A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities
Abstract
1. Introduction
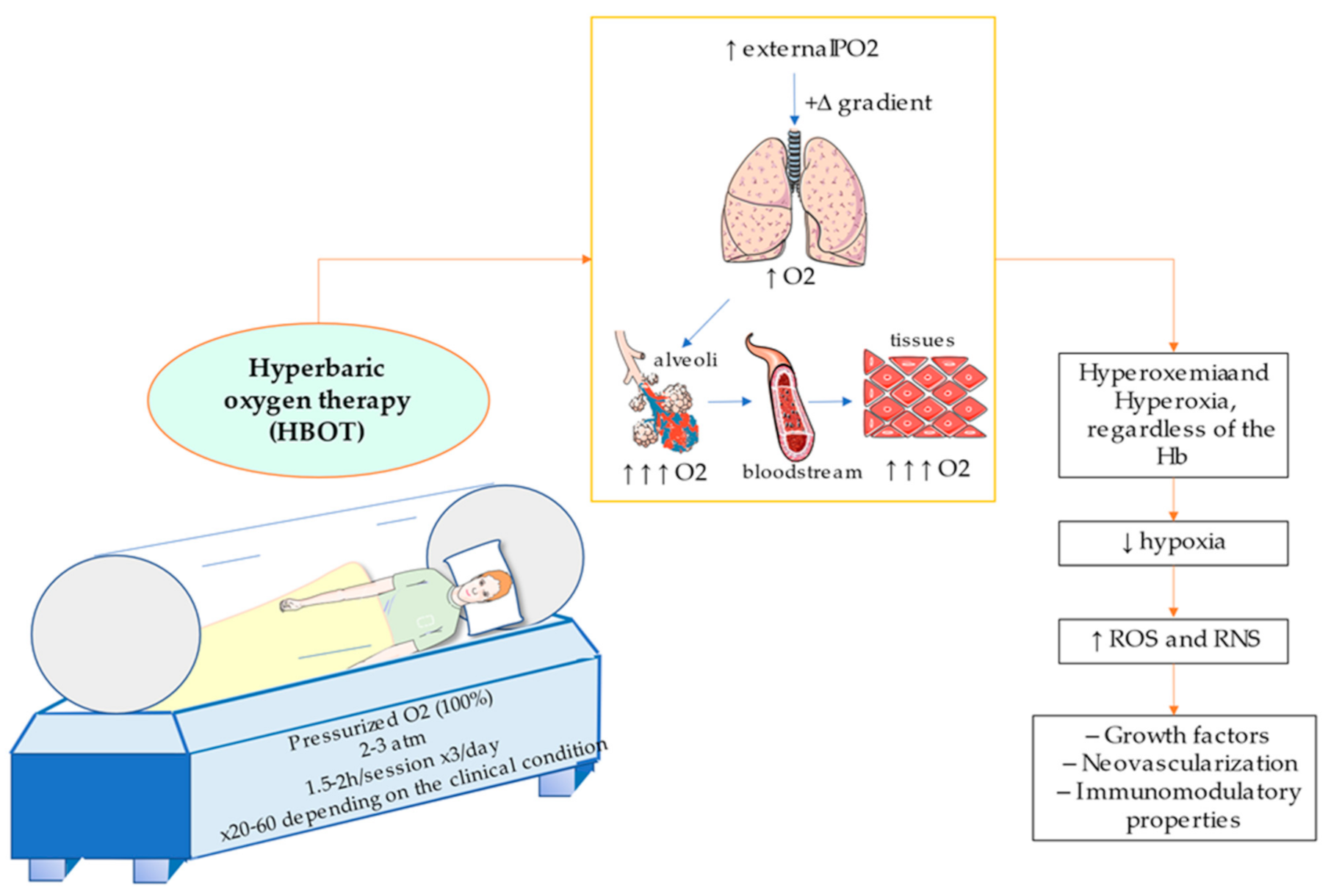
2. Physiological Role of Oxygen in the Organism
3. Principles of Hyperbaric Oxygen Therapy. Therapeutical Basis
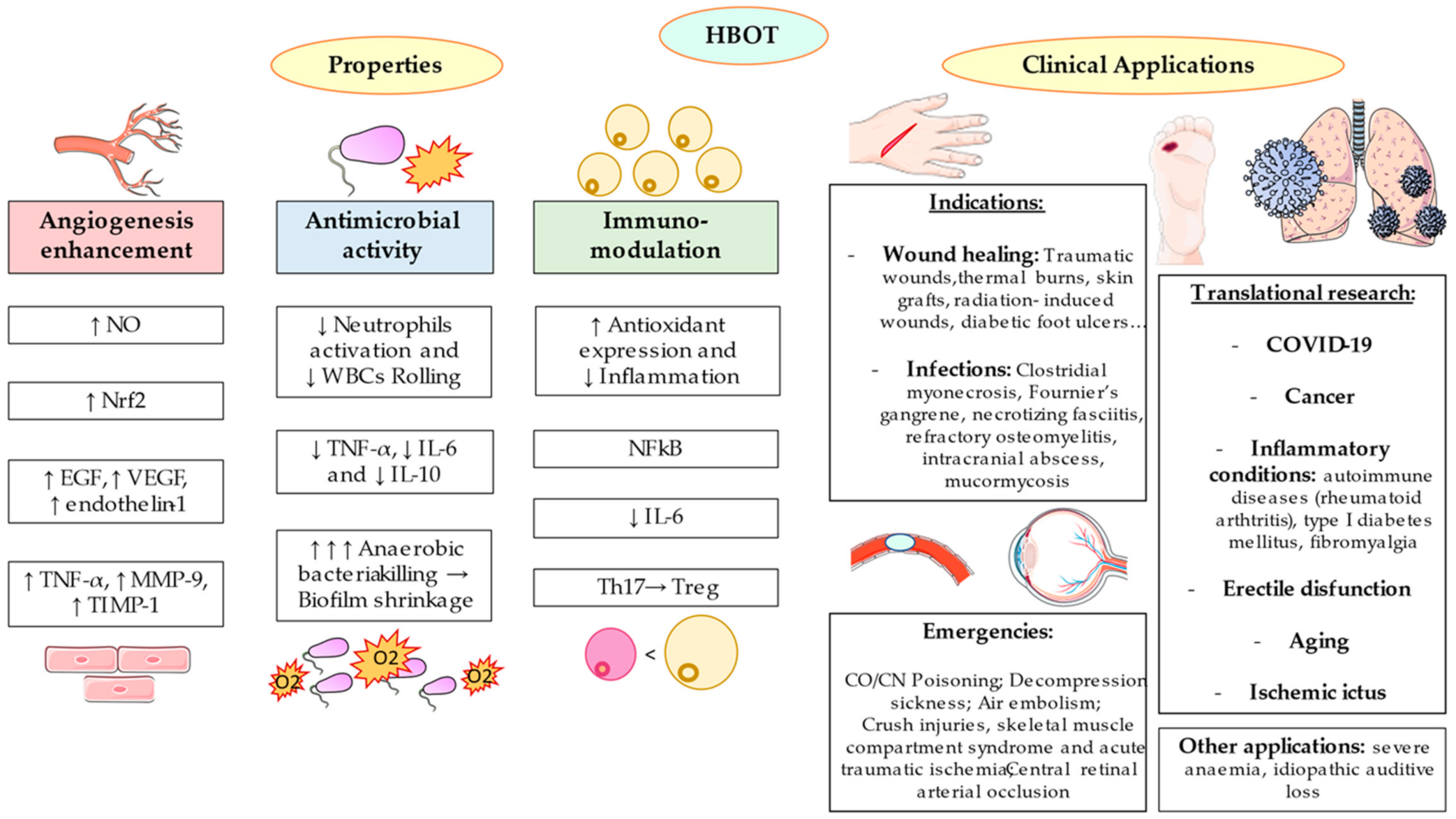
4. Approved Indications for HBOT
4.1. HBOT and Wound Healing: The Angiogenesis Enhancement
4.2. HBOT and Infections: The Antimicrobial Activity
4.3. HBOT in Medical Emergencies
5. Translational and Potential Applications of HBOT
5.1. HBOT and Inflammation: Immunomodulatory Properties
5.2. Role of HBOT in the COVID-19 Pandemic
5.3. HBOT and Cancer
5.4. Other Applications
6. Adverse Effects and Contraindications
7. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- HBO Indications—Undersea & Hyperbaric Medical Society. Available online: https://www.uhms.org/resources/hbo-indications.html# (accessed on 3 April 2021).
- UHMS Position Statement: Low-Pressure Fabric Hyperbaric Chambers Title: Low-Pressure Fabric Hyperbaric Chambers. 2017. Available online: https://www.uhms.org/images/Position-Statements/UHMS_Position_Statement_LP_chambers_revised.pdf (accessed on 23 May 2021).
- Edwards, M.L. Hyperbaric Oxygen Therapy. Part 1: History and Principles. J. Vet. Emergy Crit. Care 2010, 20, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Dejours, P.; Dejours, S. The Effects of Barometric Pressure According to Paul Bert: The Question Today. Int. J. Sports Med. 1992, 13, S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Hedley-Whyte, J. Pulmonary Oxygen Toxicity: Investigation and Mentoring. Ulst. Med. J. 2008, 77, 39–42. [Google Scholar]
- Jones, M.W.; Wyatt, H.A. Hyperbaric, Physics; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Moon, R.E.; Camporesi, E.M. Hyperbaric Oxygen Therapy: From the Nineteenth to the Twenty-First Century. Respir. Care Clin. N. Am. 1999, 5, 1–5. [Google Scholar]
- Mathieu, D.; Marroni, A.; Kot, J. Tenth European Consensus Conference on Hyperbaric Medicine: Recommendations for Accepted and Non-Accepted Clinical Indications and Practice of Hyperbaric Oxygen Treatment. Diving Hyperb. Med. 2017, 47, 24–31. [Google Scholar] [CrossRef]
- Trayhurn, P. Oxygen—The Forgotten Nutrient. J. Nutr. Sci. 2017, 6, e47. [Google Scholar] [CrossRef]
- Martin, W.F.; Garg, S.; Zimorski, V. Endosymbiotic Theories for Eukaryote Origin. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140330. [Google Scholar] [CrossRef]
- Trayhurn, P. Oxygen—A Critical, but Overlooked, Nutrient. Front. Nutr. 2019, 6, 10. [Google Scholar] [CrossRef]
- Butler, J.P.; Tsuda, A. Transport of Gases between the Environment and Alveoli-Theoretical Foundations. Compr. Physiol. 2011, 1, 1301–1316. [Google Scholar] [CrossRef]
- Harris, R.S. Pressure-Volume Curves of the Respiratory System. Respir. Care 2005, 50, 78–99. [Google Scholar]
- Pittman, R.N. Oxygen Gradients in the Microcirculation. Acta Physiol. 2011, 202, 311–322. [Google Scholar] [CrossRef]
- Gossman, W.; Alghoula, F.; Berim, I. Anoxia (Hypoxic Hypoxia); StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Choudhry, H.; Harris, A.L. Advances in Hypoxia-Inducible Factor Biology. Cell Metab. 2018, 27, 281–298. [Google Scholar] [CrossRef]
- Soares, M.J.; Iqbal, K.; Kozai, K. Hypoxia and Placental Development. Birth Defects Res. 2017, 109, 1309–1329. [Google Scholar] [CrossRef]
- Navarrete-Opazo, A.; Mitchell, G.S. Therapeutic Potential of Intermittent Hypoxia: A Matter of Dose. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2014, 307, R1181–R1197. [Google Scholar] [CrossRef]
- Chen, P.S.; Chiu, W.T.; Hsu, P.L.; Lin, S.C.; Peng, I.C.; Wang, C.Y.; Tsai, S.J. Pathophysiological Implications of Hypoxia in Human Diseases. J. Biomed. Sci. 2020, 27, 63. [Google Scholar] [CrossRef]
- Horner, D.; O’Driscoll, R. Oxygen Therapy for Medical Patients. BMJ 2018, 363. [Google Scholar] [CrossRef]
- Daste, T. The Oxygen Therapy. Prat. Vet 2013, 20, 30–32. [Google Scholar] [CrossRef]
- Lee, J.W.; Ko, J.; Ju, C.; Eltzschig, H.K. Hypoxia Signaling in Human Diseases and Therapeutic Targets. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef]
- Macintyre, N.R. Tissue Hypoxia: Implications for the Respiratory Clinician. Respir. Care 2014, 59, 1590–1596. [Google Scholar] [CrossRef]
- Choudhury, R. Hypoxia and Hyperbaric Oxygen Therapy: A Review. Int. J. Gen. Med. 2018, 11, 431–442. [Google Scholar] [CrossRef]
- Kirby, J.P.; Snyder, J.; Schuerer, D.J.E.; Peters, J.S.; Bochicchio, G. V Essentials of Hyperbaric Oxygen Therapy: 2019 Review. Mol. Med. 2019, 116, 176–179. [Google Scholar]
- Lind, F. A pro/Con Review Comparing the Use of Mono- and Multiplace Hyperbaric Chambers for Critical Care. Diving Hyperb. Med. 2015, 45, 56–60. [Google Scholar]
- Weaver, L.K. Monoplace Hyperbaric Chamber Use of U.S. Navy Table 6: A 20-Year Experience. Undersea Hyperb. Med. 2006, 33, 85. [Google Scholar]
- Lam, G.; Fontaine, R.; Ross, F.L.; Chiu, E.S. Hyperbaric Oxygen Therapy: Exploring the Clinical Evidence. Adv. Ski. Wound Care 2017, 30, 181–190. [Google Scholar] [CrossRef]
- Harch, P.G.; Andrews, S.R.; Fogarty, E.F.; Amen, D.; Pezzullo, J.C.; Lucarini, J.; Aubrey, C.; Taylor, D.V.; Staab, P.K.; Van Meter, K.W. A Phase I Study of Low-Pressure Hyperbaric Oxygen Therapy for Blast-Induced Post-Concussion Syndrome and Post-Traumatic Stress Disorder. J. Neurotrauma 2012, 29, 168–185. [Google Scholar] [CrossRef]
- Izquierdo-Alventosa, R.; Inglés, M.; Cortés-Amador, S.; Gimeno-Mallench, L.; Sempere-Rubio, N.; Chirivella, J.; Serra-Añó, P. Comparative Study of the Effectiveness of a Low-Pressure Hyperbaric Oxygen Treatment and Physical Exercise in Women with Fibromyalgia: Randomized Clinical Trial. Ther. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20930493. [Google Scholar] [CrossRef]
- Camporesi, E.M.; Mascia, M.F.; Thom, S.R. Physiological Principles of Hyperbaric Oxygenation. In Handbook on Hyperbaric Medicine; Springer: Milan, Italy, 1996; pp. 35–58. [Google Scholar]
- Bennett, M.H.; French, C.; Schnabel, A.; Wasiak, J.; Kranke, P.; Weibel, S. Normobaric and Hyperbaric Oxygen Therapy for the Treatment and Prevention of Migraine and Cluster Headache. Cochrane Database Syst. Rev. 2015, 2015, CD005219. [Google Scholar] [CrossRef]
- Lin, C.-H.; Su, W.-H.; Chen, Y.-C.; Feng, P.-H.; Shen, W.-C.; Ong, J.-R.; Wu, M.-Y.; Wong, C.S. Treatment with Normobaric or Hyperbaric Oxygen and Its Effect on Neuropsychometric Dysfunction after Carbon Monoxide Poisoning. Medicine 2018, 97, e12456. [Google Scholar] [CrossRef]
- Casillas, S.; Galindo, A.; Camarillo-Reyes, L.A.; Varon, J.; Surani, S.R. Effectiveness of Hyperbaric Oxygenation Versus Normobaric Oxygenation Therapy in Carbon Monoxide Poisoning: A Systematic Review. Cureus 2019, 11, e5916. [Google Scholar] [CrossRef]
- Leach, R.M.; Rees, P.J.; Wilmshurst, P. ABC of Oxygen: Hyperbaric Oxygen Therapy. Br. Med. J. 1998, 317, 1140–1143. [Google Scholar] [CrossRef]
- Brugniaux, J.V.; Coombs, G.B.; Barak, O.F.; Dujic, Z.; Sekhon, M.S.; Ainslie, P.N. Highs and Lows of Hyperoxia: Physiological, Performance, and Clinical Aspects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R1–R27. [Google Scholar] [CrossRef] [PubMed]
- Amir, H.; Shai, E. The Hyperoxic-hypoxic Paradox. Biomolecules 2020, 10, 958. [Google Scholar]
- Calabrese, E.J. Hormesis: Path and Progression to Significance. Int. J. Mol. Sci. 2018, 19, 2871. [Google Scholar] [CrossRef] [PubMed]
- Thom, S.R. Hyperbaric Oxygen: Its Mechanisms and Efficacy. Plast. Reconstr. Surg. 2011, 127, 131S–141S. [Google Scholar] [CrossRef]
- Camporesi, E.M.; Bosco, G. Mechanisms of Action of Hyperbaric Oxygen Therapy. Undersea Hyperb. Med. 2014, 41, 247–252. [Google Scholar]
- Longobardi, P.; Hoxha, K.; Perreca, F. Is Hyperbaric Oxygen an Effective Treatment for the Prevention of Complications in SARS-CoV-2 Asymptomatic Patients? Infect. Microbes Dis. 2021, 3, 109–111. [Google Scholar] [CrossRef]
- Chen, W.; Liang, X.; Nong, Z.; Li, Y.; Pan, X.; Chen, C.; Huang, L. The Multiple Applications and Possible Mechanisms of the Hyperbaric Oxygenation Therapy. Med. Chem. 2019, 15, 459–471. [Google Scholar] [CrossRef]
- DuBose, K.J.; Cooper, J.S. Hyperbaric Patient Selection; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Fife, C.E.; Eckert, K.A.; Carter, M.J. An Update on the Appropriate Role for Hyperbaric Oxygen: Indications and Evidence. Plast. Reconstr. Surg. 2016, 138, 107S–116S. [Google Scholar] [CrossRef]
- Bhutani, S.; Vishwanath, G. Hyperbaric Oxygen and Wound Healing. Indian J. Plast. Surg. 2012, 45, 316–324. [Google Scholar] [CrossRef]
- Longobardi, P.; Hoxha, K.; Bennett, M.H. Is There a Role for Hyperbaric Oxygen Therapy in the Treatment of Refractory Wounds of Rare Etiology? Diving Hyperb. Med. 2019, 49, 216–224. [Google Scholar] [CrossRef]
- Dhamodharan, U.; Karan, A.; Sireesh, D.; Vaishnavi, A.; Somasundar, A.; Rajesh, K.; Ramkumar, K.M. Tissue-Specific Role of Nrf2 in the Treatment of Diabetic Foot Ulcers during Hyperbaric Oxygen Therapy. Free Radic. Biol. Med. 2019, 138, 53–62. [Google Scholar] [CrossRef]
- Löndahl, M.; Katzman, P.; Nilsson, A.; Hammarlund, C. Hyperbaric Oxygen Therapy Facilitates Healing of Chronic Foot Ulcers in Patients with Diabetes. Diabetes Care 2010, 33, 998–1003. [Google Scholar] [CrossRef]
- Salama, S.E.; Eldeeb, A.E.; Elbarbary, A.H.; Abdelghany, S.E. Adjuvant Hyperbaric Oxygen Therapy Enhances Healing of Nonischemic Diabetic Foot Ulcers Compared With Standard Wound Care Alone. Int. J. Low. Extrem. Wounds 2019, 18, 75–80. [Google Scholar] [CrossRef]
- Sharma, R.; Sharma, S.K.; Mudgal, S.K.; Jelly, P.; Thakur, K. Efficacy of Hyperbaric Oxygen Therapy for Diabetic Foot Ulcer, a Systematic Review and Meta-Analysis of Controlled Clinical Trials. Sci. Rep. 2021, 11, 2189. [Google Scholar] [CrossRef]
- Game, F.L.; Apelqvist, J.; Attinger, C.; Hartemann, A.; Hinchliffe, R.J.; Löndahl, M.; Price, P.E.; Jeffcoate, W.J. Effectiveness of Interventions to Enhance Healing of Chronic Ulcers of the Foot in Diabetes: A Systematic Review. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. 1), 154–168. [Google Scholar] [CrossRef]
- Lalieu, R.C.; Brouwer, R.J.; Ubbink, D.T.; Hoencamp, R.; Raap, R.B.; Van Hulst, R.A. Hyperbaric Oxygen Therapy for Nonischemic Diabetic Ulcers: A Systematic Review. Wound Repair Regen. Off. Publ. Wound Health Soc. Eur. Tissue Repair Soc. 2020, 28, 266–275. [Google Scholar] [CrossRef]
- Brouwer, R.J.; Lalieu, R.; Hoencamp, R.; van Hulst, R.A.; Ubbink, D.T. A Systematic Review and Meta-Analysis of Hyperbaric Oxygen Therapy for Diabetic Foot Ulcers with Arterial Insufficiency. J. Vasc. Surg. 2020, 71, 682–692. [Google Scholar] [CrossRef]
- Londahl, M.; Fagher, K.; Nilson, A.; Katzman, P. Hyperbaric Oxygen Therapy Is Associated with Improved Six-Year Survival in People with Chronic Diabetic Foot Ulcers. Diabetes 2018, 67, 2225. [Google Scholar] [CrossRef]
- Edwards, M.L. Hyperbaric Oxygen Therapy. Part 2: Application in Disease. J. Vet. Emergy Crit. Care 2010, 20, 289–297. [Google Scholar] [CrossRef]
- Marx, R.E.; Ehler, W.J.; Tayapongsak, P.; Pierce, L.W. Relationship of Oxygen Dose to Angiogenesis Induction in Irradiated Tissue. Am. J. Surg. 1990, 160, 519–524. [Google Scholar] [CrossRef]
- Sander, A.L.; Henrich, D.; Muth, C.M.; Marzi, I.; Barker, J.H.; Frank, J.M. In Vivo Effect of Hyperbaric Oxygen on Wound Angiogenesis and Epithelialization. Wound Repair Regen. 2009, 17, 179–184. [Google Scholar] [CrossRef]
- Peña-Villalobos, I.; Casanova-Maldonado, I.; Lois, P.; Prieto, C.; Pizarro, C.; Lattus, J.; Osorio, G.; Palma, V. Hyperbaric Oxygen Increases Stem Cell Proliferation, Angiogenesis and Wound-Healing Ability of WJ-MSCs in Diabetic Mice. Front. Physiol. 2018, 9, 995. [Google Scholar] [CrossRef]
- Sureda, A.; Batle, J.M.; Martorell, M.; Capó, X.; Tejada, S.; Tur, J.A.; Pons, A. Antioxidant Response of Chronic Wounds to Hyperbaric Oxygen Therapy. PLoS ONE 2016, 11, e0163371. [Google Scholar] [CrossRef]
- Boykin, J.V.; Baylis, C. Hyperbaric Oxygen Therapy Mediates Increased Nitric Oxide Production Associated with Wound Healing. Adv. Ski. Wound Care 2007, 20, 382–389. [Google Scholar] [CrossRef]
- Dulai, P.S.; Buckey, J.C.; Raffals, L.E.; Swoger, J.M.; Claus, P.L.; O’Toole, K.; Ptak, J.A.; Gleeson, M.W.; Widjaja, C.E.; Chang, J.; et al. Hyperbaric Oxygen Therapy Is Well Tolerated and Effective for Ulcerative Colitis Patients Hospitalized for Moderate-Severe Flares: A Phase 2A Pilot Multi-Center, Randomized, Double-Blind, Sham-Controlled Trial. Am. J. Gastroenterol. 2018, 113, 1516–1523. [Google Scholar] [CrossRef]
- Wang, W.; He, Y.; Wen, D.; Jiang, S.; Zhao, X. Efficacy and Safety Evaluation of Hyperbaric Oxygen Therapy for Patients with Ulcerative Colitis: A Protocol of Systematic Review and Meta-Analysis. Medicine 2021, 100, e23966. [Google Scholar] [CrossRef]
- Oliai, C.; Fisher, B.; Jani, A.; Wong, M.; Poli, J.; Brady, L.W.; Komarnicky, L.T. Hyperbaric Oxygen Therapy for Radiation-Induced Cystitis and Proctitis. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 733–740. [Google Scholar] [CrossRef]
- Davis, D.D.; Hanley, M.E.; Cooper, J.S. Osteoradionecrosis. Curr. Otorhinolaryngol. Rep. 2021, 6, 285–291. [Google Scholar]
- Malone, M.; Bjarnsholt, T.; McBain, A.J.; James, G.A.; Stoodley, P.; Leaper, D.; Tachi, M.; Schultz, G.; Swanson, T.; Wolcott, R.D. The Prevalence of Biofilms in Chronic Wounds: A Systematic Review and Meta-Analysis of Published Data. J. Wound Care 2017, 26, 20–25. [Google Scholar] [CrossRef]
- Kadam, S.; Shai, S.; Shahane, A.; Kaushik, K.S. Recent Advances in Non-Conventional Antimicrobial Approaches for Chronic Wound Biofilms: Have We Found the “Chink in the Armor”? Biomedicines 2019, 7, 35. [Google Scholar] [CrossRef]
- Kościuczuk, E.M.; Lisowski, P.; Jarczak, J.; Strzałkowska, N.; Jóźwik, A.; Horbańczuk, J.; Krzyżewski, J.; Zwierzchowski, L.; Bagnicka, E. Cathelicidins: Family of Antimicrobial Peptides. A Review. Mol. Biol. Rep. 2012, 39, 10957–10970. [Google Scholar] [CrossRef] [PubMed]
- Peyssonnaux, C.; Datta, V.; Cramer, T.; Doedens, A.; Theodorakis, E.A.; Gallo, R.L.; Hurtado-Ziola, N.; Nizet, V.; Johnson, R.S. HIF-1α Expression Regulates the Bactericidal Capacity of Phagocytes. J. Clin. Investig. 2005, 115, 1806–1815. [Google Scholar] [CrossRef] [PubMed]
- Zarember, K.A.; Malech, H.L. HIF-1alpha: A Master Regulator of Innate Host Defenses? J. Clin. Investig. 2005, 115, 1702–1704. [Google Scholar] [CrossRef] [PubMed]
- Tecle, T.; Tripathi, S.; Hartshorn, K. Review: Defensins and Cathelicidins in Lung Immunity. Innate Immun. 2010, 16, 151–159. [Google Scholar] [CrossRef]
- Gaudreault, É.; Gosselin, J. Leukotriene B4 Induces Release of Antimicrobial Peptides in Lungs of Virally Infected Mice. J. Immunol. 2008, 180, 6211–6221. [Google Scholar] [CrossRef]
- Memar, M.Y.; Yekani, M.; Alizadeh, N.; Baghi, H.B. Hyperbaric Oxygen Therapy: Antimicrobial Mechanisms and Clinical Application for Infections. Biomed. Pharmacother. 2019, 109, 440–447. [Google Scholar] [CrossRef]
- Shaw, J.J.; Psoinos, C.M.; Emhoff, T.A.; Shah, S.A.; Santry, H. Not Just Full of Hot Air: Hyperbaric Oxygen Therapy Increases Survival in Cases of Necrotizing Soft Tissue Infections. Surg. Infect. 2014, 15, 328–335. [Google Scholar] [CrossRef]
- Nedrebø, T.; Bruun, T.; Skjåstad, R.; Holmaas, G.; Skrede, S. Hyperbaric Oxygen Treatment in Three Cases of Necrotizing Infection of the Neck. Infect. Dis. Rep. 2012, 4, 73–76. [Google Scholar] [CrossRef]
- Sanford, N.E.; Wilkinson, J.E.; Nguyen, H.; Diaz, G.; Wolcott, R. Efficacy of Hyperbaric Oxygen Therapy in Bacterial Biofilm Eradication. J. Wound Care 2018, 27, S20–S28. [Google Scholar] [CrossRef]
- Gibson, A.; Davis, F.M. Hyperbaric Oxygen Therapy in the Management of Clostridium Perfringens Infections. N. Z. Med. J. 1986, 99, 617–620. [Google Scholar]
- Sison-Martinez, J.; Hendriksen, S.; Cooper, J.S. Hyperbaric Treatment Of Clostridial Myositis And Myonecrosis. 2021. Available online: https://europepmc.org/article/nbk/nbk500002 (accessed on 13 May 2021).
- Halbach, J.L.; Prieto, J.M.; Wang, A.W.; Hawisher, D.; Cauvi, D.M.; Reyes, T.; Okerblom, J.; Ramirez-Sanchez, I.; Villarreal, F.; Patel, H.H.; et al. Early Hyperbaric Oxygen Therapy Improves Survival in a Model of Severe Sepsis. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2019, 317, R160–R168. [Google Scholar] [CrossRef]
- Hung, M.C.; Chou, C.L.; Cheng, L.C.; Ho, C.H.; Niu, K.C.; Chen, H.L.; Tian, Y.F.; Liu, C.L. The Role of Hyperbaric Oxygen Therapy in Treating Extensive Fournier’s Gangrene. Urol. Sci. 2016, 27, 148–153. [Google Scholar] [CrossRef]
- Walter, G.; Vernier, M.; Pinelli, P.O.; Million, M.; Coulange, M.; Seng, P.; Stein, A. Bone and Joint Infections Due to Anaerobic Bacteria: An Analysis of 61 Cases and Review of the Literature. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1355–1364. [Google Scholar] [CrossRef]
- Muzumdar, D.; Jhawar, S.; Goel, A. Brain Abscess: An Overview. Int. J. Surg. 2011, 9, 136–144. [Google Scholar] [CrossRef]
- Tomoye, E.O.; Moon, R.E. Hyperbaric Oxygen for Intracranial Abscess. Undersea Hyperb. Med. 2021, 48, 97–102. [Google Scholar] [CrossRef]
- Bartek, J.; Jakola, A.S.; Skyrman, S.; Förander, P.; Alpkvist, P.; Schechtmann, G.; Glimåker, M.; Larsson, A.; Lind, F.; Mathiesen, T. Hyperbaric Oxygen Therapy in Spontaneous Brain Abscess Patients: A Population-Based Comparative Cohort Study. Acta Neurochir. 2016, 158, 1259–1267. [Google Scholar] [CrossRef]
- M Das, J.; Tommeraasen, M.A.; Cooper, J.S. Hyperbaric Evaluation and Treatment of Intracranial Abscess; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Hanley, M.E.; Hendriksen, S.; Cooper, J.S. Hyperbaric Treatment of Chronic Refractory Osteomyelitis; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Rose, D. Hyperbaric Oxygen Therapy for Chronic Refractory Osteomyelitis. Am. Fam. Physician 2012, 86, 888–893. [Google Scholar]
- Savvidou, O.D.; Kaspiris, A.; Bolia, I.K.; Chloros, G.D.; Goumenos, S.D.; Papagelopoulos, P.J.; Tsiodras, S. Effectiveness of Hyperbaric Oxygen Therapy for the Management of Chronic Osteomyelitis: A Systematic Review of the Literature. Orthopedics 2018, 41, 193–199. [Google Scholar] [CrossRef]
- Byun, Y.J.; Patel, J.; Nguyen, S.A.; Lambert, P.R. Hyperbaric Oxygen Therapy in Malignant Otitis Externa: A Systematic Review of the Literature. World J. Otorhinolaryngol. Head Neck Surg. 2020. [Google Scholar] [CrossRef]
- Kirby, J.P. Hyperbaric Oxygen Therapy Emergencies. Mol. Med. 2019, 116, 180–183. [Google Scholar]
- Leung, J.K.S.; Lam, R.P.K. Hyperbaric Oxygen Therapy: Its Use in Medical Emergencies and Its Development in Hong Kong. Hong Kong Med. J. 2018, 24, 191–199. [Google Scholar] [CrossRef]
- Cooper, J.S.; Hanson, K.C. Decompression Sickness (DCS, Bends, Caisson Disease); StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Pollock, N.W.; Buteau, D. Updates in Decompression Illness. Emerg. Med. Clin. N. Am. 2017, 35, 301–319. [Google Scholar] [CrossRef]
- Vann, R.D.; Butler, F.K.; Mitchell, S.J.; Moon, R.E. Decompression Illness. Lancet 2011, 377, 153–164. [Google Scholar] [CrossRef]
- Moon, R.E. Hyperbaric Oxygen Treatment for Decompression Sickness. Undersea Hyperb. Med. 2014, 41, 151–157. [Google Scholar]
- Moon, R.E. Adjunctive Therapy for Decompression Illness: A Review and Update. Diving Hyperb. Med. 2009, 39, 81–87. [Google Scholar]
- Malik, N.; Claus, P.L.; Illman, J.E.; Kligerman, S.J.; Moynagh, M.R.; Levin, D.L.; Woodrum, D.A.; Arani, A.; Arunachalam, S.P.; Araoz, P.A. Air Embolism: Diagnosis and Management. Future Cardiol. 2017, 13, 365–378. [Google Scholar] [CrossRef]
- Yesilaras, M.; Atılla, O.D.; Aksay, E.; Kilic, T.Y.; Atilla, O.D. Retrograde Cerebral Air Embolism. Am. J. Emerg. Med. 2014, 32, 1562.e1–1562.e2. [Google Scholar] [CrossRef]
- Moon, R.E. Hyperbaric Treatment of Air or Gas Embolism: Current Recommendations. Undersea Hyperb. Med. 2019, 46, 673–683. [Google Scholar] [CrossRef]
- Blanc, P.; Boussuges, A.; Henriette, K.; Sainty, J.; Deleflie, M. Iatrogenic Cerebral Air Embolism: Importance of an Early Hyperbaric Oxygenation. Intensive Care Med. 2002, 28, 559–563. [Google Scholar] [CrossRef]
- Bitterman, H.; Melamed, Y. Delayed Hyperbaric Treatment of Cerebral Air Embolism. Isr. J. Med. Sci. 1993, 29, 22–26. [Google Scholar]
- Schlimp, C.J.; Bothma, P.A.; Brodbeck, A.E. Cerebral Venous Air Embolism: What Is It and Do We Know How to Deal With It Properly? JAMA Neurol. 2014, 71, 243. [Google Scholar] [CrossRef] [PubMed]
- Bothma, P.A.; Schlimp, C.J., II. Retrograde Cerebral Venous Gas Embolism: Are We Missing Too Many Cases? Br. J. Anaesth. 2014, 112, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Hayreh, S.S. Central Retinal Artery Occlusion. Indian J. Ophthalmol. 2018, 66, 1684–1694. [Google Scholar] [CrossRef] [PubMed]
- Hanley, M.E.; Cooper, J.S. Hyperbaric, Central Retinal Artery Occlusion; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Bağlı, B.S.; Çevik, S.G.; Çevik, M.T. Effect of Hyperbaric Oxygen Treatment in Central Retinal Artery Occlusion. Undersea Hyperb. Med. 2018, 45, 421–425. [Google Scholar] [CrossRef]
- Olson, E.A.; Lentz, K. Central Retinal Artery Occlusion: A Literature Review and the Rationale for Hyperbaric Oxygen Therapy. Mol. Med. 2016, 113, 53–57. [Google Scholar]
- Kim, S.H.; Cha, Y.S.; Lee, Y.; Kim, H.; Yoon, I.N. Successful Treatment of Central Retinal Artery Occlusion Using Hyperbaric Oxygen Therapy. Clin. Exp. Emerg. Med. 2018, 5, 278–281. [Google Scholar] [CrossRef]
- Youn, T.S.; Lavin, P.; Patrylo, M.; Schindler, J.; Kirshner, H.; Greer, D.M.; Schrag, M. Current Treatment of Central Retinal Artery Occlusion: A National Survey. J. Neurol. 2018, 265, 330–335. [Google Scholar] [CrossRef]
- Yu, M.; Yuan, H.S.; Li, Q.; Li, Q.; Teng, Y.F. Combination of Cells-Based Therapy with Apelin-13 and Hyperbaric Oxygen Efficiently Promote Neovascularization in Ischemic Animal Model. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 2630–2639. [Google Scholar] [CrossRef]
- Santema, K.T.B.; Stoekenbroek, R.M.; Koelemay, M.J.W.; Reekers, J.A.; Van Dortmont, L.M.C.; Oomen, A.; Smeets, L.; Wever, J.J.; Legemate, D.A.; Ubbink, D.T. Hyperbaric Oxygen Therapy in the Treatment of Ischemic Lower-Extremity Ulcers in Patients with Diabetes: Results of the DAMO2CLES Multicenter Randomized Clinical Trial. Diabetes Care 2018, 41, 112–119. [Google Scholar] [CrossRef]
- Abidia, A.; Laden, G.; Kuhan, G.; Johnson, B.F.; Wilkinson, A.R.; Renwick, P.M.; Masson, E.A.; McCollum, P.T. The Role of Hyperbaric Oxygen Therapy in Ischaemic Diabetic Lower Extremity Ulcers: A Double-Blind Randomized-Controlled Trial. Eur. J. Vasc. Endovasc. Surg. 2003, 25, 513–518. [Google Scholar] [CrossRef]
- Nakamura, H.; Makiguchi, T.; Atomura, D.; Yamatsu, Y.; Shirabe, K.; Yokoo, S. Changes in Skin Perfusion Pressure After Hyperbaric Oxygen Therapy Following Revascularization in Patients With Critical Limb Ischemia: A Preliminary Study. Int. J. Low. Extrem. Wounds 2020, 19, 57–62. [Google Scholar] [CrossRef]
- Rose, J.J.; Wang, L.; Xu, Q.; McTiernan, C.F.; Shiva, S.; Tejero, J.; Gladwin, M.T. Carbon Monoxide Poisoning: Pathogenesis, Management, and Future Directions of Therapy. Am. J. Respir. Crit. Care Med. 2017, 195, 596–606. [Google Scholar] [CrossRef]
- Martani, L.; Cantadori, L.; Paganini, M.; Camporesi, E.M.; Bosco, G. Carbon Monoxide Intoxication: Prehospital Diagnosis and Direct Transfer to the Hyperbaric Chamber. Minerva Anestesiol. 2019, 85, 920–922. [Google Scholar] [CrossRef]
- Rose, J.J.; Nouraie, M.; Gauthier, M.C.; Pizon, A.F.; Saul, M.I.; Donahoe, M.P.; Gladwin, M.T. Clinical Outcomes and Mortality Impact of Hyperbaric Oxygen Therapy in Patients With Carbon Monoxide Poisoning. Crit. Care Med. 2018, 46, e649–e655. [Google Scholar] [CrossRef]
- Weaver, L.K.; Hopkins, R.O.; Chan, K.J.; Churchill, S.; Elliott, C.G.; Clemmer, T.P.; Orme, J.F.; Thomas, F.O.; Morris, A.H. Hyperbaric Oxygen for Acute Carbon Monoxide Poisoning. N. Engl. J. Med. 2002, 347, 1057–1067. [Google Scholar] [CrossRef]
- Hampson, N.B.; Piantadosi, C.A.; Thom, S.R.; Weaver, L.K. Practice Recommendations in the Diagnosis, Management, and Prevention of Carbon Monoxide Poisoning. Am. J. Respir. Crit. Care Med. 2012, 186, 1095–1101. [Google Scholar] [CrossRef]
- Hanley, M.E.; Murphy-Lavoie, H.M. Hyperbaric, Cyanide Toxicity; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Lawson-Smith, P.; Jansen, E.C.; Hilsted, L.; Johnsen, A.H.; Hyldegaard, O. Effect of Acute and Delayed Hyperbaric Oxygen Therapy on Cyanide Whole Blood Levels during Acute Cyanide Intoxication. Undersea Hyperb. Med. 2011, 38, 17–26. [Google Scholar]
- Van Meter, K.W. The Effect of Hyperbaric Oxygen on Severe Anemia. Undersea Hyperb. Med. 2012, 39, 937–942. [Google Scholar]
- Rhee, T.M.; Hwang, D.; Lee, J.S.; Park, J.; Lee, J.M. Addition of Hyperbaric Oxygen Therapy vs. Medical Therapy Alone for Idiopathic Sudden Sensorineural Hearing Loss: A Systematic Review and Meta-Analysis. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 1153–1161. [Google Scholar] [CrossRef]
- Bayoumy, A.B.; de Ru, J.A. The Use of Hyperbaric Oxygen Therapy in Acute Hearing Loss: A Narrative Review. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 1859–1880. [Google Scholar] [CrossRef]
- Paderno, E.; Zanon, V.; Vezzani, G.; Giacon, T.; Bernasek, T.; Camporesi, E.; Bosco, G. Evidence-Supported HBO Therapy in Femoral Head Necrosis: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2888. [Google Scholar] [CrossRef]
- Brenner, I.; Shephard, R.J.; Shek, P.N. Immune Function in Hyperbaric Environments, Diving, and Decompression. Undersea Hyperb. Med. 1999, 26, 27–39. [Google Scholar]
- Xu, X.; Yi, H.; Kato, M.; Suzuki, H.; Kobayashi, S.; Takahashi, H.; Nakashima, I. Differential Sensitivities to Hyperbaric Oxygen of Lymphocyte Subpopulations of Normal and Autoimmune Mice. Immunol. Lett. 1997, 59, 79–84. [Google Scholar] [CrossRef]
- Saito, K.; Tanaka, Y.; Ota, T.; Eto, S.; Yamashita, U. Suppressive Effect of Hyperbaric Oxygenation on Immune Responses of Normal and Autoimmune Mice. Clin. Exp. Immunol. 1991, 86, 322–327. [Google Scholar] [CrossRef]
- Chen, S.Y.; Chen, Y.C.; Wang, J.K.; Hsu, H.P.; Ho, P.S.; Chen, Y.C.; Sytwu, H.K. Early Hyperbaric Oxygen Therapy Attenuates Disease Severity in Lupus-Prone Autoimmune (NZB × NZW) F1 Mice. Clin. Immunol. 2003, 108, 103–110. [Google Scholar] [CrossRef]
- Harnanik, T.; Soeroso, J.; Suryokusumo, M.G.; Juliandhy, T. Effects of Hyperbaric Oxygen on t Helper 17/Regulatory t Polarization in Antigen and Collagen-Induced Arthritis: Hypoxia-Inducible Factor-1α as a Target. Oman Med. J. 2020, 35, e90. [Google Scholar] [CrossRef] [PubMed]
- Novak, S.; Drenjancevic, I.; Vukovic, R.; Kellermayer, Z.; Cosic, A.; Tolusic Levak, M.; Balogh, P.; Culo, F.; Mihalj, M. Anti-Inflammatory Effects of Hyperbaric Oxygenation during DSS-Induced Colitis in BALB/c Mice Include Changes in Gene Expression of HIF-1 α, Proinflammatory Cytokines, and Antioxidative Enzymes. Mediat. Inflamm. 2016, 2016, 7141430. [Google Scholar] [CrossRef] [PubMed]
- Resanovic, I.; Gluvic, Z.; Zaric, B.; Sudar-Milovanovic, E.; Jovanovic, A.; Milacic, D.; Isakovic, R.; Isenovic, E.R. Early Effects of Hyperbaric Oxygen on Inducible Nitric Oxide Synthase Activity/Expression in Lymphocytes of Type 1 Diabetes Patients: A Prospective Pilot Study. Int. J. Endocrinol. 2019, 2019, 2328505. [Google Scholar] [CrossRef] [PubMed]
- Bellato, E.; Marini, E.; Castoldi, F.; Barbasetti, N.; Mattei, L.; Bonasia, D.E.; Blonna, D. Fibromyalgia Syndrome: Etiology, Pathogenesis, Diagnosis, and Treatment. Pain Res. Treat. 2012, 2012, 17. [Google Scholar] [CrossRef]
- Guggino, G.; Schinocca, C.; Lo Pizzo, M.; Di Liberto, D.; Garbo, D.; Raimondo, S.; Alessandro, R.; Brighina, F.; Ruscitti, P.; Giacomelli, R.; et al. T Helper 1 Response Is Correlated with Widespread Pain, Fatigue, Sleeping Disorders and the Quality of Life in Patients with Fibromyalgia and Is Modulated by Hyperbaric Oxygen Therapy. Clin. Exp. Rheumatol. 2019, 37 (Suppl. 116), 81–89. [Google Scholar]
- Woo, J.; Min, J.H.; Lee, Y.H.; Roh, H.T. Effects of Hyperbaric Oxygen Therapy on Inflammation, Oxidative/Antioxidant Balance, and Muscle Damage after Acute Exercise in Normobaric, Normoxic and Hypobaric, Hypoxic Environments: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 7377. [Google Scholar] [CrossRef]
- Ortega, M.A.; Fraile-Martínez, O.; García-Montero, C.; García-Gallego, S.; Sánchez-Trujillo, L.; Torres-Carranza, D.; Álvarez-Mon, M.Á.; Pekarek, L.; García-Honduvilla, N.; Bujan, J.; et al. An Integrative Look at SARS-CoV-2 (Review). Int. J. Mol. Med. 2021, 47, 415–434. [Google Scholar] [CrossRef]
- del Barco, A.A.; Ortega, M.A. Epidemiology and Public Health in the COVID-19 Epidemic. Medicine 2020, 13, 1297–1304. [Google Scholar] [CrossRef]
- Chandra, A.; Chakraborty, U.; Pal, J.; Karmakar, P. Silent Hypoxia: A Frequently Overlooked Clinical Entity in Patients with COVID-19. BMJ Case Rep. 2020, 13, 237207. [Google Scholar] [CrossRef]
- Dhont, S.; Derom, E.; Van Braeckel, E.; Depuydt, P.; Lambrecht, B.N. The Pathophysiology of “happy” Hypoxemia in COVID-19. Respir. Res. 2020, 21, 198. [Google Scholar] [CrossRef]
- Álvarez-Mon, M.; Ortega, M.A.; Gasulla, Ó.; Fortuny-Profitós, J.; Mazaira-Font, F.A.; Saurina, P.; Monserrat, J.; Plana, M.N.; Troncoso, D.; Moreno, J.S.; et al. A Predictive Model and Risk Factors for Case Fatality of Covid-19. J. Pers. Med. 2021, 11, 36. [Google Scholar] [CrossRef]
- Tobin, M.J.; Laghi, F.; Jubran, A. Why COVID-19 Silent Hypoxemia Is Baffling to Physicians. Am. J. Respir. Crit. Care Med. 2020, 202, 356–360. [Google Scholar] [CrossRef]
- Wilkerson, R.G.; Adler, J.D.; Shah, N.G.; Brown, R. Silent Hypoxia: A Harbinger of Clinical Deterioration in Patients with COVID-19. Am. J. Emerg. Med. 2020, 38, 2243.e5–2243.e6. [Google Scholar] [CrossRef]
- Brouqui, P.; Amrane, S.; Million, M.; Cortaredona, S.; Parola, P.; Lagier, J.C.; Raoult, D. Asymptomatic Hypoxia in COVID-19 Is Associated with Poor Outcome. Int. J. Infect. Dis. 2021, 102, 233–238. [Google Scholar] [CrossRef]
- Lindahl, S.G.E. Using the Prone Position Could Help to Combat the Development of Fast Hypoxia in Some Patients with COVID-19. Acta Paediatr. Int. J. Paediatr. 2020, 109, 1539–1544. [Google Scholar] [CrossRef]
- Oliaei, S.; SeyedAlinaghi, S.; Mehrtak, M.; Karimi, A.; Noori, T.; Mirzapour, P.; Shojaei, A.; Mohsseni Pour, M.; Mirghaderi, S.P.; Alilou, S.; et al. The effects of hyperbaric oxygen therapy (HBOT) on coronavirus disease-2019 (COVID-19): A systematic review. Eur. J. Med. Res. 2021, 26, 96. [Google Scholar] [CrossRef] [PubMed]
- Paganini, M.; Bosco, G.; Perozzo, F.A.G.; Kohlscheen, E.; Sonda, R.; Bassetto, F.; Garetto, G.; Camporesi, E.M.; Thom, S.R. The Role of Hyperbaric Oxygen Treatment for COVID-19: A Review. Adv. Exp. Med. Biol. 2021, 1289, 27–35. [Google Scholar] [CrossRef] [PubMed]
- De Maio, A.; Hightower, L.E. COVID-19, Acute Respiratory Distress Syndrome (ARDS), and Hyperbaric Oxygen Therapy (HBOT): What Is the Link? Cell Stress Chaperones 2020, 25, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Criado, P.R.; Miot, H.A.; Pincelli, T.P.H.; Fabro, A.T. From Dermatological Conditions to COVID-19: Reasoning for Anticoagulation, Suppression of Inflammation, and Hyperbaric Oxygen Therapy. Dermatol. Ther. 2021, 34, e14565. [Google Scholar] [CrossRef]
- Xiaoling, Z.; Xiaolan, T.; Yanchao, T.; Ruiyong, C. The Outcomes of Hyperbaric Oxygen Therapy to Retrieve Hypoxemia of Severe Novel Coronavirus Pneumonia: First Case Report. Chin. J. Naut. Med. Hyperb. Med. 2020, 27, E001. [Google Scholar] [CrossRef]
- Kjellberg, A.; De Maio, A.; Lindholm, P. Can Hyperbaric Oxygen Safely Serve as an Anti-Inflammatory Treatment for COVID-19? Med. Hypotheses 2020, 144, 110224. [Google Scholar] [CrossRef]
- Senniappan, K.; Jeyabalan, S.; Rangappa, P.; Kanchi, M. Hyperbaric Oxygen Therapy: Can It Be a Novel Supportive Therapy in COVID-19? Indian J. Anaesth. 2020, 64, 835–841. [Google Scholar]
- Thibodeaux, K.; Speyrer, M.; Raza, A.; Yaakov, R.; Serena, T.E. Hyperbaric Oxygen Therapy in Preventing Mechanical Ventilation in COVID-19 Patients: A Retrospective Case Series. J. Wound Care 2020, 29, S4–S8. [Google Scholar] [CrossRef]
- Guo, D.; Pan, S.; Wang, M.; Guo, Y. Hyperbaric Oxygen Therapy May Be Effective to Improve Hypoxemia in Patients with Severe COVID-2019 Pneumonia: Two Case Reports. Undersea Hyperb. Med. J. Undersea Hyperb. Med. Soc. Inc. 2020, 47, 181–187. [Google Scholar] [CrossRef]
- Tian, S.; Hu, W.; Niu, L.; Liu, H.; Xu, H.; Xiao, S.Y. Pulmonary Pathology of Early-Phase 2019 Novel Coronavirus (COVID-19) Pneumonia in Two Patients With Lung Cancer. J. Thorac. Oncol. 2020, 15, 700–704. [Google Scholar] [CrossRef]
- Cavezzi, A.; Troiani, E.; Corrao, S. COVID-19: Hemoglobin, Iron, and Hypoxia beyond Inflammation. A Narrative Review. Clin. Pract. 2020, 10, 24–30. [Google Scholar] [CrossRef]
- Allali, G.; Marti, C.; Grosgurin, O.; Morélot-Panzini, C.; Similowski, T.; Adler, D. Dyspnea: The vanished warning symptom of COVID-19 pneumonia. J. Med. Virol. 2020, 92, 2272–2273. [Google Scholar] [CrossRef]
- El Hawa, A.A.A.; Charipova, K.; Bekeny, J.C.; Johnson-Arbor, K.K. The Evolving Use of Hyperbaric Oxygen Therapy during the COVID-19 Pandemic. J. Wound Care 2021, 30, S8–S11. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Muz, B.; de la Puente, P.; Azab, F.; Azab, A.K. The Role of Hypoxia in Cancer Progression, Angiogenesis, Metastasis, and Resistance to Therapy. Hypoxia 2015, 3, 83. [Google Scholar] [CrossRef]
- Ortega, M.A.; Fraile-Martínez, O.; Asúnsolo, Á.; Buján, J.; García-Honduvilla, N.; Coca, S. Signal Transduction Pathways in Breast Cancer: The Important Role of PI3K/Akt/MTOR. J. Oncol. 2020, 2020, 9258396. [Google Scholar] [CrossRef]
- Jing, X.; Yang, F.; Shao, C.; Wei, K.; Xie, M.; Shen, H.; Shu, Y. Role of Hypoxia in Cancer Therapy by Regulating the Tumor Microenvironment. Mol. Cancer 2019, 18, 157. [Google Scholar] [CrossRef]
- Dhani, N.; Fyles, A.; Hedley, D.; Milosevic, M. The Clinical Significance of Hypoxia in Human Cancers. Semin. Nucl. Med. 2015, 45, 110–121. [Google Scholar] [CrossRef]
- Kim, S.W.; Kim, I.K.; Lee, S.H. Role of Hyperoxic Treatment in Cancer. Exp. Biol. Med. 2020, 245, 851–860. [Google Scholar] [CrossRef]
- Moen, I.; Stuhr, L.E.B. Hyperbaric Oxygen Therapy and Cancer—A Review. Target. Oncol. 2012, 7, 233–242. [Google Scholar] [CrossRef]
- Stępień, K.; Ostrowski, R.P.; Matyja, E. Hyperbaric Oxygen as an Adjunctive Therapy in Treatment of Malignancies, Including Brain Tumours. Med. Oncol. 2016, 33, 101. [Google Scholar] [CrossRef] [PubMed]
- Thews, O.; Vaupel, P. Spatial Oxygenation Profiles in Tumors during Normo- and Hyperbaric Hyperoxia. Strahlenther Onkol. 2015, 191, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Feldmeier, J.; Carl, U.; Hartmann, K.; Sminia, P. Hyperbaric Oxygen: Does It Promote Growth or Recurrence of Malignancy? Undersea Hyperb. Med. 2003, 30, 1–18. [Google Scholar] [PubMed]
- Pande, S.; Sengupta, A.; Srivastava, A.; Gude, R.P.; Ingle, A. Re-Evaluate the Effect of Hyperbaric Oxygen Therapy in Cancer—A Preclinical Therapeutic Small Animal Model Study. PLoS ONE 2012, 7, e48432. [Google Scholar] [CrossRef]
- Lu, Q.Z.; Li, X.; Ouyang, J.; Li, J.Q.; Chen, G. Further Application of Hyperbaric Oxygen in Prostate Cancer. Med. Gas Res. 2018, 8, 167–171. [Google Scholar]
- Batra, S.; Adekola, K.; Rosen, S.; Shanmugam, M. Cancer Metabolism as a Therapeutic Target. Oncology 2013, 27, 460–467. [Google Scholar]
- Poff, A.M.; Ari, C.; Seyfried, T.N.; D’Agostino, D.P. The Ketogenic Diet and Hyperbaric Oxygen Therapy Prolong Survival in Mice with Systemic Metastatic Cancer. PLoS ONE 2013, 8, e65522. [Google Scholar] [CrossRef]
- Poff, A.M.; Ward, N.; Seyfried, T.N.; Arnold, P.; D’Agostino, D.P. Non-Toxic Metabolic Management of Metastatic Cancer in VM Mice: Novel Combination of Ketogenic Diet, Ketone Supplementation, and Hyperbaric Oxygen Therapy. PLoS ONE 2015, 10, e0127407. [Google Scholar] [CrossRef]
- Baskar, R.; Lee, K.A.; Yeo, R.; Yeoh, K.W. Cancer and Radiation Therapy: Current Advances and Future Directions. Int. J. Med. Sci. 2012, 9, 193–199. [Google Scholar] [CrossRef]
- Arienti, C.; Pignatta, S.; Zanoni, M.; Zamagni, A.; Cortesi, M.; Sarnelli, A.; Romeo, A.; Arpa, D.; Longobardi, P.; Bartolini, D.; et al. High-Pressure Oxygen Rewires Glucose Metabolism of Patient-Derived Glioblastoma Cells and Fuels Inflammasome Response. Cancer Lett. 2021, 506, 152–166. [Google Scholar] [CrossRef]
- Arpa, D.; Parisi, E.; Ghigi, G.; Cortesi, A.; Longobardi, P.; Cenni, P.; Pieri, M.; Tontini, L.; Neri, E.; Micheletti, S.; et al. Role of Hyperbaric Oxygenation Plus Hypofractionated Stereotactic Radiotherapy in Recurrent High-Grade Glioma. Front. Oncol. 2021, 11, 964. [Google Scholar] [CrossRef]
- Majeed, H.; Gupta, V. Adverse Effects of Radiation Therapy; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Brush, J.; Lipnick, S.L.; Phillips, T.; Sitko, J.; McDonald, J.T.; McBride, W.H. Molecular Mechanisms of Late Normal Tissue Injury. Semin. Radiat. Oncol. 2007, 17, 121–130. [Google Scholar] [CrossRef]
- Cooper, J.S.; Hanley, M.E.; Hendriksen, S.; Robins, M. Hyperbaric Treatment of Delayed Radiation Injury; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Feldmeier, J.J. Hyperbaric Oxygen Therapy and Delayed Radiation Injuries (Soft Tissue and Bony Necrosis): 2012 Update. Undersea Hyperb. Med. 2012, 39, 1121–1139. [Google Scholar]
- Bennett, M.H.; Feldmeier, J.; Hampson, N.B.; Smee, R.; Milross, C. Hyperbaric Oxygen Therapy for Late Radiation Tissue Injury. Cochrane Database Syst. Rev. 2016, 2016, CD005005. [Google Scholar] [CrossRef]
- Brewer, A.L.; Shirachi, D.Y.; Quock, R.M.; Craft, R.M. Effect of Hyperbaric Oxygen on Chemotherapy-Induced Neuropathy in Male and Female Rats. Behav. Pharmacol. 2020, 31, 61–72. [Google Scholar] [CrossRef]
- Fu, H.; Li, F.; Thomas, S.; Yang, Z. Hyperbaric Oxygenation Alleviates Chronic Constriction Injury (CCI)-Induced Neuropathic Pain and Inhibits GABAergic Neuron Apoptosis in the Spinal Cord. Scand. J. Pain 2017, 17, 330–338. [Google Scholar] [CrossRef]
- Zhang, Y.; Brewer, A.L.; Nelson, J.T.; Smith, P.T.; Shirachi, D.Y.; Quock, R.M. Hyperbaric Oxygen Produces a Nitric Oxide Synthase-Regulated Anti-Allodynic Effect in Rats with Paclitaxel-Induced Neuropathic Pain. Brain Res. 2019, 1711, 41–47. [Google Scholar] [CrossRef]
- Gibbons, C.R.; Liu, S.; Zhang, Y.; Sayre, C.L.; Levitch, B.R.; Moehlmann, S.B.; Shirachi, D.Y.; Quock, R.M. Involvement of Brain Opioid Receptors in the Anti-Allodynic Effect of Hyperbaric Oxygen in Rats with Sciatic Nerve Crush-Induced Neuropathic Pain. Brain Res. 2013, 1537, 111–116. [Google Scholar] [CrossRef]
- Kawasoe, Y.; Yokouchi, M.; Ueno, Y.; Iwaya, H.; Yoshida, H.; Komiya, S. Hyperbaric Oxygen as a Chemotherapy Adjuvant in the Treatment of Osteosarcoma. Oncol. Rep. 2009, 22, 1045–1050. [Google Scholar] [CrossRef][Green Version]
- Petre, P.M.; Baciewicz, F.A.; Tigan, S.; Spears, J.R.; Patterson, G.A.; Swisher, S.G.; Harpole, D.H.; Goldstraw, P. Hyperbaric Oxygen as a Chemotherapy Adjuvant in the Treatment of Metastatic Lung Tumors in a Rat Model. J. Thorac. Cardiovasc. Surg. 2003, 125, 85–95. [Google Scholar] [CrossRef][Green Version]
- Ohguri, T.; Imada, H.; Narisada, H.; Yahara, K.; Morioka, T.; Nakano, K.; Miyaguni, Y.; Korogi, Y. Systemic Chemotherapy Using Paclitaxel and Carboplatin plus Regional Hyperthermia and Hyperbaric Oxygen Treatment for Non-Small Cell Lung Cancer with Multiple Pulmonary Metastases: Preliminary Results. Int. J. Hyperth. 2009, 25, 160–167. [Google Scholar] [CrossRef]
- Baude, J.; Cooper, J.S. Hyperbaric Contraindicated Chemotherapeutic Agents; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Ortega, M.A.; Fraile-Martínez, O.; García-Montero, C.; Pekarek, L.; Guijarro, L.G.; Castellanos, A.J.; Sanchez-Trujillo, L.; García-Honduvilla, N.; Álvarez-Mon, M.; Buján, J.; et al. Physical Activity as an Imperative Support in Breast Cancer Management. Cancers 2021, 13, 55. [Google Scholar] [CrossRef]
- Hadanny, A.; Lang, E.; Copel, L.; Meir, O.; Bechor, Y.; Fishlev, G.; Bergan, J.; Friedman, M.; Zisman, A.; Efrati, S. Hyperbaric Oxygen Can Induce Angiogenesis and Recover Erectile Function. Int. J. Impot. Res. 2018, 30, 292–299. [Google Scholar] [CrossRef]
- Chiles, K.A.; Staff, I.; Johnson-Arbor, K.; Champagne, A.; McLaughlin, T.; Graydon, R.J. A Double-Blind, Randomized Trial on the Efficacy and Safety of Hyperbaric Oxygenation Therapy in the Preservation of Erectile Function after Radical Prostatectomy. J. Urol. 2018, 199, 805–811. [Google Scholar] [CrossRef]
- Cormier, J.; Theriot, M. Patient Diagnosed with Chronic Erectile Dysfunction Refractory to PDE 5 Inhibitor Therapy Reports Improvement in Function after Hyperbaric Oxygen Therapy. Undersea Hyperb. Med. 2016, 43, 463–465. [Google Scholar]
- Yuan, J.-B.; Yang, L.Y.; Wang, Y.H.; Ding, T.; Chen, T.D.; Lu, Q. Hyperbaric Oxygen Therapy for Recovery of Erectile Function after Posterior Urethral Reconstruction. Int. Urol. Nephrol. 2011, 43, 755–761. [Google Scholar] [CrossRef]
- Lippert, T.; Borlongan, C.V. Prophylactic Treatment of Hyperbaric Oxygen Treatment Mitigates Inflammatory Response via Mitochondria Transfer. CNS Neurosci. Ther. 2019, 25, 815–823. [Google Scholar] [CrossRef]
- Liska, G.M.; Lippert, T.; Russo, E.; Nieves, N.; Borlongan, C. V A Dual Role for Hyperbaric Oxygen in Stroke Neuroprotection: Preconditioning of the Brain and Stem Cells. Cond. Med. 2018, 1, 151–166. [Google Scholar]
- Ding, Z.; Tong, W.C.; Lu, X.-X.; Peng, H.-P. Hyperbaric Oxygen Therapy in Acute Ischemic Stroke: A Review. Interv. Neurol. 2014, 2, 201–211. [Google Scholar] [CrossRef]
- Hachmo, Y.; Hadanny, A.; Abu Hamed, R.; Daniel-Kotovsky, M.; Catalogna, M.; Fishlev, G.; Lang, E.; Polak, N.; Doenyas, K.; Friedman, M.; et al. Hyperbaric Oxygen Therapy Increases Telomere Length and Decreases Immunosenescence in Isolated Blood Cells: A Prospective Trial. Aging 2020, 12, 22445–22456. [Google Scholar] [CrossRef]
- Nishizaka, T.; Nomura, T.; Higuchi, K.; Takemura, A.; Ishihara, A. Mild Hyperbaric Oxygen Activates the Proliferation of Epidermal Basal Cells in Aged Mice. J. Dermatol. 2018, 45, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Godman, C.A.; Joshi, R.; Giardina, C.; Perdrizet, G.; Hightower, L.E. Hyperbaric Oxygen Treatment Induces Antioxidant Gene Expression. Ann. N. Y. Acad. Sci. 2010, 1197, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Amir, H.; Malka, D.K.; Gil, S.; Rahav, B.G.; Merav, C.; Kobi, D.; Yafit, H.; Ramzia, A.H.; Efrat, S.; Gregory, F.; et al. Cognitive Enhancement of Healthy Older Adults Using Hyperbaric Oxygen: A Randomized Controlled Trial. Aging 2020, 12, 13740–13761. [Google Scholar] [CrossRef] [PubMed]
- Shwe, T.; Bo-Htay, C.; Ongnok, B.; Chunchai, T.; Jaiwongkam, T.; Kerdphoo, S.; Kumfu, S.; Pratchayasakul, W.; Pattarasakulchai, T.; Chattipakorn, N.; et al. Hyperbaric Oxygen Therapy Restores Cognitive Function and Hippocampal Pathologies in Both Aging and Aging-Obese Rats. Mech. Ageing Dev. 2021, 195, 111465. [Google Scholar] [CrossRef]
- Camporesi, E.M. Side Effects of Hyperbaric Oxygen Therapy. Undersea Hyperb. Med. 2014, 41, 253–257. [Google Scholar]
- Heyboer, M.; Sharma, D.; Santiago, W.; McCulloch, N. Hyperbaric Oxygen Therapy: Side Effects Defined and Quantified. Adv. Wound Care 2017, 6, 210–224. [Google Scholar] [CrossRef]
- Hadanny, A.; Meir, O.; Bechor, G.; Fishlev, J.; Efrati, S. Seizures during Hyperbaric Oxygen Therapy: Retrospective Analysis of 62,614 Treatment Sessions. Undersea Hyperb. Med. 2016, 43, 21–28. [Google Scholar]
- Cooper, J.S.; Phuyal, P.; Shah, N. Oxygen Toxicity; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK430743/ (accessed on 28 March 2021).
- Domachevsky, L.; Rachmany, L.; Barak, Y.; Rubovitch, V.; Abramovich, A.; Pick, C.G. Hyperbaric Oxygen-Induced Seizures Cause a Transient Decrement in Cognitive Function. Neuroscience 2013, 247, 328–334. [Google Scholar] [CrossRef]
- Nakane, M. Biological Effects of the Oxygen Molecule in Critically Ill Patients. J. Intensive Care 2020, 8, 95. [Google Scholar] [CrossRef]
- Hadanny, A.; Zubari, T.; Tamir-Adler, L.; Bechor, Y.; Fishlev, G.; Lang, E.; Polak, N.; Bergan, J.; Friedman, M.; Efrati, S. Hyperbaric Oxygen Therapy Effects on Pulmonary Functions: A Prospective Cohort Study. BMC Pulm. Med. 2019, 19, 148. [Google Scholar] [CrossRef]
- Mcmonnies, C.W. Hyperbaric Oxygen Therapy and the Possibility of Ocular Complications or Contraindications. Clin. Exp. Optom. 2015, 98, 122–125. [Google Scholar] [CrossRef]
- Sola, A.; Chow, L.; Rogido, M. Retinopathy of Prematurity and Oxygen Therapy: A Changing Relationship. An. Pediatr. 2005, 62, 48–63. [Google Scholar] [CrossRef]
- Gawdi, R.; Cooper, J.S. Hyperbaric Contraindications; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Arslan, A. Hyperbaric Oxygen Therapy in Carbon Monoxide Poisoning in Pregnancy: Maternal and Fetal Outcome. Am. J. Emerg. Med. 2021, 43, 41–45. [Google Scholar] [CrossRef]
- Stevens, S.L.; Narr, A.J.; Claus, P.L.; Millman, M.P.; Steinkraus, L.W.; Shields, R.C.; Buchta, W.G.; Haddon, R.; Wang, Z.; Murad, M.H. The Incidence of Hypoglycemia during HBO2 Therapy: A Retrospective Review. Undersea Hyperb. Med. 2015, 42, 191–196. [Google Scholar]
- Al-Waili, N.S.; Butler, G.J.; Beale, J.; Abdullah, M.S.; Finkelstein, M.; Merrow, M.; Rivera, R.; Petrillo, R.; Carrey, Z.; Lee, B.; et al. Influences of Hyperbaric Oxygen on Blood Pressure, Heart Rate and Blood Glucose Levels in Patients with Diabetes Mellitus and Hypertension. Arch. Med. Res. 2006, 37, 991–997. [Google Scholar] [CrossRef]
- Weaver, L.K.; Churchill, S. Pulmonary Edema Associated with Hyperbaric Oxygen Therapy. Chest 2001, 120, 1407–1409. [Google Scholar] [CrossRef]
- Kahle, A.C.; Cooper, J.S. Hyperbaric Physiological And Pharmacological Effects Gases; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Wang, X.; Li, S.; Liu, X.; Wu, X.; Ye, N.; Yang, X.; Li, Z. Boosting Nanomedicine Efficacy with Hyperbaric Oxygen Therapy. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2021; Volume 1295, pp. 77–95. [Google Scholar]
| Air or gas embolism |
| Acute thermal burn injury |
| Carbon monoxide poisoning |
| Carbon monoxide poisoning complicated by cyanide poisoning |
| Central retinal artery occlusion |
| Clostridial myositis and myonecrosis (gas gangrene) |
| Compromised grafts and Flaps |
| Crush injury, Compartment Syndrome and other acute traumatic ischemia |
| Decompression sickness |
| Delayed radiation injury (soft tissue and bony necrosis) |
| Enhancement of healing in selected problem wounds |
| Idiopathic sudden sensorineural hearing loss |
| Intracranial abscess |
| Necrotizing soft tissue infections |
| Refractory osteomyelitis |
| Severe anaemia |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortega, M.A.; Fraile-Martinez, O.; García-Montero, C.; Callejón-Peláez, E.; Sáez, M.A.; Álvarez-Mon, M.A.; García-Honduvilla, N.; Monserrat, J.; Álvarez-Mon, M.; Bujan, J.; et al. A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina 2021, 57, 864. https://doi.org/10.3390/medicina57090864
Ortega MA, Fraile-Martinez O, García-Montero C, Callejón-Peláez E, Sáez MA, Álvarez-Mon MA, García-Honduvilla N, Monserrat J, Álvarez-Mon M, Bujan J, et al. A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina. 2021; 57(9):864. https://doi.org/10.3390/medicina57090864
Chicago/Turabian StyleOrtega, Miguel A., Oscar Fraile-Martinez, Cielo García-Montero, Enrique Callejón-Peláez, Miguel A. Sáez, Miguel A. Álvarez-Mon, Natalio García-Honduvilla, Jorge Monserrat, Melchor Álvarez-Mon, Julia Bujan, and et al. 2021. "A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities" Medicina 57, no. 9: 864. https://doi.org/10.3390/medicina57090864
APA StyleOrtega, M. A., Fraile-Martinez, O., García-Montero, C., Callejón-Peláez, E., Sáez, M. A., Álvarez-Mon, M. A., García-Honduvilla, N., Monserrat, J., Álvarez-Mon, M., Bujan, J., & Canals, M. L. (2021). A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina, 57(9), 864. https://doi.org/10.3390/medicina57090864












