Comparison of Hybrid Abdominal Flap versus Homodigital Neurovascular Island Flap for Fingertip Amputation
Abstract
1. Background and Objectives
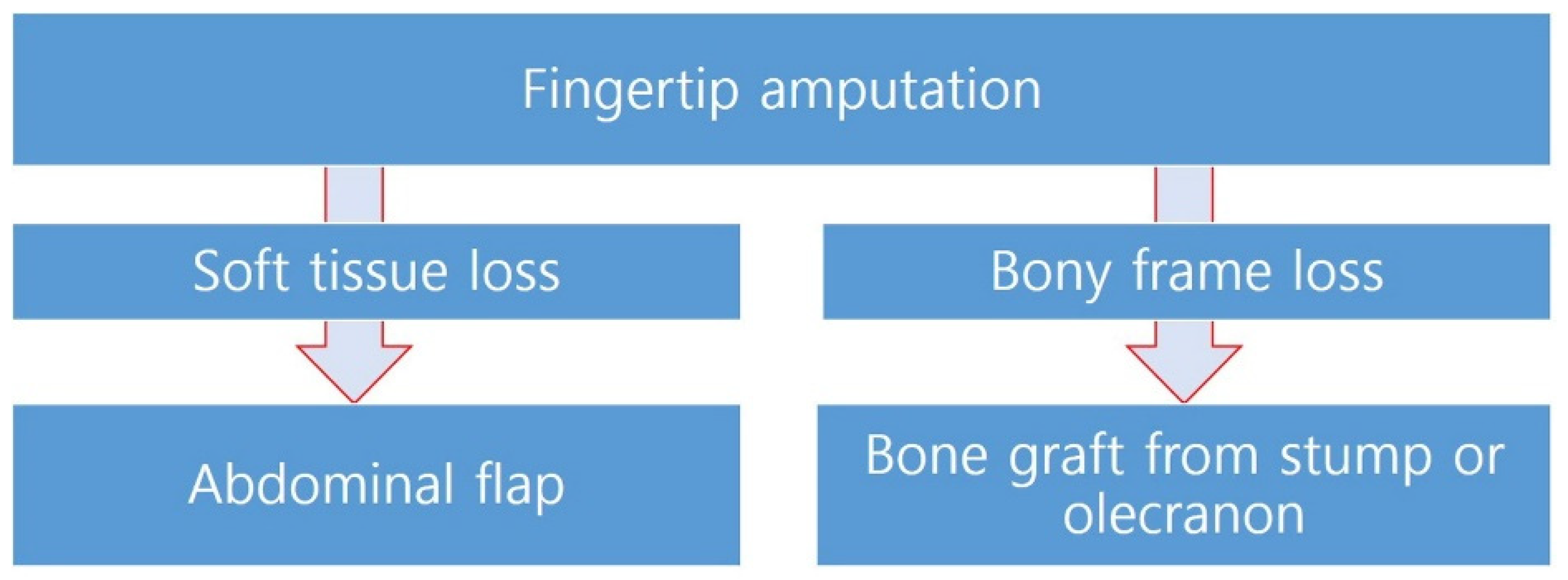
2. Materials and Methods
- Surgical Technique of the Hybrid Abdominal Flap
- Post-Division Management
- Surgical Technique of the Homodigital Neurovascular Island Flap
- The patients were placed in a supine position with the injured hand gently placed on an arm table or an arm board. The procedure was performed under tourniquet control. After measuring the defect size, a flap was drawn over either the distal ulnar or the radial aspect of the finger centered over the neurovascular bundle.
- A mid-lateral incision was then performed proximal to the outlined flap. The neurovascular bundle was dissected free of the surrounding tissues at the proximal phalangeal level. Once the neurovascular bundle was isolated, it was traced distally toward the base of the flap. Once the flap was confirmed directly over the pedicle, the central or volar aspect of the flap was then incised and dissected down to the flexor tendon sheath. The dissection proceeded under the flap in a central to lateral fashion, freeing the flap from the flexor tendon sheath. After the completion of the neurovascular bundle dissection, the flap was advanced and inserted into the area of deficit at the tip and sutured with fine absorbable sutures. A full-thickness skin graft was then harvested from the donor site of preference and used for coverage of the donor defect.
- After the completion of the surgical procedure, a customized short-arm splint was used for flap stabilization.
3. Results
3.1. Case Reports
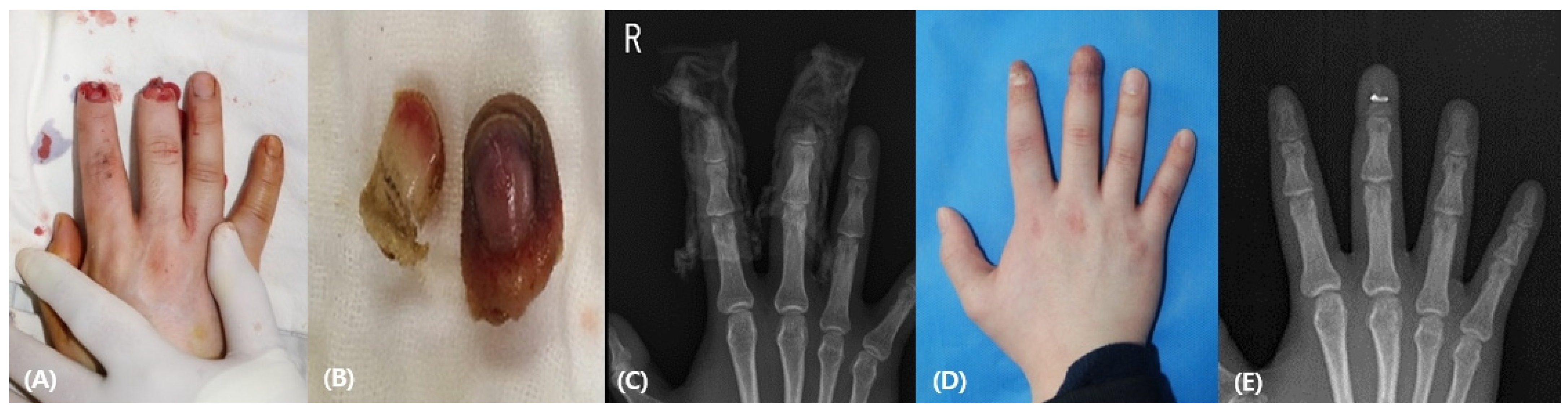
3.1.1. Patient 1
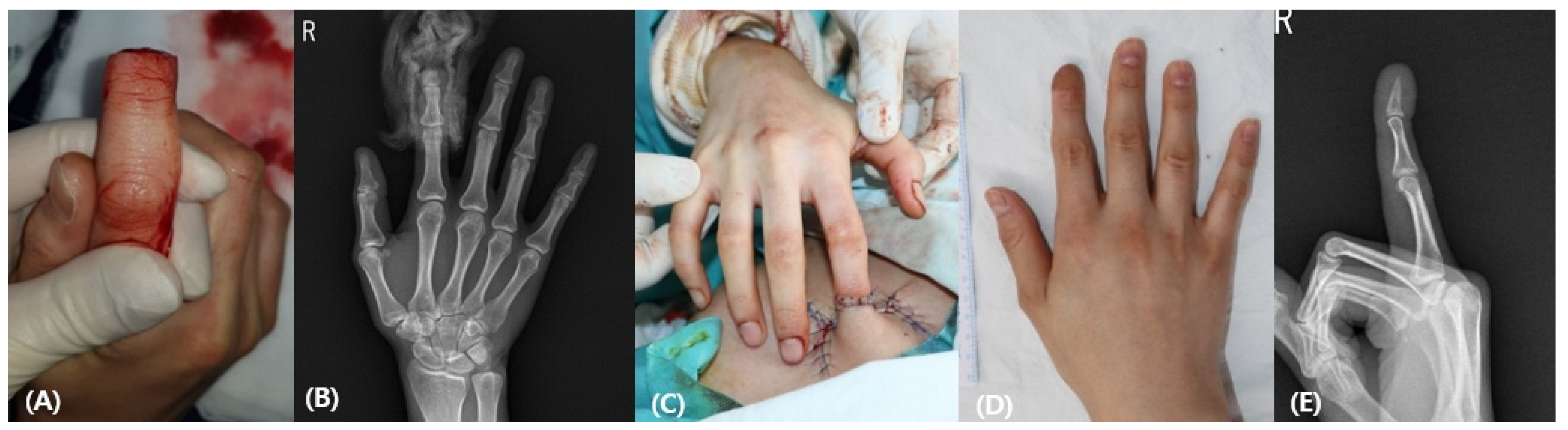
3.1.2. Patient 2
3.1.3. Patient 3
3.1.4. Patient 4
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Win, T.S.; Henderson, J. Management of traumatic amputations of the upper limb. BMJ 2014, 348, g255. [Google Scholar] [CrossRef] [PubMed]
- Shauver, M.J.; Nishizuka, T.; Hirata, H.; Chung, K.C. Traumtic finger amputation treatment preference among hand surgeons in the United states and Japan. Plast. Reconstr. Surg. 2016, 137, 1193–1202. [Google Scholar] [CrossRef]
- Sebastin, S.J.; Chung, K.C. A systemic review of the outcomes of replantation of distal digital amputation. Plast. Reconstr. Surg. 2011, 128, 723–737. [Google Scholar] [CrossRef] [PubMed]
- Borman, H.; Maral, T.; Tancer, M. Fingertip reconstruction using two variations of direct-flow homodigital neurovascular island flaps. Ann. Plast. Surg. 2000, 45, 24–30. [Google Scholar] [CrossRef]
- Foucher, G.; Khouri, R.K. Digital reconstruction with island flaps. Clin. Plast. Surg. 1997, 24, 1–32. [Google Scholar] [CrossRef]
- Nakanishi, A.; Omokawa, S.; Iida, A.; Kaji, D.; Tanaka, Y. Predictors of proximal interphalangeal joint flexion contracture after homodigital island flap. J. Hand Surg. Am. 2015, 40, 2155–2159. [Google Scholar] [CrossRef] [PubMed]
- Sano, K.; Ozeki, S.; Kimura, K.; Hyakusoku, H. Relationship between sensory recovery and advancement distance of oblique triangular flap for fingertip reconstruction. J. Hand Surg. Am. 2008, 33, 1088–1092. [Google Scholar] [CrossRef] [PubMed]
- Usami, S.; Kawahara, S.; Yamaguchi, Y.; Hirase, T. Homodigital artery flap reconstruction for fingertip amputation: A comparative study of the oblique triangular neurovascular advancement flap and the reverse digital artery island flap. J. Hand Surg. 2015, 40, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Varitimidis, S.E.; Dailiana, Z.H.; Zibis, A.H.; Hantes, M.; Bargiotas, K.; Malizos, K.N. Restoration of function and sensitivity utilizing a homodigital neurovascular island flap after amputation injuries of the fingertip. J. Hand Surg. Br. 2005, 30, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Adani, R.; Busa, R.; Castagnetti, C.; Bathia, A.; Caroli, A. Homodigital neurovascular island flaps with “direct flow” vascularization. Ann. Plast. Surg. 1997, 38, 36–40. [Google Scholar] [CrossRef]
- Evans, D.M.; Martin, D.L. Step-advancement island flap for fingertip reconstruction. Br. J. Plast. Surg. 1988, 41, 105–111. [Google Scholar] [CrossRef]
- Katz, R.D. The anterograde homodigital neurovascular island flap. J. Hand Surg. Am. 2013, 38, 1226–1233. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, J.C.; Sullivan, J.G.; Baibak, G.J.; Deab, R.K. Use of a tailored abdominal pedicle flap for surgical reconstruction of the hand. J. Bone Jt. Surg. 1970, 52, 1552–1562. [Google Scholar] [CrossRef]
- Waikakul, S.; Sakkarnkosol, S.; Vanadurongwan, V.; Un-nanuntana, A. Results of 1018 digital replantations in 552 patients. Injury 2000, 31, 33–40. [Google Scholar] [CrossRef]
- Matsuzaki, H.; Yoshizu, T.; Maki, Y.; Tsubokawa, N. Functional and cosmetic results of fingertip replantation: Anastomosing only the digital artery. Ann. Plast. Surg. 2004, 53, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Aydyn, N.; Lin, Y.T.; Hsu, C.T.; Lin, C.H.; Yeh, J.T. Hand and finger replantation after protracted ischemia (more than 24 hours). Ann. Plast. Surg. 2010, 64, 286–290. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, Y.M. Fingertip Replantation Using Y-Shaped Vein Graft to Pulp Artery. Ann. Plast. Surg. 2015, 75, 424–429. [Google Scholar] [CrossRef]
- Joshi, R.; Duong, H. Anatomy, Abdomen and Pelvis, Scarpa Fascia; StatPearls. Available online: https://www.ncbi.nlm.nih.gov/books/NBK553137 (accessed on 11 August 2021).
- Hester, T.R., Jr.; Nahai, F.; Beegle, P.E.; Bostwick, J., 3rd. Blood supply of the abdomen revisited, with emphasis on the superficial inferior epigastric artery. Plast. Reconstr. Surg. 1984, 74, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Boyd, J.B.; Taylor, G.I.; Corlett, R. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast. Reconstr. Surg. 1984, 73, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Acharya, A.M.; Ravikiran, N.; Jayakrishnan, K.N.; Bhat, A.K. The role of pedicled abdominal flaps in hand and forearm composite tissue injuries: Results of technical refinements for safe harvest. J. Orthop. 2019, 16, 369–376. [Google Scholar] [CrossRef]
- Al-Qattan, M.M.; Alammar, A.K.; Alfaqeeh, F.A.; Altamimi, L.A.; Alfehaid, N.S.; Mahabbat, N.A.; Pant, R. Pedicled Abdominal Flaps for Hand Reconstruction in Adults: Physiotherapy of the Attached Hand. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3474. [Google Scholar] [CrossRef]
- Ercin, B.S.; Kabakas, F.; Keles, M.K.; Ozcelik, I.B.; Mersa, B. Olecranon bone grafting for the treatment of nonunion after distal finger replantation. Plast. Aesthetic Res. 2020, 7, 38. [Google Scholar] [CrossRef]
- Arrington, E.D.; Smith, W.J.; Chambers, H.G.; Bucknell, A.L.; Davino, N.A. Complications of iliac crest bone graft harvesting. Clin. Orthop. Relat. Res. 1996, 329, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.C.; Watson, K.; Joseph, E.; Garcia, J.; Wollstein, R. Long-term complications of distal radius bone grafts. J. Hand Surg. Am. 2003, 28, 784–788. [Google Scholar] [CrossRef]
- Mersa, B.; Ozcelik, I.B.; Kabakas, F.; Sacak, B.; Aydin, A. Olecranon bone graft: Revisited. Tech. Hand Extrem. Surg. 2010, 14, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.D.; Zhang, Y.Z.; Bi, W.D.; Wu, T. Functional sensory function recovery of random-pattern abdominal skin flap in the repair of fingertip skin defects. Exp. Ther. Med. 2013, 5, 830–834. [Google Scholar] [CrossRef] [PubMed]


| HAF Group | HNIF Group | p Value | ||
|---|---|---|---|---|
| Age of patients | 39.2 | 37.8 | 0.794 | |
| Number of fingertips | Index | 6 | 5 | |
| Middle | 2 | 3 | ||
| Ring | 1 | - | ||
| Little | 2 | 1 | ||
| Donor site | Stump | 7 | - | |
| Olecranon | 4 | - | ||
| Operative time (min) | 43 | 38 | ||
| Flap survival | 11 | 9 | 0.803 | |
| ROM of DIP joint (degree) | Reconstructed | 76.2 ± 4.8 | 70.3 ± 5.7 | 0.031 |
| Contralateral | 77.8 ± 5.2 | 78.2 ± 6.1 | - | |
| ROM of PIP joint (degree) | Reconstructed | 97.4 ± 3.4 | 94.7 ± 2.8 | 0.268 |
| Contralateral | 98.2 ± 4.5 | 97.5 ± 5.2 | - | |
| Static 2-PD (mm) | Reconstructed | 7.9 ± 1.3 | 7.3 ± 2.1 | 0.565 |
| Contralateral | 3.6 ± 0.4 | 3.5 ± 0.5 | ||
| Scar assessment (VSS) | 1.4 | 2.6 | 0.012 | |
| CISS score | Reconstructed | 31.4 | 30.8 | 0.547 |
| Contralateral | 11.6 ± 2.9 | 11.9 ± 1.8 | 0.982 | |
| ANA score | 6.60 | 3.17 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.H.; Kim, T.H.; Park, J.H. Comparison of Hybrid Abdominal Flap versus Homodigital Neurovascular Island Flap for Fingertip Amputation. Medicina 2022, 58, 1483. https://doi.org/10.3390/medicina58101483
Kim YH, Kim TH, Park JH. Comparison of Hybrid Abdominal Flap versus Homodigital Neurovascular Island Flap for Fingertip Amputation. Medicina. 2022; 58(10):1483. https://doi.org/10.3390/medicina58101483
Chicago/Turabian StyleKim, Yung Hoon, Tae Hyung Kim, and Jun Ho Park. 2022. "Comparison of Hybrid Abdominal Flap versus Homodigital Neurovascular Island Flap for Fingertip Amputation" Medicina 58, no. 10: 1483. https://doi.org/10.3390/medicina58101483
APA StyleKim, Y. H., Kim, T. H., & Park, J. H. (2022). Comparison of Hybrid Abdominal Flap versus Homodigital Neurovascular Island Flap for Fingertip Amputation. Medicina, 58(10), 1483. https://doi.org/10.3390/medicina58101483






