Post-Operative Results of ACL Reconstruction Techniques on Single-Leg Hop Tests in Athletes: Hamstring Autograft vs. Hamstring Grafts Fixed Using Adjustable Cortical Suspension in Both the Femur and Tibia
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
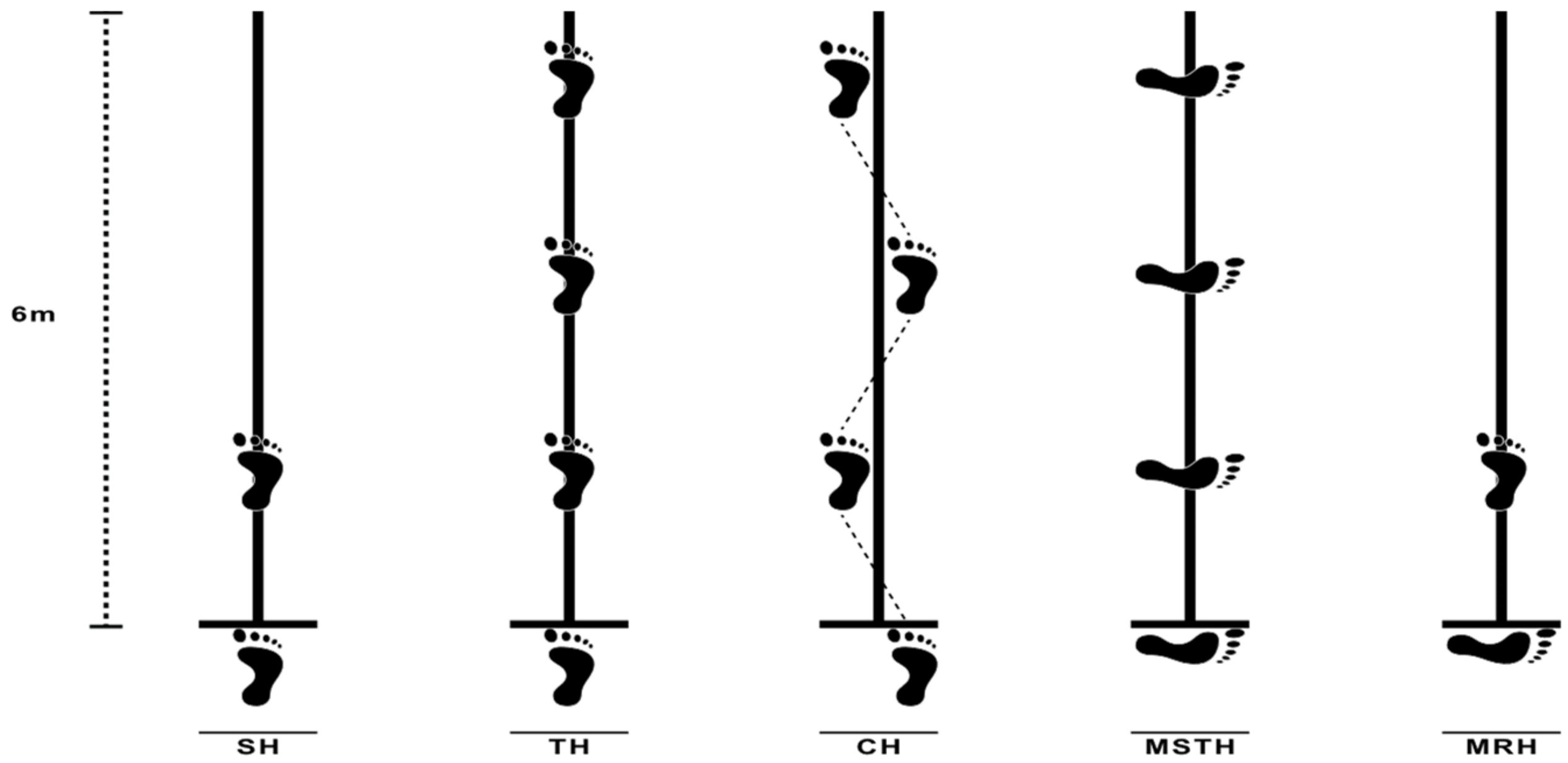
2.2. Procedures
2.3. Statistical Analysis
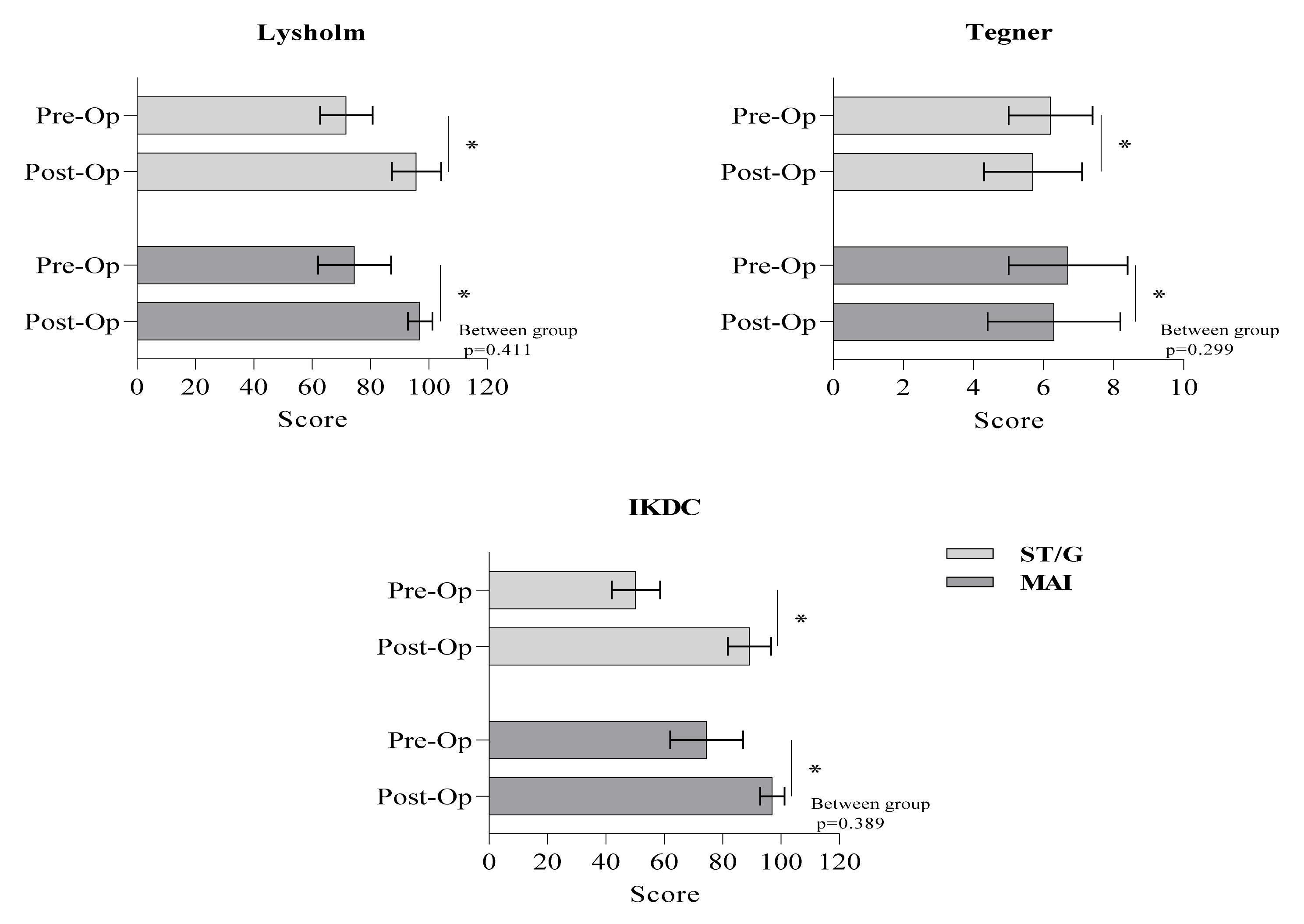
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olsson, O.; Isacsson, A.; Englund, M.; Frobell, R.B. Epidemiology of intra- and peri-articular structural injuries in traumatic knee joint hemarthrosis—Data from 1145 consecutive knees with subacute MRI. Osteoarthr. Cartil. 2016, 24, 1890–1897. [Google Scholar] [CrossRef] [PubMed]
- Roger, J.; Bertani, A.; Vigouroux, F.; Mottier, F.; Gaillard, R.; Have, L.; Rongièras, F. ACL reconstruction using a quadruple semitendinosus graft with cortical fixations gives suitable isokinetic and clinical outcomes after 2 years. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2468–2477. [Google Scholar] [CrossRef]
- Nordenvall, R.; Bahmanyar, S.; Adami, J.; Stenros, C.; Wredmark, T.; Felländer-Tsai, L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: Incidence, treatment, and sex differences. Am. J. Sports Med. 2012, 40, 1808–1813. [Google Scholar] [CrossRef] [PubMed]
- Middleton, K.K.; Hamilton, T.; Irrgang, J.J.; Karlsson, J.; Harner, C.D.; Fu, F.H. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1467–1482. [Google Scholar] [CrossRef]
- Streich, N.A.; Reichenbacher, S.; Barié, A.; Buchner, M.; Schmitt, H. Long-term outcome of anterior cruciate ligament reconstruction with an autologous four-strand semitendinosus tendon autograft. Int. Orthop. 2013, 37, 279–284. [Google Scholar] [CrossRef]
- Petre, B.M.; Smith, S.D.; Jansson, K.S.; de Meijer, P.P.; Hackett, T.R.; LaPrade, R.F.; Wijdicks, C.A. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: A comparative biomechanical study. Am. J. Sports Med. 2013, 41, 416–422. [Google Scholar] [CrossRef]
- Saccomanno, M.F.; Shin, J.J.; Mascarenhas, R.; Haro, M.; Verma, N.N.; Cole, B.J.; Bach, B.R., Jr. Clinical and functional outcomes after anterior cruciate ligament reconstruction using cortical button fixation versus transfemoral suspensory fixation: A systematic review of randomized controlled trials. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 1491–1498. [Google Scholar] [CrossRef]
- Lubowitz, J.H.; Amhad, C.H.; Anderson, K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 717–727. [Google Scholar] [CrossRef] [PubMed]
- Kouloumentas, P.; Kavroudakis, E.; Charalampidis, E.; Kavroudakis, D.; Triantafyllopoulos, G.K. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3592–3598. [Google Scholar] [CrossRef]
- Volpi, P.; Bait, C.; Cervellin, M.; Prospero, E.; Morenghi, E.; Quaglia, A. No difference at two years between all inside transtibial technique and traditional transtibial technique in anterior cruciate ligament reconstruction. Muscle Ligaments Tendons J. 2014, 4, 95–99. [Google Scholar] [CrossRef]
- Pasquali, M.; Plante, M.J.; Monchik, K.O.; Spenciner, D.B. A comparison of three adjustable cortical button ACL fixation devices. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1613–1616. [Google Scholar] [CrossRef] [PubMed]
- Dingenen, B.; Truijen, J.; Bellemans, J.; Gokeler, A. Test–retest reliability and discriminative ability of forward, medial and rotational single-leg hop tests. Knee 2019, 26, 978–987. [Google Scholar] [CrossRef]
- Putnis, S.; Neri, T.; Grasso, S.; Linklater, J.; Fritsch, B.; Parker, D. ACL hamstring grafts fixed using adjustable cortical suspension in both the femur and tibia demonstrate healing and integration on MRI at one year. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 906–914. [Google Scholar] [CrossRef]
- Cournapeau, J.; Klouche, S.; Hardy, P. Material costs of anterior cruciate ligament reconstruction with hamstring tendons by two different techniques. Orthop. Traumatol. Surg Res. 2013, 99, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, E.J.; McDonough, S.M.; Bleakley, C.; Baxter, D.; Cook, C.E. Clinician-friendly lower extremity physical performance tests in athletes: A systematic review of measurement properties and correlation with injury. Part 2—The tests for the hip, thigh, foot and ankle including the star excursion balance test. Br. J. Sports Med. 2015, 49, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Logerstedt, D.S.; Scalzitti, D.; Risberg, M.A.; Engebretsen, L.; Webster, K.E.; Feller, J.; Zachazewski, J. Knee Stability and Movement Coordination Impairments: Knee Ligament Sprain Revision 2017: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A47. [Google Scholar]
- Dingenen, B.; Gokeler, A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: A critical step back to move forward. Sports Med. 2017, 47, 1487–1500. [Google Scholar] [CrossRef]
- Abrams, G.D.; Harris, J.D.; Gupta, A.K.; McCormick, F.M.; Bush-Joseph, C.A.; Verma, N.N.; Bach, B.R., Jr. Functional performance testing after anterior cruciate ligament reconstruction: A systematic review. Orthop. J. Sports Med. 2014, 2, 13–18. [Google Scholar] [CrossRef]
- Rosen, A.B.; Needle, A.R.; Ko, J. Ability of functional performance tests to identify individuals with chronic ankle instability: A systematic review with meta-analysis. Clin. J. Sport Med. 2019, 29, 509–522. [Google Scholar] [CrossRef]
- Harrison, J.J.; Yorgey, M.K.; Csiernik, A.J.; Vogler, J.H.; Games, K.E. Clinician-friendly physical performance tests for the knee. J. Athl. Train. 2017, 52, 1068–1069. [Google Scholar] [CrossRef]
- Gokeler, A.; Welling, W.; Zaffagnini, S.; Seil, R.; Padua, D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Lysholm, J.; Gillquist, J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am. J. Sports Med. 1982, 10, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Tegner, Y.; Lysholm, J. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985, 198, 43–49. [Google Scholar] [CrossRef]
- Irrgang, J.J.; Anderson, A.F.; Boland, A.L.; Harner, C.D.; Kurosaka, M.; Neyret, P.; Richmond, J.C.; Shelborne, K.D. Development and validation of the international knee documentation committee subjective knee form. Am. J. Sports Med. 2001, 29, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Reid, A.; Birmingham, T.B.; Stratford, P.W.; Alcock, G.K.; Giffin, J.R. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys. Ther. 2007, 87, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Kivlan, B.R.; Carcia, C.R.; Clemente, F.R.; Phelps, A.L.; Martin, R.L. Reliability and validity of functional performance tests in dancers with hip dysfunction. Int. J. Sports Phys. Ther. 2013, 8, 360. [Google Scholar] [PubMed]
- Acar, K.; Yilmaz, A.K. Functional dimorphism and relationship between different lower extremity strength tests in young elite judokas. Rev. Artes Marciales Asiáticas 2021, 16, 56–66. [Google Scholar]
- Munro, A.G.; Herrington, L.C. Between-session reliability of four hop tests and the agility t-test. J. Strength Cond. Res. 2011, 25, 1470–1477. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Maccagnano, G.; Barletta, F.; Ascatigno, L.; Astuto, L.; Panella, A.; Moretti, B. Returning to sport after anterior cruciate ligament reconstruction in amateur sports men: A retrospective study. Muscles Ligament Tendons J. 2016, 6, 486. [Google Scholar] [CrossRef]
- Barfod, K.W.; Feller, J.A.; Hartwig, T.; Devitt, B.M.; Webster, K.E. Knee extensor strength and hop test performance following anterior cruciate ligament reconstruction. Knee 2019, 26, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Herrington, L.; Ghulam, H.; Comfort, P. Quadriceps strength and functional performance after anterior cruciate ligament reconstruction in professional soccer players at time of return to sport. J. Strength Cond. Res. 2021, 35, 769–775. [Google Scholar] [CrossRef]
- Augustsson, J.; Thomeé, R.; Karlsson, J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2004, 12, 350–356. [Google Scholar] [CrossRef]
- Hardesty, K.; Hegedus, E.J.; Ford, K.R.; Nguyen, A.D.; Taylor, J.B. Determination of clinically relevant differences in frontal plane hop tests in women’s collegiate basketball and soccer players. Int. J. Sports Phys. Ther. 2017, 12, 182. [Google Scholar]
- Sinsurin, K.; Vachalathiti, R.; Jalayondeja, W.; Limroongreungrat, W. Different sagittal angles and moments of lower extremity joints during single-leg jump landing among various directions in basketball and volleyball athletes. J. Phys. Ther. 2013, 25, 1109–1113. [Google Scholar] [CrossRef]
- Taylor, J.B.; Ford, K.R.; Nguyen, A.D.; Shultz, S.J. Biomechanical comparison of single-and double-leg jump landings in the sagittal and frontal plane. Orthop. J. Sports Med. 2016, 4, 16–18. [Google Scholar] [CrossRef]
- Liu, K.; Heise, G.D. The effect of jump-landing directions on dynamic stability. J. Appl. Biomech. 2013, 29, 634–638. [Google Scholar] [CrossRef]
- Powers, C.M. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J. Orthop. Sports Phys. Ther. 2010, 40, 42–51. [Google Scholar] [CrossRef]

| ST/G (23) | MAI (16) | Total (39) | |
|---|---|---|---|
| Age (years) | 24.7 ± 5.4 | 27.6 ± 7.9 | 25.8 ± 6.6 |
| Weight (kg) | 78.3 ± 9 | 81.5 ± 14.1 | 79.6 ± 11.3 |
| Height (cm) | 179 ± 4.7 | 177.6 ± 5 | 178.4 ± 4.8 |
| BMI (kg/m2) | 24.4 ± 2.5 | 25.8 ± 3.8 | 25 ± 3.1 |
| RTS (months) | 6.7 ± 0.9 | 6.8 ± 1.1 | 6.7 ± 1 |
| ST/G (23) | MAI (16) | t | p-Values | |
|---|---|---|---|---|
| SH | 96.6 ± 8 | 97 ± 7.3 | 0.147 | 0.884 |
| TH | 98.5 ± 7.1 | 98.3 ± 6.1 | −0.079 | 0.938 |
| CH | 100.4 ± 6.7 | 99.6 ± 8.4 | −0.035 | 0.732 |
| MSTH | 98.3 ± 6.8 | 99.2 ± 7.6 | 0.405 | 0.688 |
| MRH | 98.4 ± 6.5 | 99.2 ± 7.7 | 0.371 | 0.712 |
| p-values | 0.314 | 0.786 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kehribar, L.; Yılmaz, A.K.; Karaduman, E.; Kabadayı, M.; Bostancı, Ö.; Sürücü, S.; Aydın, M.; Mahiroğulları, M. Post-Operative Results of ACL Reconstruction Techniques on Single-Leg Hop Tests in Athletes: Hamstring Autograft vs. Hamstring Grafts Fixed Using Adjustable Cortical Suspension in Both the Femur and Tibia. Medicina 2022, 58, 435. https://doi.org/10.3390/medicina58030435
Kehribar L, Yılmaz AK, Karaduman E, Kabadayı M, Bostancı Ö, Sürücü S, Aydın M, Mahiroğulları M. Post-Operative Results of ACL Reconstruction Techniques on Single-Leg Hop Tests in Athletes: Hamstring Autograft vs. Hamstring Grafts Fixed Using Adjustable Cortical Suspension in Both the Femur and Tibia. Medicina. 2022; 58(3):435. https://doi.org/10.3390/medicina58030435
Chicago/Turabian StyleKehribar, Lokman, Ali Kerim Yılmaz, Emre Karaduman, Menderes Kabadayı, Özgür Bostancı, Serkan Sürücü, Mahmud Aydın, and Mahir Mahiroğulları. 2022. "Post-Operative Results of ACL Reconstruction Techniques on Single-Leg Hop Tests in Athletes: Hamstring Autograft vs. Hamstring Grafts Fixed Using Adjustable Cortical Suspension in Both the Femur and Tibia" Medicina 58, no. 3: 435. https://doi.org/10.3390/medicina58030435
APA StyleKehribar, L., Yılmaz, A. K., Karaduman, E., Kabadayı, M., Bostancı, Ö., Sürücü, S., Aydın, M., & Mahiroğulları, M. (2022). Post-Operative Results of ACL Reconstruction Techniques on Single-Leg Hop Tests in Athletes: Hamstring Autograft vs. Hamstring Grafts Fixed Using Adjustable Cortical Suspension in Both the Femur and Tibia. Medicina, 58(3), 435. https://doi.org/10.3390/medicina58030435







