Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis
Abstract
:1. Introduction
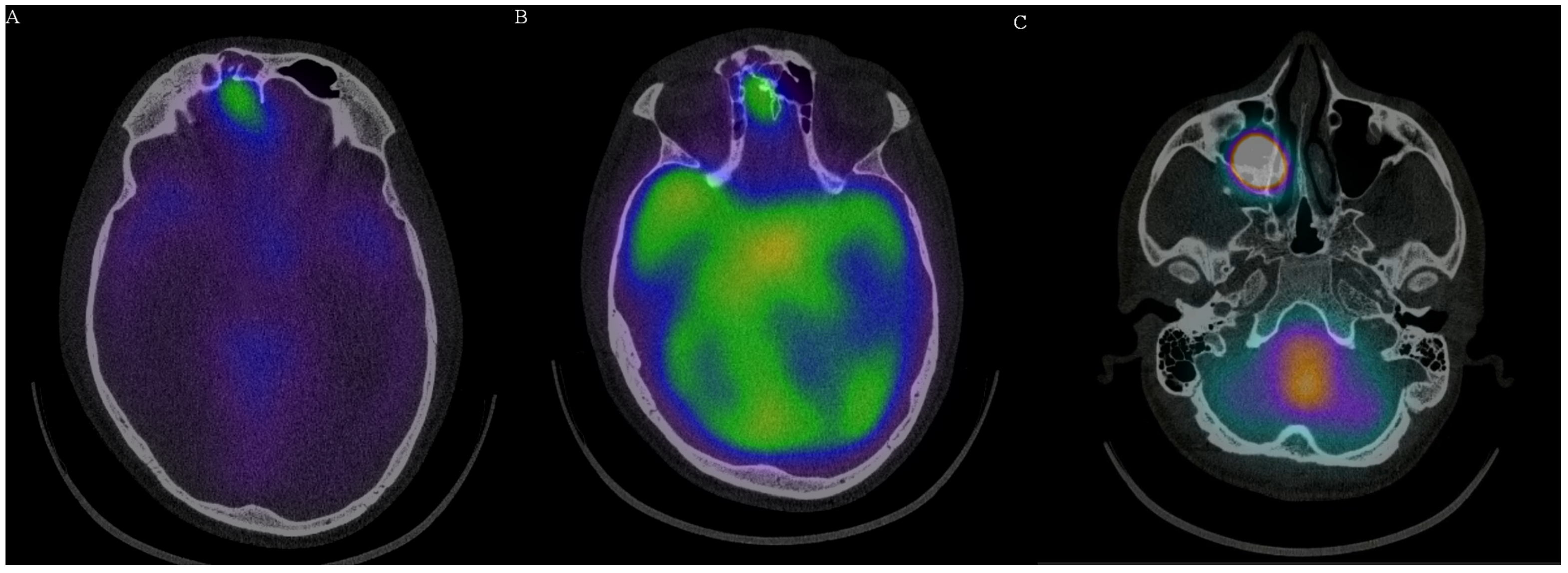
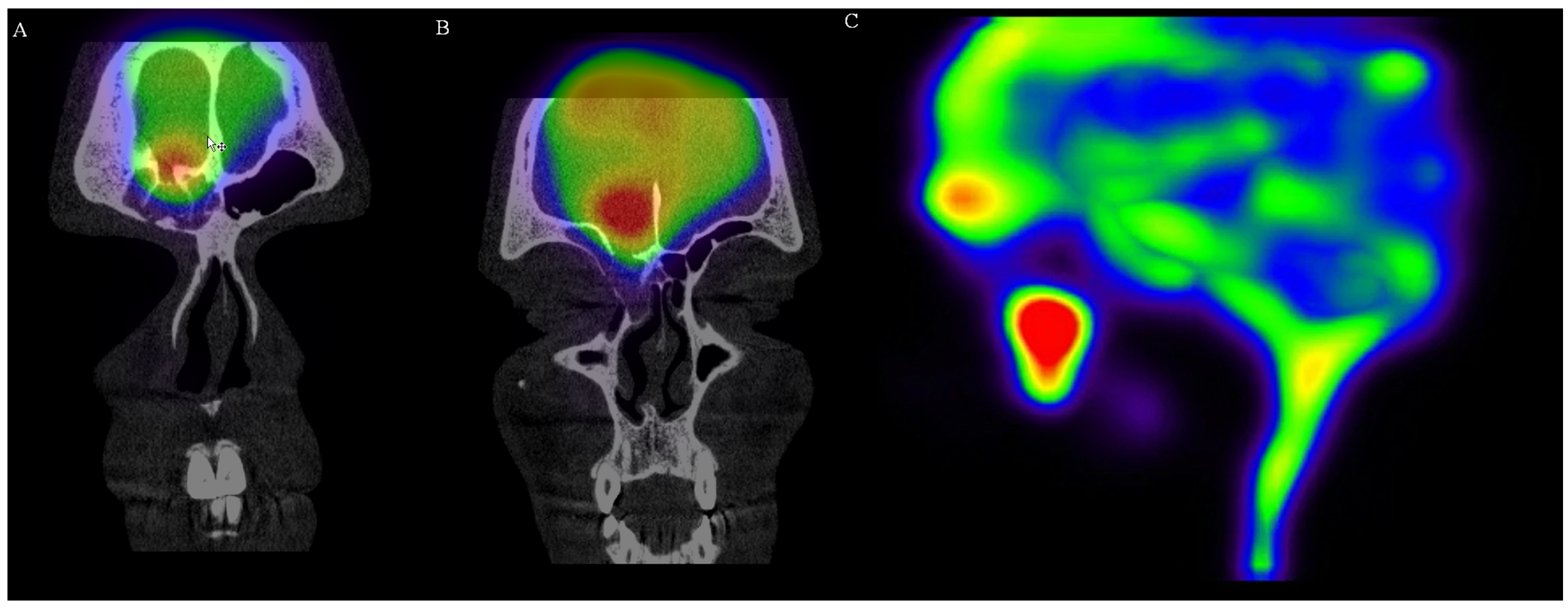
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oakley, G.M.; Alt, J.A.; Schlosser, R.J.; Harvey, R.J.; Orlandi, R.R. Diagnosis of cerebrospinal fluid rhinorrhea: An evidence-based review with recommendations. Int. Forum Allergy Rhinol. 2016, 6, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Eljamel, M.S.; Foy, P.M. Acute traumatic CSF fistulae: The risk of intracranial infection. Br. J. Neurosurg. 1990, 4, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Atyani, A.; Salameh, J.P.; McInnes, M.; Chakraborty, S. Safety of Intrathecal Administration of Gadolinium-based Contrast Agents: A Systematic Review and Meta-Analysis. Radiology 2020, 297, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Ter Horst, L.; Brouwer, M.C.; van der Ende, A.; van de Beek, D. Community-acquired Bacterial Meningitis in Adults with Cerebrospinal Fluid Leakage. Clin. Infect Dis. 2020, 70, 2256–2261. [Google Scholar] [CrossRef] [Green Version]
- Van der Linden, M.; Perniciaro, S.; Imöhl, M. Increase of serotypes 15A and 23B in IPD in Germany in the PCV13 vaccination era. BMC Infect Dis. 2015, 15, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aydin, K.; Terzibasioglu, E.; Sencer, S.; Sencer, A.; Suoglu, Y.; Karasu, A.; Kiris, T.; Turantan, M.I. Localization of cerebrospinal fluid leaks by gadolinium-enhanced magnetic resonance cisternography: A 5-year single-center experience. Neurosurgery 2008, 62, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Zhou, K.; Kachra, S.; McHugh, T.; Sommer, D.D. Diagnosis and Localization of Cerebrospinal Fluid Rhinorrhea: A Systematic Review. Am. J. Rhinol. Allergy 2021, 36, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Eljamel, M.S.; Pidgeon, C.N.; Toland, J.; Phillips, J.B.; O’Dwyer, A.A. MRI cisternography, and the localization of CSF fistulae. Br. J. Neurosurg. 1994, 8, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Algin, O.; Hakyemez, B.; Gokalp, G.; Ozcan, T.; Korfali, E.; Parlak, M. The contribution of 3D-CISS and contrast-enhanced MR cisternography in detecting cerebrospinal fluid leak in patients with rhinorrhoea. Br. J. Radiol. 2010, 83, 225–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dichiro, G. Movement of the cerebrospinal fluid in human beings. Nature 1964, 204, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Wolfstein, R.S.; Tanasescu, D.; Sakimura, I.T.; Waxman, A.D.; Siemsen, J.K. Brain imaging with 99mTc-DTPA: A clinical comparison of early and delayed studies. J. Nucl. Med. 1974, 15, 1135–1137. [Google Scholar] [PubMed]
- Hnatowich, D.J. Recent developments in the radiolabeling of antibodies with iodine, indium, and technetium. Semin. Nucl. Med. 1990, 20, 80–91. [Google Scholar] [CrossRef]
- Bova, D.; Boles, M.A. Cerebrospinal fluid imaging. In Nuclear Medicine; Henkin, R.E., Bova, D., Dillehay, G.L., Karesh, S.M., Halama, J.R., Wagner, R.H., Eds.; Mosby: Philadelphia, PA, USA, 2006. [Google Scholar]
- Tins, B. Technical aspects of CT imaging of the spine. Insights Imaging 2010, 1, 349–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, D.L.; Menda, Y.; Graham, M.M. Radionuclide cisternography in detecting cerebrospinal fluid leak in spontaneous intracranial hypotension: A series of four case reports. Clin. Nucl. Med. 2009, 34, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, H.; Higuchi, T.; Achmad, A.; Taketomi-Takahashi, A.; Fujimaki, H.; Tsushima, Y. A new approach for simple radioisotope cisternography examination in cerebrospinal fluid leakage detection. Ann. Nucl. Med. 2016, 30, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, K.; Nishio, M.; Sasaki, S.; Ogino, H.; Tohyama, J.; Yamada, K.; Shibamoto, Y. Postpuncture CSF leakage: A potential pitfall of radionuclide cisternography. Neurology 2010, 75, 1730–1734. [Google Scholar] [CrossRef] [PubMed]
- Halac, M.; Albayram, S.; Ceyhan, E.; Ozer, H.; Doǧan, I.; Sager, S.; Uslu, I. Is early bladder activity in radionuclide cisternography anindirect sign of spontaneous intracranial hypotension or sequence of lumbar puncture? Clin. Nucl. Med. 2007, 32, 850–853. [Google Scholar] [CrossRef] [PubMed]


| Variable | Reference Range, Adults | On Admission | Follow-Up * |
|---|---|---|---|
| Hematocrit (%) | 36–46 | 47 | 41 |
| Hemoglobin (g/dL) | 12–16 | 15.9 | 14.1 |
| White cell count (×109/L) | 4.0–10 | 26 | 13 |
| Differential count (×109/L) | |||
| Neutrophils | 1.4–6.5 | 24.12 | 11.39 |
| Lymphocytes | 1.5–4.0 | 0.67 | 0.8 |
| Monocytes | 0.25–0.6 | 1.1 | 1.02 |
| Eosinophils | 0.05–0.25 | 0.03 | 0.0 |
| Platelet count (×109/L) | 150–400 | 238 | 274 |
| Prothrombin–time international normalized ratio | 0.85–1.15 | 1.19 | 1.07 |
| Fibrinogen (g/L) | 1.8–3.5 | 10.4 | 1.9 |
| C-reactive protein (mg/L) | <5 | 391 | 8.45 |
| Urea (mmol/L) | 2.8–7.2 | 6.86 | 5.37 |
| Creatinine (mmol/L) | 49–90 | 91.6 | 82 |
| Aspartate aminotransferase (µkat/L) | 0.05–0.6 | 0.47 | 0.27 |
| Alanine aminotransferase (µkat/L) | 0.05–0.6 | 0.26 | 0.36 |
| Gamma glutamyl transpeptidase (µkat/L) | 0.05–0.63 | 0.30 | 0.28 |
| Alkaline phosphatase (µkat/L) | 0.5–2 | 1.32 | 1.09 |
| Procalcitonin (µg/L) | <0.5 | 25.2 | 0.1 |
| Lactate (mmol/L) | 0.5–2.2 | 2.6 | 1.7 |
| Urine culture | - | negative | - |
| Blood culture | - | negative | - |
| CSF culture | - | Streptococcus pneumoniae | negative |
| CSF Latex agglutination Streptococcus pneumoniae | - | positive | negative |
| CSF neutrophils (/mm3) | 0–10 | >5000 | 13 |
| CSF protein level (g/L) | <0.5 | 3.86 | 0.56 |
| CSF glucose level (mmol/L) | 2.5–4.4 | 1.75 | 3.2 |
| CSF chloride level (mmol/L) | 116–127 | 120 | 122 |
| CSF lactate (mmol/L) | 1.1–2.4 | 10.1 | 1.68 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porubcin, S.; Rovnakova, A.; Zahornacky, O.; Jarcuska, P. Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis. Medicina 2022, 58, 714. https://doi.org/10.3390/medicina58060714
Porubcin S, Rovnakova A, Zahornacky O, Jarcuska P. Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis. Medicina. 2022; 58(6):714. https://doi.org/10.3390/medicina58060714
Chicago/Turabian StylePorubcin, Stefan, Alena Rovnakova, Ondrej Zahornacky, and Pavol Jarcuska. 2022. "Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis" Medicina 58, no. 6: 714. https://doi.org/10.3390/medicina58060714
APA StylePorubcin, S., Rovnakova, A., Zahornacky, O., & Jarcuska, P. (2022). Diagnostic Value of Radioisotope Cisternography Using 111In-DTPA in a Patient with Rhinorrhea and Purulent Meningitis. Medicina, 58(6), 714. https://doi.org/10.3390/medicina58060714






