Fractional Q-Switched 1064 nm Laser for Treatment of Atrophic Scars in Asian Skin
Abstract
1. Introduction
2. Materials and Methods
2.1. Laser Device
2.2. Laser Session Protocol
2.3. Efficacy and Safety
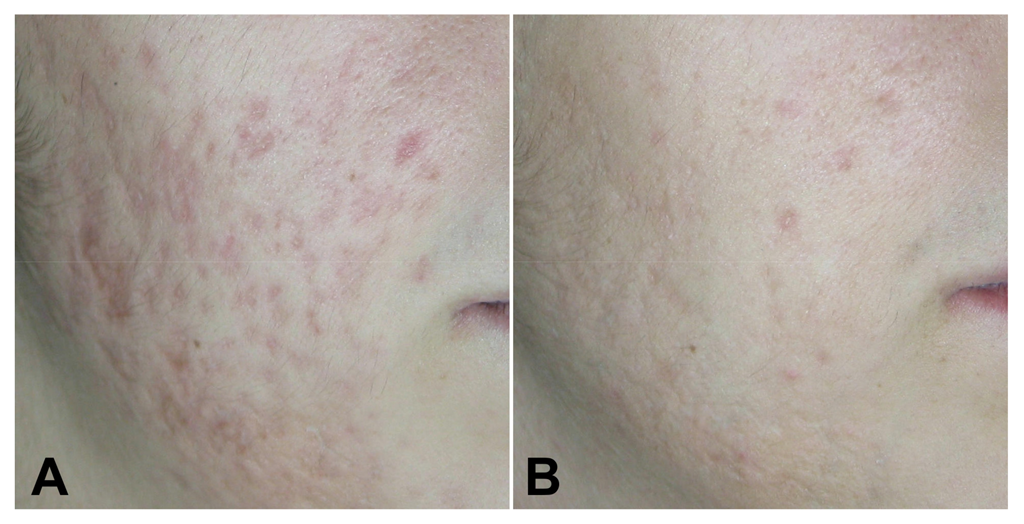
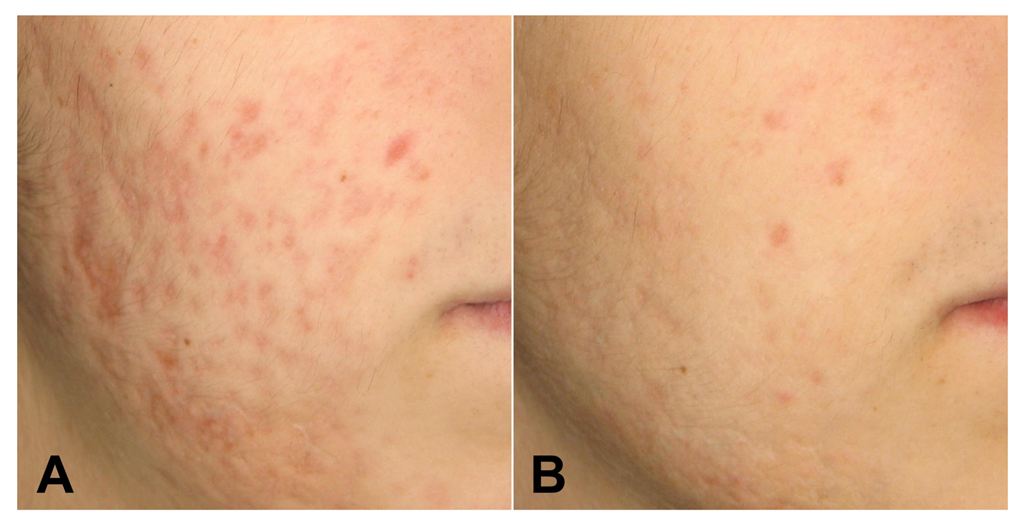
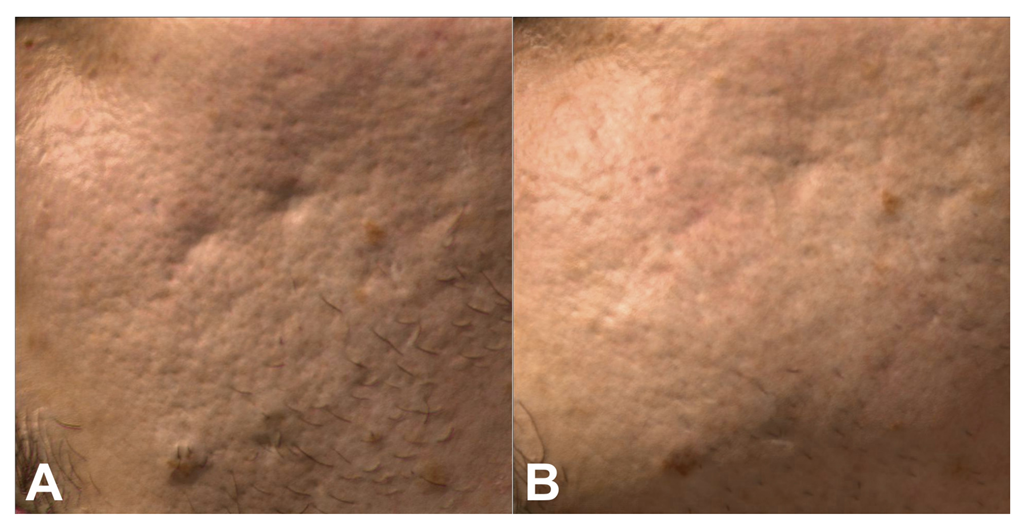
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cannarozzo, G.; Silvestri, M.; Tamburi, F.; Sicilia, C.; Del Duca, E.; Scali, E.; Bennardo, L.; Nisticò, S.P. A new 675-nm laser device in the treatment of acne scars: An observational study. Lasers Med. Sci. 2020, 36, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Taub, A.F. The Treatment of Acne Scars, a 30-Year Journey. Am. J. Clin. Dermatol. 2019, 20, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Jaloux, C.; Bertrand, B.; Degardin, N.; Casanova, D.; Kerfant, N.; Philandrianos, C. Les cicatrices chéloïdes (deuxième partie): Arsenal et stratégie thérapeutique [Keloid scars (part II): Treatment and prevention]. Ann. Chir. Plast. Esthet. 2017, 62, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Kono, T.; Chan, H.H.L.; Do, W.F.G.; Manstein, D.; Sakurai, H.; Takeuchi, M.; Yamaki, T.; Soejima, K.; Nozaki, M. Prospective direct comparison study of fractional resurfacing using different fluences and densities for skin rejuvenation in Asians. Lasers Surg Med. 2007, 39, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Chan, I.L.; Cohen, S.; Da Cunha, M.G.; Maluf, L.C. Characteristics and management of Asian skin. Int. J. Dermatol. 2018, 58, 131–143. [Google Scholar] [CrossRef]
- Cannarozzo, G.; Negosanti, F.; Sannino, M.; Santoli, M.; Bennardo, L.; Banzola, N.; Negosanti, L.; Nisticò, S.P. Q-switched Nd:YAG laser for cosmetic tattoo removal. Dermatol. Ther. 2019, 32, e13042. [Google Scholar] [CrossRef]
- Cannarozzo, G.; Nisticò, S.; Zappia, E.; Del Duca, E.; Provenzano, E.; Patruno, C.; Negosanti, F.; Sannino, M.; Bennardo, L. Q-Switched 1064/532 nm Laser with Nanosecond Pulse in Tattoo Treatment: A Double-Center Retrospective Study. Life 2021, 11, 699, Published on 16 July 2021. [Google Scholar] [CrossRef] [PubMed]
- Del Duca, E.; Zingoni, T.; Bennardo, L.; Di Raimondo, C.; Garofalo, V.; Sannino, M.; Petrini, N.; Cannarozzo, G.; Bianchi, L.; Nisticò, S.P. Long-Term Follow-Up for Q-Switched Nd:YAG Treatment of Nevus of Ota: Are High Number of Treatments Really Required? A Case Report. Photobiomodul Photomed Laser Surg. 2021, 39, 137–140. [Google Scholar] [CrossRef]
- Bennardo, L.; Cannarozzo, G.; Tamburi, F.; Patruno, C.; Provenzano, E.; Nisticò, S.P. Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience. Appl. Sci. 2021, 11, 9712. [Google Scholar] [CrossRef]
- Silvestri, M.; Bennardo, L.; Zappia, E.; Tamburi, F.; Cameli, N.; Cannarozzo, G.; Nisticò, S.P. Q-Switched 1064/532 nm Laser with Picosecond Pulse to Treat Benign Hyperpigmentations: A Single-Center Retrospective Study. Appl. Sci. 2021, 11, 7478. [Google Scholar] [CrossRef]
- Akerman, L.; Solomon-Cohen, E.; Rozenblat, M.; Hodak, E.; Lapidoth, M.; Levi, A. 1064-nm Q-switched fractional Nd:YAG laser is safe and effective for the treatment of post-surgical facial scars. Lasers Med. Sci. 2020, 36, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Goodman, G.J.; Baron, J.A. Postacne scarring—A quantitative global scarring grading system. J. Cosmet. Dermatol. 2006, 5, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Jang, Y.J. Recent Understandings of Biology, Prophylaxis and Treatment Strategies for Hypertrophic Scars and Keloids. Int. J. Mol. Sci. 2018, 19, 711. [Google Scholar] [CrossRef]
- Berman, B.; Maderal, A.; Raphael, B. Keloids and Hypertrophic Scars: Pathophysiology, Classification, and Treatment. Derm. Surg. 2017, 43 (Suppl. 1), S3–S18. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R. Keloid and Hypertrophic Scars Are the Result of Chronic Inflammation in the Reticular Dermis. Int. J. Mol. Sci. 2017, 18, 606, Published 10 March 2017. [Google Scholar] [CrossRef] [PubMed]
- Bs, R.S.C.; Borovikova, A.A.; Bs, K.K.; Banyard, D.A.; Bs, S.L.; Toranto, J.D.; Paydar, K.Z.; Wirth, G.A.; Evans, G.R.D.; Widgerow, A.D.; et al. Current concepts related to hypertrophic scarring in burn injuries. Wound Repair Regen. 2016, 24, 466–477. [Google Scholar] [CrossRef]
- Jacob, C.I.; Dover, J.S.; Kaminer, M.S. Acne scarring: A classification system and review of treatment options. J. Am. Acad. Dermatol. 2001, 45, 109–117. [Google Scholar] [CrossRef]
- Manstein, D.; Herron, G.S.; Sink, R.K.; Tanner, H.; Anderson, R.R. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg. Med. 2004, 34, 426–438. [Google Scholar] [CrossRef]
- Sobanko, J.F.; Alster, T.S. Management of acne scarring, part I: A comparative review of laser surgical approaches. Am. J. Clin. Dermatol. 2012, 1, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Walia, S.; Alster, T.S. Prolonged clinical and histologic effects from CO2 laser resurfacing of atrophic acne scars. Dermatol. Surg. 1999, 25, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Nisticò, S.P.; Tolone, M.; Zingoni, T.; Tamburi, F.; Scali, E.; Bennardo, L.; Cannarozzo, G. A New 675 nm Laser Device in the Treatment of Melasma: Results of a Prospective Observational Study. Photobiomodul Photomed Laser Surg. 2020, 38, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Cannarozzo, G.; Fazia, G.; Bennardo, L.; Tamburi, F.; Amoruso, G.F.; Del Duca, E.; Nisticò, S.P. A New 675 nm Laser Device in the Treatment of Facial Aging: A Prospective Observational Study. Photobiomodul Photomed Laser Surg. 2021, 39, 118–122. [Google Scholar] [CrossRef]
- Sannino, M.; Ambrosio, A.G.; Lodi, G.; Cannarozzo, G.; Bennardo, L.; Nisticò, S.P. A giant epidermal nevus of the face treated with a CO2 and dye laser combination: A case report and literature review. J. Cosmet. Laser Ther. 2021, 23, 59–64. [Google Scholar] [CrossRef]
- Viviano, M.T.; Provini, A.; Mazzanti, C.; Nisticò, S.P.; Patruno, C.; Cannarozzo, G.; Bennardo, S.; Fusco, I.; Bennardo, L. Clinical Evaluation on the Performance and Safety of a Non-Ablative Fractional 1340 nm Laser for the Treatment of Stretch Marks in Adolescents and Young Adults: A Case Series. Bioengineering 2022, 9, 139, Published on 25 March 2022. [Google Scholar] [CrossRef]
- Anderson, R.R.; Parrish, J.A. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983, 220, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Sardana, K.; Manjhi, M.; Garg, V.K.; Sagar, V. Which type of atrophic acne scar (icepick, boxcar, or rolling) responds to non-ablative fractional laser therapy? Dermatol. Surg. 2014, 40, 288–300. [Google Scholar] [CrossRef]
- Wong, T.-S.; Li, J.Z.-H.; Chen, S.; Chan, J.Y.-W.; Gao, W. The Efficacy of Triamcinolone Acetonide in Keloid Treatment: A Systematic Review and Meta-analysis. Front. Med. 2016, 3, 71, Published on 27 December 2016. [Google Scholar] [CrossRef]
- Ogawa, R.; Akaishi, S.; Huang, C.; Dohi, T.; Aoki, M.; Omori, Y.; Koike, S.; Kobe, K.; Akimoto, M.; Hyakusoku, H. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: The importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J. Nippon Med. Sch. 2011, 78, 68–76. [Google Scholar] [CrossRef]
- Leventhal, D.; Furr, M.; Reiter, D. Treatment of keloids and hypertrophic scars: A meta-analysis and review of the literature. Arch. Facial. Plast. Surg. 2006, 8, 362–368. [Google Scholar] [CrossRef]
- Muir, I.F. On the nature of keloid and hypertrophic scars. Br. J. Plast. Surg. 2006, 8, 362–368. [Google Scholar] [CrossRef]
- Har-Shai, Y.; Zouboulis, C.C. Intralesional Cryotherapy for the Treatment of Keloid Scars: A Prospective Study. Plast Reconstr. Surg. 2015, 136, 397e–398e. [Google Scholar] [CrossRef] [PubMed]
- Nisticò, S.; Campolmi, P.; Moretti, S.; Del Duca, E.; Bruscino, N.; Conti, R.; Bassi, A.; Cannarozzo, G. Nonconventional Use of Flash-Lamp Pulsed-Dye Laser in Dermatology. Bio. Med. Res. Int. 2016, 2016, 7981640. [Google Scholar] [CrossRef] [PubMed]
- Guida, S.; Galimberti, M.G.; Bencini, M.; Pellacani, G.; Bencini, P.L. Treatment of striae distensae with non-ablative fractional laser: Clinical and in vivo microscopic documentation of treatment efficacy. Lasers Med. Sci. 2017, 33, 75–78. [Google Scholar] [CrossRef]
- Koike, S.; Akaishi, S.; Nagashima, Y.; Dohi, T.; Hyakusoku, H.; Ogawa, R. Nd: YAG Laser Treatment for Keloids and Hypertrophic Scars: An Analysis of 102 Cases. Plast Reconstr. Surg. Glob. Open. 2015, 2, e272, Published on 8 January 2015. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, J.F.; Petit, L.; Hermanns-Le, T.; Pierard, G.E. Analytic quantification of phototype-related regional skin complexion. Ski. Res. Technol. 2001, 7, 168–171. [Google Scholar] [CrossRef]
- Chiwo, F.S.; Guevara, E.; Ramírez-Elías, M.G.; Castillo-Martínez, C.C.; Osornio-Martínez, C.E.; Cabrera-Alonso, R.; Pérez-Atamoros, R. Use of Raman spectroscopy in the assessment of skin after CO2 ablative fractional laser surgery on acne scars. Ski. Res. Technol. 2019, 25, 805–809. [Google Scholar] [CrossRef]
- Naouri, M.; Atlan, M.; Perrodeau, E.; Georgesco, G.; Khallouf, R.; Martin, L.; Machet, L. High-resolution ultrasound imaging to demonstrate and predict efficacy of carbon dioxide fractional resurfacing laser treatment. Dermatol. Surg. 2011, 37, 596–603. [Google Scholar] [CrossRef]
- Berardesca, E.; Maibach, H. Ethnic skin: Overview of structure and function. J. Am. Acad. Dermatol. 2003, 48 (Suppl. 6), S139–S142. [Google Scholar] [CrossRef]
- Alaluf, S.; Atkins, D.; Barrett, K.; Blount, M.; Carter, N.; Heath, A. Ethnic variation in melanin content and composition in photoexposed and photoprotected human skin. Pigment. Cell Res. 2002, 15, 112–118. [Google Scholar] [CrossRef]
- Taylor, S.C. Skin of color: Biology, structure, function, and implications for dermatologic disease. J. Am. Acad. Dermatol. 2002, 46 (Suppl. 2), S41–S62. [Google Scholar] [CrossRef]
- Yeung, C.K.; Teo, L.H.Y.; Xiang, L.H.; Chan, H.H. A community-based epidemiological study of acne vulgaris in Hong Kong adolescents. Acta Derm Venereol. 2002, 82, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.H. Photoaging in Asians. Photodermatol Photoimmunol Photomed. 2003, 19, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Battle, E.F., Jr.; Soden, C.E., Jr. The use of lasers in darker skin types. Semin. Cutan. Med. Surg. 2009, 28, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.H.; Wong, D.S.; Ho, W.S.; Lam, L.K.; Wei, W. The use of pulsed dye laser for the prevention and treatment of hypertrophic scars in chinese persons. Derm. Surg. 2004, 30, 987–994. [Google Scholar] [CrossRef]
- Alster, T.S.; Williams, C.M. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet 1995, 345, 1198–1200. [Google Scholar] [CrossRef]
- Bernstein, L.J.; Kauvar, A.N.B.; Grossman, M.C.; Geronemus, R.G. The short- and long-term side effects of carbon dioxide laser resurfacing. Derm. Surg. 1997, 23, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Nanni, C.A.; Alster, T.S. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Derm. Surg. 1998, 24, 315–320. [Google Scholar] [CrossRef]
- Manaloto, R.M.P.; Alster, T. Laser resurfacing for refractory melasma. Dermatol. Surg. 1999, 25, 121–123. [Google Scholar] [CrossRef][Green Version]
- Polnikorn, N.; Goldberg, D.J.; Suwanchinda, A.; Ng, S.W. Erbium:YAG laser resurfacing in Asians. Derm. Surg. 1998, 24, 1303–1307. [Google Scholar] [CrossRef]
- Cho, S.I.; Kim, Y.C. Treatment of facial wrinkles with char-free carbon dioxide laser and erbium: YAG laser. Kor. J. Derm. 1999, 37, 177–184. [Google Scholar]
- Alster, T.; Hirsch, R. Single-pass CO2 laser skin resurfacing of light and dark skin: Extended experience with 52 patients. J. Cosmet. Laser. 2003, 5, 39–42. [Google Scholar] [CrossRef]
- Haimovic, A.; Brauer, J.A.; Cindy Bae, Y.S.; Geronemus, R.G. Safetyof a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: A retrospective review. J. Am. Acad. Derm. 2016, 74, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Brauer, J.A.; Kazlouskaya, V.; Alabdulrazzaq, H.; Bae, Y.S.; Bernstein, L.J.; Anolik, R.; Heller, P.A.; Geronemus, R.G. Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol. 2015, 151, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.S.; Blinder, P.; Migliori, B.J.; Neev, J.; Jin, Y.; Squier, J.A.; Kleinfeld, D. Plasma-mediated ablation: An optical tool for submicrometer surgery on neuronal and vascular systems. Curr. Opin. Biotechnol. 2009, 20, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Haedersdal, M.; Bech-Thomsen, N.; Poulsen, T.; Wulf, C.H. Ultraviolet exposure influences laser-induced wounds, scars, and hyperpigmentation: A murine study. Plast Reconstr Surg. 1998, 101, 1315–1322. [Google Scholar] [CrossRef]
| (Grade) Type | Number of lesions: 1 (1–10) | Number of lesions: 2 (11–20) | Number of lesions: 3 (21–30) |
|---|---|---|---|
| A Milder scarring (1 point each) B Moderate scarring (2 points each) C Severe scarring (3 points each) D Hyperplastic (papular) E Hyperplastic | 1 point 2 points 3 points 2 points <5 cm2 Area 6 points | 2 points 4 points 6 points 4 points 5–20 cm2 Area 12 points | 3 points 6 points 9 points 6 points >20 cm2 Area 18 points |
| ID | Sex | Age | Photo Type | Acne Scarring Grading System before | Acne Scarring Grading System after 3 Months | Pain VAS | Side Effect |
|---|---|---|---|---|---|---|---|
| treatment | |||||||
| 1 | F | 24 | 3 | 15 | 8 | 3 | None |
| 2 | F | 31 | 3 | 21 | 12 | 2 | None |
| 3 | F | 19 | 4 | 18 | 9 | 2 | None |
| 4 | F | 26 | 4 | 24 | 18 | 1 | None |
| 5 | F | 25 | 4 | 31 | 23 | 2 | None |
| 6 | F | 31 | 3 | 32 | 21 | 4 | Erythema |
| 7 | F | 42 | 2 | 13 | 4 | 1 | None |
| 8 | F | 28 | 4 | 28 | 15 | 2 | None |
| 9 | F | 29 | 3 | 37 | 26 | 3 | None |
| 10 | F | 20 | 3 | 25 | 13 | 2 | None |
| 11 | F | 33 | 4 | 21 | 9 | 1 | None |
| 12 | F | 37 | 4 | 17 | 6 | 2 | None |
| 13 | F | 29 | 3 | 30 | 18 | 2 | None |
| 14 | M | 19 | 3 | 21 | 16 | 3 | Erythema |
| 15 | F | 44 | 3 | 16 | 13 | 2 | None |
| 16 | F | 41 | 4 | 24 | 22 | 5 | None |
| 17 | M | 31 | 4 | 31 | 27 | 3 | None |
| 18 | F | 28 | 3 | 34 | 31 | 1 | Erythema |
| 19 | F | 32 | 4 | 35 | 16 | 5 | None |
| 20 | F | 37 | 4 | 14 | 14 | 2 | None |
| 21 | F | 21 | 4 | 10 | 4 | 4 | None |
| 22 | F | 26 | 4 | 18 | 11 | 3 | None |
| 23 | F | 24 | 3 | 21 | 9 | 2 | None |
| 24 | F | 21 | 3 | 13 | 5 | 3 | None |
| 25 | F | 27 | 3 | 15 | 9 | 2 | None |
| 26 | F | 18 | 4 | 24 | 12 | 2 | None |
| 27 | F | 37 | 4 | 21 | 11 | 1 | None |
| 28 | F | 34 | 3 | 17 | 9 | 3 | None |
| 29 | F | 46 | 3 | 29 | 19 | 3 | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nisticò, S.P.; Sannino, M.; Fasano, G.; Marigliano, M.; Negosanti, F.; Bennardo, L.; Cannarozzo, G. Fractional Q-Switched 1064 nm Laser for Treatment of Atrophic Scars in Asian Skin. Medicina 2022, 58, 1190. https://doi.org/10.3390/medicina58091190
Nisticò SP, Sannino M, Fasano G, Marigliano M, Negosanti F, Bennardo L, Cannarozzo G. Fractional Q-Switched 1064 nm Laser for Treatment of Atrophic Scars in Asian Skin. Medicina. 2022; 58(9):1190. https://doi.org/10.3390/medicina58091190
Chicago/Turabian StyleNisticò, Steven Paul, Mario Sannino, Gaia Fasano, Miriam Marigliano, Francesca Negosanti, Luigi Bennardo, and Giovanni Cannarozzo. 2022. "Fractional Q-Switched 1064 nm Laser for Treatment of Atrophic Scars in Asian Skin" Medicina 58, no. 9: 1190. https://doi.org/10.3390/medicina58091190
APA StyleNisticò, S. P., Sannino, M., Fasano, G., Marigliano, M., Negosanti, F., Bennardo, L., & Cannarozzo, G. (2022). Fractional Q-Switched 1064 nm Laser for Treatment of Atrophic Scars in Asian Skin. Medicina, 58(9), 1190. https://doi.org/10.3390/medicina58091190








