Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
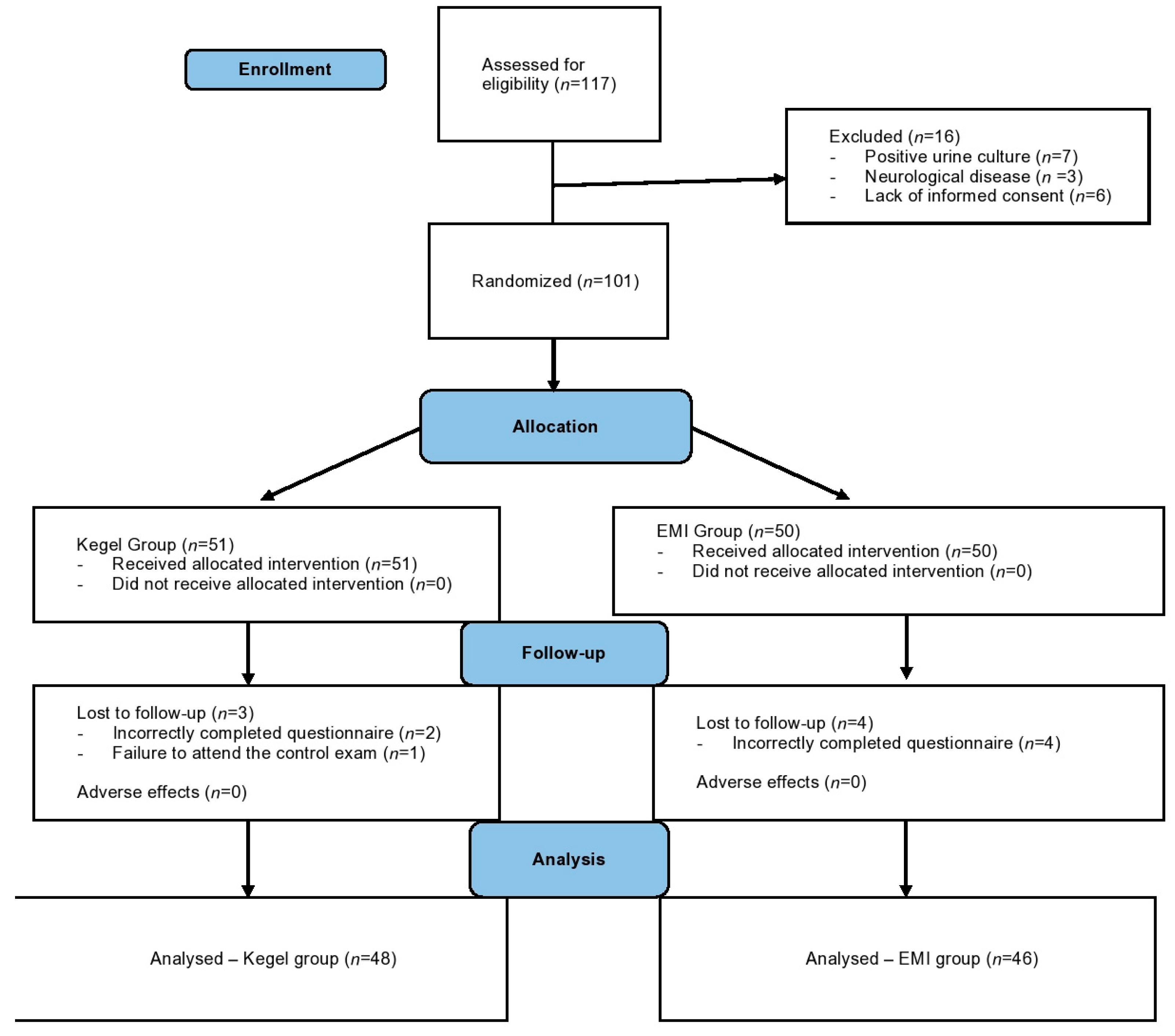
2.1. Participants and Study Design
2.2. Perineometer
2.3. Questionnaires
2.4. Interventions
2.4.1. Kegel Exercises
2.4.2. Extracorporeal Magnetic Innervation
2.4.3. Outcomes
- The average increase in vaginal pressure, as measured with the PeritronTM perineometer at eight weeks and 3 months after treatment.
- The participant’s overall treatment satisfaction, measured by the PGI-I scale three months after the end of treatment.
- Symptom distress, using the ICIQ-UI-SF questionnaire at the initial visit (T0), after the intervention was completed (T1), and three months (T2) following the end of the intervention.
- Quality of life, measured by ICIQ-LUTSqol also at the initial visit (T0), after the intervention was completed (T1), and three months (T2) following the end of the intervention.
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Intravaginal Pressure Assessment with a Perineometer
3.3. Symptom Distress Comparison
3.4. Quality of Life Assessment
3.5. Voiding Diary Analysis
3.6. Overall Treatment Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A. The Standardisation of Terminology in Lower Urinary Tract Function: Report from the Standardisation Sub-Committee of the International Continence Society. Urology 2003, 61, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Ayeleke, R.O.; Hay-Smith, E.J.C.; Omar, M.I. Pelvic Floor Muscle Training Added to Another Active Treatment versus the Same Active Treatment Alone for Urinary Incontinence in Women. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2013; p. CD010551. [Google Scholar]
- Nguyen, M.-L.T.; Armstrong, A.A.; Wieslander, C.K.; Tarnay, C.M. Now Anyone Can Kegel: One-Time Office Teaching of Pelvic Floor Muscle Exercises. Female Pelvic Med. Reconstr. Surg. 2019, 25, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Lim, R.; Lee, S.W.H.; Tan, P.Y.; Liong, M.L.; Yuen, K.H. Efficacy of Electromagnetic Therapy for Urinary Incontinence: A Systematic Review: Efficacy of Electromagnetic Therapy in Urinary Incontinence. Neurourol. Urodynam. 2015, 34, 713–722. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, E.; Ávila-Gandía, V.; López-Román, J.; Martínez-Rodríguez, A.; Rubio-Arias, J.Á. What Pelvic Floor Muscle Training Load Is Optimal in Minimizing Urine Loss in Women with Stress Urinary Incontinence? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4358. [Google Scholar] [CrossRef] [PubMed]
- Lim, R.; Liong, M.L.; Leong, W.S.; Khan, N.A.K.; Yuen, K.H. Patients’ Perception and Satisfaction with Pulsed Magnetic Stimulation for Treatment of Female Stress Urinary Incontinence. Int. Urogynecol. J. 2018, 29, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Gilling, P.J.; Wilson, L.C.; Westenberg, A.M.; McAllister, W.J.; Kennett, K.M.; Frampton, C.M.; Bell, D.F.; Wrigley, P.M.; Fraundorfer, M.R. A Double-Blind Randomized Controlled Trial of Electromagnetic Stimulation of the Pelvic Floor vs. Sham Therapy in the Treatment of Women with Stress Urinary Incontinence. BJU International. 2009, 103, 1386–1390. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Zeng, X.; Shen, H.; Luo, D. Magnetic Stimulation for Female Patients with Stress Urinary Incontinence, a Meta-Analysis of Studies with Short-Term Follow-Up. Medicine 2019, 98, e15572. [Google Scholar] [CrossRef] [PubMed]
- Moroni, R.; Magnani, P.; Haddad, J.; Castro, R.; Brito, L. Conservative Treatment of Stress Urinary Incontinence: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Rev. Bras. Ginecol. Obstet. 2016, 38, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A Brief and Robust Measure for Evaluating the Symptoms and Impact of Urinary Incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Mikuš, M.; Ćorić, M.; Matak, L.; Škegro, B.; Vujić, G.; Banović, V. Validation of the UDI-6 and the ICIQ-UI SF—Croatian Version. Int. Urogynecol. J 2020, 12, 2625–2630. [Google Scholar] [CrossRef] [PubMed]
- Nyström, E.; Sjöström, M.; Stenlund, H.; Samuelsson, E. ICIQ Symptom and Quality of Life Instruments Measure Clinically Relevant Improvements in Women with Stress Urinary Incontinence: ICIQ-UI SF and ICIQ-LUTSqol Correlation to PGI-I. Neurourol. Urodynam. 2015, 34, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Diokno, A.; Yuhico, M. Preference, Compliance and Initial Outcome of Therapeutic Options Chosen by Female Patients with Urinary Incontinence. J. Urol. 1995, 154, 1727–1730, discussion 1731. [Google Scholar] [CrossRef] [PubMed]
- Weber-Rajek, M.; Strączyńska, A.; Strojek, K.; Piekorz, Z.; Pilarska, B.; Podhorecka, M.; Sobieralska-Michalak, K.; Goch, A.; Radzimińska, A. Assessment of the Effectiveness of Pelvic Floor Muscle Training (PFMT) and Extracorporeal Magnetic Innervation (ExMI) in Treatment of Stress Urinary Incontinence in Women: A Randomized Controlled Trial. BioMed Res. Int. 2020, 2020, 1019872. [Google Scholar] [CrossRef] [PubMed]
- Ghoniem, G.; Stanford, E.; Kenton, K.; Achtari, C.; Goldberg, R.; Mascarenhas, T.; Parekh, M.; Tamussino, K.; Tosson, S.; Lose, G.; et al. Evaluation and Outcome Measures in the Treatment of Female Urinary Stress Incontinence: International Urogynecological Association (IUGA) Guidelines for Research and Clinical Practice. Int. Urogynecol. J. 2007, 19, 5–33. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, N.; Mohseni-Bandpei, M.A. Application of Perineometer in the Assessment of Pelvic Floor Muscle Strength and Endurance: A Reliability Study. J. Bodyw. Mov. Ther. 2011, 15, 209–214. [Google Scholar] [CrossRef] [PubMed]
- dos Ribeiro, J.S.; de Guirro, E.C.O.; de Franco, M.M.; Duarte, T.B.; Pomini, J.M.; Ferreira, C.H.J. Inter-Rater Reliability Study of the PeritronTM Perineometer in Pregnant Women. Physiother. Theory Pract. 2016, 32, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Norton, P.A.; Nager, C.W.; Brubaker, L.; Lemack, G.E.; Sirls, L.T.; Holley, R.; Chai, T.C.; Kraus, S.R.; Zyczynski, H.; Smith, B.; et al. The cost of preoperative urodynamics: A secondary analysis of the value trial. Neurourol. Urodyn. 2014, 35, 81–84. [Google Scholar] [CrossRef] [PubMed]
| TIMEPOINT | Pre-Study Screening, Enrolment and Consent | Baseline/Randomisation and Allocation | t0 Prior to Treatment | t1 after Treatment | t2 3 Months after End of Treatment |
|---|---|---|---|---|---|
| ENROLMENT: Eligibility screen Informed consent Allocation | |||||
| X | |||||
| X | |||||
| X | |||||
| INTERVENTIONS: Kegel exercises Extracorporeal magnetic innervation (EMI) | |||||
| 8 weeks | |||||
| 8 weeks | |||||
| ASSESSMENTS: Baseline variables Primary outcome variables Secondary outcome variables PGI-I scale assessment | |||||
| X | X | ||||
| X | X | X | |||
| X | X | X | |||
| X |
| Total (n = 94) | EMI Group (n = 46) | Kegel Group (n = 48) | p | |
|---|---|---|---|---|
| Age, years | 48.33 ± 7.5 | 47.45 ± 7.4 | 49.16 ± 7.6 | 0.272 |
| Height, cm | 166.29 ± 6.9 | 167.21 ± 6.9 | 165.41 ± 6.9 | 0.211 |
| Weight, kg | 71.00 (62.0–81.0) | 69.00 (61.0–81.0) | 73.00 (62.7–80.5) | 0.612 |
| BMI, kg/m2 | 26.30 ± 5.6 | 25.74 ± 5.46 | 26.83 ± 5.7 | 0.348 |
| Tobacco use, n (%) | 48 (51.1) | 27 (58.7) | 21 (43.7) | 0.214 |
| Alcohol use, n (%) | 8 (8.5) | 3 (6.2) | 5 (10.9) | 0.665 |
| Menopause, n (%) | 39 (41.5) | 19 (41.3) | 20 (41.7) | 0.826 |
| Hysterectomy, n (%) | 12 (12.8) | 8 (17.4) | 4 (8.3) | 0.314 |
| Duration of symptoms, months | 12.00 (12.0–24.0) | 12.00 (12.0–24.0) | 15.00 (12.0–27.0) | 0.373 |
| Childbirth, n (%) | 92 (97.9) | 45 (97.8) | 47 (97.9) | 0.999 |
| Parity, n | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 2.0 (1.75–3.0) | 0.128 |
| Vaginal delivery, n | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 2.0 (1.0–3.0) | 0.282 |
| Episiotomy, n (%) | 61 (66.3) | 30 (66.7) | 31 (66.0) | 0.882 |
| Vacuum/forceps use, n (%) | 11 (12.0) | 8 (17.8) | 3 (6.4) | 0.096 |
| Cesarean section, n (%) | 11 (11.9) | 5 (11.1) | 6 (12.8) | 0.806 |
| Newborn >4000 g, n (%) | 37 (40.2) | 19 (42.2) | 18 (38.3) | 0.701 |
| Marital status, n (%) | 0.174 | |||
| Married | 78 (83.0) | 37 (80.4) | 41 (85.4) | |
| Unmarried | 2 (2.1) | 2 (4.3) | 0 (0) | |
| Divorced | 9 (9.6) | 6 (13.0) | 3 (6.2) | |
| Widow | 1 (2.2) | 1 (2.2) | 4 (8.3) | |
| Employment, n (%) | 0.012 | |||
| Employed | 76 (80.9) | 40 (87.0) | 36 (75.0) | |
| Unemployed | 7 (7.4) | 5 (10.9) | 2 (4.2) | |
| Retired | 11 (11.7) | 1 (2.2) | 10 (20.8) | |
| Education, n (%) | 0.246 | |||
| Elementary school | 2 (2.1) | 1 (2.2) | 1 (2.1) | |
| High school | 44 (46.8) | 21 (45.7) | 23 (47.9) | |
| BsC | 23 (24.5) | 15 (32.6) | 8 (16.7) | |
| MA | 25 (26.6) | 9 (19.6) | 16 (33.3) |
| Total (n = 92) | EMI Group (n = 46) | Kegel Group (n = 48) | p | |
|---|---|---|---|---|
| Baseline, cmH2O | 22.85 (18.8–26.6) | 23.30 (19.1–27.3) | 22.25 (18.1–24.6) | 0.354 |
| 8 weeks, cmH2O | 27.65 (22.6–33.8) | 30.45 (26.2–35.2) | 23.50 (20.3–30.6) | 0.001 |
| 3 months, cmH2O | 26.35 (21.1–33.2) | 29.15 (25.3–34.2) | 22.55 (18.0–31.0) | 0.001 |
| Total (n = 94) | EMI Group (n = 46) | Kegel Group (n = 48) | p | |
|---|---|---|---|---|
| Baseline | 14.00 (11.0–16.0) | 14.00 (10.0–16.0) | 14.00 (12.0–16.0) | 0.984 |
| 8 weeks | 10.00 (7.0–14.0) | 8.00 (6.0–11.0) | 12.00 (8.0–15.0) | <0.001 |
| 3 points | 9.50 (6.0–14.0) | 7.50 (5.0–12.0) | 13.00 (6.5–16.0) | 0.001 |
| Total (n = 94) | EMI Group (n = 46) | Kegel Group (n = 48) | p | |
|---|---|---|---|---|
| Baseline | 60.00 (54.0–64.0) | 58.00 (54.0–62.0) | 61.00 (54.5–66.5) | 0.162 |
| 8 weeks | 47.50 (37.0–57.0) | 39.00 (29.0–51.0) | 54.50 (44.0–62.5) | <0.001 |
| 3 months | 44.50 (28.0–62.0) | 36.50 (23.0–47.0) | 57.50 (44.0–64.0) | <0.001 |
| Total (n = 94) | EMI Group (n = 46) | Kegel Group (n = 48) | p | |
|---|---|---|---|---|
| Baseline | 10.00 (8.0–12.0) | 10.00 (8.0–12.0) | 10.50 (8.5–12.0) | 0.616 |
| 8 weeks | 6.00 (3.0–12.0) | 4.00 (2.0–7.0) | 11.50 (6.0–15.0) | <0.001 |
| 3 months | 7.00 (2.0–12.0) | 3.00 (2.0–8.0) | 10.50 (5.5–15.0) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikuš, M.; Kalafatić, D.; Vrbanić, A.; Šprem Goldštajn, M.; Herman, M.; Živković Njavro, M.; Živković, K.; Marić, G.; Ćorić, M. Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial. Medicina 2022, 58, 1863. https://doi.org/10.3390/medicina58121863
Mikuš M, Kalafatić D, Vrbanić A, Šprem Goldštajn M, Herman M, Živković Njavro M, Živković K, Marić G, Ćorić M. Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial. Medicina. 2022; 58(12):1863. https://doi.org/10.3390/medicina58121863
Chicago/Turabian StyleMikuš, Mislav, Držislav Kalafatić, Adam Vrbanić, Marina Šprem Goldštajn, Mislav Herman, Marta Živković Njavro, Klara Živković, Goran Marić, and Mario Ćorić. 2022. "Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial" Medicina 58, no. 12: 1863. https://doi.org/10.3390/medicina58121863
APA StyleMikuš, M., Kalafatić, D., Vrbanić, A., Šprem Goldštajn, M., Herman, M., Živković Njavro, M., Živković, K., Marić, G., & Ćorić, M. (2022). Efficacy Comparison between Kegel Exercises and Extracorporeal Magnetic Innervation in Treatment of Female Stress Urinary Incontinence: A Randomized Clinical Trial. Medicina, 58(12), 1863. https://doi.org/10.3390/medicina58121863






