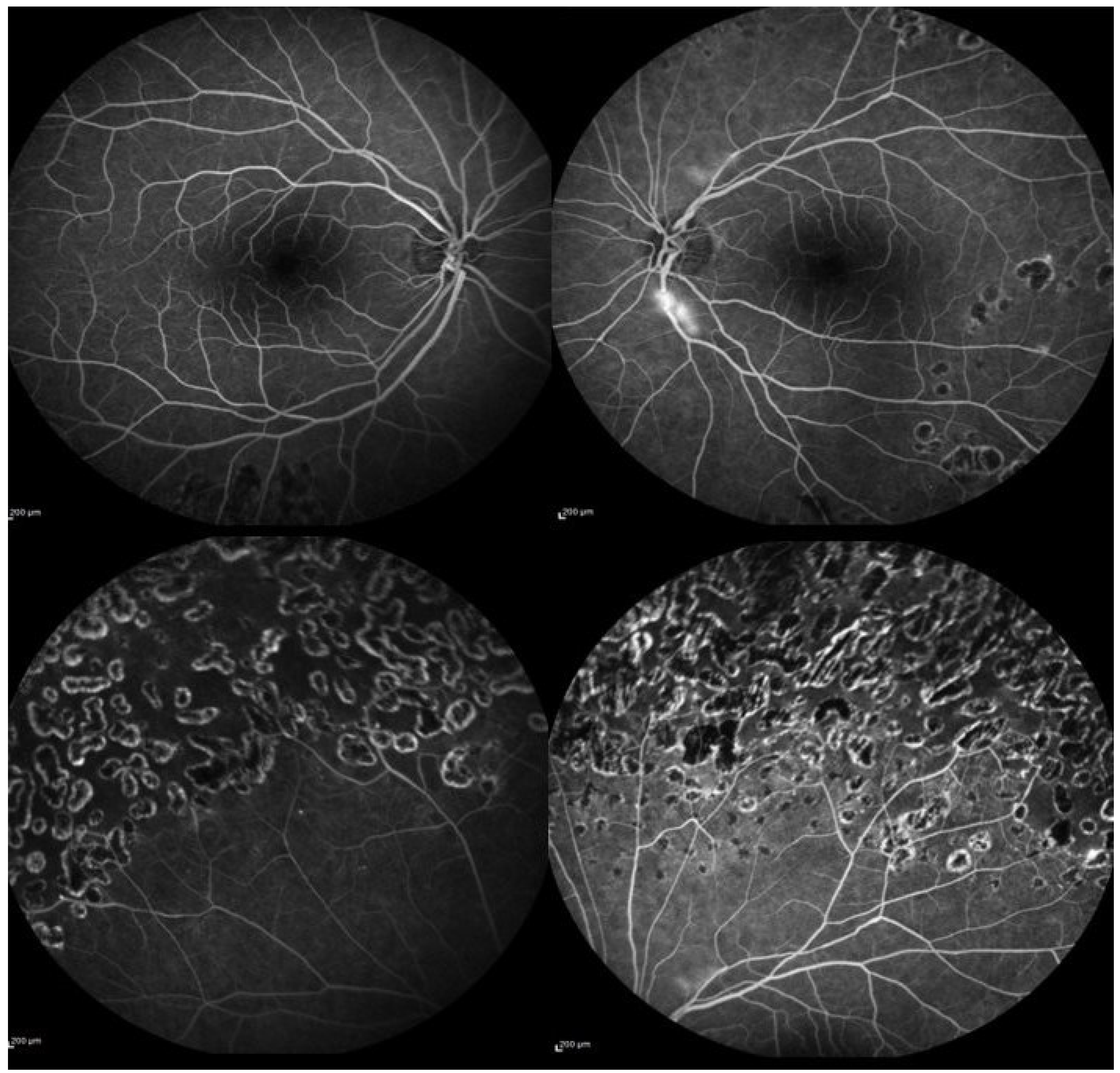
2. Case Presentation
3. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LE | left eye |
| RE | right eye |
| BE | both eyes |
| FFA | fundus fluorescein angiography |
References
- Raizada, K.; Tripathy, K. Eales Disease. In StatPearls. Edn. Treasure Island (FL): StatPearls Publishing Copyright © 2022; StatPearls Publishing LLC: Tampa, FL, USA, 2022. [Google Scholar]
- Biswas, J.; Sharma, T.; Gopal, L.; Madhavan, H.N.; Sulochana, K.N.; Ramakrishnan, S. Eales disease—An update. Surv. Ophthalmol. 2002, 47, 197–214. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Biswas, J. Further evidence of the association of latent Mycobacterium tuberculosis in Eales’ disease. Int. Ophthalmol. 2021, 41, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Kolar, P. Risk factors for central and branch retinal vein occlusion: A meta-analysis of published clinical data. J. Ophthalmol. 2014, 2014, 724780. [Google Scholar] [CrossRef] [PubMed]
- Eller, A.W.; Bontempo, F.A.; Faruki, H.; Hassett, A.C. Peripheral retinal neovascularization (Eales disease) associated with the factor V Leiden mutation. Am. J. Ophthalmol. 1998, 126, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Havakuk, O.; Rezkalla, S.H.; Kloner, R.A. The Cardiovascular Effects of Cocaine. J. Am. Coll Cardiol. 2017, 70, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Carroll, W.J.; Maganti, N.; Gill, M.K. Hypoperfusion of the deep capillary plexus associated with acute on chronic cocaine use. Am. J. Ophthalmol. Case Rep. 2020, 18, 100684. [Google Scholar] [CrossRef] [PubMed]
- Fortenbach, C.R.; Modjtahedi, B.S. Bilateral Enlargement of the Foveal Avascular Zone on Optical Coherence Tomography Angiography Associated With Cocaine Use. JAMA Ophthalmol. 2020, 138, 708–710. [Google Scholar] [CrossRef] [PubMed]
- Rahman, W.; Thomas, S.; Wiselka, M.; Bibby, K. Cocaine-induced chorioretinal infarction. Br. J. Ophthalmol. 2008, 92, 150–151. [Google Scholar] [CrossRef] [PubMed]
- Roohipourmoallai, R.; Davoudi, S.; Hosseinian Benvidi, S.M.; Iyer, S.S.R. Peripheral Retinal Neovascularization in a Patient with Sarcoidosis and Cocaine-Associated Autoimmunity. Case Rep. Ophthalmol. Med. 2021, 2021, 9923260. [Google Scholar] [CrossRef] [PubMed]
- Pontieri, F.E.; Tanda, G.; Orzi, F.; Di Chiara, G. Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature 1996, 382, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Biswas, J.K.R.R.; Pal, B.; Gondhale, H.P.; Kharel Sitaula, R. Long-Term Outcomes of a Large Cohort of Patients with Eales’ Disease. Ocul. Immunol. Inflamm. 2018, 26, 870–876. [Google Scholar] [CrossRef] [PubMed]
- El-Asrar, A.M.; Al-Kharashi, S.A. Full panretinal photocoagulation and early vitrectomy improve prognosis of retinal vasculitis associated with tuberculoprotein hypersensitivity (Eales’ disease). Br. J. Ophthalmol. 2002, 86, 1248–1251. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iannetti, L.; Scarinci, F.; Alisi, L.; Beccia, A.; Cacciamani, A.; Saturno, M.C.; Gharbiya, M. Cocaine Abuse as an Immunological Trigger in a Case Diagnosed with Eales Disease. Medicina 2023, 59, 169. https://doi.org/10.3390/medicina59010169
Iannetti L, Scarinci F, Alisi L, Beccia A, Cacciamani A, Saturno MC, Gharbiya M. Cocaine Abuse as an Immunological Trigger in a Case Diagnosed with Eales Disease. Medicina. 2023; 59(1):169. https://doi.org/10.3390/medicina59010169
Chicago/Turabian StyleIannetti, Ludovico, Fabio Scarinci, Ludovico Alisi, Alessandro Beccia, Andrea Cacciamani, Maria Carmela Saturno, and Magda Gharbiya. 2023. "Cocaine Abuse as an Immunological Trigger in a Case Diagnosed with Eales Disease" Medicina 59, no. 1: 169. https://doi.org/10.3390/medicina59010169
APA StyleIannetti, L., Scarinci, F., Alisi, L., Beccia, A., Cacciamani, A., Saturno, M. C., & Gharbiya, M. (2023). Cocaine Abuse as an Immunological Trigger in a Case Diagnosed with Eales Disease. Medicina, 59(1), 169. https://doi.org/10.3390/medicina59010169







