Efficacy of Therapeutic Plasma Exchange in Severe Acute Respiratory Distress Syndrome in COVID-19 Patients from the Western Part of Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Part
2.2. Statistical Analysis
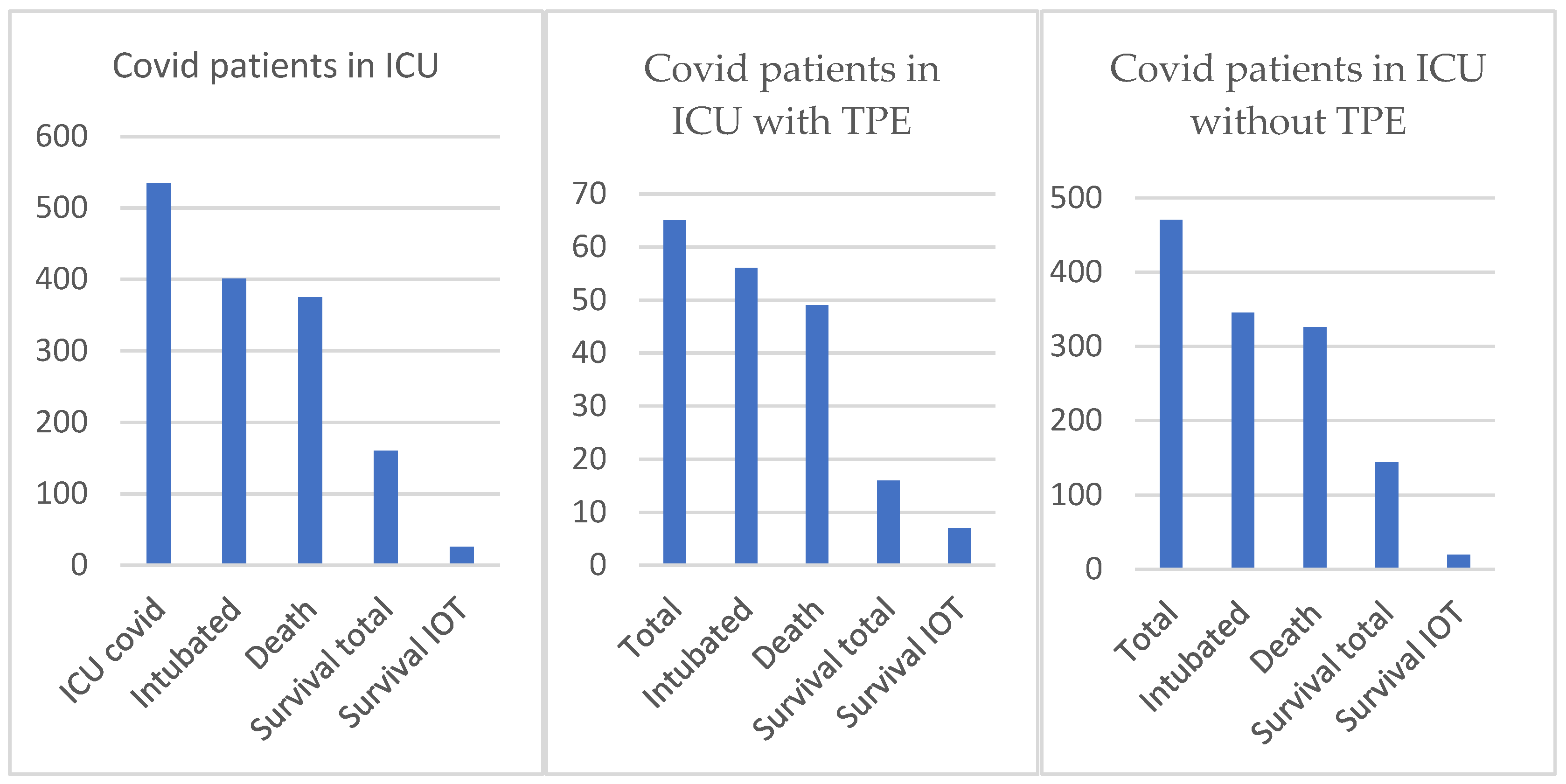
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar]
- Seok Kim, J.; Young Lee, J.; Won Yang, J.; Hwa Lee, K.; Effenberger, M.; Szpirt, W. Immunopathogenesis and treatment of cytokine storm in COVID-19. Theranostics 2021, 11, 316–329. [Google Scholar]
- Yavuz, S.; Ünal, S. Antiviral treatment of COVID-19. Turk. J. Med. Sci. 2020, 50, 611–619. [Google Scholar]
- Ghasemnejad-Berenji, M.; Pashapour, S. Favipiravir and COVID-19: A Simplified Summary. Drug Res. 2021, 71, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Echeverría-Esnal, D.; Martin-Ontiyuelo, C.; Navarrete-Rouco, E.; De-Antonio Cuscó, M.; Ferrández, O. Azithromycin in the treatment of COVID-19: A review. Expert. Rev. Anti-Infect Ther. 2021, 19, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.I.; Khan, M.S.I.; Debnath, C.R.; Nath, P.N.; Mahtab, M.; Nabeka, H. Ivermectin Treatment May Improve the Prognosis of Patients with COVID-19. Arch. De Broncopneumol. 2020, 56, 828–830. [Google Scholar]
- Luo, P.; Liu, Y.; Qiu, L.; Liu, X.; Liu, D.; Li, J. Tocilizumab treatment in COVID-19: A single center experience. J. Med. Virol. 2020, 92, 814–818. [Google Scholar] [CrossRef]
- Peter Horby, F.R.C.P.; Wei, S.L.; Jonathan, R.E.; Marion Mafham, M.D.; Jenifer Bell, L. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [PubMed]
- Hadid, T.; Kafri, Z.; Al-Katib, A. Coagulation and anticoagulation in COVID-19. Blood Rev. 2021, 47, 100–112. [Google Scholar] [CrossRef]
- Tabibi, S.; Tabibi, T.Z.; Conic, R.R.; Banisaeed, N.; Streiff, M.B. Therapeutic Plasma Exchange: A potential Management Strategy for Critically Ill COVID-19 Patients. J. Intensive Care Med. 2020, 35, 827–835. [Google Scholar] [CrossRef]
- Lu, W.; Kelley, W.; Fang, D.C.; Joshi, S.; Kim, Y.; Paroder, M. The use of therapeutic plasma exchange as adjunctive therapy in the treatment of coronavirus disease 2019: A critical appraisal of the current evidence. J. Clin. Apher. 2021, 36, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Lyu, R.K.; Chen, W.H.; Hsieh, S.T. Plasma Exchange Versus Double Filtration Plasmapheresis in the Treatment of Guillain-Barré Syndrome. Ther. Apher. 2002, 6, 163–166. [Google Scholar] [CrossRef]
- Khamis, F.; Al-Zakwani, I.; Al Hashmi, S.; Al Dowaiki, S.; Al Bahrani, M.; Pandak, N. Therapeutic plasma exchange in adults with severe COVID-19 infection. Int. J. Infect. Dis. 2020, 99, 214–218. [Google Scholar] [CrossRef]
- Moore, J.B.; June, C.H. Cytokine release syndrome in severe COVID-19. Science 2020, 368, 473–474. [Google Scholar] [CrossRef] [PubMed]
- Blot, M.; Bour, J.B.; Quenot, J.P.; Bourredjem, A.; Nguyen, M.; Guy, J. The dysregulated innate immune response in severe COVID-19 pneumonia that could drive poorer outcome. J. Transl. Med. 2020, 18, 457. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhai, H.; Ma, S.; Chen, J.; Gao, Y. Efficacy of therapeutic plasma exchange in severe COVID-19 patients. Br. J. Haematol. 2020, 190, 181–183. [Google Scholar] [CrossRef]
- Biban, P.; Standage, S.W.; Jayashree, M.; Samprathi, M. Biomarkers in COVID-19: An Up-To-Date Review. Rev. Front. Pediatr. 2020, 8, 607–647. [Google Scholar]
- Krzych, Ł.J.; Putowski, Z.; Czok, M.; Hofman, M.; Fraaij, P.L. What Is the Role of Therapeutic Plasma Exchange as an Adjunctive Treatment in Severe COVID-19: A Systematic Review. Viruses 2021, 13, 1484. [Google Scholar] [CrossRef]
- Faqihi, F.; Alharthy, A.; Abdulaziz, S.; Balhamar, A.; Alomari, A.; Al Aseri, Z. Therapeutic plasma exchange in patients with life-threatening COVID-19: A randomised controlled clinical trial. Int. J. Antimicrob. Agents 2021, 57, 106334. [Google Scholar] [CrossRef]
- Kamran, M.; Mirza, Z.E.H.; Naseem, A.; Liaqat, J.; Fazal, I.; Alamgir, W. Therapeutic plasma exchange for coronavirus disease-2019 triggered cytokine release syndrome: A retrospective propensity matched control study. PLoS ONE 2021, 16, 0244853. [Google Scholar] [CrossRef]
- Behrens, E.M.; Koretzky, G.A. Cytokine Storm Syndrome Looking Toward the Precision Medicine Era. Arthritis Rheumatol. 2017, 69, 1135–1143. [Google Scholar] [CrossRef]
- Zaid, I.; Essaad, O.; El Aidouni, G.; Aabdi, M.; Berrichi, S.; Taouihar, S. Therapeutic plasma exchange in patients with COVID-19 pneumonia in intensive care unit: Cases series. Ann. Med. Surg. 2021, 71, 102920. [Google Scholar] [CrossRef] [PubMed]
- Lionte, C.; Sorodoc, V.; Haliga, R.E.; Bologa, C.; Ceasovschih, A.; Petris, O.R.; Coman, A.E.; Stoica, A.; Sirbu, O.; Puha, G.; et al. Inflammatory and Cardiac Biomarkers in Relation with Post-Acute COVID-19 and Mortality: What We Know after Succesive Pandemic Vawes. Diagnostics 2022, 12, 1373. [Google Scholar] [CrossRef]
- Brandon Michael Henry, M.; Gaurav, A.; Johnny, W. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis. Am. J. Emerg. Med. 2020, 38, 1722–1726. [Google Scholar] [CrossRef] [PubMed]
- Hashemian, S.M.; Shafigh, N.; Afzal, G.; Jamaati, H.; Tabarsi, P.; Marjani, M. Plasmapheresis reduces cytokine and immune cell levels in COVID-19 patients with acute respiratory distress syndrome (ARDS). Pulmonology 2021, 27, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Furong, Z.; Yuzhao, H.; Ying, G.; Mingzhu, Y. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar]
- Haliga, R.E.; Sorodoc, V.; Lionte, C.; Petris, O.; Bologa, C.; Coman, A.E.; Vata, L.G.; Puha, G.; Dumitrescu, G.; Sirbu, O.; et al. Acute clinical Syndromes and Suspicion of SARS-CoV-2 Infection. The Experience of a Single Romanian Center in the early Pandemic Period. Medicina 2021, 57, 121. [Google Scholar] [CrossRef]
- Truong, A.D.; Auld, S.C.; Barker, N.A.; Friend, S.; Wynn, A.; Thanushi Cobb, J. Therapeutic plasma exchange for COVID-19-associated hyperviscosity. Transfusion 2021, 61, 1029–1034. [Google Scholar] [CrossRef]
- Gavriatopoulou, M.; Ntanasis-Stathopoulos, I.; Korompoki, E.; Fotiou, D.; Migkou, M.; Tzanninis, I.G. Emerging treatment strategies for COVID-19 infection. Clin. Exp. Med. 2021, 21, 167–179. [Google Scholar] [CrossRef]
- Gosangi, B.; Rubinowitz, A.N.; David, I.; Gange, C.; Bader, A.; Cortopassi, I. COVID-19 ARDS: A review of imaging features and overview of mechanical ventilation and its complications. Emerg. Radiol. 2022, 29, 23–34. [Google Scholar] [CrossRef]
| Age-mean (min–max) | 52.70 (21–80) |
| Body Mass Index-mean | 33.2 |
| Gender | |
| Male | 45 |
| Female | 20 |
| Days from RT-PCR COVID-19 and TPE mean, (min–max) | 16.6 (5–51) |
| Respiratory status | |
| Invasive Mechanical Ventilation | 40 |
| Noninvasive Mechanical Ventilation | 25 |
| Comorbidities (no. and % from total no. of patients) | |
| Diabetes Mellitus | 10 (15.38%) |
| Hypertension | 33 (50.76%) |
| Obesity | 27 (41.53%) |
| COPD/asthma | 6 (9.23%) |
| No. of sessions (total) | 120 |
| Patients with 1 session | 41 |
| Patients with 2 sessions | 13 |
| Patients with more than 2 sessions | 11 |
| Variable | Average/Median before TPE | Average/Median after TPE | p-Value for Median |
|---|---|---|---|
| IL-6, pg/ml | 799/129 | 480/79 | 0.0003 |
| Ferritin, µg/L | 2364/1529 | 1660/1120 | <0.0001 |
| D-dimers, µg/ml | 5.18/1.9 | 3.50/1.57 | 0.0024 |
| CRP, mg/L | 122/88 | 87/60 | 0.0001 |
| LDH, U/L | 579/512 | 461/419 | <0.0001 |
| PCT, ng/ml | 2.28/0.33 | 2.26/0.42 | 0.34 |
| Fibrinogen, g/L | 4.90/4.23 | 3.42/3.26 | <0.0001 |
| ESR, mm/h | 46/35 | 22/15 | <0.0001 |
| Leucocytes, ×103/µL | 14/13 | 16/15.5 | 0.19 |
| % Lymphocytes | 7.66/5.2 | 8.14/5.5 | 0.53 |
| Lymph abs, ×103/µL | 0.96/0.69 | 1.11/0.80 | 0.003 |
| TAM, mmHg | 80.9/77 | 81.9/80 | 0.9 |
| Temperature, °C | 36.5/36.4 | 36.6/36.4 | 0.26 |
| BUN, mg/dL | 72.7/58.5 | 74.2/62 | 0.29 |
| Creatinine, mg/dL | 1.02/0.8 | 1.08/0.81 | 0.98 |
| PH | 7.42/7.43 | 7.41/7.42 | 0.79 |
| Lactate, mmol/L | 2.49/2.30 | 2.55/2.27 | 0.72 |
| SOFA | 7.71/7 | 7.76/7 | 0.96 |
| APACHE 2 | 11.7/11 | 12.1/12 | 0.056 |
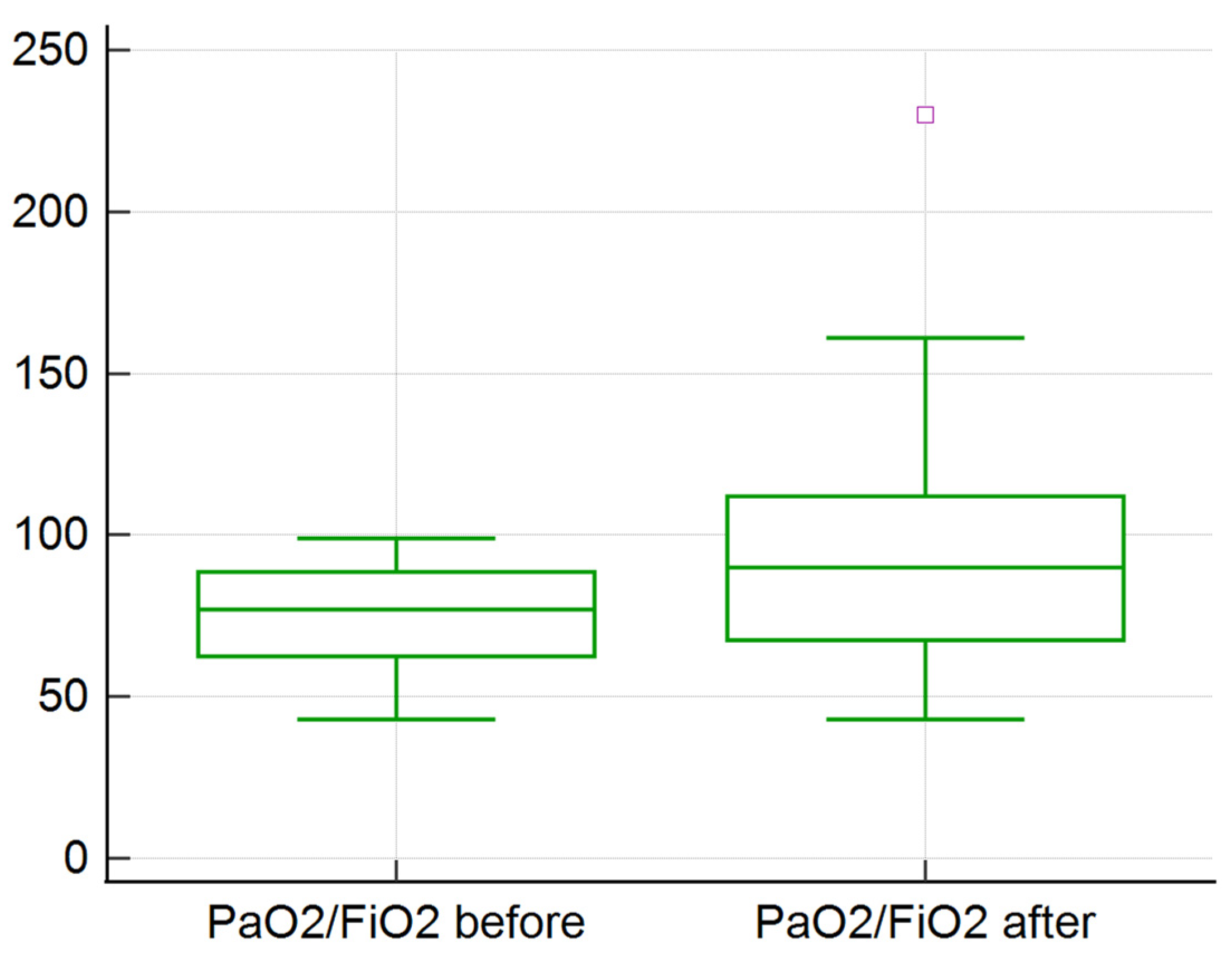
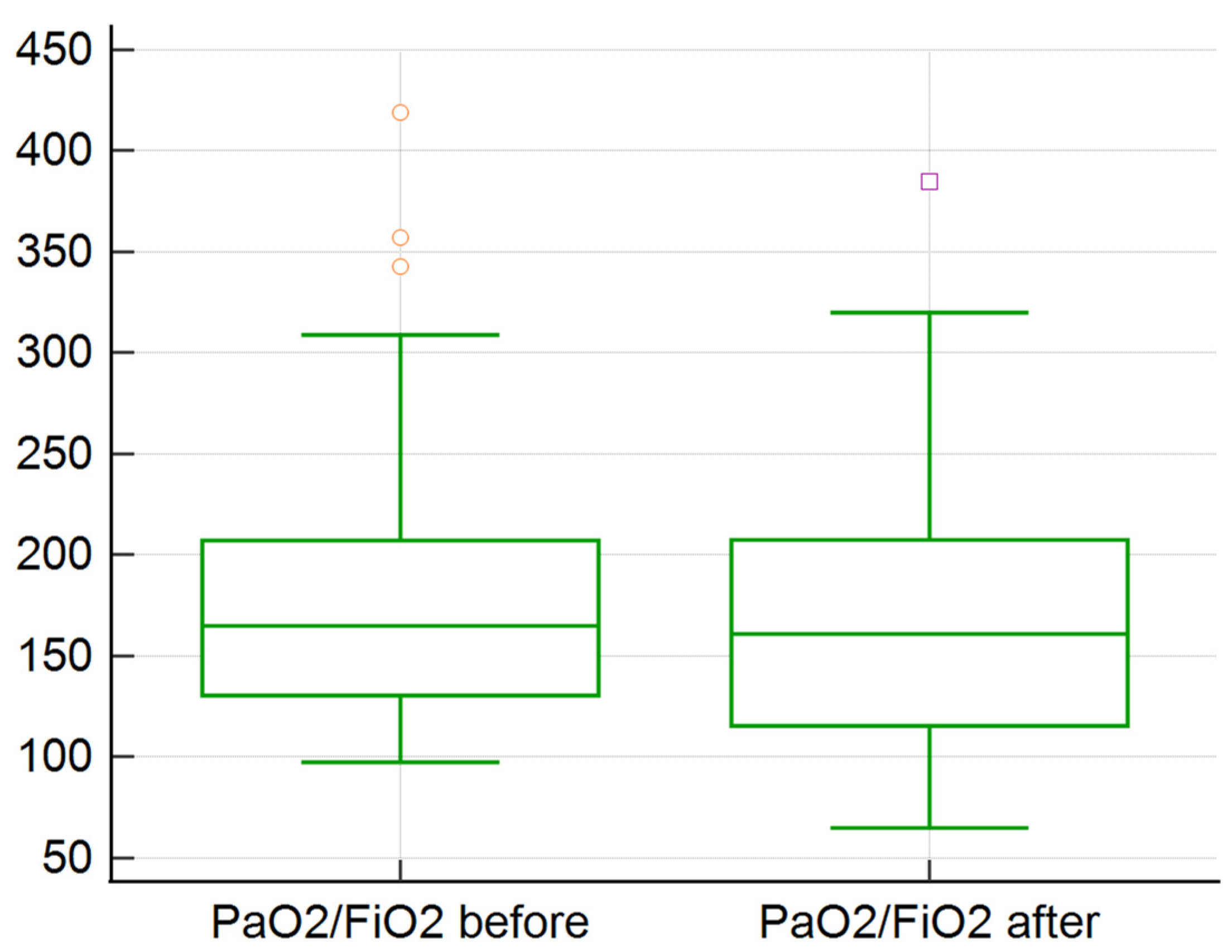
| PaO2/FiO2 | 128.1/98.25 | 131.7/113.25 | 0.23 |
| P/F < 100 for 55 sessions | 75/77 | 92/90 | 0.0002 |
| P/F ≥ 100 for 55 sessions | 184/168 | 173/162 | 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porosnicu, T.M.; Gindac, C.; Popovici, S.; Marinescu, A.; Jipa, D.; Lazaroiu, V.; Sandesc, D.; Oancea, C.; Folescu, R.; Zamfir, A.-S.; et al. Efficacy of Therapeutic Plasma Exchange in Severe Acute Respiratory Distress Syndrome in COVID-19 Patients from the Western Part of Romania. Medicina 2022, 58, 1707. https://doi.org/10.3390/medicina58121707
Porosnicu TM, Gindac C, Popovici S, Marinescu A, Jipa D, Lazaroiu V, Sandesc D, Oancea C, Folescu R, Zamfir A-S, et al. Efficacy of Therapeutic Plasma Exchange in Severe Acute Respiratory Distress Syndrome in COVID-19 Patients from the Western Part of Romania. Medicina. 2022; 58(12):1707. https://doi.org/10.3390/medicina58121707
Chicago/Turabian StylePorosnicu, Tamara Mirela, Ciprian Gindac, Sonia Popovici, Adelina Marinescu, Daniel Jipa, Valentina Lazaroiu, Dorel Sandesc, Cristian Oancea, Roxana Folescu, Alexandra-Simona Zamfir, and et al. 2022. "Efficacy of Therapeutic Plasma Exchange in Severe Acute Respiratory Distress Syndrome in COVID-19 Patients from the Western Part of Romania" Medicina 58, no. 12: 1707. https://doi.org/10.3390/medicina58121707
APA StylePorosnicu, T. M., Gindac, C., Popovici, S., Marinescu, A., Jipa, D., Lazaroiu, V., Sandesc, D., Oancea, C., Folescu, R., Zamfir, A.-S., Zamfir, C. L., Nussbaum, L. A., & Sirbu, I. O. (2022). Efficacy of Therapeutic Plasma Exchange in Severe Acute Respiratory Distress Syndrome in COVID-19 Patients from the Western Part of Romania. Medicina, 58(12), 1707. https://doi.org/10.3390/medicina58121707






