Impact of Local Anesthetics on Cancer Behavior and Outcome during the Perioperative Period: A Review
Abstract
1. Introduction
2. Circulating Tumor Cells (CTCs)
3. Anti-Inflammatory Effects of Local Anesthetics Potentially Affecting Metastases Immune Modulation/Natural Killer (NK) Cell Activity
4. Endothelial Barrier, Leucocyte Activation, Leukocyte/Tumor Cell Adhesion, and Transmigration
5. Direct Effects of LAs on Cancer Cells
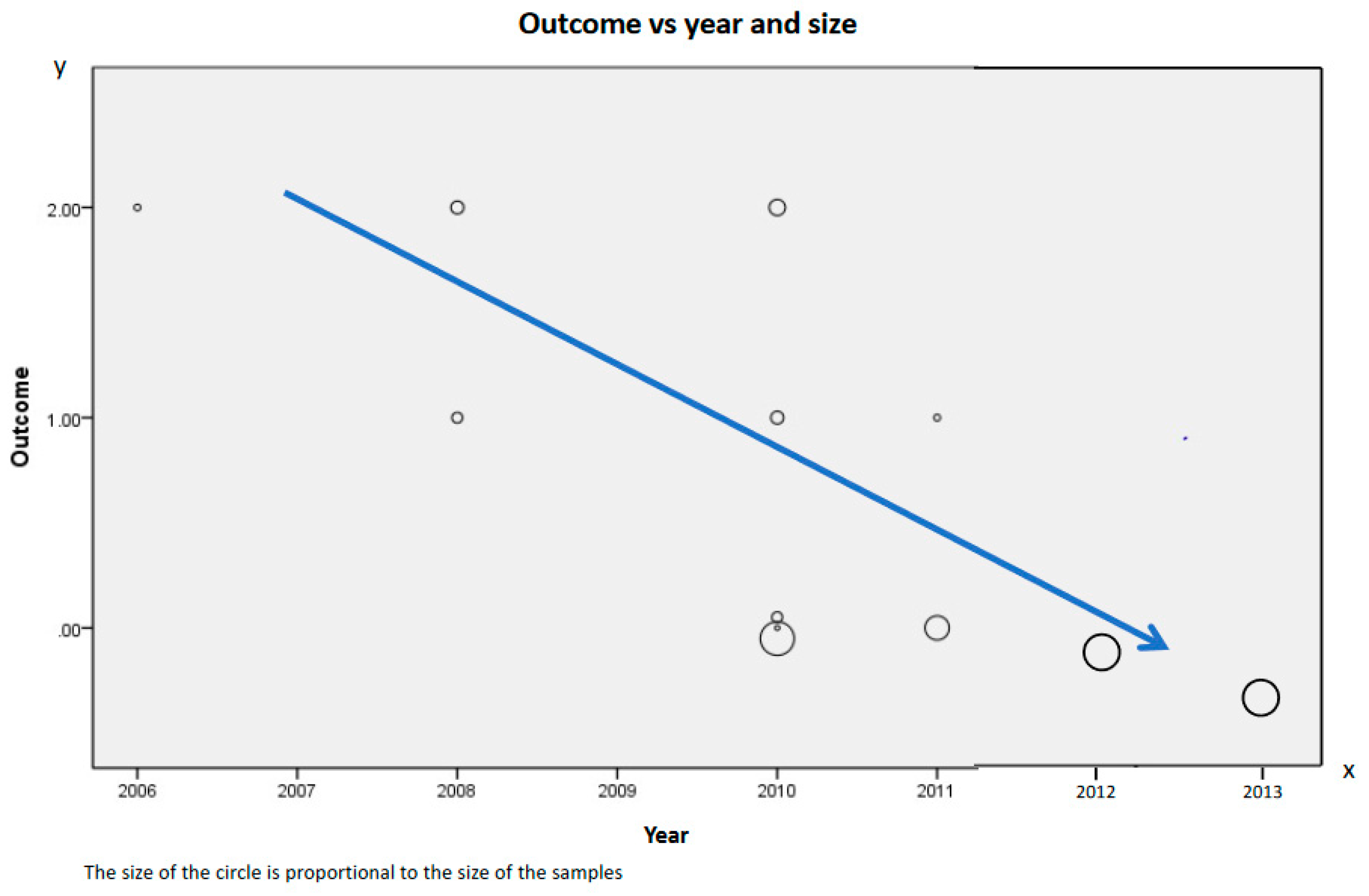
6. Human Retrospective Studies
7. Prospective Human Studies
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, P.; Vejborg, I.; Kroman, N.; Holten, I.; Garne, J.P.; Vedsted, P.; Moller, S.; Lynge, E. Position paper: Breast cancer screening, diagnosis, and treatment in Denmark. Acta Oncol. 2014, 53, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, M.; Neeman, E.; Sharon, E.; Ben-Eliyahu, S. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat. Rev. Clin. Oncol. 2015, 12, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef]
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444. [Google Scholar] [CrossRef]
- Dillekas, H.; Rogers, M.S.; Straume, O. Are 90% of deaths from cancer caused by metastases? Cancer Med. 2019, 8, 5574–5576. [Google Scholar] [CrossRef]
- Guan, X. Cancer metastases: Challenges and opportunities. Acta Pharm. Sin. B 2015, 5, 402–418. [Google Scholar] [CrossRef]
- Hollmann, M.W.; Durieux, M.E. Local anesthetics: Effects on inflammation, wound healing and coagulation. Prog. Anesthesiol. 2000, 14, 291–304. [Google Scholar]
- Hollmann, M.W.; Durieux, M.E. Effects on the central nervous system and bronchial reactivity. Prog. Anesthesiol. 2000, 14, 323–336. [Google Scholar]
- Hollmann, M.W.; Difazio, C.A.; Durieux, M.E. Ca-signaling G-protein-coupled receptors: A new site of local anesthetic action? Reg. Anesth. Pain Med. 2001, 26, 565–571. [Google Scholar] [CrossRef]
- Lin, E.; Calvano, S.E.; Lowry, S.F. Cytokine response in abdominal surgery. In Cytokines and the Abdominal Surgeon; Landes Bioscience: Austin, TX, USA, 1998; pp. 17–34. [Google Scholar]
- Brochner, A.C.; Toft, P. Pathophysiology of the systemic inflammatory response after major accidental trauma. Scand. J. Trauma Resusc. Emerg. Med. 2009, 17, 43. [Google Scholar] [CrossRef] [PubMed]
- De Wit, S.; vaevon Dalum, G.; Terstappen, L.W. Detection of circulating tumor cells. Scientifica 2014, 2014, 819362. [Google Scholar] [CrossRef] [PubMed]
- Gorges, T.M.; Pantel, K. Circulating tumor cells as therapy-related biomarkers in cancer patients. Cancer Immunol. Immunother. 2013, 62, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Asworth, T.R. A case of cancer in which cells similar to those in tumors were seen in the blood after death. Aust. Med. J. 1869, 14, 146–149. [Google Scholar]
- Glodblatt, S.A.; Nadel, E.M. Cancer Cells in the Circulating Blood. Cancer Prog. 1963, 92, 119–140. [Google Scholar]
- Sergeant, G.; Roskams, T.; van Pelt, J.; Houtmeyers, F.; Aerts, R.; Topal, B. Perioperative cancer cell dissemination detected with a real-time RT-PCR assay for EpCAM is not associated with worse prognosis in pancreatic ductal adenocarcinoma. BMC Cancer 2011, 11, 47. [Google Scholar] [CrossRef]
- Lurje, G.; Schiesser, M.; Claudius, A.; Schneider, P.M. Circulating tumor cells in gastrointestinal malignancies: Current techniques and clinical implications. J. Oncol. 2010, 2010, 392652. [Google Scholar] [CrossRef]
- Plaks, V.; Koopman, C.D.; Werb, Z. Cancer. Circulating tumor cells. Science 2013, 341, 1186–1188. [Google Scholar] [CrossRef]
- Alsina, E.; Matute, E.; Ruiz-Huerta, A.D.; Gilsanz, F. The effects of sevoflurane or remifentanil on the stress response to surgical stimulus. Curr. Pharm. Des. 2014, 20, 5449–5468. [Google Scholar] [CrossRef]
- Angele, M.K.; Faist, E. Clinical review: Immunodepression in the surgical patient and increased susceptibility to infection. Crit. Care 2002, 6, 298–305. [Google Scholar] [CrossRef]
- Salmon, P.; Kaufman, L. Preoperative anxiety and endocrine response to surgery. Lancet 1990, 335, 1340. [Google Scholar] [CrossRef]
- Chachkhiani, I.; Gurlich, R.; Maruna, P.; Frasko, R.; Lindner, J. The postoperative stress response and its reflection in cytokine network and leptin plasma levels. Physiol. Res. 2005, 54, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Angka, L.; Khan, S.T.; Kilgour, M.K.; Xu, R.; Kennedy, M.A. Auer RC: Dysfunctional Natural Killer Cells in the Aftermath of Cancer Surgery. Int. J. Mol. Sci. 2017, 18, 1787. [Google Scholar] [CrossRef] [PubMed]
- Kiessling, R.; Klein, E.; Wigzell, H. “Natural” killer cells in the mouse. I. Cytotoxic cells with specificity for mouse Moloney leukemia cells. Specificity and distribution according to genotype. Eur. J. Immunol. 1975, 5, 112–117. [Google Scholar] [CrossRef]
- Baginska, J.; Viry, E.; Paggetti, J.; Medves, S.; Berchem, G.; Moussay, E.; Janji, B. The critical role of the tumor microenvironment in shaping natural killer cell-mediated anti-tumor immunity. Front. Immunol. 2013, 4, 490. [Google Scholar] [CrossRef]
- Iannone, F.; Porzia, A.; Peruzzi, G.; Birarelli, P.; Milana, B.; Sacco, L.; Dinatale, G.; Peparini, N.; Prezioso, G.; Battella, S.; et al. Effect of surgery on pancreatic tumor-dependent lymphocyte asset: Modulation of natural killer cell frequency and cytotoxic function. Pancreas 2015, 44, 386–933. [Google Scholar] [CrossRef]
- Ramirez, M.F.; Ai, D.; Bauer, M.; Vauthey, J.N.; Gottumukkala, V.; Kee, S.; Shon, D.; Truty, M.; Kuerer, H.M.; Kurz, A.; et al. Innate immune function after breast, lung, and colorectal cancer surgery. J. Surg. Res. 2015, 194, 185–193. [Google Scholar] [CrossRef]
- Ben-Eliyahu, S.; Page, G.G.; Yirmiya, R.; Shakhar, G. Evidence that stress and surgical interventions promote tumor development by suppressing natural killer cell activity. Int. J. Cancer 1999, 80, 880–888. [Google Scholar] [CrossRef]
- Melamed, R.; Bar-Yosef, S.; Shakhar, G.; Shakhar, K.; Ben-Eliyahu, S. Suppression of natural killer cell activity and promotion of tumor metastasis by ketamine, thiopental, and halothane, but not by propofol: Mediating mechanisms and prophylactic measures. Anesth. Analg. 2003, 97, 1331–1339. [Google Scholar] [CrossRef]
- Krog, J.; Hokland, M.; Ahlburg, P.; Parner, E.; Tonnesen, E. Lipid solubility- and concentration-dependent attenuation of in vitro natural killer cell cytotoxicity by local anesthetics. Acta Anaesthesiol. Scand. 2002, 46, 875–881. [Google Scholar] [CrossRef]
- Ramirez, M.F.; Tran, P.; Cata, J.P. The effect of clinically therapeutic plasma concentrations of lidocaine on natural killer cell cytotoxicity. Reg. Anesth. Pain Med. 2015, 40, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Jaura, A.I.; Flood, G.; Gallagher, H.C.; Buggy, D.J. Differential effects of serum from patients administered distinct anaesthetic techniques on apoptosis in breast cancer cells in vitro: A pilot study. Br. J. Anaesth. 2014, 113 (Suppl. S1), i63–i67. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Zhang, Y.; Xi, H. The effects of epidural anaesthesia and analgesia on natural killer cell cytotoxicity and cytokine response in patients with epithelial ovarian cancer undergoing radical resection. J. Int Med. Res. 2012, 40, 1822–1829. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.L.; Yan, H.D.; Liu, Y.Y.; Sun, B.Z.; Huang, R.; Wang, X.S.; Lei, W.F. Intraoperative intravenous lidocaine exerts a protective effect on cell-mediated immunity in patients undergoing radical hysterectomy. Mol. Med. Rep. 2015, 12, 7039–7044. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Gu, F.M.; Gao, Q.; Li, Q.L.; Zhou, J.; Miao, C.H. Effects of anesthetic methods on preserving anti-tumor T-helper polarization following hepatectomy. World J. Gastroenterol. 2012, 18, 3089–3098. [Google Scholar] [CrossRef] [PubMed]
- Bernabe, D.G.; Tamae, A.C.; Biasoli, E.R.; Oliveira, S.H. Stress hormones increase cell proliferation and regulates interleukin-6 secretion in human oral squamous cell carcinoma cells. Brain Behav. Immun. 2011, 25, 574–583. [Google Scholar] [CrossRef]
- Yang, E.V.; Kim, S.J.; Donovan, E.L.; Chen, M.; Gross, A.C.; Webster Marketon, J.I.; Barsky, S.H.; Glaser, R. Norepinephrine upregulates VEGF, IL-8, and IL-6 expression in human melanoma tumor cell lines: Implications for stress-related enhancement of tumor progression. Brain Behav. Immun. 2009, 23, 267–275. [Google Scholar] [CrossRef]
- Ortiz, M.P.; Godoy, M.C.; Schlosser, R.S.; Ortiz, R.P.; Godoy, J.P.; Santiago, E.S.; Rigo, F.K.; Beck, V.; Duarte, T.; Duarte, M.M.; et al. Effect of endovenous lidocaine on analgesia and serum cytokines: Double-blinded and randomized trial. J. Clin. Anesth. 2016, 35, 70–77. [Google Scholar] [CrossRef]
- Blumenthal, S.; Borgeat, A.; Pasch, T.; Reyes, L.; Booy, C.; Lambert, M.; Schimmer, R.C.; Beck-Schimmer, B. Ropivacaine decreases inflammation in experimental endotoxin-induced lung injury. Anesthesiology 2006, 104, 961–969. [Google Scholar] [CrossRef]
- Piegeler, T.; Dull, R.O.; Hu, G.; Castellon, M.; Chignalia, A.Z.; Koshy, R.G.; Votta-Velis, E.G.; Borgeat, A.; Schwartz, D.E.; Beck-Schimmer, B.; et al. Ropivacaine attenuates endotoxin plus hyperinflation-mediated acute lung injury via inhibition of early-onset Src-dependent signaling. BMC Anesthesiol. 2014, 14, 57. [Google Scholar] [CrossRef][Green Version]
- Piegeler, T.; Votta-Velis, E.G.; Bakhshi, F.R.; Mao, M.; Carnegie, G.; Bonini, M.G.; Schwartz, D.E.; Borgeat, A.; Beck-Schimmer, B.; Minshall, R.D. Endothelial barrier protection by local anesthetics: Ropivacaine and lidocaine block tumor necrosis factor-alpha-induced endothelial cell Src activation. Anesthesiology 2014, 120, 1414–1428. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Minshall, R.D. Regulation of transendothelial permeability by Src kinase. Microvasc. Res. 2009, 77, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Roman, J.; Zentella-Dehesa, A. Vascular permeability changes involved in tumor metastasis. Cancer Lett. 2013, 335, 259–269. [Google Scholar] [CrossRef]
- Fakler, C.R.; Wu, B.; McMicken, H.W.; Geske, R.S.; Welty, S.E. Molecular mechanisms of lipopolysaccharide induced ICAM-1 expression in A549 cells. Inflamm. Res. 2000, 49, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Guney, N.; Soydinc, H.O.; Derin, D.; Tas, F.; Camlica, H.; Duranyildiz, D.; Yasasever, V.; Topuz, E. Serum levels of intercellular adhesion molecule ICAM-1 and E-selectin in advanced stage non-small cell lung cancer. Med. Oncol. 2008, 25, 194–200. [Google Scholar] [CrossRef]
- Lin, Y.C.; Shun, C.T.; Wu, M.S.; Chen, C.C. A novel anticancer effect of thalidomide: Inhibition of intercellular adhesion molecule-1-mediated cell invasion and metastasis through suppression of nuclear factor-kappaB. Clin. Cancer Res. 2006, 12, 7165–7173. [Google Scholar] [CrossRef] [PubMed]
- Melis, M.; Spatafora, M.; Melodia, A.; Pace, E.; Gjomarkaj, M.; Merendino, A.M.; Bonsignore, G. ICAM-1 expression by lung cancer cell lines: Effects of upregulation by cytokines on the interaction with LAK cells. Eur. Respir. J. 1996, 9, 1831–1888. [Google Scholar] [CrossRef]
- Beck-Schimmer, B.; Schimmer, R.C.; Warner, R.L.; Schmal, H.; Nordblom, G.; Flory, C.M.; Lesch, M.E.; Friedl, H.P.; Schrier, D.J.; Ward, P.A. Expression of lung vascular and airway ICAM-1 after exposure to bacterial lipopolysaccharide. Am. J. Respir. Cell Mol. Biol. 1997, 17, 344–352. [Google Scholar] [CrossRef][Green Version]
- Liu, G.; Place, A.T.; Chen, Z.; Brovkovych, V.M.; Vogel, S.M.; Muller, W.A.; Skidgel, R.A.; Malik, A.B.; Minshall, R.D. ICAM-1-activated Src and eNOS signaling increase endothelial cell surface PECAM-1 adhesivity and neutrophil transmigration. Blood 2012, 120, 1942–1952. [Google Scholar] [CrossRef]
- Wu, Q.D.; Wang, J.H.; Condron, C.; Bouchier-Hayes, D.; Redmond, H.P. Human neutrophils facilitate tumor cell transendothelial migration. Am. J. Physiol. Cell Physiol. 2001, 280, C814–C822. [Google Scholar] [CrossRef]
- Fischer, L.G.; Bremer, M.; Coleman, E.J.; Conrad, B.; Krumm, B.; Gross, A.; Hollmann, M.W.; Mandell, G.; Durieux, M.E. Local anesthetics attenuate lysophosphatidic acid-induced priming in human neutrophils. Anesth. Analg. 2001, 92, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Picardi, S.; Cartellieri, S.; Groves, D.; Hahnenkamp, K.; Gerner, P.; Durieux, M.E.; Stevens, M.F.; Lirk, P.; Hollmann, M.W. Local anesthetic-induced inhibition of human neutrophil priming: The influence of structure, lipophilicity, and charge. Reg. Anesth. Pain Med. 2013, 38, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Hollmann, M.W.; Gross, A.; Jelacin, N.; Durieux, M.E. Local anesthetic effects on priming and activation of human neutrophils. Anesthesiology 2001, 95, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Hollmann, M.W.; Kurz, K.; Herroeder, S.; Struemper, D.; Hahnenkamp, K.; Berkelmans, N.S.; den Bakker, C.G.; Durieux, M.E. The effects of S(−)-, R(+)-, and racemic bupivacaine on lysophosphatidate-induced priming of human neutrophils. Anesth. Analg. 2003, 97, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Chen, L.; Zhao, H.; Wu, L.; Masters, J.; Han, C.; Hirota, K.; Ma, D. Both Bupivacaine and Levobupivacaine inhibit colon cancer cell growth but not melanoma cells in vitro. J. Anesth. 2019, 33, 17–25. [Google Scholar] [CrossRef]
- Piegeler, T.; Votta-Velis, E.G.; Liu, G.; Place, A.T.; Schwartz, D.E.; Beck-Schimmer, B.; Minshall, R.D.; Borgeat, A. Antimetastatic potential of amide-linked local anesthetics: Inhibition of lung adenocarcinoma cell migration and inflammatory Src signaling independent of sodium channel blockade. Anesthesiology 2012, 117, 548–559. [Google Scholar] [CrossRef]
- Baptista-Hon, D.T.; Robertson, F.M.; Robertson, G.B.; Owen, S.J.; Rogers, G.W.; Lydon, E.L.; Lee, N.H.; Hales, T.G. Potent inhibition by ropivacaine of metastatic colon cancer SW620 cell invasion and NaV1.5 channel function. Br. J. Anaesth. 2014, 113 (Suppl. S1), i39–i48. [Google Scholar] [CrossRef]
- Koh, S.Y.; Moon, J.Y.; Unno, T.; Cho, S.K. Baicalein Suppresses Stem Cell-Like Characteristics in Radio- and Chemoresistant MDA-MB-231 Human Breast Cancer Cells through Up-Regulation of IFIT2. Nutrients 2019, 11, 624–643. [Google Scholar] [CrossRef]
- Ye, L.; Zhang, Y.; Chen, Y.J.; Liu, Q. Anti-tumor effects of lidocaine on human gastric cancer cells in vitro. Bratisl. Lek Listy 2019, 120, 212–217. [Google Scholar] [CrossRef]
- Du, J.; Zhang, L.; Ma, H.; Wang, Y.; Wang, P. Lidocaine Suppresses Cell Proliferation and Aerobic Glycolysis by Regulating circHOMER1/miR-138-5p/HEY1 Axis in Colorectal Cancer. Cancer Manag. Res. 2020, 12, 5009–5022. [Google Scholar] [CrossRef]
- House, C.D.; Vaske, C.J.; Schwartz, A.M.; Obias, V.; Frank, B.; Luu, T.; Sarvazyan, N.; Irby, R.; Strausberg, R.L.; Hales, T.G.; et al. Voltage-gated Na+ channel SCN5A is a key regulator of a gene transcriptional network that controls colon cancer invasion. Cancer Res. 2010, 70, 6957–6967. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, M.; Kuroda, Y.; Hirose, M. The antiproliferative effect of lidocaine on human tongue cancer cells with inhibition of the activity of epidermal growth factor receptor. Anesth. Analg. 2006, 102, 1103–1107. [Google Scholar] [CrossRef] [PubMed]
- Xing, W.; Chen, D.T.; Pan, J.H.; Chen, Y.H.; Yan, Y.; Li, Q.; Xue, R.F.; Yuan, Y.F.; Zeng, W.A. Lidocaine Induces Apoptosis and Suppresses Tumor Growth in Human Hepatocellular Carcinoma Cells In Vitro and in a Xenograft Model In Vivo. Anesthesiology 2017, 126, 868–881. [Google Scholar] [CrossRef] [PubMed]
- Lirk, P.; Berger, R.; Hollmann, M.W.; Fiegl, H. Lidocaine time- and dose-dependently demethylates deoxyribonucleic acid in breast cancer cell lines in vitro. Br. J. Anaesth. 2012, 109, 200–207. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, G.; Saporito, A.; Cecchinato, V.; Silvestri, Y.; Borgeat, A.; Anselmi, L.; Uguccioni, M. Lidocaine inhibits cytoskeletal remodelling and human breast cancer cell migration. Br. J. Anaesth. 2018, 121, 962–968. [Google Scholar] [CrossRef]
- Exadaktylos, A.K.; Buggy, D.J.; Moriarty, D.C.; Mascha, E.; Sessler, D.I. Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology 2006, 105, 660–664. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, L.; Zhu, X.; Zhu, M.; Sun, Z.; Cata, J.P.; Chen, W.; Miao, C. Association between intraoperative intravenous lidocaine infusion and survival in patients undergoing pancreatectomy for pancreatic cancer: A retrospective study. Br. J. Anaesth. 2020, 125, 141–148. [Google Scholar] [CrossRef]
- Christopherson, R.; James, K.E.; Tableman, M.; Marshall, P.; Johnson, F.E. Long-term survival after colon cancer surgery: A variation associated with choice of anesthesia. Anesth. Analg. 2008, 107, 325–332. [Google Scholar] [CrossRef]
- De Oliveira, G.S., Jr.; Ahmad, S.; Schink, J.C.; Singh, D.K.; Fitzgerald, P.C.; McCarthy, R.J. Intraoperative neuraxial anesthesia but not postoperative neuraxial analgesia is associated with increased relapse-free survival in ovarian cancer patients after primary cytoreductive surgery. Reg. Anesth. Pain Med. 2011, 36, 271–277. [Google Scholar] [CrossRef]
- Gottschalk, A.; Brodner, G.; Van Aken, H.K.; Ellger, B.; Althaus, S.; Schulze, H.J. Can regional anaesthesia for lymph-node dissection improve the prognosis in malignant melanoma? Br. J. Anaesth. 2012, 109, 253–259. [Google Scholar] [CrossRef][Green Version]
- Karmakar, M.K.; Samy, W.; Lee, A.; Li, J.W.; Chan, W.C.; Chen, P.P.; Tsui, B.C.H. Survival Analysis of Patients with Breast Cancer Undergoing a Modified Radical Mastectomy With or Without a Thoracic Paravertebral Block: A 5-Year Follow-up of a Randomized Controlled Trial. Anticancer Res. 2017, 37, 5813–5820. [Google Scholar] [PubMed]
- Weng, M.; Chen, W.; Hou, W.; Li, L.; Ding, M.; Miao, C. The effect of neuraxial anesthesia on cancer recurrence and survival after cancer surgery: An updated meta-analysis. Oncotarget 2016, 7, 15262–15273. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I.; Pei, L.; Huang, Y.; Fleischmann, E.; Marhofer, P.; Kurz, A.; Mayers, D.B.; Meyer-Treschan, T.A.; Grady, M.; Tan, E.Y.; et al. Breast Cancer Recurrence C: Recurrence of breast cancer after regional or general anaesthesia: A randomised controlled trial. Lancet 2019, 394, 1807–1815. [Google Scholar] [CrossRef]
| Human Studies | ||
|---|---|---|
| Without Surgery | With Surgery | |
| Opioids | ||
| ↑, =, ↓ | =, ↓ |
| ↑, = | =, ↓ |
| = | ? |
| Ketamine | ? | ↑,↓ |
| Propofol | ? | ↑ |
| NSAID | ↑ | ↑ |
| Local anesthetics | ||
| ↑ | ↑ |
| (=) | (=) |
| Inhibition of Src-Kinase/ICAM-1 Phosphorylation | Piegeler et al., 2014, 2012 [42,57] |
| Downregulation of VGSC (Voltage-Gated Sodium Channel) | House et al., 2010 [62] |
| Antiproliferative effects | Sakaguchi et al., 2006 [63] |
| Increase the apoptotic effect | Xing et al., 2017 [64] |
| Increase the demethylation | Lirk et al., 2012 [65] |
| Inhibition of cytoskeletal remodeling | D’Agostino et al., 2018 [66] |
| Potentiation in vitro and in vivo of NK cell activity | Ramirez et al., 2015 [32] Jaura et al., 2014 [33] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borgeat, A.; Aguirre, J. Impact of Local Anesthetics on Cancer Behavior and Outcome during the Perioperative Period: A Review. Medicina 2022, 58, 882. https://doi.org/10.3390/medicina58070882
Borgeat A, Aguirre J. Impact of Local Anesthetics on Cancer Behavior and Outcome during the Perioperative Period: A Review. Medicina. 2022; 58(7):882. https://doi.org/10.3390/medicina58070882
Chicago/Turabian StyleBorgeat, Alain, and José Aguirre. 2022. "Impact of Local Anesthetics on Cancer Behavior and Outcome during the Perioperative Period: A Review" Medicina 58, no. 7: 882. https://doi.org/10.3390/medicina58070882
APA StyleBorgeat, A., & Aguirre, J. (2022). Impact of Local Anesthetics on Cancer Behavior and Outcome during the Perioperative Period: A Review. Medicina, 58(7), 882. https://doi.org/10.3390/medicina58070882





