Title Cross-Sectional Study to Evaluate Knowledge and Attitudes on Oral Hygiene of Romanian Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Sample
2.3. Study Instrument Development and Validation
2.4. Questionnaire Contents
2.5. Assessment of the Oral Hygiene Knowledge and Attitudes
2.6. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Criteria for Choosing Toothbrush and Toothpaste
3.3. The Attitude towards the Amount of Toothpaste Used, the Frequency of Toothbrushing Use
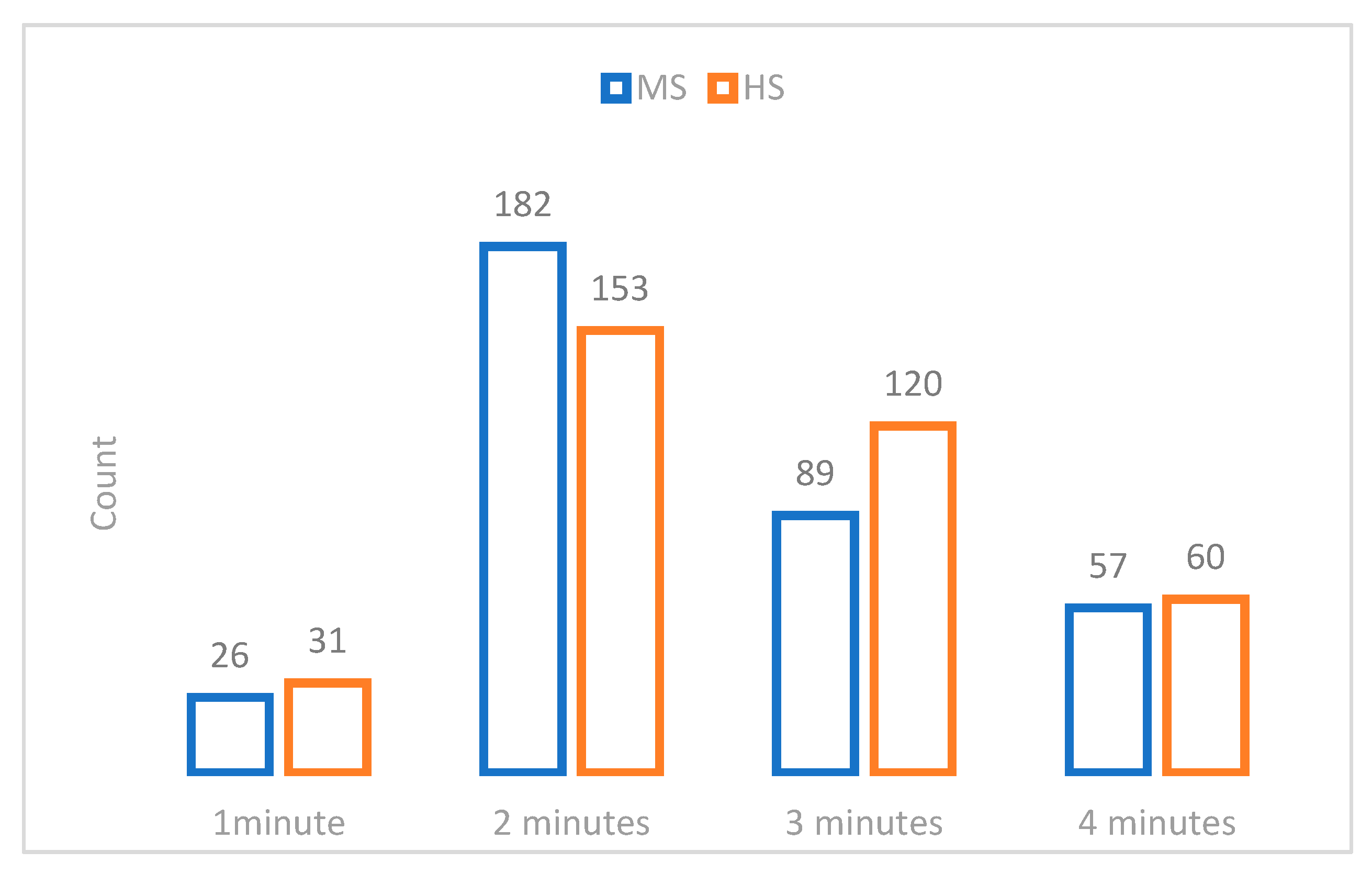
3.4. The Attitude towards the Time of Toothbrushing
3.5. The Attitude towards the Mouthwash and Dental Floss
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Hiiri, A.; Nordblad, A.; Mäkelä, M.; Worthington, H.V. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst. Rev. 2013, 3, CD001830. [Google Scholar] [CrossRef]
- Dye, B.A.; Li, X.; Beltran-Aguilar, E.D. Selected oral health indicators in the United States, 2005–2008. NCHS Data Brief. 2012, 27, 1–8. [Google Scholar]
- Marinho, V.C.; Higgins, J.P.; Sheiham, A.; Logan, S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2003, 1, CD002278. [Google Scholar] [CrossRef] [PubMed]
- Marinho, V.C.; Worthington, H.V.; Walsh, T.; Clarkson, J.E. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2013, 7, CD002279. [Google Scholar] [CrossRef]
- Kappenberg-Nitescu, D.C.; Luchian, I.; Martu, I.; Solomon, S.M.; Martu, S.; Pasarin, L.; Marțu, A.; Sioustis, I.A.; Goriuc, A.; Tatarciuc, M. Periodontal effects of two innovative oral rinsing substances in oncologic patients. Exp. Ther. Med. 2021, 21, 98. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2019; pp. 4–8.
- Dye, B.A.; Tan, S.; Smith, V.; Lewis, B.G.; Barker, L.K.; Thornton-Evans, G.; Eke, P.I.; Beltrán-Aguilar, E.D.; Horowitz, A.M.; Li, C.H. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital and Health Statistic. Series 11, Data from the National Health Survey; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2007; Volume 248, pp. 1–92.
- Eke, P.I.; Thornton-Evans, G.O.; Wei, L.; Borgnakke, W.S.; Dye, B.A.; Genco, R.J. Periodontitis in US Adults: National Health and Nutrition Examination Survey 2009–2014. J. Am. Dent. Assoc. 2018, 149, 576–588.e6. [Google Scholar] [CrossRef] [PubMed]
- Griffin, S.O.; Barker, L.K.; Griffin, P.M.; Cleveland, J.L.; Kohn, W. Oral health needs among adults in the United States with chronic diseases. J. Am. Dent. Assoc. 2009, 140, 1266–1274. [Google Scholar] [CrossRef]
- Kumar, S.; Tadakamadla, J.; Kroon, J.; Johnson, N.W. Impact of parent-related factors on dental caries in the permanent dentition of 6–12-year-old children: A systematic review. J. Dent. 2016, 46, 1–11. [Google Scholar] [CrossRef]
- National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. (N.D.) SEER Stat Fact Sheets: Oral Cavity and Pharynx Cancer website. Available online: http://seer.cancer.gov/statfacts/html/oralcav.htmlexternalicon (accessed on 5 July 2016).
- Saveanu, C.I.; Forna, N.C.; Mohamed, D.; Bobu, L.; Anistoroaei, D.; Bamboi, I.; Balcos, C.; Cheptea, C.; Saveanu, A.E.; Tanculescu-Doloca, O. Study on dietary habits of first grade schoolchildren in Iasi, Romania. RJDME 2020, 9, 62–68. [Google Scholar]
- Saveanu, C.I.; Gheorghiu-Rusu, T.; Balcos, C.; Bamboi, I.; Bobu, L.; Saveanu, A.E.; Anistoroaei, D.; Golovcencu, L.; Tanculescu-Doloca, O. Comparative study of assessment of educational level high school students in Suceava, Romania. RJDME 2020, 9, 6–14. [Google Scholar]
- Saveanu, C.I.; Bobu, L.; Mohamed, D.; Balcos, C.; Bamboi, I.; Golovcencu, L.; Săveanu, A.E.; Anistoroaei, D.; Melian, A. Study on oral health attitudes and behaviors of first grade schoolchildren in Iasi, Romania. RJOR 2019, 11, 223–227. [Google Scholar]
- Saveanu, C.I.; Anistoroaei, D.; Golovcencu, L.; Saveanu, A.E. Assessing the level of knowledge and attitudes about oral health behaviors of preschoolers. RJDME 2019, 8, 71–78. [Google Scholar]
- Gupta, T.; Sequeira, P.; Achary, S. Oral health knowledge, attitude and practices of a 15-year-old adolescent population in Southern India and their social determinants. Oral. Health Prev. Dent. 2012, 10, 345–354. [Google Scholar]
- Traebert, J.Y.; De Lacerda, J.T. Association between maternal schooling and caries prevalence: A cross-sectional study in southern Brazil. Oral. Health Prev. Dent. 2011, 9, 47–52. [Google Scholar] [PubMed]
- Institute for Health Metrics and Evaluation (IHME). Findings from the Global Burden of Disease Study 2017; Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2018. [Google Scholar]
- Peres, M.A.; Macpherson, L.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Hosseinpoor, A.R.; Itani, L.; Petersen, P.E. Socio-economic inequality in oral healthcare coverage: Results from the World Health Survey. J. Dent. Res. 2012, 91, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Ending Childhood Dental Caries: WHO Implementation Manual; World Health Organization: Geneva, Switzerland, 2019.
- O’Mullane, D.M.; Baez, R.J.; Jones, S.; Lennon, M.A.; Petersen, P.E.; Rugg-Gunn, A.J.; Whelton, H.; Whitford, G.M. Fluoride and Oral Health. Comm. Dent. Health 2016, 33, 69–99. [Google Scholar]
- WHO Expert Committee on Oral Health Status and Fluoride Use & World Health Organization. Fluorides and Oral Health: Report of a WHO Expert Committee on Oral Health Status and Fluoride Use [Meeting Held in Geneva from 22 to 28 November 1993]; World Health Organization: Geneva, Switzerland, 1994; Available online: https://apps.who.int/iris/handle/10665/39746 (accessed on 18 July 2021).
- Resolution WHA 60.17. Oral health: Action plan for promotion and integrated disease prevention. In Sixtieth World Health Assembly, Geneva, 23 May 2007; World Health Organization: Geneva, Switzerland; Available online: http://apps.who.int/iris/bitstream/handle/10665/22590/A60_R17-en.pdf (accessed on 21 August 2021).
- Petersen, P.E.; Ogawa, H. Prevention of dental caries through the use of fluoride-the WHO approach. Comm. Dent. Health 2016, 33, 66–68. [Google Scholar]
- Marinho, V.C.; Higgins, J.P.; Logan, S.; Sheiham, A. Topical fluoride (toothpastes, mouthrins, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2003, 4, CD002782. [Google Scholar] [CrossRef]
- Sharon, E.M.; Barmes, D.E.; Bailey, K.V.; Sundram, C.J. Guidelines on Oral Health; A manual for health personnel Dental Health. Unit; Penang Printed and distributed by the Regional Office for the Western Pacific of the World Health Organization: Penang, Malaysia, 1971; pp. 15–20. [Google Scholar]
- Smyth, E.; Caamano, F.; Fernández-Riveiro, P. Oral health knowledge, attitudes and practice in 12-year-old schoolchildren. Med. Oral Patol. Oral Cir. Bucal. 2007, 12, 614–620. [Google Scholar]
- Singh, A.; Gambhir, R.S.; Singh, S.; Kapoor, V.; Singh, J. Oral health: How much do you know?-A study on knowledge, attitude and practices of patients visiting a North Indian dental school. Eur. J. Dent. 2014, 8, 63–67. [Google Scholar] [CrossRef]
- Carneiro, L.; Kabulwa, M.; Makyao, M.; Mrosso, G.; Choum, R. Oral Health Knowledge and Practices of Secondary School Students, Tanga, Tanzania. Int. J. Dent. 2011. [CrossRef] [PubMed]
- Duangthip, D.; Chu, C.H. Challenges in Oral Hygiene and Oral Health Policy. Front. Oral. Health 2020, 1, 575428. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Rakhshanderou, S.; Ramezankhani, A.; Noroozi, M.; Armoon, B. Oral Health Education and Promotion Programmes: Meta-Analysis of 17-Year Intervention. Int. J. Dent. Hyg. 2018, 16, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Rakhshanderou, S.; Ramezankhani, A.; Buunk-Werkhoven, Y.; Noroozi, M.; Armoon, B. Are educating and promoting interventions effective in oral health? A systematic review. Int. J. Dent. Hyg 2018, 16, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Petersen, P.E.; Wang, H.Y.; Bian, J.Y.; Zhang, B.X. Oral health knowledge, attitudes and behaviour of children and adolescents in China. Int. Dent. J. 2003, 53, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, R.; Al Shulayyi, M.; Baseer, M.A.; Saeed Bahamid, A.A.; Al Saffan, A.D.; Al Herbisch, R. Self-Reported Basic Oral Health Knowledge of Primary School Students and Teachers in Rural Areas of Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021, 13, 521–529. [Google Scholar] [CrossRef]
- Genco, R.J.; Sanz, M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontology 2020, 83, 7–13. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.; Marcenes, W.; GBD 2015 Oral Health Collaborators (2017). Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Shaghaghian, S.; Zeraatkar, M. Factors Affecting Oral Hygiene and Tooth Brushing in Preschool Children, Shiraz/Iran. J. Dent. Biomater. 2017, 4, 394–402. [Google Scholar]
- Sharma, A.S.; Sheth, S.A.; Dhaduk, P.J.; Chovateeya, S.R.; Mistry, B.J.; Jogi, M.R. Oral Hygiene Practices and Factors Affecting Oral Health Service Utilization among Children (11–14 Years) of Government School of Nikol Ward of East Zone of Ahmedabad, Gujarat, India. Contemp. Clin. Dent. 2019, 10, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Beyene, D.H.; Beyene, B.S.; Digesa, L.E.; Tariku, E.Z. Oral Hygiene Practices and Associated Factors among Patients Visiting Private Dental Clinics at Hawassa City, Southern Ethiopia, 2018. Int. J. Dent. 2021, 2021. [Google Scholar] [CrossRef] [PubMed]
- Muller-Bolla, M.; Courson, F. Toothbrushing methods to use in children: A systematic review. Oral. Health Prev. Dent. 2013, 11, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Rajwani, A.R.; Hawes, S.N.D.T.A.; Quaranta, A.; Rincon Aguilar, J.C. Effectiveness of Manual Toothbrushing Techniques on Plaque and Gingivitis: A Systematic Review. Oral. Health Prev. Dent. 2020, 18, 843–854. [Google Scholar] [CrossRef]
- Jackson, S.L.; Vann, W.F.; Jr Kotch, J.B.; Pahel, B.T.; Lee, J.Y. Impact of poor oral health on children’s school attendance and performance. Am. J. Public Health 2011, 101, 1900–1906. [Google Scholar] [CrossRef]
- Tachalov, V.V.; Orekhova, L.Y.; Kudryavtseva, T.V.; Isaeva, E.R.; Loboda, E.S. Manifestations of personal characteristics in individual oral care. EPMA J. 2016, 7, 8. [Google Scholar] [CrossRef]
- Skafida, V.; Chambers, S. Positive association between sugar consumption and dental decay prevalence independent of oral hygiene in pre-school children: A longitudinal prospective study. J. Public Health 2018, 40, e275–e283. [Google Scholar] [CrossRef]
- Nazarianpirdosti, M.; Janatolmakan, M.; Andayeshgar, B.; Khatony, A. Assessment of Knowledge, Attitude, and Practice of Iranian Nurses towards Toothbrush Maintenance and Use. Nurs. Res. Pract. 2021, 3694141. [Google Scholar] [CrossRef]
- Marsh, P.D. Dental plaque as a biofilm and a microbial community–Implications for health and disease. BMC Oral Health 2006, 6, S14. [Google Scholar] [CrossRef]
- Al-Qahtani, S.M.; Razak, P.A.; Khan, S.D. Knowledge and Practice of Preventive Measures for Oral Health Care among Male Intermediate Schoolchildren in Abha, Saudi Arabia. Int. J. Environ. Res. Public Health 2020, 17, 703. [Google Scholar] [CrossRef]
- Hou, R.; Mi, Y.; Xu, Q.; Wu, F.; Ma, Y.; Xue, P.; Xiao, G.; Zhang, Y.; Wei, Y.; Yang, W. Oral health survey and oral health questionnaire for high school students in Tibet, China. Head Face Med. 2014, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Ogunrinde, T.J.; Oyewole, O.E.; Dosumu, O.O. Dental care knowledge and practices among secondary school adolescents in Ibadan North Local Government Areas of Oyo State, Nigeria. Eur. J. Gen. Dent. 2015, 4, 68–73. [Google Scholar] [CrossRef]
- Graça, S.R.; Albuquerque, T.S.; Luis, H.S.; Assunção, V.A.; Malmqvist, S.; Cuculescu, M.; Johannsen, A. Oral Health Knowledge, Perceptions, and Habits of Adolescents from Portugal, Romania, and Sweden: A Comparative Study. J. Int Soc. Prev Community Dent. 2019, 9, 470–480. [Google Scholar] [CrossRef]
- Gao, J.; Ruan, J.; Zhao, L.; Zhou, H.; Huang., R.; Tian, J. Oral health status and oral health knowledge, attitudes and behavior among rural children in Shaanxi, western China: A cross-sectional survey. BMC Oral Health 2014, 14, 144. [Google Scholar] [CrossRef]
- Kulkarni, P.; Singh, D.K.; Jalaluddin, M. Comparison of Efficacy of Manual and Powered Toothbrushes in Plaque Control and Gingival Inflammation: A Clinical Study among the Population of East Indian Region. J. Int. Soc. Prev. Community Dent. 2017, 7, 168–174. [Google Scholar] [CrossRef]
- Wyne, A.H.; Chohan, A.N.; Al-Dosari, K.; Al-Dokheil, M. Oral health knowledge and sources of information among male Saudi school children. Odontostomatol. Trop. 2004, 27, 22–26. [Google Scholar] [PubMed]
- Wahengbam, P.P.; Kshetrimayum, N.; Wahengbam, B.S.; Nandkeoliar, T.; Lyngdoh, D. Assessment of oral health knowledge, attitude and self-care practice among adolescents—A state wide cross- sectional study in Manipur, North Eastern India. J. Clin. Diagn. Res. 2016, 10, ZC65–ZC70. [Google Scholar] [CrossRef]
- Buckeridge, A.; King, N.; Anthonappa, R. Relationships between parental education, choice of child dentifrice, and their children’s caries experience. Int. J. Ped. Dent. 2021, 31, 115–121. [Google Scholar] [CrossRef]
- Walsh, T.; Worthington, H.V.; Glenny, A.M.; Marinho, V.C.; Jeroncic, A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst. Rev. 2019, 3, CD007868. [Google Scholar] [CrossRef]
- Creeth, J.; Bosma, M.L.; Govier, K. How much is a ‘pea-sized amount’? A study of dentifrice dosing by parents in three countries. Int. Dent. J. 2013, 63, 25–30. [Google Scholar] [CrossRef]
- Nordström, A.; Birkhed, D. Attitudes and behavioural factors relating to toothbrushing and the use of fluoride toothpaste among caries-active Swedish adolescents-A questionnaire study. Acta Odontol. Scand. 2017, 75, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.T.; Hanson, N.; Ristic, H.; Whall, C.W.; Estrich, C.G.; Zentz, R.R. Fluoride toothpaste efficacy and safety in children younger than 6 years: A systematic review. J. Am. Dental Assoc. 2014, 145, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, F.I.; Groisman, S.; Toledo, E.; Sampaio, F.H.; Verbicario, R.J.; Ricardo, H.; Olival, R. Habits and Knowledge about Toothpaste of Students from Legiao da Boa Vontade (LBV). J. Dent. Health Oral. Disord. Ther. 2015, 3, 00076. [Google Scholar] [CrossRef]
- Kumar, S.; Tadakamadla, J.; Johnson, N.W. Effect of Toothbrushing Frequency on Incidence and Increment of Dental Caries: A Systematic Review and Meta-Analysis. J. Dent. Res. 2016, 95, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Holmes, R.D. Tooth brushing frequency and risk of new carious lesions. Evid. Based Dent. 2016, 17, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Gudipaneni, R.K.; Patil, S.R.; Assiry, A.A.; Karobari, M.I.; Bandela, V.; Metta, K.K.; Almuhanna, R. Association of oral hygiene practices with the outcome of untreated dental caries and its clinical consequences in pre- and primary school children: A cross-sectional study in a northern province of Saudi Arabia. Clin. Exp. Dent. Res. 2021, 7, 968–977. [Google Scholar] [CrossRef]
- Prasai Dixit, L.; Shakya, A.; Shrestha, M.; Shrestha, A. Dental caries prevalence, oral health knowledge and practice among indigenous Chepang school children of Nepal. BMC Oral Health 2013, 13, 20. [Google Scholar] [CrossRef]
- Obregón-Rodríguez, N.; Fernández-Riveiro, P.; Piñeiro-Lamas, M.; Smyth-Chamosa, E.; Montes-Martínez, A.; Suárez-Cunqueiro, M.M. Prevalence and caries-related risk factors in schoolchildren of 12-and 15-year-old: A cross-sectional study. BMC Oral Health 2019, 19, 120. [Google Scholar] [CrossRef]
- Zhang, M.; Lan, J.; Zhang, T.; Sun, W.; Liu, P.; Wang, Z. Oral health and caries/gingivitis-associated factors of adolescents aged 12–15 in Shandong province, China: A cross-sectional Oral Health Survey. BMC Oral Health 2021, 21, 288. [Google Scholar] [CrossRef]
- Folayan, M.O.; El Tantawi, M.; Chukwumah, N.M.; Alade, M.; Oginni, O.; Mapayi, B.; Arowolo, O.; Sam-Agudu, N.A. Individual and familial factors associated with caries and gingivitis among adolescent’s resident in a semi-urban community in South-Western Nigeria. BMC Oral Health 2021, 21, 166. [Google Scholar] [CrossRef]
- Ausenda, F.; Jeong, N.; Arsenault, P.; Gyurko, R.; Finkelman, M.; Dragan, I.F.; Levi, P.A., Jr. The Effect of the Bass Intrasulcular Toothbrushing Technique on the Reduction of Gingival Inflammation: A Randomized Clinical Trial. J. Evid. Based Dent. Pract. 2019, 19, 106–114. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Diseases and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Seneviratne, C.J.; Zhang, C.F.; Samaranayake, L.P. Dental plaque biofilm in oral health and disease. Chin. J. Dent. Res. 2011, 14, 87–94. [Google Scholar]
- Zareban, I.; Karimy, M.; Araban, M.; Delaney, D. Oral self-care behavior and its influencing factors in a sample of school children from Central Iran. Arch. Public Health 2021, 79, 175. [Google Scholar] [CrossRef] [PubMed]
- Hawrot, H. Does motivational interviewing promote oral health in adolescents? Evid. Based Dent. 2021, 22, 134–135. [Google Scholar] [CrossRef]
- Shahid, M. Regular supervised fluoride mouthrinse use by children and adolescents associated with caries reduction. Evid. Based Dent. 2017, 18, 11–12. [Google Scholar] [CrossRef]
- Marinho, V.C.; Chong, L.Y.; Worthington, H.V.; Walsh, T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2016, 7, CD002284. [Google Scholar] [CrossRef] [PubMed]
- Thangavelu, A.; Kaspar, S.S.; Kathirvelu, R.P.; Srinivasan, B.; Srinivasan, S.; Sundram, R. Chlorhexidine: An Elixir for Periodontics. J. Pharm. Bio Allied Sci. 2020, 12, S57–S59. [Google Scholar] [CrossRef]
- Fernandez, M.; Guedes, M.; Langa, G.; Rösing, C.K.; Cavagni, J.; Muniz, F. Virucidal efficacy of chlorhexidine: A systematic review. Odontology 2021, 2021, 1–17. [Google Scholar] [CrossRef]
- Rösing, C.K.; Cavagni, J.; Gaio, E.J.; Muniz, F.; Ranzan, N.; Oballe, H.; Friedrich, S.A.; Severo, R.M.; Stewart, B.; Zhang, Y.P. Efficacy of two mouthwashes with cetylpyridinium chloride: A controlled randomized clinical trial. Braz. Oral Res. 2017, 31, 47. [Google Scholar] [CrossRef]
- Williams, M.I. The antibacterial and antiplaque ef.ffectiveness of mouthwashes containing cetylpyridinium chloride with and without alcohol in improving gingival health. J. Clin. Dent. 2011, 22, 179–182. [Google Scholar] [PubMed]
- Pelino, J.; Passero, A.; Martin, A.A.; Charles, C.A. In vitro effects of alcohol-containing mouthwashes on human enamel and restorative materials. Braz. Oral Res. 2018, 32, e25. [Google Scholar] [CrossRef] [PubMed]
- Vlachojannis, C.; Al-Ahmad, A.; Hellwig, E.; Chrubasik, S. Listerine® Products: An Update on the Efficacy and Safety. Phytother. Res. PTR 2016, 30, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Lai, W.P.B.; Lim, W.; Yee, R. Recommending 1000 ppm fluoride toothpaste for caries prevention in children. Proc. Singap. Healthcare 2021, 30, 250–253. [Google Scholar] [CrossRef]
- Blaggana, A.; Grover, V.; Anjali, A.K.; Blaggana, V.; Tanwar, R.; Kaur, H.; Haneet, R.K. Oral health knowledge, attitudes and practice behaviour among secondary school children in Chandigarh. J. Clin. Diagn. Res. 2016, 10, ZC01–ZC06. [Google Scholar] [CrossRef]
- Togoo, R.A.; Yaseen, S.; Zakirulla, M.; Nasim, V.S.; Al Zamzami, M. Oral hygiene knowledge and practices among school children in a rural area of southern Saudi Arabia. Int. J. Contemp. Dent. 2012, 3, 57–62. [Google Scholar]
- Amarlal, D.; Devdas, K.; Priya, M.; Venkatachalapathy, A. Oral health attitudes, knowledge and practice among school children in Chennai, India. J. Educ. Ethic Dent. 2013, 3, 26. [Google Scholar] [CrossRef]
- NHS–Why Should I use Interdental Brushes? 2021. Available online: https://www.nhs.uk/common-health-questions/dental-health/why-should-i-use-interdental-brushes (accessed on 15 July 2021).
- Rosenauer, T.; Wagenschwanz, C.; Kuhn, M.; Kensche, A.; Stiehl, S.; Hannig, C. The Bleeding on Brushing Index: A novel index in preventive dentistry. Int. Dent. J. 2017, 67, 299–307. [Google Scholar] [CrossRef]
- Silva, C.; Albuquerque, P.; De Assis, P.; Lopes, C.; Anníbal, H.; Lago, M.; Braz, R. Does flossing before or after brushing influence the reduction in the plaque index? A systematic review and meta-analysis. Int. J. Dent. Hyg. 2022, 20, 18–25. [Google Scholar] [CrossRef]
- Marchetti, G.; Assunção, L.R.D.S.; Soares, G.M.S.; Fraiz, F.C. Are Information Technologies Capable of Stimulating the Use of Dental Floss by Adolescents? A Cluster Randomized Clinical Trial. Oral. Health Prev. Dent. 2020, 18, 427–432. [Google Scholar] [CrossRef]
- Worthington, H.V.; MacDonald, L.; Poklepovic Pericic, T.; Sambunjak, D.; Johnson, T.M.; Imai, P.; Clarkson, J.E. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochrane Database Syst. Rev. 2019, 4, CD012018. [Google Scholar] [CrossRef] [PubMed]
- Gallie, A. Home use of interdental cleaning devices and toothbrushing and their role in disease prevention. Evid. Based Dent. 2019, 20, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Wigen, T.I.; Wang, N.J. Characteristics of teenagers who use dental floss. Comm. Dental Health 2021, 38, 10–14. [Google Scholar] [CrossRef]
- Baumgartner, C.S.; Wang, N.J.; Wigen, T.I. Oral health behaviors in 12-year-olds. Association with caries and characteristics of the children? Acta Odontol. Scand. 2022, 80, 15–20. [Google Scholar] [CrossRef]
- Pandey, N.; Koju, S.; Khapung, A.; Gupta, S.; Aryal, D.; Dhami, B. Dental Floss Prescription Pattern among the Dental Interns of Nepal. JNMA J. Nepal Medical Assoc. 2020, 58, 580–586. [Google Scholar] [CrossRef]
- Akhionbare, O.; Ehizele, A.O. Use of dental floss: Opinion of present and future oral health workers. Odonto-Stomatol. Trop. Trop. Dent. J. 2016, 39, 40–48. [Google Scholar]
| Q 1 = How old are you? |
| Q 2 = What is your gender? (F = female; M = male). |
| Q 3 = What is the county where you study? (IS = Iasi; BT = Botosani; SV = Suceava; PH = Prahova; NT = Neamt; B = Bucharest; BC = Bacau). |
| Q 4 = What is the class level? (MS = middle school/HS = high school). |
| Q 5 = What class grade are you in? (5-th; 6-th; 7-th; 8-th; 9-th; 10-th; 11-th; 12-th). |
| Q 6 = Do you know a special dental brushing technique? (Yes/No). |
| Q 7 = Do you think that dental brushing is done to remove dental bacterial plaque? (Yes/No). |
| Q 8 = Do you think that dental brushing is done to remove food? (Yes/No). |
| Q 9 = Do you think that dental brushing is done to have whiter teeth? (Yes/No). |
| Q 10 = Do you think that dental brushing aims to remineralizers your teeth? (Yes/No). |
| Q 11 = How long do you think dental brushing should last? 1 = 1 min; 2 = 2 min; 3 = 3 min; 4 = 4 min. |
| Q 12 = Is the design important when choosing a toothbrush? (Yes/No). |
| Q 13 = Is the price important when choosing a toothbrush? (Yes/No). |
| Q 14 = Is the manufacturer company important when buying a toothbrush? (Yes/No). |
| Q 15 = Is age important when choosing a toothbrush? (Yes/No). |
| Q 16 = Is it important to follow dental professional recommendations when choosing a toothbrush? (Yes/No). |
| Q 17 = Is it important to consider advertising when choosing a toothbrush? (Yes/No). |
| Q 18 = Is it important to take into account the design when choosing toothpaste? (Yes/No). |
| Q 19 = Is it important to take into account the price when choosing toothpaste? (Yes/No). |
| Q 20 =Is it important to take the manufacturer company into account when choosing toothpaste? (Yes/No). |
| Q 21 = Is it important to take into account the fluoride content when choosing toothpaste? (Yes/No). |
| Q 22 = Is it important to take into account the properties of paste when choosing your toothpaste? (Yes/No). |
| Q 23 = It is important to take into account advertising when choosing your toothpaste? (Yes/No). |
| Q 24 = How much toothpaste do you use when you brush your teeth? (1 = the length of the toothbrush; 2 = as much as a pea; 3 = less than a pea). |
| Q 25 = What is the frequency of brushing? (1 = once a day; 2 = twice a day; 3 = three times a day; 4 = after each meal; 5 = when I feel the need). |
| Q 26 = When do you brush your teeth? (1 = in the morning; 2 = in the evening; 3 = both morning and evening; 4 = after each meal; 5 = when I feel the need). |
| Q 27 = Do you use mouthwash? (Yes/No). |
| Q 28 = When do you use mouthwash? (1 = after each brushing; 2 = when I feel the need; 3 = in the morning; 4 = in the evening; 5 = I don’t use). |
| Q 29 = Do you floss for dental cleaning? (Yes/No). |
| Q 30 When do you use dental floss for interdental cleaning? (1 = after each brushing; 2 = when I feel the need; 3 = in the morning; 4 = in the evening; 5 = I do not use). |
| Count | Study Level | Gender | County | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ms | Hs | M | F | IS | BT | SV | PH | NT | B | BC | |||
| Class | 5th | 60 | - | 21 | 39 | 48 | 0 | 2 | 1 | 0 | 5 | 4 | 60 |
| 6th | 116 | - | 39 | 77 | 104 | 0 | 7 | 0 | 1 | 3 | 1 | 116 | |
| 7th | 135 | - | 55 | 80 | 38 | 0 | 15 | 2 | 35 | 14 | 31 | 135 | |
| 8th | 43 | - | 20 | 23 | 7 | 0 | 14 | 2 | 16 | 3 | 1 | 43 | |
| 9th | - | 76 | 18 | 58 | 69 | 0 | 3 | 1 | 0 | 3 | 0 | 76 | |
| 10th | - | 86 | 26 | 60 | 59 | 0 | 1 | 19 | 0 | 6 | 1 | 86 | |
| 11th | - | 135 | 38 | 97 | 91 | 2 | 9 | 23 | 1 | 9 | 0 | 135 | |
| 12th | - | 67 | 33 | 34 | 42 | 6 | 5 | 11 | 0 | 3 | 0 | 67 | |
| Total | 354 | 364 | 250 | 468 | 458 | 8 | 56 | 59 | 53 | 46 | 38 | 718 | |
| Questions | Yes | MS | HS | p | R | |
|---|---|---|---|---|---|---|
| Criteria for choosing a toothbrush: | ||||||
| Q12 | Is design important? | 231 | 84 | 147 | 0 * | −0.178 |
| Q13 | Is price important? | 140 | 52 | 88 | 0.001 * | 0.12 |
| Q14 | Is the manufacturer company important? | 213 | 82 | 131 | 0 * | −0.14 |
| Q15 | Is age important? | 247 | 160 | 87 | 0 * | 0.224 |
| Q16 | Are dental professional recommendations important? | 372 | 202 | 170 | 0.003 * | 0.104 |
| Q17 | Is advertising important? | 45 | 18 | 27 | 0.128 | −0.048 |
| Criteria for choosing a tube of toothpaste: | ||||||
| Q18 | Is design important? | 66 | 33 | 33 | 0.341 | 0.02 |
| Q19 | Is price important? | 107 | 49 | 58 | 0.431 | −0.029 |
| Q20 | Is the manufacturer company important? | 220 | 92 | 128 | 0.005 * | −0.1 |
| Q21 | Is the fluoride content important? | 173 | 83 | 90 | 0.689 | −0.015 |
| Q22 | Are the properties important? | 550 | 275 | 275 | 0.282 | 0.025 |
| Q23 | Is advertising important? | 55 | 20 | 35 | 0.031 * | −0.074 |
| Questions | MS | HS | Total | p | R | |
|---|---|---|---|---|---|---|
| Q24 | How much toothpaste do you use when brushing your teeth? | 0.625 | −0.035 | |||
| 1 = the length of the toothbrush | 178 | 195 | 373 | |||
| 2 = as much as a pea | 173 | 167 | 340 | |||
| 3 = less than a pea | 3 | 2 | 5 | |||
| Q25 | What is the frequency of brushing? | 0.079 | 0.037 | |||
| 1 = once a day | 55 | 37 | 92 | |||
| 2 = twice a day | 234 | 248 | 482 | |||
| 3 = three times a day | 21 | 36 | 57 | |||
| 4 = after each meal | 25 | 28 | 53 | |||
| 5 = when I feel the need | 19 | 15 | 34 | |||
| Q26 | When do you brush your teeth? | 0.099 | 0.095 | |||
| 1 = in the morning | 36 | 24 | 60 | |||
| 2 = in the evening | 25 | 15 | 40 | |||
| 3 = both morning and evening | 246 | 262 | 508 | |||
| 4 = after each meal | 33 | 40 | 73 | |||
| 5 = when I feel the need | 11 | 21 | 32 | |||
| 6 = I don’t use | 3 | 2 | 5 | |||
| Questions | MS | HS | Total | p | R | |
|---|---|---|---|---|---|---|
| Q27 | Do you use mouthwash? | 0.194 | −0.048 | |||
| Yes | 199 | 222 | 421 | |||
| No | 155 | 142 | 297 | |||
| Q28 | When do you use mouthwash? | 0.062 | −0.078 | |||
| 1 = after each brushing | 109 | 119 | 228 | |||
| 2 = when I feel the need | 56 | 83 | 139 | |||
| 3 = in the morning | 20 | 22 | 42 | |||
| 4 = in the evening | 19 | 12 | 31 | |||
| 5 = I don’t use | 150 | 128 | 278 | |||
| Q29 | Do you floss for dental cleaning? | 0.051 | −0.073 | |||
| Yes | 106 | 134 | 240 | |||
| No | 248 | 230 | 478 | |||
| Q30 | When do you use dental floss for interdental cleaning? | 0.091 | −0.038 | |||
| 1 = after each brushing | 41 | 33 | 74 | |||
| 2 = when I feel the need | 52 | 80 | 132 | |||
| 3 = in the morning | 1 | 0 | 1 | |||
| 4 = in the evening | 19 | 21 | 40 | |||
| 5 = I do not use | 241 | 230 | 471 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saveanu, C.I.; Cretu, C.C.; Bamboi, I.; Săveanu, A.E.; Anistoroaei, D. Title Cross-Sectional Study to Evaluate Knowledge and Attitudes on Oral Hygiene of Romanian Students. Medicina 2022, 58, 406. https://doi.org/10.3390/medicina58030406
Saveanu CI, Cretu CC, Bamboi I, Săveanu AE, Anistoroaei D. Title Cross-Sectional Study to Evaluate Knowledge and Attitudes on Oral Hygiene of Romanian Students. Medicina. 2022; 58(3):406. https://doi.org/10.3390/medicina58030406
Chicago/Turabian StyleSaveanu, Catalina Iulia, Cosmin Constantin Cretu, Irina Bamboi, Alexandra Ecaterina Săveanu, and Daniela Anistoroaei. 2022. "Title Cross-Sectional Study to Evaluate Knowledge and Attitudes on Oral Hygiene of Romanian Students" Medicina 58, no. 3: 406. https://doi.org/10.3390/medicina58030406
APA StyleSaveanu, C. I., Cretu, C. C., Bamboi, I., Săveanu, A. E., & Anistoroaei, D. (2022). Title Cross-Sectional Study to Evaluate Knowledge and Attitudes on Oral Hygiene of Romanian Students. Medicina, 58(3), 406. https://doi.org/10.3390/medicina58030406







