Abstract
Osteoporosis is mainly a geriatric disease with a high incidence, and the resulting spinal fractures and hip fractures cause great harm to patients. Anti-osteoporosis drugs are the main treatment for osteoporosis currently, but these drugs have potential clinical limitations and side effects, so the development of new therapies is of great significance to patients with osteoporosis. Electrical stimulation therapy mainly includes pulsed electromagnetic fields (PEMF), direct current (DC), and capacitive coupling (CC). Meanwhile, electrical stimulation therapy is clinically convenient without side effects. In recent years, many researchers have explored the use of electrical stimulation therapy for osteoporosis. Based on this, the role of electrical stimulation therapy in osteoporosis was summarized. In the future, electrical stimulation might become a new treatment for osteoporosis.
1. Introduction
Osteoporosis, a systemic bone disease, can cause fractures due to a decrease in bone density and bone quality for various reasons, the destruction of bone microstructure, and an increase in bone fragility [1,2,3]. The diagnosis of osteoporosis mainly relies on dual energy X-ray absorptiometry, and the main measurement sites are the lumbar spine, proximal femur, and distal radius. Generally speaking, the measurement value is less than −2.5 [4,5], and the incidence of osteoporosis is very high. In a community survey of 5585 people with an average age of 77 years old in the UK, it was found that the incidence of osteoporosis was more than 50% [6]. In osteoporosis patients, spine fractures and hip fractures are common; they affect the quality of life of patients, threaten the health of elderly patients, and can cause fatal complications [7,8,9]. Osteoporosis treatments include bisphosphonates, selective estrogen receptor modulators, estrogens, and parathyroid hormones. However, some of these drugs are clinically inconvenient to use, and most of them have side effects, so it is clinically meaningful to develop new osteoporosis treatments [10,11,12,13,14].
Electrical stimulation therapy mainly includes pulsed electromagnetic fields (PEMFs), direct current (DC), and capacitive coupling (CC) [15,16,17] (Figure 1). The main working principle of a PEMF is to convert electric current into electromagnetic wave signal, and a PEMF has curative effect on nonunion and delayed fracture healing [18,19,20]. DC is an invasive technique that delivers constant direct current through an implanted electrical stimulator [21,22,23]. CC is a non-invasive technology that applies an electric field, and two skin electrodes are aimed at the treatment site. Therefore, electrical energy is induced from one electrode to the other electrode through frequency changes to stimulate the treatment site and achieve the purpose of treatment [24,25,26]. Studies have reported that a PEMF, DC, and CC have therapeutic effects on osteoporosis. Based on this, the relevant literature was reviewed to provide information for new treatment options for osteoporosis.
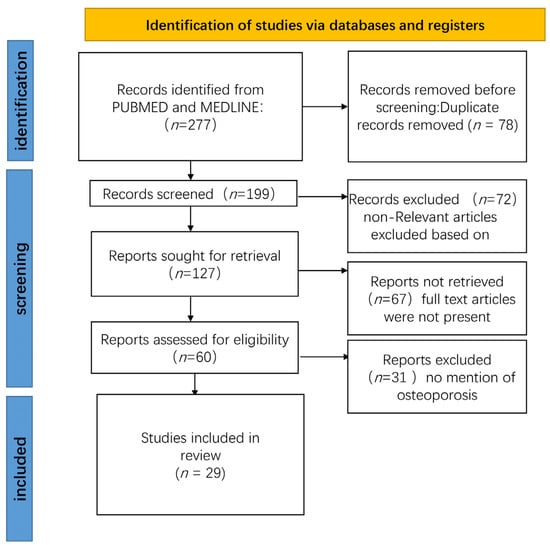
Figure 1.
PRISMA flowchart showing the process of study selection.
2. Methods
We used “electrical stimulation”, “osteoporosis”, “pulsed electromagnetic fields”, and “osteoporosis” as keywords and searched all the articles from 1968 to 2022 in PUBMED and MEDLINE articles. We included only publications published in English and selected those findings that were, in our opinion, the most important. We further analyzed these articles, mainly selected papers from the past 5 years, but also included well-respected older publications (Figure 1).
3. PEMFs for Osteoporosis
The main mechanism of a PEMF is to convert electric current into a magnetic field that can activate the biological current of the organism to achieve the purpose of treatment. A PEMF has good effects on nonunion and delayed fracture healing, and there are also many reports that a PEMF can treat osteoporosis [27,28,29]. The clinical research into PEMFs in osteoporosis, the effects of a PEMF on osteogenesis and its mechanism, and the effects of a PEMF on osteoclasts and its mechanism will be discussed.
3.1. The Clinical Research into PEMFs in Osteoporosis
The improvement of osteoporotic bone pain and osteoporosis using PEMFs have been reported on many times (Table 1).
At present, there is clinical evidence that PEMFs could relieve osteoporotic bone pain [30]. Many clinical trials have proved that PEMFs can promote the recovery of osteoporotic bone mass. Antonino Catalano et al. conducted a randomized controlled clinical trial of 43 people and revealed that a PEMF may play a role in restoring osteoporosis and bone mass through RANKL/OPG and Wnt/β-catenin pathways [31]. Of course, other clinical studies have come to similar conclusions [32,33]. Although the FDA (Food and Drug Administration) has not yet approved PEMFs for the treatment of osteoporosis, the above clinical trials have indicated that PEMFs are a non-invasive, safe, and effective treatment for osteoporosis. We look forward to more large-scale clinical trials using PEMFs for osteoporosis in the future. Through further trials, PEMFs would be approved by the FDA for osteoporosis treatment in the future, which will benefit patients; however, this technology is not mature enough for clinical use and needs more research

Table 1.
The clinical research of PEMFs in osteoporosis.
Table 1.
The clinical research of PEMFs in osteoporosis.
| Researchers | Contents | Patients | References |
|---|---|---|---|
| Antonino Catalano et al. | restoring osteoporosis and bone mass | 43 | [31] |
| Hui-Fang Liu et al. | as effective as alendronate | 44 | [32] |
| F Tabrah et al. | prevention and treatment of osteoporosis | 20 | [33] |
3.2. The Effects of a PEMF on Osteogenesis and Its Mechanism
A PEMF inhibits osteoporosis progression mainly through primary cilia, H-type angiogenesis, and WNT signaling pathways (Table 2).
Cilia are hair-like organelles protruding from the cell surface and are composed of microtubules to form axons. Furthermore, cilia play an important role in the basic life activities of cells. Immobile cilia are also commonly referred to as primary cilia; they sense changes in the microenvironment surrounding the cell and mediate a variety of important signal transductions within the cell [34,35,36]. Wen-Fang He et al. revealed that PEMFs promote osteogenic differentiation through nitric oxide signaling within primary cilia, thus inhibiting osteoporosis progression [37]. According to Yan-Fang Xie et al., PEMFs stimulated osteoblast differentiation and mineralization in a primary cilia-dependent manner and inhibited osteoporosis progression [38]. Juan-Li Yan et al. illustrated that PEMFs promote osteoblast mineralization and maturation through primary cilia as a potential treatment for osteoporosis [39]. Therefore, it can be said that primary cilia play an important role in the mechanism of PEMF treatment of osteoporosis.
There are special capillaries in the bone—H-type blood vessels—that are CD31 protein-positive vessels, and H-type angiogenesis is also considered as a key factor in osteoporosis [40,41,42,43]. Qian Wang et al. found that PEMFs promote osteogenesis by promoting the formation of H-type blood vessels which inhibits the occurrence of osteoporosis [44]. Tiantian Wang et al. also found that, as a potential treatment for glucocorticoid-induced osteoporosis, PEMFs maintain H-type angiogenesis and osteogenesis [45].
The WNT pathway is an evolutionarily conserved signaling pathway that is involved in various biological activities. It can be divided into a canonical Wnt/β-catenin signaling pathway, planar cell polarity pathway, Wnt/Ca+ pathway, and spindle regulation pathway [46,47,48,49,50]. The WNT signaling pathway plays an important role in promoting osteogenesis and inhibiting osteoporosis as well [51,52,53]. Based on evidence from Xi Shao et al., PEMFs treat osteoporosis in type 2 diabetic mice by activating Wnt/β-catenin signaling [54]. Shaoyu Wu et al. found that PEMFs promote the osteogenic differentiation of mesenchymal stem cells through the Wnt/Ca+ pathway and inhibit the progression of osteoporosis [55]. Xi Shao et al. discovered that PEMFs enhance canonical Wnt signaling-mediated bone formation in spinal cord injured rats [56]. In addition, other researchers have also revealed that PEMFs inhibit the progression of osteoporosis through the WNT signaling pathway [57,58].

Table 2.
The effects of a PEMF on osteogenesis and its mechanism.
Table 2.
The effects of a PEMF on osteogenesis and its mechanism.
| Researchers | Outcome | Mechanism | References |
|---|---|---|---|
| Wen-Fang He et al. | osteogenic differentiation | primary cilia | [37] |
| Yan-Fang Xie et al. | osteoblast mineralization | primary cilia-dependent | [38] |
| Juan-Li Yan et al. | osteoblast maturation | primary cilia | [39] |
| Qian Wang et al. | osteogenesis | H-type blood vessels | [44] |
| Tiantian Wang et al. | osteogenesis | H-type angiogenesis | [45] |
| Xi Shao et al. | osteogenesis | Wnt/β-catenin | [54] |
| Shaoyu Wu et al. | osteogenic differentiation | Wnt/Ca+ | [55] |
| Xi Shao et al. | bone formation | Wnt/β-catenin | [56] |
| Da Jing et al. | bone formation | Wnt/β-catenin | [57] |
| Jun Zhou et al. | osteogenesis | Wnt/β-catenin | [58] |
3.3. The Effects of a PEMF on Osteoclasts and Its Mechanism
PEMFs can also inhibit the progression of osteoporosis by affecting osteoclasts (Table 3). Pan Wang et al. found that PEMFs inhibit osteoclast formation by regulating the ratio of RANKL/OPG through primary cilia, thus inhibiting the progression of osteoporosis [59]. Ying Pi et al. found that a low-frequency PEMF inhibits osteoclast differentiation by scavenging reactive oxygen species, and it is a potential treatment for osteoporosis [60]. Yutian Lei et al. found that PEMFs inhibit osteoclast differentiation and inhibit the progression of osteoporosis by regulating the Akt/mTOR signaling pathway [61]. Moreover, many other researchers have found that PEMFs inhibit the progression of osteoporosis by inhibiting osteoclast formation and differentiation [62,63,64,65,66].

Table 3.
PEMFs inhibit the progression of osteoporosis by affecting osteoclasts.
4. DC for Osteoporosis
DC is an invasive technique that provides a constant direct current by implanting an electrical stimulator and implanting the cathode and anode into the repair site for continuous electrical stimulation to treat diseases. In addition, DC also has a therapeutic effect on fracture nonunion [67,68]. At present, many animal experiments have confirmed that DC has a therapeutic effect on osteoporosis (Table 4). Kaori Iimura et al. discovered that chronic stimulation of the superior roaring nerve in rats with implanted electrodes stimulated the thyroid to release calcitonin and partially ameliorated bone loss in OVX (ovariectomy) rats [69]. Roy Yuen-Chi Lau et al. illustrated that electrical stimulation of the dorsal root ganglion of rats using an implantable micro-electrical stimulation system can stimulate the secretion of calcitonin gene-related peptides and inhibit osteoporosis as well [70]. Y-C Lau et al. also demonstrated that DC can be used to stimulate dorsal root nerve energy-saving treatment for osteoporosis in rats [71]. However, at present, DC has a more important problem, which is the potential infectivity of implanted electrical stimulation devices for patients, and researchers should take this factor into consideration in future studies.

Table 4.
Animal experiments using DC for osteoporosis.
5. CC for Osteoporosis
CC is a non-invasive technology that applies an electric field; two skin electrodes are aimed at the treatment site so that the electric energy is induced from one electrode to the other electrode through frequency changes, thereby stimulating the treatment site and achieving the purpose of treatment. Furthermore, the current therapeutic role of CC in fractures and bone pain has also been reported [72,73]. The therapeutic effects of CC in osteoporosis are also limited to animal experiments (Table 5). Jayanand Manjhi et al. found that low-level capacitively coupled pulsed electric field stimulation has a therapeutic effect on osteoporosis in rats [74]. Jayanand Behari et al. revealed that capacitively coupled stimulation of rat legs can inhibit the progression of osteoporosis [75]. C T Brighton et al. proved that the stimulation of vertebrae at the paraspinal level using capacitively coupled electrodes on the dorsal skin surface of the 11th thoracic and 4th lumbar vertebrae treats osteoporosis [76]. Other researchers have also obtained similar conclusions [77,78]. In general, CC is a promising treatment modality, with good efficacy in animal models, and more clinical trials are needed to confirm this.

Table 5.
Animal experiments using CC for osteoporosis.
6. Conclusions
Electrical stimulation might be a good, non-invasive, and effective treatment for osteoporosis. A PEMF is the treatment method with the most research and many clinical trials. Many clinical trials have also shown its efficacy, but the specific treatment parameters of frequency and treatment time are not yet conclusive. Meanwhile, the FDA has not approved the treatment for osteoporosis, and even though PEMFs have huge potential, PEMFs need more large-scale clinical trials in the future to investigate the optimal frequency and duration of treatment for osteoporosis. DC is an invasive therapy. At present, only animal experiments have proved its efficacy, and researchers need to solve the potential infection problems of DC before going to clinical trials. CC is also a promising treatment for osteoporosis, and multiple animal experiments have confirmed its efficacy; however, it still needs clinical trials to confirm its effects on osteoporosis patients.
Our study has limitations. The first is the small number of cases included in the study, and the conclusions drawn may have limitations. The second is that the exact magnitude and frequency of the effects of PEMFs, CC, and DC were not determined, which might pose difficulties for future applications in the clinic.
Author Contributions
Q.K. designed the manuscript; C.G., X.S., J.S. and L.L. checked the related literature; W.Z., Y.L. and J.X. wrote the manuscript and participated in the revision. All authors reviewed the final version and agreed to submit. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Sichuan Science and Technology Program, China (2020YFS0080, 2020YFQ0007, 2021JDRC0159); the Science and Technology Project of the Tibet Autonomous Re-gion (XZ201901-GB-08); the 1·3·5 Project for Disciplines of Excellence, West China Hospital, Si-chuan University (ZYJC21026, ZYJC21077); the Natural Science Fund of the Tibet Autonomous Region (XZ202101ZR0112G); Science and Technology Major Project of Tibet Autonomous Region of China (XZ202201ZD0001G); and the Project of the Hospital of Chengdu Office of the People’s Government of the Tibet Autonomous Region (2020-YJYB-1).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no competing interests.
References
- Brown, C. Osteoporosis: Staying strong. Nature 2017, 550, S15–S17. [Google Scholar] [CrossRef]
- Leslie, W.D.; Crandall, C.J. Serial Bone Density Measurement for Osteoporosis Screening. JAMA 2021, 326, 1622–1623. [Google Scholar] [CrossRef] [PubMed]
- Compston, J.E.; McClung, M.R.; Leslie, W.D. Osteoporosis. Lancet 2019, 393, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Al Jumaily, K.; Lin, M.; Siminoski, K.; Ye, C. Dual-energy X-ray absorptiometry scanner mismatch in follow-up bone mineral density testing. Osteoporos. Int. 2022, 33, 1981–1988. [Google Scholar] [CrossRef] [PubMed]
- Gatti, S.; Quattrini, S.; Palpacelli, A.; Catassi, G.N.; Lionetti, M.E.; Catassi, C. Metabolic Bone Disease in Children with Intestinal Failure and Long-Term Parenteral Nutrition: A Systematic Review. Nutrients 2022, 14, 995. [Google Scholar] [CrossRef] [PubMed]
- Lyu, H.; Zhao, S.; Li, J.; Li, X.; Wang, Y.; Xie, D.; Zeng, C.; Lei, G.; Wei, J.; Li, H. Denosumab and Risk of Community-acquired Pneumonia: A Population-based Cohort Study. J. Clin. Endocrinol. Metab. 2022, 107, e3366–e3373. [Google Scholar] [CrossRef]
- Lippuner, K.; Rimmer, G.; Stuck, A.K.; Schwab, P.; Bock, O. Hospitalizations for major osteoporotic fractures in Switzerland: A long-term trend analysis between 1998 and 2018. Osteoporos. Int. 2022, 33, 2327–2335. [Google Scholar] [CrossRef]
- Kadri, A.; Binkley, N.; Daffner, S.D.; Anderson, P.A. Clinical risk factor status in patients with vertebral fracture but normal bone mineral density. Spine J. Off. J. N. Am. Spine Soc. 2022, 22, 1634–1641. [Google Scholar] [CrossRef]
- Leguy, D.; Magro, L.; Pierache, A.; Coiteux, V.; Agha, I.Y.; Cortet, B.; Legroux-Gerot, I. Changes in bone mineral density after allogenic stem cell transplantation. Jt. Bone Spine 2022, 89, 105373. [Google Scholar] [CrossRef]
- Reid, I.R.; Billington, E.O. Drug therapy for osteoporosis in older adults. Lancet 2022, 399, 1080–1092. [Google Scholar] [CrossRef]
- Nakatoh, S.; Fujimori, K.; Ishii, S.; Tamaki, J.; Okimoto, N.; Ogawa, S.; Iki, M. Association of pharmacotherapy with the second hip fracture incidence in women: A retrospective analysis of the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Geriatr. Gerontol. Int. 2022, 22, 930–937. [Google Scholar] [CrossRef]
- Dimai, H.P.; Fahrleitner-Pammer, A. Osteoporosis and Fragility Fractures: Currently available pharmacological options and future directions. Best Pract. Res. Clin. Rheumatol. 2022, 36, 101780. [Google Scholar] [CrossRef]
- Iida, H.; Sakai, Y.; Seki, T.; Watanabe, T.; Wakao, N.; Matsui, H.; Imagama, S. Bisphosphonate treatment is associated with decreased mortality rates in patients after osteoporotic vertebral fracture. Osteoporos. Int. 2022, 33, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Palacios, S. Medical treatment of osteoporosis. Climacteric J. Int. Menopause Soc. 2022, 25, 43–49. [Google Scholar] [CrossRef]
- Akhter, S.; Qureshi, A.R.; Aleem, I.; El-Khechen, H.A.; Khan, S.; Sikder, O.; Khan, M.; Bhandari, M.; Aleem, I. Efficacy of Electrical Stimulation for Spinal Fusion: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sci. Rep. 2020, 10, 4568. [Google Scholar] [CrossRef]
- Al-Jabri, T.; Tan, J.Y.Q.; Tong, G.Y.; Shenoy, R.; Kayani, B.; Parratt, T.; Khan, T. The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: A systematic review. BMC Musculoskelet. Disord. 2017, 18, 319. [Google Scholar] [CrossRef]
- Gan, J.C.; Glazer, P.A. Electrical stimulation therapies for spinal fusions: Current concepts. Eur. Spine J. 2006, 15, 1301–1311. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.J.K.; Tai, Y.K.; Yap, J.L.Y.; Fong, C.H.H.; Loo, L.S.W.; Kukumberg, M.; Fröhlich, J.; Zhang, S.; Li, J.Z.; Wang, J.-W.; et al. Brief exposure to directionally-specific pulsed electromagnetic fields stimulates extracellular vesicle release and is antagonized by streptomycin: A potential regenerative medicine and food industry paradigm. Biomaterials 2022, 287, 121658. [Google Scholar] [CrossRef]
- Ganse, B.; Orth, M.; Roland, M.; Diebels, S.; Motzki, P.; Seelecke, S.; Kirsch, S.-M.; Welsch, F.; Andres, A.; Wickert, K.; et al. Concepts and clinical aspects of active implants for the treatment of bone fractures. Acta Biomater. 2022, 146, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Yang, L.; Jiang, J.; Liu, Y.; Fan, Z.; Zhong, C.; He, C. Pulsed electromagnetic fields: Promising treatment for osteoporosis. Osteoporos. Int. 2019, 30, 267–276. [Google Scholar] [CrossRef]
- Abellaneda-Pérez, K.; Vaqué-Alcázar, L.; Perellón-Alfonso, R.; Solé-Padullés, C.; Bargalló, N.; Salvador, R.; Ruffini, G.; Nitsche, M.A.; Pascual-Leone, A.; Bartrés-Faz, D. Multifocal Transcranial Direct Current Stimulation Modulates Resting-State Functional Connectivity in Older Adults Depending on the Induced Current Density. Front. Aging Neurosci. 2021, 13, 725013. [Google Scholar] [CrossRef]
- Li, M.; Zhang, D.; Chen, Y.; Chai, X.; He, L.; Chen, Y.; Guo, J.; Sui, X. Discrimination and Recognition of Phantom Finger Sensation Through Transcutaneous Electrical Nerve Stimulation. Front. Neurosci. 2018, 12, 283. [Google Scholar] [CrossRef]
- Fornell, S.; Ribera, J.; Mella, M.; Carranza, A.; Serrano-Toledano, D.; Domecq, G. Effects of electrical stimulation in the treatment of osteonecrosis of the femoral head. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2018, 28, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Goyal, K.; Borkholder, D.A.; Day, S.W. Dependence of Skin-Electrode Contact Impedance on Material and Skin Hydration. Sensors 2022, 22, 8510. [Google Scholar] [CrossRef]
- Ng, C.L.; Reaz, M.B.I.; Crespo, M.L.; Cicuttin, A.; Chowdhury, M.E.H. Characterization of capacitive electromyography biomedical sensor insulated with porous medical bandages. Sci. Rep. 2020, 10, 14891. [Google Scholar] [CrossRef]
- Zheng, Y.-N.; Yu, Z.; Mao, G.; Li, Y.; Pravarthana, D.; Asghar, W.; Liu, Y.; Qu, S.; Shang, J.; Li, R.-W. A Wearable Capacitive Sensor Based on Ring/Disk-Shaped Electrode and Porous Dielectric for Noncontact Healthcare Monitoring. Glob. Chall. 2020, 4, 1900079. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Menger, M.M.; Braun, B.J.; Schweizer, S.; Linnemann, C.; Falldorf, K.; Ronniger, M.; Wang, H.; Histing, T.; Nussler, A.K.; et al. Modulation of Macrophage Activity by Pulsed Electromagnetic Fields in the Context of Fracture Healing. Bioengineering 2021, 8, 167. [Google Scholar] [CrossRef]
- Androjna, C.; Fort, B.; Zborowski, M.; Midura, R.J. Pulsed electromagnetic field treatment enhances healing callus biomechanical properties in an animal model of osteoporotic fracture. Bioelectromagnetics 2014, 35, 396–405. [Google Scholar] [CrossRef]
- Tong, J.; Chen, Z.; Sun, G.; Zhou, J.; Zeng, Y.; Zhong, P.; Deng, C.; Chen, X.; Liu, L.; Wang, S.; et al. The Efficacy of Pulsed Electromagnetic Fields on Pain, Stiffness, and Physical Function in Osteoarthritis: A Systematic Review and Meta-Analysis. Pain Res. Manag. 2022, 2022, 9939891. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.-Q.; He, H.-C.; He, C.-Q.; Chen, J.; Yang, L. Clinical update of pulsed electromagnetic fields on osteoporosis. Chin. Med. J. 2008, 121, 2095–2099. [Google Scholar] [CrossRef]
- Catalano, A.; Loddo, S.; Bellone, F.; Pecora, C.; Lasco, A.; Morabito, N. Pulsed electromagnetic fields modulate bone metabolism via RANKL/OPG and Wnt/β-catenin pathways in women with postmenopausal osteoporosis: A pilot study. Bone 2018, 116, 42–46. [Google Scholar] [CrossRef]
- Liu, H.-F.; Yang, L.; He, H.-C.; Zhou, J.; Liu, Y.; Wang, C.-Y.; Wu, Y.-C.; He, C.-Q. Pulsed electromagnetic fields on postmenopausal osteoporosis in southwest China: A randomized, active-controlled clinical trial. Bioelectromagnetics 2013, 34, 323–332. [Google Scholar] [CrossRef]
- Tabrah, F.; Hoffmeier, M.; Gilbert, F., Jr.; Batkin, S.; Bassett, C.A. Bone density changes in osteoporosis-prone women exposed to pulsed electromagnetic fields (PEMFs). J. Bone Miner. Res. 1990, 5, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Amack, J.D. Structures and functions of cilia during vertebrate embryo development. Mol. Reprod. Dev. 2022, 89, 579–596. [Google Scholar] [CrossRef] [PubMed]
- Klena, N.; Pigino, G. Structural Biology of Cilia and Intraflagellar Transport. Annu. Rev. Cell Dev. Biol. 2022, 38, 103–123. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Wu, S.; Ling, H.; Zhang, C.; Kong, Y. Primary Cilia: A Cellular Regulator of Articular Cartilage Degeneration. Stem Cells Int. 2022, 2022, 2560441. [Google Scholar] [CrossRef]
- He, W.; Qin, R.; Gao, Y.; Zhou, J.; Wei, J.; Liu, J.; Hou, X.; Ma, H.; Xian, C.J.; Li, X.; et al. The interdependent relationship between the nitric oxide signaling pathway and primary cilia in pulse electromagnetic field-stimulated osteoblastic differentiation. FASEB J. 2022, 36, e22376. [Google Scholar] [CrossRef]
- Xie, Y.-F.; Shi, W.-G.; Zhou, J.; Gao, Y.-H.; Li, S.-F.; Fang, Q.-Q.; Wang, M.-G.; Ma, H.-P.; Wang, J.-F.; Xian, C.J.; et al. Pulsed electromagnetic fields stimulate osteogenic differentiation and maturation of osteoblasts by upregulating the expression of BMPRII localized at the base of primary cilium. Bone 2016, 93, 22–32. [Google Scholar] [CrossRef]
- Yan, J.-L.; Zhou, J.; Ma, H.-P.; Ma, X.-N.; Gao, Y.-H.; Shi, W.-G.; Fang, Q.-Q.; Ren, Q.; Xian, C.J.; Chen, K.-M. Pulsed electromagnetic fields promote osteoblast mineralization and maturation needing the existence of primary cilia. Mol. Cell. Endocrinol. 2015, 404, 132–140. [Google Scholar] [CrossRef]
- Liu, S.; Chen, T.; Wang, R.; Huang, H.; Fu, S.; Zhao, Y.; Wang, S.; Wan, L. Exploring the effect of the “quaternary regulation” theory of “peripheral nerve-angiogenesis-osteoclast-osteogenesis” on osteoporosis based on neuropeptides. Front. Endocrinol. 2022, 13, 908043. [Google Scholar] [CrossRef]
- Lin, X.; Xu, F.; Zhang, K.-W.; Qiu, W.-X.; Zhang, H.; Hao, Q.; Li, M.; Deng, X.-N.; Tian, Y.; Chen, Z.-H.; et al. Acacetin Prevents Bone Loss by Disrupting Osteoclast Formation and Promoting Type H Vessel Formation in Ovariectomy-Induced Osteoporosis. Front. Cell Dev. Biol. 2022, 10, 796227. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liao, L.; Hu, Y.; Xu, Y.; Zhang, Y.; Huo, F.; Tian, W.; Guo, W. Identification of Type H Vessels in Mice Mandibular Condyle. J. Dent. Res. 2021, 100, 983–992. [Google Scholar] [CrossRef] [PubMed]
- Jing, H.; Liao, L.; Su, X.; Shuai, Y.; Zhang, X.; Deng, Z.; Jin, Y. Declining histone acetyltransferase GCN5 represses BMSC-mediated angiogenesis during osteoporosis. FASEB J. 2017, 31, 4422–4433. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhou, J.; Wang, X.; Xu, Y.; Liang, Z.; Gu, X.; He, C. Coupling induction of osteogenesis and type H vessels by pulsed electromagnetic fields in ovariectomy-induced osteoporosis in mice. Bone 2022, 154, 116211. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Yang, L.; Liang, Z.; Bai, L.; Pei, H.; Zhang, T.; Wu, L.; Wang, L.; Wang, X.; You, X.; et al. Pulsed electromagnetic fields attenuate glucocorticoid-induced bone loss by targeting senescent LepR+ bone marrow mesenchymal stromal cells. Biomater. Adv. 2022, 133, 112635. [Google Scholar] [CrossRef]
- Zhao, H.; Ming, T.; Tang, S.; Ren, S.; Yang, H.; Liu, M.; Tao, Q.; Xu, H. Wnt signaling in colorectal cancer: Pathogenic role and therapeutic target. Mol. Cancer 2022, 21, 144. [Google Scholar] [CrossRef]
- Hayat, R.; Manzoor, M.; Hussain, A. Wnt signaling pathway: A comprehensive review. Cell Biol. Int. 2022, 46, 863–877. [Google Scholar] [CrossRef]
- Bats, M.-L.; Peghaire, C.; Delobel, V.; Dufourcq, P.; Couffinhal, T.; Duplàa, C. Wnt/frizzled Signaling in Endothelium: A Major Player in Blood-Retinal- and Blood-Brain-Barrier Integrity. Cold Spring Harb. Perspect. Med. 2022, 12, a041219. [Google Scholar] [CrossRef]
- Neuhaus, J.; Weimann, A.; Berndt-Paetz, M. Immunocytochemical Analysis of Endogenous Frizzled-(Co-)Receptor Interactions and Rapid Wnt Pathway Activation in Mammalian Cells. Int. J. Mol. Sci. 2021, 22, 12057. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, M.; Xu, F.; Jiang, S. Wnt signaling in breast cancer: Biological mechanisms, challenges and opportunities. Mol. Cancer 2020, 19, 165. [Google Scholar] [CrossRef]
- Sardar, A.; Gautam, S.; Sinha, S.; Rai, D.; Tripathi, A.K.; Dhaniya, G.; Mishra, P.R.; Trivedi, R. Nanoparticles of naturally occurring PPAR-γ inhibitor betulinic acid ameliorates bone marrow adiposity and pathological bone loss in ovariectomized rats via Wnt/β-catenin pathway. Life Sci. 2022, 309, 121020. [Google Scholar] [CrossRef] [PubMed]
- Kalyanaraman, H.; China, S.P.; Cabriales, J.A.; Moininazeri, J.; Casteel, D.E.; Garcia, J.J.; Wong, V.W.; Chen, A.; Sah, R.L.; Boss, G.R.; et al. Protein Kinase G2 Is Essential for Skeletal Homeostasis and Adaptation to Mechanical Loading in Male but Not Female Mice. J. Bone Miner. Res. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Bo, Y.; Tian, Y.; Mao, L.; Xue, C.; Dong, P.; Wang, J. Docosahexaenoic Acid-Enriched Phosphatidylcholine Exerted Superior Effects to Triglyceride in Ameliorating Obesity-Induced Osteoporosis through Up-Regulating the Wnt/β-Catenin Pathway. J. Agric. Food Chem. 2022, 70, 13904–13912. [Google Scholar] [CrossRef]
- Shao, X.; Yang, Y.; Tan, Z.; Ding, Y.; Luo, E.; Jing, D.; Cai, J. Amelioration of bone fragility by pulsed electromagnetic fields in type 2 diabetic KK-Ay mice involving Wnt/β-catenin signaling. Am. J. Physiol. Metab. 2021, 320, E951–E966. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Yu, Q.; Lai, A.; Tian, J. Pulsed electromagnetic field induces Ca(2+)-dependent osteoblastogenesis in C3H10T1/2 mesenchymal cells through the Wnt-Ca(2+)/Wnt-β-catenin signaling pathway. Biochem. Biophys. Res. Commun. 2018, 503, 715–721. [Google Scholar] [CrossRef]
- Shao, X.; Yan, Z.; Wang, D.; Yang, Y.; Ding, Y.; Luo, E.; Jing, D.; Cai, J. Pulsed Electromagnetic Fields Ameliorate Skeletal Deterioration in Bone Mass, Microarchitecture, and Strength by Enhancing Canonical Wnt Signaling-Mediated Bone Formation in Rats with Spinal Cord Injury. J. Neurotrauma 2021, 38, 765–776. [Google Scholar] [CrossRef]
- Jing, D.; Li, F.; Jiang, M.; Cai, J.; Wu, Y.; Xie, K.; Wu, X.; Tang, C.; Liu, J.; Guo, W.; et al. Pulsed electromagnetic fields improve bone microstructure and strength in ovariectomized rats through a Wnt/Lrp5/β-catenin signaling-associated mechanism. PLoS ONE 2013, 8, e79377. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; He, H.; Yang, L.; Chen, S.; Guo, H.; Xia, L.; Liu, H.; Qin, Y.; Liu, C.; Wei, X.; et al. Effects of Pulsed Electromagnetic Fields on Bone Mass and Wnt/β-Catenin Signaling Pathway in Ovariectomized Rats. Arch. Med. Res. 2012, 43, 274–282. [Google Scholar] [CrossRef]
- Wang, P.; Tang, C.; Wu, J.; Yang, Y.; Yan, Z.; Liu, X.; Shao, X.; Zhai, M.; Gao, J.; Liang, S.; et al. Pulsed electromagnetic fields regulate osteocyte apoptosis, RANKL/OPG expression, and its control of osteoclastogenesis depending on the presence of primary cilia. J. Cell. Physiol. 2019, 234, 10588–10601. [Google Scholar] [CrossRef]
- Pi, Y.; Liang, H.; Yu, Q.; Yin, Y.; Xu, H.; Lei, Y.; Han, Z.; Tian, J. Low-frequency pulsed electromagnetic field inhibits RANKL-induced osteoclastic differentiation in RAW264.7 cells by scavenging reactive oxygen species. Mol. Med. Rep. 2019, 19, 4129–4136. [Google Scholar] [CrossRef]
- Lei, Y.; Su, J.; Xu, H.; Yu, Q.; Zhao, M.; Tian, J. Pulsed electromagnetic fields inhibit osteoclast differentiation in RAW264.7 macrophages via suppression of the protein kinase B/mammalian target of rapamycin signaling pathway. Mol. Med. Rep. 2018, 18, 447–454. [Google Scholar] [CrossRef]
- He, Z.; Selvamurugan, N.; Warshaw, J.; Partridge, N.C. Pulsed electromagnetic fields inhibit human osteoclast formation and gene expression via osteoblasts. Bone 2018, 106, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Liu, J.; Yang, Y.; Zhai, M.; Shao, X.; Yan, Z.; Zhang, X.; Wu, Y.; Cao, L.; Sui, B.; et al. Differential intensity-dependent effects of pulsed electromagnetic fields on RANKL-induced osteoclast formation, apoptosis, and bone resorbing ability in RAW264.7 cells. Bioelectromagnetics 2017, 38, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, H.; Han, Z.; Chen, P.; Yu, Q.; Lei, Y.; Li, Z.; Zhao, M.; Tian, J. Pulsed electromagnetic field inhibits RANKL-dependent osteoclastic differentiation in RAW264.7 cells through the Ca 2+-calcineurin-NFATc1 signaling pathway. Biochem. Biophys. Res. Commun. 2017, 482, 289–295. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Zhang, Y.; Chen, J.; Zheng, S.; Huang, H.; Dong, X. Effects of pulsed electromagnetic fields on the expression of NFATc1 and CAII in mouse osteoclast-like cells. Aging Clin. Exp. Res. 2015, 27, 13–19. [Google Scholar] [CrossRef]
- Chang, K.; Chang, W.H.; Tsai, M.-T.; Shih, C. Pulsed Electromagnetic Fields Accelerate Apoptotic Rate in Osteoclasts. Connect. Tissue Res. 2006, 47, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Forsted, D.L.; Dalinka, M.K.; Mitchell, E.; Brighton, C.T.; Alavi, A. Radiologic Evaluation of the Treatment of Nonunion of Fractures by Electrical Stimulation. Radiology 1978, 128, 629–634. [Google Scholar] [CrossRef]
- Creasey, G.H.; Ho, C.H.; Triolo, R.J.; Gater, D.R.; DiMarco, A.F.; Bogie, K.M.; Keith, M.W. Clinical applications of electrical stimulation after spinal cord injury. J. Spinal Cord Med. 2004, 27, 365–375. [Google Scholar] [CrossRef]
- Iimura, K.; Watanabe, N.; Milliken, P.; Hsieh, Y.-H.; Lewis, S.J.; Sridhar, A.; Hotta, H. Chronic Electrical Stimulation of the Superior Laryngeal Nerve in the Rat: A Potential Therapeutic Approach for Postmenopausal Osteoporosis. Biomedicines 2020, 8, 369. [Google Scholar] [CrossRef]
- Lau, R.Y.-C.; Qian, X.; Po, K.-T.; Li, L.-M.; Guo, X. Response of Rat Tibia to Prolonged Unloading Under the Influence of Electrical Stimulation at the Dorsal Root Ganglion. Neuromodulation J. Int. Neuromodulation Soc. 2017, 20, 284–289. [Google Scholar] [CrossRef]
- Lau, Y.C.; Qian, X.; Po, K.T.; Li, L.M.; Guo, X. Electrical stimulation at the dorsal root ganglion preserves trabecular bone mass and microarchitecture of the tibia in hindlimb-unloaded rats. Osteoporos. Int. 2015, 26, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Piazzolla, A.; Solarino, G.; Bizzoca, D.; Garofalo, N.; Dicuonzo, F.; Setti, S.; Moretti, B. Capacitive coupling electric fields in the treatment of vertebral compression fractures. J. Biol. Regul. Homeost. Agents 2015, 29, 637–646. [Google Scholar]
- Rossini, M.; Viapiana, O.; Gatti, D.; de Terlizzi, F.; Adami, S. Capacitively Coupled Electric Field for Pain Relief in Patients with Vertebral Fractures and Chronic Pain. Clin. Orthop. Relat. Res. 2010, 468, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Manjhi, J.; Mathur, R.; Behari, J. Effect of low level capacitive-coupled pulsed electric field stimulation on mineral profile of weight-bearing bones in ovariectomized rats. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 92, 189–195. [Google Scholar] [CrossRef]
- Behari, J.; Behari, J. Changes in bone histology due to capacitive electric field stimulation of ovariectomized rat. Indian J. Med. Res. 2009, 130, 720–725. [Google Scholar]
- Brighton, C.T.; Luessenhop, C.P.; Pollack, S.R.; Steinberg, D.R.; Petrik, M.E.; Kaplan, F.S. Treatment of castration-induced osteoporosis by a capacitively coupled electrical signal in rat vertebrae. J. Bone Jt. Surg. Am. Vol. 1989, 71, 228–236. [Google Scholar] [CrossRef]
- Brighton, C.T.; Tadduni, G.T.; Goll, S.R.; Pollack, S.R. Treatment of denervation/disuse osteoporosis in the rat with a capacitively coupled electrical signal: Effects on bone formation and bone resorption. J. Orthop. Res. 1988, 6, 676–684. [Google Scholar] [CrossRef]
- Brighton, C.T.; Tadduni, G.T.; Pollack, S.R. Treatment of sciatic denervation disuse osteoporosis in the rat tibia with capacitively coupled electrical stimulation. Dose response and duty cycle. J. Bone Jt. Surg. Am. Vol. 1985, 67, 1022–1028. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).