A Rare Case of Orbitocranial Penetrating Injury with Intracranial Wooden Foreign Body Residue
Abstract
1. Introduction
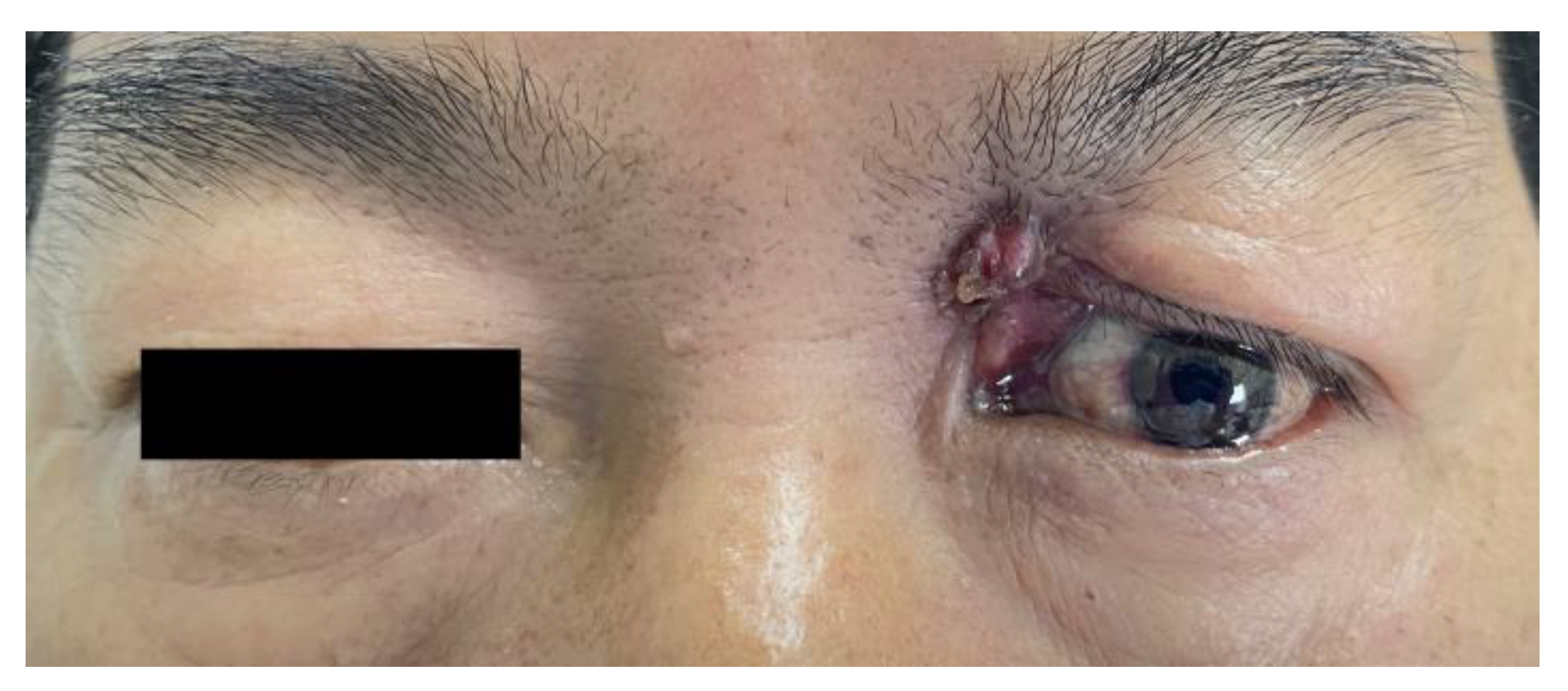
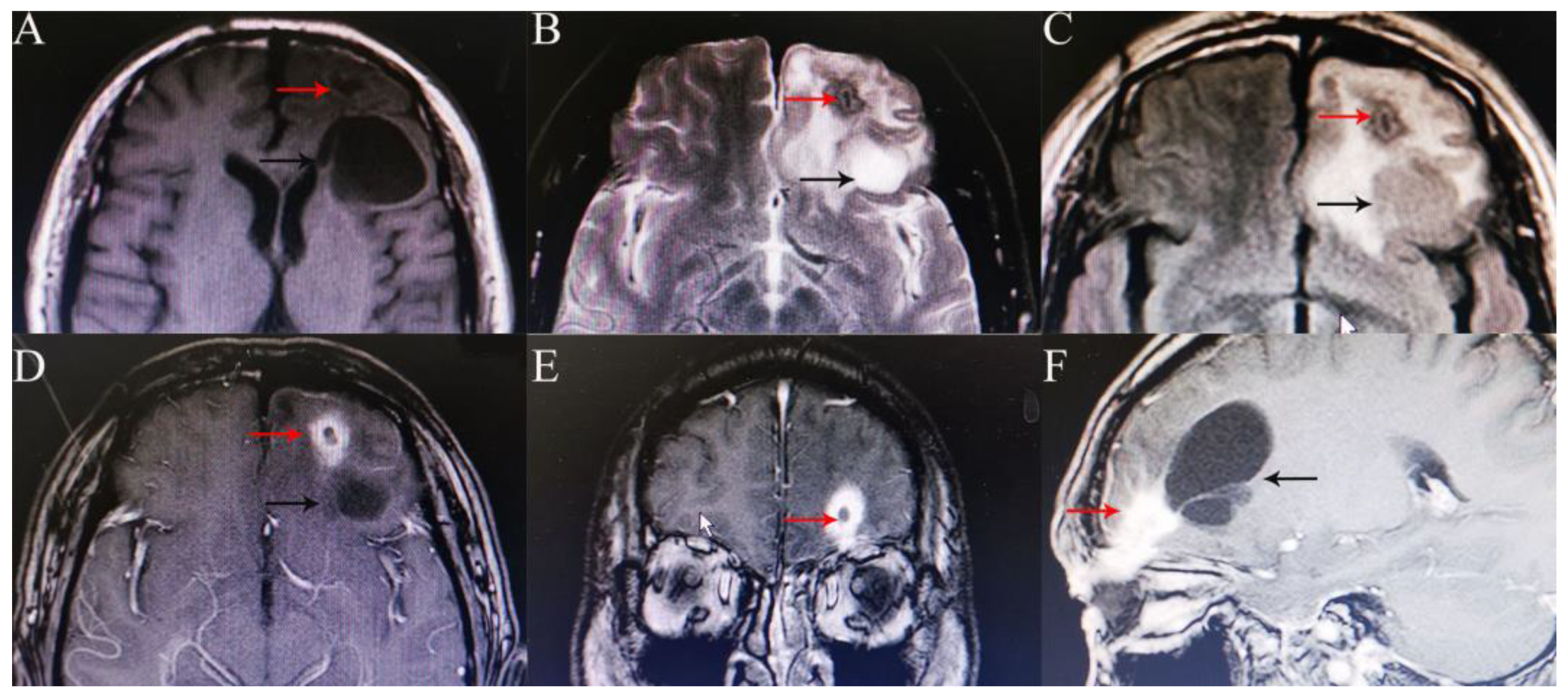
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kasamo, S.; Asakura, T.; Kusumoto, K.; Nakayama, M.; Kadota, K.; Atsuchi, M.; Yamamoto, Y. Transorbital penetrating brain injury. No Shinkei Geka 1992, 20, 433–438. [Google Scholar] [PubMed]
- Dudani, A.; Pawar, H.; Dudani, A.A.; Dudani, K.; Dudani, A. A challenging case of a large orbitocranial wooden foreign body in a child. Indian J. Ophthalmol. 2019, 67, 1510–1512. [Google Scholar] [CrossRef]
- Dunn, I.F.; Kim, D.H.; Rubin, P.A.; Blinder, R.; Gates, J.; Golby, A.J. Orbitocranial wooden foreign body: A pre-, intra-, and postoperative chronicle: Case report. Neurosurgery 2009, 65, E383–E384. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Yagmurlu, K.; Belykh, E.; Lei, T.; Preul, M.C. Management Strategy of a Transorbital Penetrating Pontine Injury by a Wooden Chopstick. World Neurosurg. 2016, 95, 622.e7–622.e15. [Google Scholar] [CrossRef] [PubMed]
- Chehade, L.K.; Curragh, D.; Selva, D. Traumatic intraorbital wooden foreign body: Lessons learnt. Clin. Exp. Ophthalmol. 2019, 47, 543–545. [Google Scholar] [CrossRef]
- Balasubramanian, C.; Kaliaperumal, C.; Jadun, C.K.; Dias, P.S. Transorbital intracranial penetrating injury-an anatomical classification. Surg. Neurol. 2009, 71, 238–240. [Google Scholar] [CrossRef]
- Arslan, M.; Eseoğlu, M.; Güdü, B.O.; Demir. Transorbital orbitocranial penetrating injury caused by a metal bar. J. Neurosci. Rural Pract. 2012, 3, 178–181. [Google Scholar] [CrossRef]
- Harsh, G.R., 4th; Wilson, C.B. Central nervous system mesenchymal chondrosarcoma. Case report. J. Neurosurg. 1984, 61, 375–381. [Google Scholar] [CrossRef]
- Tabibkhooei, A.; Aslaninia, A.; Anousha, K. Childhood Transorbital Skull Base Penetrating Injury: Report of 2 Cases and Review of Literature. World Neurosurg. 2019, 131, 213–216. [Google Scholar] [CrossRef]
- Cho, W.K.; Ko, A.C.; Eatamadi, H.; Al-Ali, A.; Abboud, J.P.; Kikkawa, D.O.; Korn, B.S. Orbital and Orbitocranial Trauma From Pencil Fragments: Role of Timely Diagnosis and Management. Am. J. Ophthalmol. 2017, 180, 46–54. [Google Scholar] [CrossRef]
- Kudo, S.; Takei, T. Computed tomography settings for optimal detection of wooden foreign bodies. Am. J. Emerg. Med. 2016, 34, 2237–2238. [Google Scholar] [CrossRef]
- Dalley, R.W. Intraorbital wood foreign bodies on CT: Use of wide bone window settings to distinguish wood from air. Am. J. Roentgenol. 1995, 164, 434–435. [Google Scholar] [CrossRef]
- Wilson, M.H.; Collins, T.R.; Revington, P.J. Orbitocranial wooden foreign body retrieved by transcranial and superior orbitotomy. Br. J. Oral Maxillofac. Surg. 2016, 54, 1050–1051. [Google Scholar] [CrossRef]
- Maruya, J.; Yamamoto, K.; Wakai, M.; Kaneko, U. Brain abscess following transorbital penetrating injury due to bamboo fragments--case report. Neurol. Med. Chir. 2002, 42, 143–146. [Google Scholar] [CrossRef]
- Amano, K.; Kamano, S. Cerebellar abscess due to penetrating orbital wound. J. Comput. Assist. Tomo. 1982, 6, 1163–1166. [Google Scholar] [CrossRef]
- Braun, J.; Gdal-On, M.; Goldsher, D.; Borovich, B.; Guilburd, J.N. Traumatic carotid aneurysm secondary to cavernous sinus penetration by wood: CT features. J. Comput. Assist. Tomo. 1987, 11, 525–528. [Google Scholar] [CrossRef]
- Liu, H.C.; Qiu, E.; Zhang, T.M.; Zhao, J.W.; Song, W.X.; Fu, J.D. Neurosurgical therapy of transorbital intracranial foreign bodies: Review of 28 cases. Zhonghua Yi Xue Za Zhi 2008, 88, 1737–1741. [Google Scholar]
- du Trevou, M.D.; van Dellen, J.R. Penetrating stab wounds to the brain: The timing of angiography in patients presenting with the weapon already removed. J. Neurosurg. 1992, 31, 905–911. [Google Scholar] [CrossRef]
- Hamilton, A.; Meena, M.; Lawlor, M.; Kourt, G. An unusual case of intraorbital foreign body and its management. Int. Ophthalmol. 2014, 34, 337–339. [Google Scholar] [CrossRef]
- Xu, F.; Li, J.; Sun, S.; Guo, E.; Hao, S.; Hou, Z.; Leung, G.K.; Liu, B. The surgical management of a penetrating orbitocranial injury with a bakelite foreign body reaching the brain stem. Brain Inj. 2013, 27, 951–956. [Google Scholar] [CrossRef]
- Gupta, S.K.; Umredkar, A.A. Juxtapontine abscess around a retained wooden fragment following a penetrating eye injury: Surgical management via a transtentorial approach. J. Neurosurg-Pediatr. 2012, 9, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.F.; Brodkey, J.S.; Colombi, B.J. The danger of intracranial wood. Surg. Neurol. 1977, 7, 95–103. [Google Scholar] [PubMed]
- Del Verme, J.; Giordan, E.; Marton, E.; Zanata, R.; Di Paola, F.; Canova, G.; Longatti, P. Classification of orbitocranial wooden foreign body penetration injuries: What to do when they violate the intracranial space? A systematic review. J. Neurosurg. Sci. 2020, 64, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Zyck, S.; Toshkezi, G.; Krishnamurthy, S.; Carter, D.A.; Siddiqui, A.; Hazama, A.; Jayarao, M.; Chin, L. Treatment of Penetrating Nonmissile Traumatic Brain Injury. Case Series and Review of the Literature. World Neurosurg. 2016, 91, 297–307. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.; He, W.; Yang, Y.; Chen, J. A Rare Case of Orbitocranial Penetrating Injury with Intracranial Wooden Foreign Body Residue. Medicina 2022, 58, 1832. https://doi.org/10.3390/medicina58121832
Wu Y, He W, Yang Y, Chen J. A Rare Case of Orbitocranial Penetrating Injury with Intracranial Wooden Foreign Body Residue. Medicina. 2022; 58(12):1832. https://doi.org/10.3390/medicina58121832
Chicago/Turabian StyleWu, Yi, Weimin He, Yiliu Yang, and Jun Chen. 2022. "A Rare Case of Orbitocranial Penetrating Injury with Intracranial Wooden Foreign Body Residue" Medicina 58, no. 12: 1832. https://doi.org/10.3390/medicina58121832
APA StyleWu, Y., He, W., Yang, Y., & Chen, J. (2022). A Rare Case of Orbitocranial Penetrating Injury with Intracranial Wooden Foreign Body Residue. Medicina, 58(12), 1832. https://doi.org/10.3390/medicina58121832






