Risk of Spine Surgery in Patients with Rheumatoid Arthritis: A Secondary Cohort Analysis of a Nationwide, Population-Based Health Claim Database
Abstract
:1. Introduction
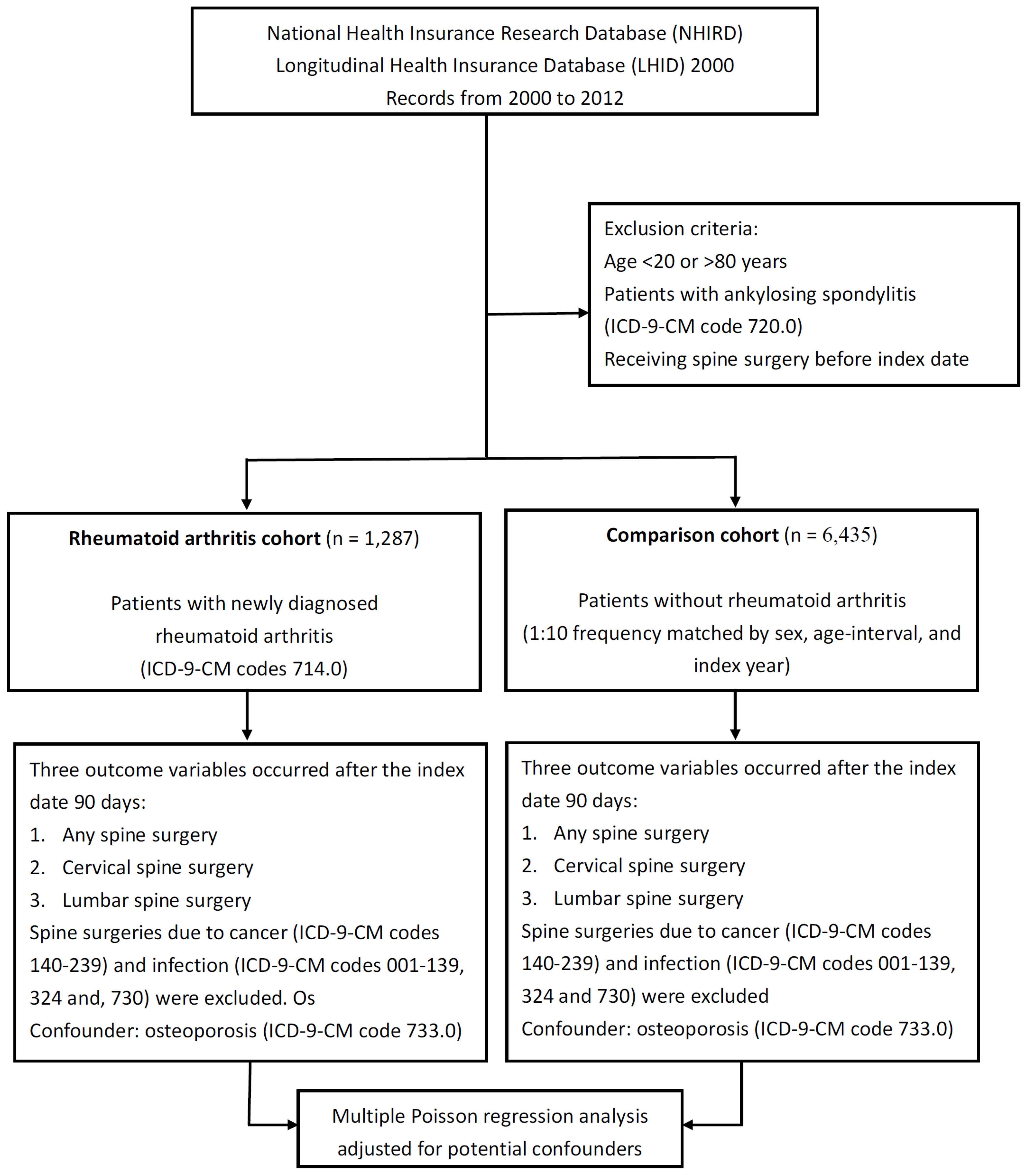
2. Materials and Methods
2.1. Identification of the Rheumatoid Arthritis and Comparison Cohort
2.2. Identification of Cervical and Lumbar Spine Surgery
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scott, D.L.; Wolfe, F.; Huizinga, T.W. Rheumatoid arthritis. Lancet 2010, 376, 1094–1108. [Google Scholar] [CrossRef]
- Lee, D.M.; Weinblatt, M.E. Rheumatoid arthritis. Lancet 2001, 358, 903–911. [Google Scholar] [CrossRef]
- Chou, C.T.; Pei, L.; Chang, D.M.; Lee, C.F.; Schumacher, H.R.; Liang, M.H. Prevalence of rheumatic diseases in Taiwan: A population study of urban, suburban, rural differences. J. Rheumatol. 1994, 21, 302–306. [Google Scholar] [PubMed]
- Kuo, C.F.; Luo, S.F.; See, L.C.; Chou, I.J.; Chang, H.C.; Yu, K.H. Rheumatoid arthritis prevalence, incidence, and mortality rates: A nationwide population study in Taiwan. Rheumatol. Int. 2013, 33, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Nemani, V.M.; Riew, K.D.; Brasington, R. Cervical spine disease in rheumatoid arthritis: Incidence, manifestations, and therapy. Curr. Rheumatol. Rep. 2015, 17, 9. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Tamai, K.; Takahashi, S.; Yamada, K.; Inui, K.; Tada, M.; Okano, T.; Sugioka, Y.; Koike, T.; Nakamura, H. Do rheumatoid arthritis patients have low back pain or radiological lumbar lesions more frequently than the healthy population?—Cross-sectional analysis in a cohort study with age and sex-matched healthy volunteers. Spine J. 2020, 20, 1995–2002. [Google Scholar] [CrossRef] [PubMed]
- Hagege, B.; Tubach, F.; Alfaiate, T.; Forien, M.; Dieudé, P.; Ottaviani, S. Increased rate of lumbar spondylolisthesis in rheumatoid arthritis: A case-control study. Eur. J. Clin. Investig. 2018, 48, e12991. [Google Scholar] [CrossRef] [PubMed]
- Sugimura, Y.; Miyakoshi, N.; Miyamoto, S.; Kasukawa, Y.; Hongo, M.; Shimada, Y. Prevalence of and factors associated with lumbar spondylolisthesis in patients with rheumatoid arthritis. Mod. Rheumatol. 2016, 26, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Suzuki, A.; Takahashi, S.; Yasuda, H.; Tada, M.; Sugioka, Y.; Okano, T.; Koike, T.; Nakamura, H. MRI evaluation of lumbar endplate and facet erosion in rheumatoid arthritis. J. Spinal Disord. Tech. 2014, 27, E128–E135. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.C.; Koo, M.; Lai, N.S. Incident spine surgery in patients with ankylosing spondylitis: A secondary cohort analysis of a nationwide, population-based health claims database. Arthritis Care Res. 2018, 70, 1416–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnett, F.C.; Edworthy, S.M.; Bloch, D.A.; McShane, D.J.; Fries, J.F.; Cooper, N.S.; Healey, L.A.; Kaplan, S.R.; Liang, M.H.; Luthra, H.S.; et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.C.; Hsu, B.B.; Koo, M.; Lai, N.S. Higher risk of incident ankylosing spondylitis in patients with uveitis: A secondary cohort analysis of a nationwide, population-based health claims database. Scand. J. Rheumatol. 2017, 46, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Xu, W.; Luo, Y.; Zhao, Y.; Liu, Y. Cervical spine involvement risk factors in rheumatoid arthritis: A meta-analysis. Int. J. Rheum. Dis. 2017, 20, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Del Grande, M.; Del Grande, F.; Carrino, J.; Bingham, C.O., III; Louie, G.H. Cervical spine involvement early in the course of rheumatoid arthritis. Semin. Arthritis Rheum. 2014, 43, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Joo, P.; Ge, L.; Mesfin, A. Surgical management of the lumbar spine in rheumatoid arthritis. Global Spine J. 2020, 10, 767–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawaguchi, Y.; Matsuno, H.; Kanamori, M.; Ishihara, H.; Ohmori, K.; Kimura, T. Radiologic findings of the lumbar spine in patients with rheumatoid arthritis, and a review of pathologic mechanisms. J. Spinal Disord. Tech. 2003, 16, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.N.; Kim, C.W.; Moon, J.K. The outcomes of instrumented posterolateral lumbar fusion in patients with rheumatoid arthritis. Bone Joint J. 2016, 98, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, S.; Sonne-Holm, S.; Rovsing, H.; Monrad, H.; Gebuhr, P. Degenerative lumbar spondylolisthesis: An epidemiological perspective: The Copenhagen Osteoarthritis Study. Spine 2007, 32, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Akkawi, I.; Zmerly, H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022, 92, e2021313. [Google Scholar] [PubMed]
- Jiang, H.; Yang, Q.; Jiang, J.; Zhan, X.; Xiao, Z. Association between COL11A1 (rs1337185) and ADAMTS5 (rs162509) gene polymorphisms and lumbar spine pathologies in Chinese Han population: An observational study. BMJ Open 2017, 7, e015644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | n (%) | p | |||
|---|---|---|---|---|---|
| RA Cohort 1287 (16.7) | Comparison Cohort 6435 (83.3) | ||||
| Sex | >0.999 | ||||
| male | 273 | (21.2) | 1365 | (21.2) | |
| female | 1014 | (78.8) | 5070 | (78.8) | |
| Age group (years) | >0.999 | ||||
| 20.0–29.9 | 58 | (4.5) | 290 | (4.5) | |
| 30.0–39.9 | 141 | (11.0) | 705 | (11.0) | |
| 40.0–49.9 | 297 | (23.1) | 1485 | (23.1) | |
| 50.0–59.9 | 376 | (29.2) | 1880 | (29.2) | |
| 60.0–69.9 | 235 | (18.3) | 1175 | (18.3) | |
| 70.0–80.0 | 180 | (14.0) | 900 | (14.0) | |
| Mean age (SD), years | 53.4 | (13.4) | 53.4 | (13.4) | 0.959 |
| Mean follow up duration (SD), years | 6.04 | (3.63) | 5.71 | (3.86) | 0.004 |
| Osteoporosis | 132 | (10.3) | 218 | (3.4) | <0.001 |
| Socioeconomic status (n = 7701) | <0.001 | ||||
| low | 595 | (46.6) | 3714 | (57.8) | |
| middle | 456 | (35.7) | 1800 | (28.0) | |
| high | 225 | (17.7) | 911 | (14.2) | |
| Geographic region (n = 7462) | 0.455 | ||||
| northern | 723 | (58.4) | 3740 | (60.1) | |
| central | 226 | (18.2) | 1030 | (16.6) | |
| southern | 262 | (21.1) | 1328 | (21.3) | |
| eastern | 28 | (2.3) | 125 | (2.0) | |
| Outcome Variable | RA Cohort (n = 1287) | Comparison Cohort (n = 6435) | IRR (95% CI) | Adjusted IRR * (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| No. of Patient | Person-Years | IR | No. of Patient | Person-Years | IR | p | p | |
| Spine surgery | ||||||||
| total | 50 | 7572 | 6.60 | 97 | 35,821 | 2.71 | 2.44 (1.73–3.43) <0.001 | 2.13 (1.49–3.04) <0.001 |
| male | 5 | 1531 | 3.27 | 23 | 7541 | 3.05 | 1.07 (0.41–2.82) 0.890 | 1.03 (0.38–2.81) 0.950 |
| female | 45 | 6041 | 7.45 | 74 | 28,280 | 2.62 | 2.85 (1.96–4.12) <0.001 | 2.43 (1.65–3.58) <0.001 |
| Cervical | ||||||||
| total | 7 | 7572 | 0.92 | 16 | 35,821 | 0.45 | 2.07 (0.85–5.03) 0.108 | 1.79 (0.68–4.71) 0.238 |
| male | 1 | 1531 | 0.65 | 7 | 7541 | 0.93 | 0.70 (0.09–5.72) 0.742 | 0.89 (0.11–7.44) 0.915 |
| female | 6 | 6041 | 0.99 | 9 | 28,280 | 0.32 | 3.12 (1.11–8.77) 0.031 | 2.27 (0.74–6.98) 0.153 |
| Lumbar | ||||||||
| total | 42 | 7572 | 5.55 | 82 | 35,821 | 2.29 | 2.42 (1.67–3.52) <0.001 | 2.14 (1.46–3.15) <0.001 |
| male | 4 | 1531 | 2.61 | 18 | 7541 | 2.39 | 1.10 (0.37–3.24) 0.870 | 0.99 (0.32–3.05) 0.989 |
| female | 38 | 6041 | 6.29 | 64 | 28,280 | 2.26 | 2.78 (1.86–4.15) <0.001 | 2.44 (1.61–3.69) <0.001 |
| Outcome Variable | RA Cohort (n = 1287) | Comparison Cohort (n = 6435) | IRR (95% CI) | Adjusted IRR * (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| No. of Patient | Person-Years | IR | No. of Patient | Person-Years | IR | p | p | |
| Spine surgery | ||||||||
| Age group, years | ||||||||
| 20–44.9 | 7 | 2050 | 3.41 | 4 | 9827 | 0.41 | 8.39 (2.46–28.66) 0.001 | 5.73 (1.55–21.21) 0.009 |
| 45–59.9 | 20 | 3362 | 5.95 | 43 | 15,938 | 2.70 | 2.20 (1.30–3.75) 0.003 | 2.22 (1.29–3.84) 0.004 |
| 60–80.0 | 23 | 2160 | 10.65 | 50 | 10,056 | 4.97 | 2.14 (1.31–3.51) 0.003 | 1.78 (1.06–2.98) 0.029 |
| Cervical | ||||||||
| Age group, years | ||||||||
| 20–44.9 | 4 | 2050 | 1.95 | 1 | 9827 | 0.10 | 19.17 (2.14–171.55) 0.008 | 8.98 (0.84–96.26) 0.070 |
| 45–59.9 | 2 | 3362 | 0.59 | 6 | 15,938 | 0.38 | 1.58 (0.32–7.83) 0.575 | 2.07 (0.40–10.70) 0.387 |
| 60–80.0 | 1 | 2160 | 0.46 | 9 | 10,056 | 0.89 | 0.52 (0.07–4.08) 0.532 | 0.50 (0.06–4.07) 0.516 |
| Lumbar | ||||||||
| Age group, years | ||||||||
| 20–44.9 | 3 | 2050 | 1.46 | 3 | 9827 | 0.31 | 4.79 (0.97–23.75) 0.055 | 4.58 (0.91–23.13) 0.066 |
| 45–59.9 | 18 | 3362 | 5.35 | 37 | 15,938 | 2.32 | 2.31 (1.31–4.05) 0.004 | 2.32 (1.30–4.13) 0.004 |
| 60–80.0 | 21 | 2160 | 9.72 | 42 | 10,056 | 4.18 | 2.33 (1.38–3.93) 0.002 | 1.90 (1.10–3.29) 0.022 |
| Overall Spine Surgery | Lumbar Spine Surgery | |||
|---|---|---|---|---|
| Variable | aIRR * (95% CI) | p | aIRR * (95% CI) | p |
| Sex (female/male) | ||||
| male | Ref | Ref | ||
| female | 2.16 (0.85–5.51) | 0.107 | 2.27 (0.80–6.45) | 0.123 |
| Age group (years) | ||||
| 20–44.9 | Ref | Ref | ||
| 45–59.9 | 1.85 (0.74–4.63) | 0.192 | 3.23 (0.94–11.05) | 0.062 |
| 60–80 | 3.06 (1.22–7.69) | 0.018 | 5.36 (1.56–18.40) | 0.008 |
| Osteoporosis | ||||
| No | Ref | |||
| Yes | 2.34 (1.25–4.38) | 0.008 | 2.80 (1.46–5.36) | 0.002 |
| Socioeconomic status | ||||
| low | Ref | Ref | ||
| Middle and high | 1.07 (0.60–1.91) | 0.816 | 1.07 (0.57–2.00) | 0.836 |
| Geographic region | ||||
| northern | Ref | Ref | ||
| central, southern, and eastern | 1.13 (0.64–2.00) | 0.678 | 0.97 (0.52–1.80) | 0.916 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-H.; Hsu, C.-W.; Lu, M.-C. Risk of Spine Surgery in Patients with Rheumatoid Arthritis: A Secondary Cohort Analysis of a Nationwide, Population-Based Health Claim Database. Medicina 2022, 58, 777. https://doi.org/10.3390/medicina58060777
Chen C-H, Hsu C-W, Lu M-C. Risk of Spine Surgery in Patients with Rheumatoid Arthritis: A Secondary Cohort Analysis of a Nationwide, Population-Based Health Claim Database. Medicina. 2022; 58(6):777. https://doi.org/10.3390/medicina58060777
Chicago/Turabian StyleChen, Chien-Han, Chia-Wen Hsu, and Ming-Chi Lu. 2022. "Risk of Spine Surgery in Patients with Rheumatoid Arthritis: A Secondary Cohort Analysis of a Nationwide, Population-Based Health Claim Database" Medicina 58, no. 6: 777. https://doi.org/10.3390/medicina58060777
APA StyleChen, C.-H., Hsu, C.-W., & Lu, M.-C. (2022). Risk of Spine Surgery in Patients with Rheumatoid Arthritis: A Secondary Cohort Analysis of a Nationwide, Population-Based Health Claim Database. Medicina, 58(6), 777. https://doi.org/10.3390/medicina58060777







