Large Duodenal Hematoma Causing an Ileus after an Endoscopic Duodenal Biopsy in a 6-Year-Old Child: A Case Report
Abstract
1. Introduction
2. Methods
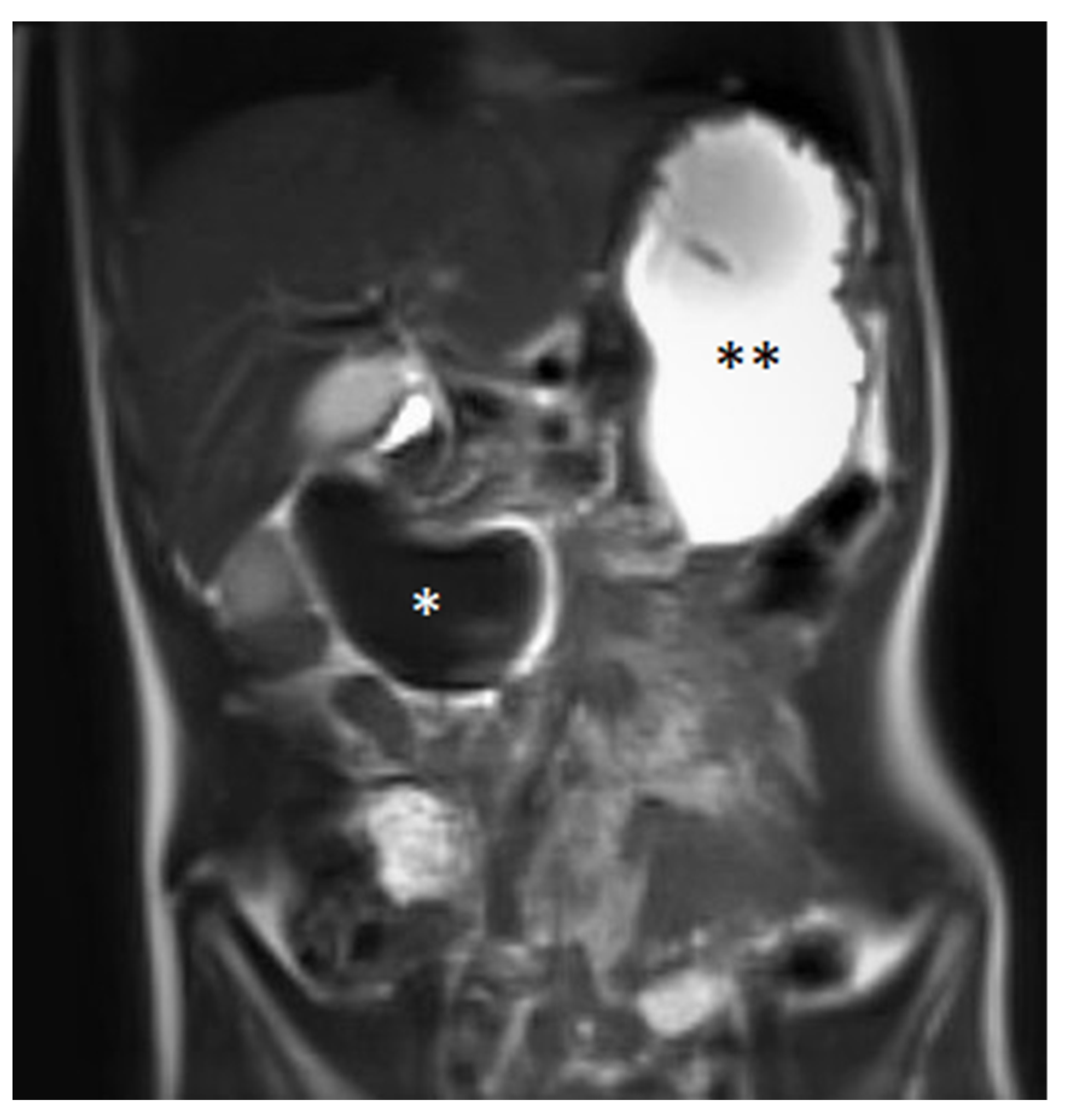
3. Case Report
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grasshof, C.; Wolf, A.; Neuwirth, F.; Posovszky, C. Intramural duodenal haematoma after endoscopic biopsy: Case report and review of the literature. Case Rep. Gastroenterol. 2012, 6, 5–14. [Google Scholar] [CrossRef]
- Yamazawa, K.; Yamada, Y.; Kuroda, T.; Mutai, H.; Matsunaga, T.; Komiyama, O.; Takahashi, T. Spontaneous intramural duodenal hematoma as the manifestation of Noonan syndrome. Am. J. Med. Genet. Part A 2018, 176, 496–498. [Google Scholar] [CrossRef] [PubMed]
- D’Arpa, F.; Orlando, G.; Tutino, R.; Salamone, G.; Battaglia, E.O.; Gulotta, G. Traumatic isolated intramural duodenal hematoma causing intestinal obstruction. ACG Case Rep. J. 2015, 2, 198–199. [Google Scholar] [CrossRef] [PubMed]
- Hoenisch, K.; Prommegger, R.; Schwaighofer, H.; Freund, M.; Schocke, M.; Vogel, W.; Kaser, A. Intramural duodenal hematoma after upper gastrointestinal endoscopy. Wien Med. Wochenschr. 2011, 161, 441–444. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.C.; Ravindranathan, S.; Choksi, V.; Kattalan, J.P.; Shankar, U.; Kaplan, S. Intraoperative Gastric Intramural Hematoma: A Rare Complication of Percutaneous Endoscopic Gastrostomy. Am. J. Case Rep. 2016, 17, 963–966. [Google Scholar] [CrossRef]
- Sadio, A.; Peixoto, P.; Cancela, E.; Castanheira, A.; Marques, V.; Ministro, P.; Silva, A.; Caldas, A. Intramural hematoma: A rare complication of endoscopic injection therapy for bleeding peptic ulcers. Endoscopy 2011, 43 (Suppl. 2), E141–E142. [Google Scholar] [CrossRef] [PubMed]
- Dibra, A.; Këlliçi, S.; Çeliku, E.; Draçini, X.; Maturo, A.; Çeliku, E. Intramural duodenal hematoma after submucosal injection of epinephrine for a bleeding ulcer: Case report and review. G. Chir. 2015, 36, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Y.; Ma, C.J.; Tsai, H.L.; Wu, D.-C.; Chen, C.-Y.; Huang, T.-J.; Hsieh, J.-S. Intramural duodenal hematoma and hemoperitoneum in anticoagulant therapy following upper gastrointestinal endoscopy. Med. Princ. Pract. 2006, 15, 453–455. [Google Scholar] [CrossRef]
- Eichele, D.D.; Ross, M.; Tang, P.; Hutchins, G.F.; Mailliard, M. Spontaneous intramural duodenal hematoma in type 2B von Willebrand disease. World J. Gastroenterol. 2013, 19, 7205–7208. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.H.B.; Esper, R.S.; Ocariz, R.C.; Sartori, F.S.; Freire, L.M.D.; Chaim, E.A.; Callejas-Neto, F.; Cazzo, E. Intramural duodenal hematoma secondary to pancreatitis: Case report and review of the literature. Sao Paulo Med. J. 2018, 136, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Kitadani, J.; Yamade, N.; Nakai, H.; Shima, K. Intramural duodenal haematoma caused by pancreatic fistula due to exacerbation of chronic pancreatitis. BMJ Case Rep. 2018, 2018, bcr-2017. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; The CARE Group. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. Dtsch. Arztebl. Int. 2013, 110, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Equator Network. Available online: http://www.equator-network.org/reporting-guidelines/care (accessed on 15 December 2020).
- Iqbal, C.W.; Askegard-Giesmann, J.R.; Pham, T.H.; Ishitani, M.B.; Moir, C.R. Pediatric endoscopic injuries: Incidence, management, and outcomes. J. Pediatr. Surg. 2008, 43, 911–915. [Google Scholar] [CrossRef]
- Gaines, B.A.; Shultz, B.S.; Morrison, K.; Ford, H.R. Duodenal injuries in children: Beware of child abuse. J. Pediatr. Surg. 2004, 39, 600–602. [Google Scholar] [CrossRef]
- Sahn, B.; Anupindi, S.A.; Dadhania, N.J.; Kelsen, J.R.; Nance, M.L.; Mamula, P. Duodenal Hematoma Following EGD. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Sierra, A.; Ecochard-Dugelay, E.; Bellaïche, M.; Tilea, B.; Cavé, H.; Viala, J. Biopsy-Induced Duodenal Hematoma Is Not an Infrequent Complication Favored by Bone Marrow Transplantation. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 627–632. [Google Scholar] [CrossRef]
- Bergero, G.; Frangi, D.; Lerendegui, L.; Busoni, V.; Lobos, P.A.; Orsi, M.; Llera, J. Duodenal hematoma after upper gastrointestinal endoscopy in pediatric graft vs host disease: Report of two cases. Arch. Argent. Pediatr. 2021, 119, e513–e517. [Google Scholar] [CrossRef]
- Dumitriu, D.; Menten, R.; Smets, F.; Clapuyt, P. Postendoscopic duodenal hematoma in children: Ultrasound diagnosis and follow-up. J. Clin. Ultrasound 2014, 42, 550–553. [Google Scholar] [CrossRef] [PubMed]
- Homma, Y.; Mori, K.; Ohnishi, Y.; Fujioka, K.; Terada, T.; Sasaki, A.; Nagai, T.; Inoue, M. Ultrasound follow-up in a patient with intestinal obstruction due to post-traumatic intramural duodenal hematoma. J. Med. Ultrason. 2016, 43, 431–434. [Google Scholar] [CrossRef]
- Mego, M.; Lugo, N.; Roura, J.; Saperas, E. Duodenal obstruction due to intramural haematoma as a complication of endoscopic biopsy. Gastroenterol. Y Hepatol. (Engl. Ed.) 2019, 42, 381–382. [Google Scholar] [CrossRef]
- Zinelis, S.A.; Hershenson, L.M.; Ennis, M.F.; Boller, M.; Ismail-Beigi, F. Intramural duodenal hematoma following upper gastrointestinal endoscopic biopsy. Dig. Dis. Sci. 1989, 34, 289–291. [Google Scholar] [CrossRef]
- Niehues, S.M.; Denecke, T.; Bassir, C.; Hamm, B.; Haas, M. Intramural duodenal hematoma: Clinical course and imaging findings. Acta Radiol. Open 2019, 8, 2058460119836256. [Google Scholar] [CrossRef]
- Szajewska, H.; Albrecht, P.; Ziolkowski, J.; Kubica, W. Intramural duodenal hematoma: An unusual complication of duodenal biopsy sampling. J. Pediatr. Gastroenterol. Nutr. 1993, 16, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.I.; Choi, K.H.; Ko, E.H.; Lee, J.H.; Song, Y.J.; Ko, K.H.; Hong, S.P.; Park, P.W. A case of duodenal intramural hematoma treated by percutaneous external drainage. Korean J. Gastroenterol. 2007, 49, 45–49. [Google Scholar] [PubMed]
- Kim, S.J.; Lee, J.H.; Park, S.M.; Kwon, K.H. Conservative management of traumatic acute intramural hematoma of duodenal 2nd and 3rd portion: A case report and review of literature. Ann. Hepatobiliary Pancreat. Surg. 2020, 24, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Guzman, C.; Bousvaros, A.; Buonomo, C.; Nurko, S. Intra-duodenal hematoma complicating intestinal biopsy: Case reports and review of the literature. Am. J. Gastroenterol. 1998, 93, 2547–2550. [Google Scholar] [CrossRef]
- Kwon, C.I.; Ko, K.H.; Kim, H.Y.; Hong, S.P.; Hwang, S.G.; Park, P.W.; Rim, K.S. Bowel obstruction caused by an intramural duodenal hematoma: A case report of endoscopic incision and drainage. J. Korean Med. Sci. 2009, 24, 179–183. [Google Scholar] [CrossRef]
- Elmoghazy, W.; Noaman, I.; Mahfouz, A.E.; Elaffandi, A.; Khalaf, H. Surgical management of complicated intra-mural duodenal hematoma: A case-report and review of literature. Int. J. Surg. Case Rep. 2015, 17, 103–105. [Google Scholar] [CrossRef][Green Version]
- Yang, J.C.; Rivard, D.C.; Morello, F.P.; Ostlie, D.J. Successful percutaneous drainage of duodenal hematoma after blunt trauma. J. Pediatr. Surg. 2008, 43, e13–e15. [Google Scholar] [CrossRef]
- Nolan, G.J.; Bendinelli, C.; Gani, J. Laparoscopic drainage of an intramural duodenal haematoma: A novel technique and review of the literature. World J. Emerg. Surg. 2011, 6, 42–46. [Google Scholar] [CrossRef]
- Samra, M.; Al-Mouradi, T.; Berkelhammer, C. Gastric Outlet Obstruction due to Intramural Duodenal Hematoma after Endoscopic Biopsy: Possible Therapeutic Role of Endoscopic Dilation. Case Rep. Gastroenterol. 2018, 12, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, K.; Tokuyama, H.; Yonezawa, T.; Doi, M.; Matsuzono, Y.; Matumoto, M.; Uragami, K.; Nishioka, S.; Yataka, I. A case of traumatic intramural hematoma of the duodenum effectively treated with ultrasonically guided aspiration drainage and endoscopic balloon catheter dilation. Gastroenterol. Jpn. 1991, 26, 218–223. [Google Scholar] [CrossRef]
- Dunkin, D.; Benkov, K.J.; Rosenberg, H.K. Duodenal and rectal hematomas complicating endoscopic biopsy: Use of sonography in pediatrics. J. Ultra-Sound Med. 2009, 28, 1575–1580. [Google Scholar] [CrossRef] [PubMed]
- Ben-Menachem, T.; Decker, G.A.; Early, D.S.; Evans, J.; Fanelli, R.D.; Fisher, D.A.; Fisher, L.; Fukami, N.; Hwang, J.H.; Ikenberry, S.O.; et al. ASGE Standards of Practice Committee. Gastrointest. Endosc. 2012, 76, 707–718. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiller, B.; Radke, M.; Hauenstein, C.; Müller, C.; Spang, C.; Reuter, D.A.; Däbritz, J.; Ehler, J. Large Duodenal Hematoma Causing an Ileus after an Endoscopic Duodenal Biopsy in a 6-Year-Old Child: A Case Report. Medicina 2022, 58, 12. https://doi.org/10.3390/medicina58010012
Schiller B, Radke M, Hauenstein C, Müller C, Spang C, Reuter DA, Däbritz J, Ehler J. Large Duodenal Hematoma Causing an Ileus after an Endoscopic Duodenal Biopsy in a 6-Year-Old Child: A Case Report. Medicina. 2022; 58(1):12. https://doi.org/10.3390/medicina58010012
Chicago/Turabian StyleSchiller, Benjamin, Michael Radke, Christina Hauenstein, Carsten Müller, Christian Spang, Daniel A. Reuter, Jan Däbritz, and Johannes Ehler. 2022. "Large Duodenal Hematoma Causing an Ileus after an Endoscopic Duodenal Biopsy in a 6-Year-Old Child: A Case Report" Medicina 58, no. 1: 12. https://doi.org/10.3390/medicina58010012
APA StyleSchiller, B., Radke, M., Hauenstein, C., Müller, C., Spang, C., Reuter, D. A., Däbritz, J., & Ehler, J. (2022). Large Duodenal Hematoma Causing an Ileus after an Endoscopic Duodenal Biopsy in a 6-Year-Old Child: A Case Report. Medicina, 58(1), 12. https://doi.org/10.3390/medicina58010012





