Assessment of Instability in Thoracolumbar Burst Fractures Using a New Bone Scan Scoring System
Abstract
:1. Introduction
2. Methods
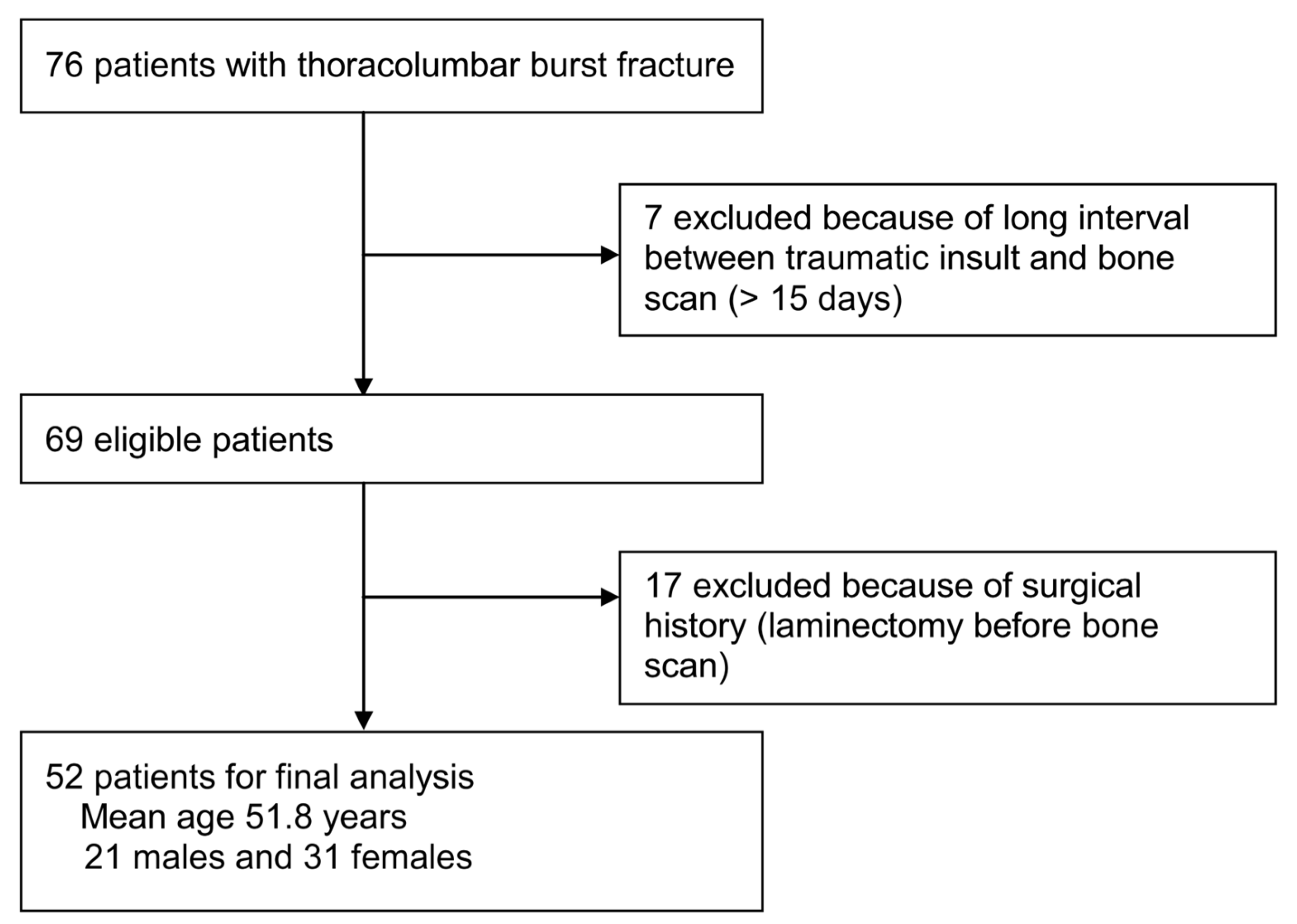
2.1. Patients
2.2. Indexes Used to Assess the Indications for Surgery
2.3. Data Analysis
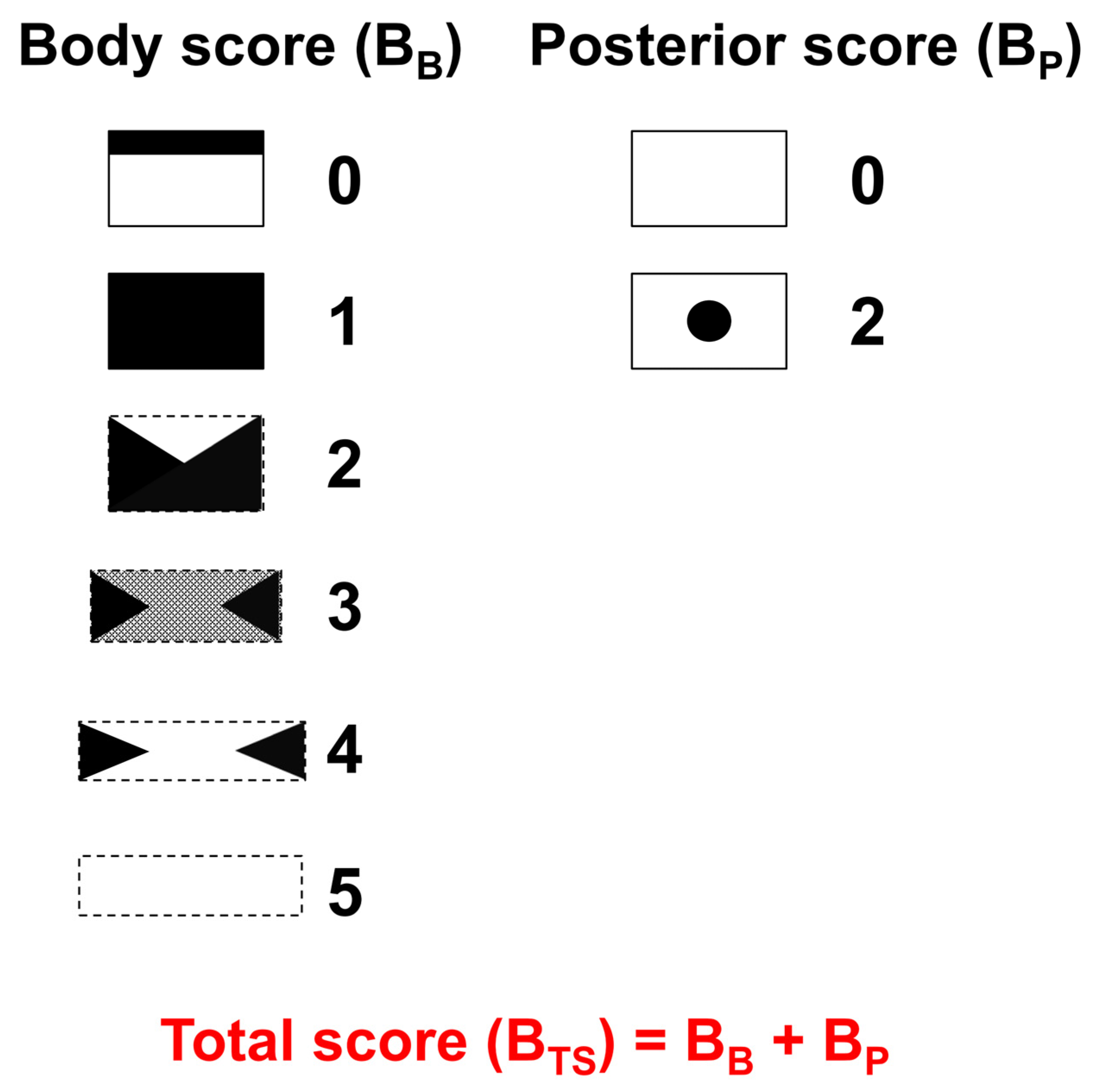
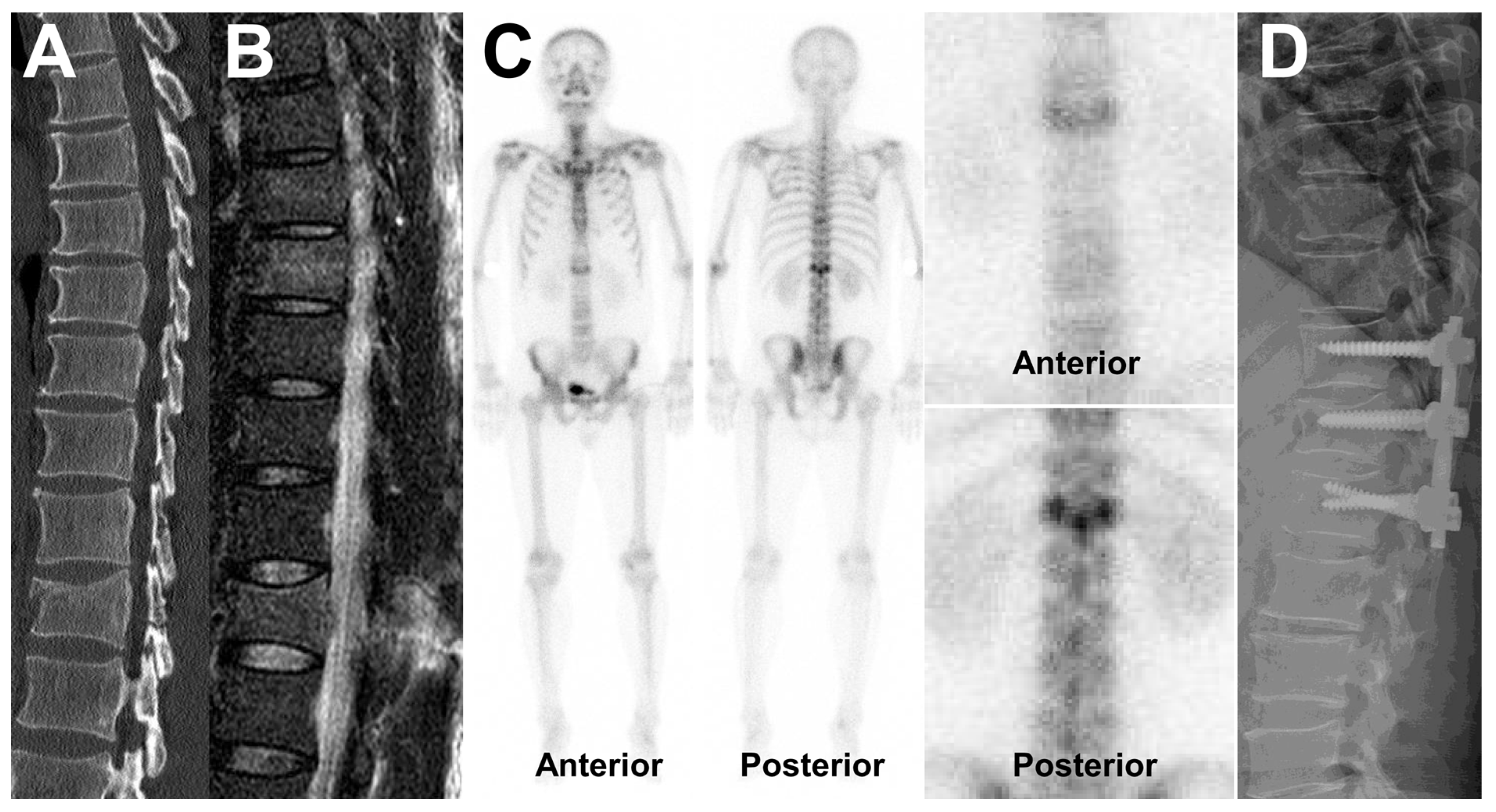
2.4. Bone Scan Assessment
2.5. MRI Assessment
2.6. Clinical Assessment
2.7. Statistical Analysis
3. Results
3.1. Patient and Lesion Characteristics
3.2. Associations between Bone Scan Scoring System Score, Instability, and TLICS
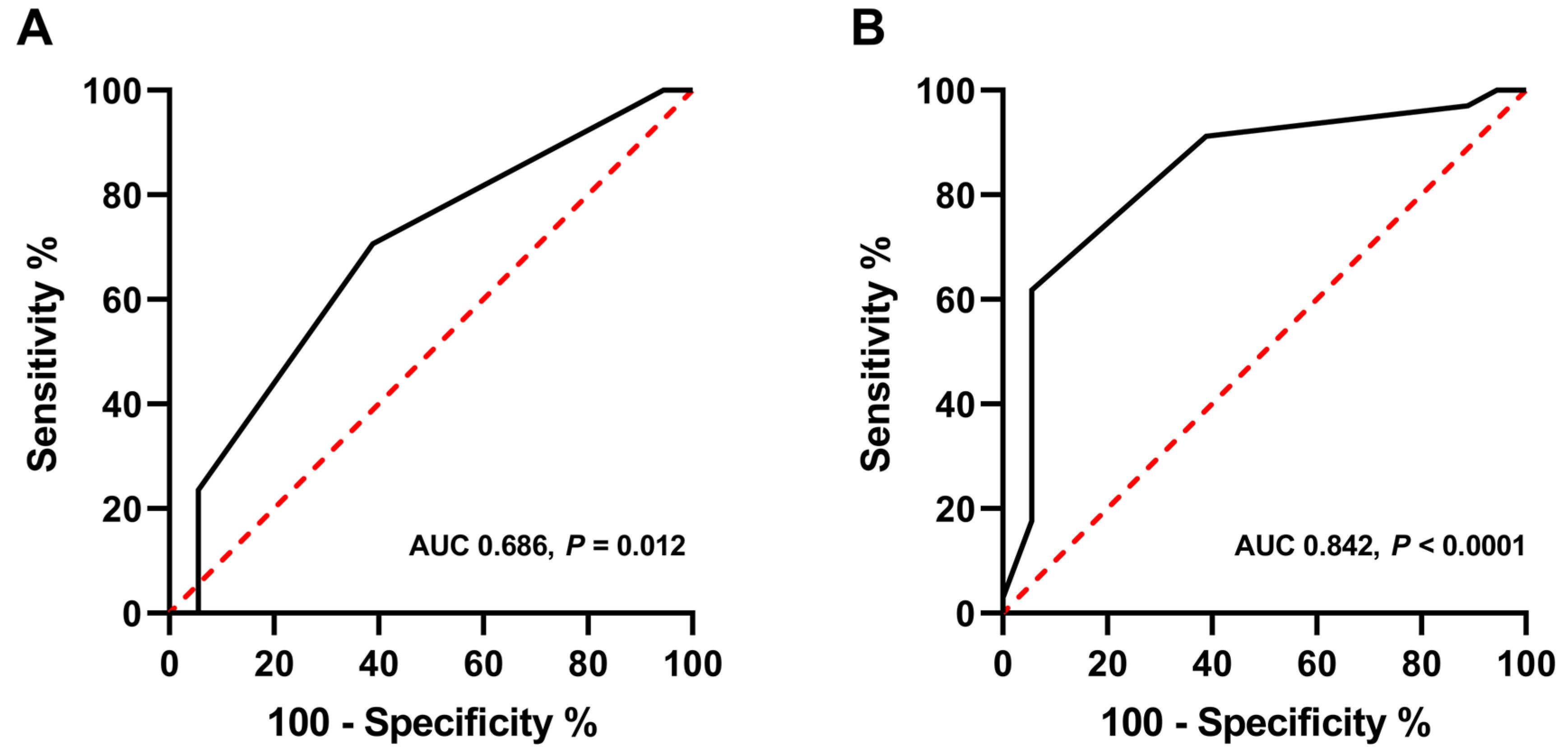
3.3. Diagnostic Performance of the Bone Scan Scoring System
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zileli, M.; Sharif, S.; Fornari, M. Incidence and Epidemiology of Thoracolumbar Spine Fractures: WFNS Spine Committee Recommendations. Neurospine 2021, 18, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Alpantaki, K.; Bano, A.; Pasku, D.; Mavrogenis, A.F.; Papagelopoulos, P.J.; Sapkas, G.S.; Korres, D.S.; Katonis, P. Thoracolumbar burst fractures: A systematic review of management. Orthopedics 2010, 33, 422–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denis, F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983, 8, 817–831. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Lehman, R.A.J.; Hurlbert, R.J.; Anderson, P.A.; Harris, M.; Hedlund, R.; Harrop, J.; Dvorak, M.; Wood, K.; Fehlings, M.G.; et al. A new classification of thoracolumbar injuries: The importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005, 30, 2325–2333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.A.; Dailey, A.; Brodke, D.S.; Daubs, M.; Harrop, J.; Whang, P.G.; Vaccaro, A.R. Thoracolumbar spine trauma classification: The Thoracolumbar Injury Classification and Severity Score system and case examples. J. Neurosurg. Spine 2009, 10, 201–206. [Google Scholar] [CrossRef]
- Cankaya, D.; Yilmaz, S.; Deveci, A.; Dundar, A.; Yoldas, B.; Toprak, A.; Tabak, Y. Clinical and radiological outcomes of conservative treatment after stable post-traumatic thoracolumbar fractures in elderly: Is it really best option for all elderly patients? Ann. Med. Surg. 2015, 4, 346–350. [Google Scholar] [CrossRef]
- Pizones, J.; Castillo, E. Assessment of acute thoracolumbar fractures: Challenges in multidetector computed tomography and added value of emergency MRI. Semin. Musculoskelet. Radiol. 2013, 17, 389–395. [Google Scholar]
- Scharf, S. SPECT/CT imaging in general orthopedic practice. Semin. Nucl. Med. 2009, 39, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Holdsworth, F.W. Fractures and Dislocations of the Lower Thoracic and Lumbar Spines, with and without Neurological Involvement. Curr. Pract. Orthop. Surg. 1964, 23, 61–83. [Google Scholar] [PubMed]
- McCormack, T.; Karaikovic, E.; Gaines, R.W. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994, 19, 1741–1744. [Google Scholar] [CrossRef] [PubMed]
- Dugonjic, S.; Ajdinovic, B.; Cirkovic, M.; Ristic, G. Bone scintigraphy can diagnose osteoporotic vertebral compression fractures better than conventional radiography. Hell J. Nucl. Med. 2017, 20, 155. [Google Scholar] [PubMed]
- Jun, D.S.; An, B.K.; Yu, C.H.; Hwang, K.H.; Paik, J.W. Practical use of bone scan in patients with an osteoporotic vertebral compression fracture. J. Korean Med. Sci. 2015, 30, 194–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, K.B.; Buttermann, G.R.; Phukan, R.; Harrod, C.C.; Mehbod, A.; Shannon, B.; Bono, C.M.; Harris, M.B. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: A prospective randomized study with follow-up at sixteen to twenty-two years. J. Bone Jt. Surg. Am. 2015, 97, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, W.J.; Liu, T.J.; Shen, Y.S. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976) 2001, 26, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Siebenga, J.; Leferink, V.J.; Segers, M.J.; Elzinga, M.J.; Bakker, F.C.; Haarman, H.J.; Rommens, P.M.; ten Duis, H.J.; Patka, P. Treatment of traumatic thoracolumbar spine fractures: A multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006, 31, 2881–2890. [Google Scholar] [CrossRef] [PubMed]
- Nataraj, A.; Jack, A.S.; Ihsanullah, I.; Nomani, S.; Kortbeek, F.; Fox, R. Outcomes in Thoracolumbar Burst Fractures with a Thoracolumbar Injury Classification Score (TLICS) of 4 Treated with Surgery Versus Initial Conservative Management. Clin. Spine Surg. 2018, 31, 317–321. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) |
| Sex | |
| Male | 21 (40%) |
| Female | 31 (60%) |
| Age (years) | Mean 51.8 (range; 20–88) |
| Lesion location | |
| Thoracic spine | 18 (35%) |
| Lumbar spine | 34 (65%) |
| Instability | |
| Stable | 18 (35%) |
| Unstable | 34 (65%) |
| TLICS | |
| ≥5 | 21 (40%) |
| <5 | 31 (60%) |
| Bone Scan Score | n (%) |
| BB (Body score) | |
| Score 0 | 1 (2%) |
| Score 1 | 2 (4%) |
| Score 2 | 18 (35%) |
| Score 3 | 22 (42%) |
| Score 4 | 8 (15%) |
| Score 5 | 1 (2%) |
| BP (Posterior score) | |
| Score 0 | 38 (73%) |
| Score 2 | 14 (27%) |
| BTS (Total score) | |
| Score 0 | 1 (2%) |
| Score 1 | 2 (4%) |
| Score 2 | 11 (21%) |
| Score 3 | 16 (31%) |
| Score 4 | 15 (29%) |
| Score 5 | 6 (11%) |
| Score 6 | 1 (2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, H.J.; Park, S.H.; Choi, J.I.; Kim, J.Y.; Seo, M. Assessment of Instability in Thoracolumbar Burst Fractures Using a New Bone Scan Scoring System. Medicina 2022, 58, 979. https://doi.org/10.3390/medicina58080979
Choi HJ, Park SH, Choi JI, Kim JY, Seo M. Assessment of Instability in Thoracolumbar Burst Fractures Using a New Bone Scan Scoring System. Medicina. 2022; 58(8):979. https://doi.org/10.3390/medicina58080979
Chicago/Turabian StyleChoi, Hyung Jin, Seol Hoon Park, Jun Ik Choi, Jae Young Kim, and Minjung Seo. 2022. "Assessment of Instability in Thoracolumbar Burst Fractures Using a New Bone Scan Scoring System" Medicina 58, no. 8: 979. https://doi.org/10.3390/medicina58080979
APA StyleChoi, H. J., Park, S. H., Choi, J. I., Kim, J. Y., & Seo, M. (2022). Assessment of Instability in Thoracolumbar Burst Fractures Using a New Bone Scan Scoring System. Medicina, 58(8), 979. https://doi.org/10.3390/medicina58080979






