Functional Mitral Regurgitation in Patients with Preserved Ejection Fraction Qualified for Pulmonary Vein Isolation: A Negative Prognostic Factor for Catheter Ablation Efficacy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methods
2.2. Laboratory Testing
2.3. Echocardiography
2.4. Definitions
2.5. PVI Procedure
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of Study Population
3.2. Echocardiographic Assessment
3.3. F-MR Grade Assessed in TEE
3.4. Three-Month PVI Efficacy
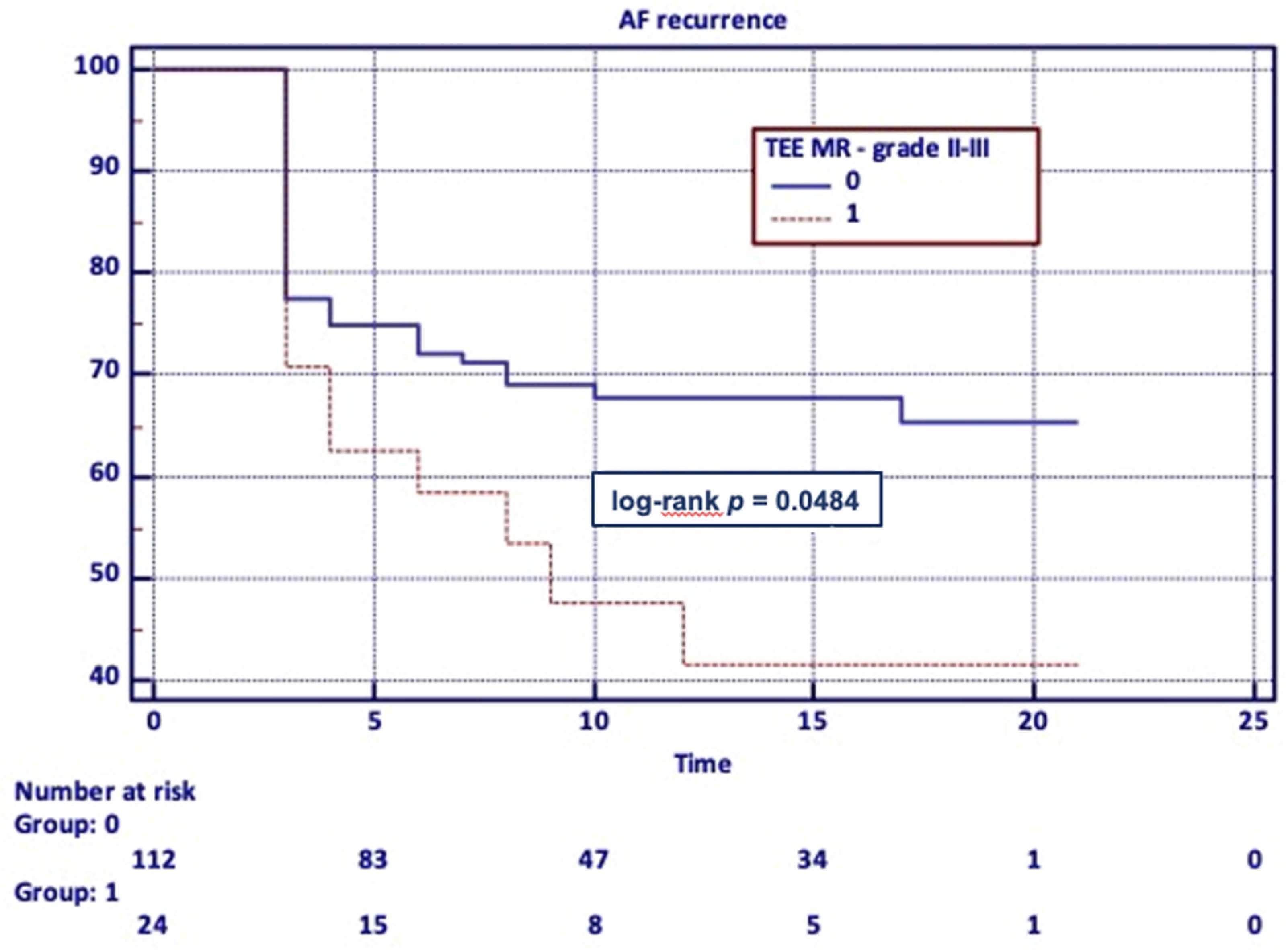
3.5. Long-Term PVI Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deferm, S.; Bertrand, P.B.; Verbrugge, F.; Verhaert, D.; Rega, F.; Thomas, J.D.; Vandervoort, P.M. Atrial Functional Mitral Regurgitation. J. Am. Coll. Cardiol. 2019, 73, 2465–2476. [Google Scholar] [CrossRef] [PubMed]
- Kagiyama, N.; Mondillo, S.; Yoshida, K.; Mandoli, G.E.; Cameli, M. Subtypes of Atrial Functional Mitral Regurgitation. Cardiovasc. Imaging 2020, 13, 820–835. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.J.; Silvestry, F.E. Mechanistic insights into mitral regurgitation due to atrial fibrillation: “Atrial functional mitral regurgitation”. Trends Cardiovasc. Med. 2016, 26, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Lancellotti, P.; Tribouilloy, C.; Hagendorff, A.; Popescu, B.A.; Edvardsen, T.; Pierard, L.A.; Badano, L.; Zamorano, J.L. Recommendations for the echocardiographic assessment of native valvular regurgitation: An executive summary from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 611–644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collabora-tion with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Kumagai, K.; Ogawa, M.; Noguchi, H.; Tojo, H.; Matsumoto, N.; Saku, K. Predictors of successful catheter ablation for atrial fibrillation using the pulmonary vein isolation technique. J. Cardiol. 2004, 44, 15373237. [Google Scholar]
- Abe, Y.; Takahashi, Y.; Shibata, T. A new disease entity: Atrial functional mitral regurgitation. J. Cardiol. 2021, 77, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Jiang, W.; Zhou, L.; Gu, J.; Wang, Y.; Liu, Y.; Zhang, X.; Wu, S.; Liu, X. The role of valvular regurgitation in catheter ablation outcomes of patients with long-standing persistent atrial fibrillation. Europace 2013, 16, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Gertz, Z.; Raina, A.; Mountantonakis, S.E.; Zado, E.; Callans, D.J.; Marchlinski, F.; Keane, M.G.; Silvestry, F.E. The impact of mitral regurgitation on patients undergoing catheter ablation of atrial fibrillation. Europace 2011, 13, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Wu, L.; Hou, B.; Sun, W.; Zheng, L.; Ding, L.; Chen, G.; Zhang, S.; Yao, Y. Functional mitral regurgitation. Medicine 2016, 95, e4333. [Google Scholar] [CrossRef] [PubMed]
- Gertz, Z.M.; Raina, A.; Saghy, L.; Zado, E.; Callans, D.J.; Marchlinski, F.; Keane, M.; Silvestry, F.E. Evidence of Atrial Functional Mitral Regurgitation Due to Atrial Fibrillation: Reversal with Arrhythmia Control. J. Am. Coll. Cardiol. 2011, 58, 1474–1481. [Google Scholar] [CrossRef] [PubMed]
- Nishino, S.; Watanabe, N.; Ashikaga, K.; Morihisa, K.; Kuriyama, N.; Asada, Y.; Shibata, Y. Reverse Remodeling of the Mitral Valve Complex After Radiofrequency Catheter Ablation for Atrial Fibrillation. Circ. Cardiovasc. Imaging 2019, 12, e009317. [Google Scholar] [CrossRef] [PubMed]
| Variable | Absolute Count and Percentage | |
|---|---|---|
| TTE | TEE | |
| F-MR any grade | 101 (74.3%) | 129 (94.9%) |
| F-MR trace | 36 (26.5%) | 24 (17.6%) |
| F-MR mild | 59 (43.4%) | 81 (59.6%) |
| F-MR moderate | 5 (3.7%) | 22 (16.2%) |
| F-MR severe | 1 (0.7%) | 2 (1.5%) |
| Variable | Absolute Count and Percentage or Median and 25–75 Percentile or Mean ± Standard Deviation | p | |
|---|---|---|---|
| Moderate to Severe F-MR | |||
| No n = 112 | Yes n = 24 | ||
| Age (years) | 58.6 (11.0) | 62 (9.1) | 0.102 |
| Sex (F/M) | 41/71 | 6/18 | 0.278 |
| Weight (kg) | 85.29 (14.6) | 86.69 (18.6) | 0.857 |
| Height (cm) | 172.56 (9.7) | 171.17 (8.9) | 0.587 |
| BMI (kg/cm2) | 28.57 (3.9) | 29.37 (4.7) | 0.423 |
| Paroxysmal AF | 92 (82.1%) | 18 (75.0%) | 0.728 |
| Persistent AF | 17 (15.8%) | 5 (20.8%) | 0.495 |
| Long-standing persistent AF | 3 (2.7%) | 1 (4.2%) | 0.695 |
| CHA2DS2-VASc | 2 (1–3) | 2 (1–3) | 0.822 |
| EHRA | |||
| 1 | 2 (1.8%) | 0 (0%) | 0.510 |
| 2 | 54 (48.2%) | 13 (54.2%) | 0.597 |
| 2a | 5 (4.5%) | 2 (8.3%) | 0.436 |
| 2b | 49 (43.8%) | 11 (45.8%) | 0.852 |
| 3 | 52 (46.4%) | 10 (41.7%) | 0.671 |
| 4 | 4 (3.6%) | 1 (4.2%) | 0.088 |
| HFpEF | 4 (4.6%) | 4 (8.2%) | 0.396 |
| Echocardiographic parameters | |||
| LV EF (%) | 56.13 (3.9) | 55.08 (3.5) | 0.181 |
| LA (mm) | 40.00 (4.5) | 42.96 (5.5) | 0.016 |
| LAA (cm2) | 21.59 (4.3) | 23.27 (5.0) | 0.136 |
| MV E/A | 1.14 (0.5) | 1.16 (0.6) | 0.976 |
| LV EDD (mm) | 50.85 (5.3) | 52.71 (5.1) | 0.092 |
| LV ESD (mm) | 30.40 (5.3) | 31.25 (4.5) | 0.350 |
| RWT | 0.38 (0.08) | 0.37 (0.1) | 0.675 |
| LV mass index (g/m2) | 103.91 (30.1) | 111.23 (24.2) | 0.097 |
| Creatinine (mg/dL) | 0.91 (0.21) | 1.06 (0.25) | 0.006 |
| eGFR (mL/min/1.73 m2) | 80.99 (12.58) | 72.83 (17.25) | 0.036 |
| TR mild in TTE | 3 (2.68%) | 3 (12.5%) | 0.033 |
| TR mild in TEE | 10 (9.01) | 7 (29.17) | 0.007 |
| 3-month PVI efficacy | 86 (76.8%) | 17 (70.8%) | 0.537 |
| Long-term PVI efficacy | 36 (32.1%) | 13 (54.2%) | 0.041 |
| Variable | Absolute Count and Percentage or Median and 25–75 Percentile or Mean ± Standard Deviation | p | |
|---|---|---|---|
| Three-Month PVI Efficiency | |||
| No n = 33 | Yes n = 103 | ||
| Age (years) | 60.15 (8.7) | 59.02 (11.4) | 0.945 |
| Sex (F/M) | 11/22 | 36/67 | 0.865 |
| Weight (kg) | 85.85 (15.2) | 85.43 (15.4) | 0.887 |
| Height (cm) | 173.24 (8.9) | 172.02 (9.8) | 0.388 |
| BMI (kg/cm2) | 28.48 (3.8) | 28.79 (4.2) | 0.726 |
| Paroxysmal AF | 27 (81.8%) | 80 (80.6%) | 0.728 |
| Persistent AF | 6 (18.2%) | 16 (15.6%) | 0.719 |
| Long-standing persistent AF | 0 (0.0%) | 4 (3.9%) | 0.251 |
| CHA2DS2-VASc | 2 (1–3) | 2 (1–3) | 0.619 |
| EHRA | |||
| 1 | 0 (0.0%) | 2 (1.9%) | 0.420 |
| 2 | 16 (48.9%) | 51 (49.5%) | 0.918 |
| 2a | 2 (6.1%) | 5 (4.9%) | 0.785 |
| 2b | 14 (42.4%) | 46 (44.7%) | 0.822 |
| 3 | 13 (39.4%) | 49 (47.6%) | 0.412 |
| 4 | 4 (12.2%) | 1 (0.9%) | 0.003 |
| HFpEF | 4 (12.2%) | 4 (3.8%) | 0.08 |
| Echocardiographic parameters | |||
| LV EF (%) | 56.39 (5.3) | 55.81 (3.6) | 0.374 |
| LA (mm) | 40.45 (5.4) | 40.54 (4.7) | 0.807 |
| LAA (cm2) | 22.07 (4.3) | 21.84 (4.5) | 0.949 |
| MV E/A | 1.09 (0.4) | 1.16 (0.5) | 0.738 |
| LV EDD (mm) | 51.67 (5.43) | 51.02 (5.3) | 0.470 |
| LV ESD (mm) | 31.36 (5.2) | 31.3 (5.1) | 0.246 |
| RWT | 0.36 (0.06) | 0.39 (0.1) | 0.086 |
| LV mass index (g/m2) | 101.21 (24.1) | 106.48 (30.7) | 0.352 |
| TTE F-MR any grade | 24 (72.7%) | 77(74.8%) | 0.816 |
| TTE F-MR trace | 9 (27.3%) | 27 (26.2%) | 0.904 |
| TTE F-MR mild | 13 (39.4%) | 46 (44.7%) | 0.595 |
| TTE F-MR moderate | 1 (3.0%) | 4 (3.9%) | 0.821 |
| TTE F-MR severe | 1 (3.0%) | 0 (0.0%) | 0.076 |
| TTE F-MR moderate-severe | 2 (6.1%) | 4 (3.9%) | 0.596 |
| TEE F-MR any grade | 31 (93.9%) | 98 (95.6%) | 0.785 |
| TEE F-MR trace | 8 (24.2%) | 16 (15.5%) | 0.253 |
| TEE F-MR mild | 16 (48.5%) | 65 (63.1%) | 0.253 |
| TEE F-MR moderate | 5 (15.2%) | 17 (16.5%) | 0.854 |
| TEE F-MR severe | 2 (6.0%) | 0 (0.0%) | 0.012 |
| TEE F-MR moderate-severe | 7 (21.2%) | 17 (16.5%) | 0.537 |
| Variable | Absolute Count and Percentage or Median and 25–75 Percentile or Mean ± Standard Deviation | p | |
|---|---|---|---|
| Long-Term PVI Efficacy | |||
| Yes n = 87 | No n = 49 | ||
| Age (years) | 58.0 (11.8) | 61 (8.5) | 0.399 |
| Sex (F/M) | 29/58 | 18/31 | 0.689 |
| Weight (kg) | 86.27 (14.9) | 84.22 (16) | 0.457 |
| Height (cm) | 172.14 (9.4) | 172.63 (9.9) | 0.773 |
| BMI (kg/cm2) | 29.07 (4.3) | 28.08 (3.6) | 0.176 |
| Paroxysmal AF | 70 (80.4%) | 40 (81.6%) | 0.728 |
| Persistent AF | 14 (16%) | 8 (16.3%) | 0.972 |
| Long-standing persistent AF | 3 (3,5%) | 1 (2%) | 0.641 |
| CHA2DS2-VASc | 2 (1–3) | 2 (1–3) | 0.926 |
| EHRA | |||
| 1 | 2 (2.3%) | 0 (0%) | 0.285 |
| 2 | 44 (50.6%) | 23 (46.9%) | 0.684 |
| 2a | 5 (5.7%) | 2 (4%) | 0.673 |
| 2b | 39 (44.8%) | 21 (42.9%) | 0.824 |
| 3 | 40 (45.9%) | 22 (44.9%) | 0.903 |
| 4 | 1 (1.2%) | 4 (8.2%) | 0.037 |
| HFpEF | 4 (4.6%) | 4 (8.2%) | 0.396 |
| Echocardiographic parameters | |||
| LV EF (%) | 55.80 (3.8) | 56.20 (3.9) | 0.427 |
| LA (mm) | 40.66 (4.9) | 40.29 (4.9) | 0.797 |
| LAA (cm2) | 22.19 (4.5) | 21.38 (4.3) | 0.307 |
| MV E/A | 1.2 (0.5) | 1.05 (0.5) | 0.123 |
| LV EDD (mm) | 51.08 (5.4) | 51.35 (5.1) | 0.691 |
| LV ESD (mm) | 30.30 (5.2) | 31 (5.0) | 0.344 |
| RWT | 0.39 (0.09) | 0.36 (0.1) | 0.074 |
| LV mass index (g/m2) | 106.82 (32.1) | 102.33 (23.4) | 0.515 |
| TTE F-MR any grade | 61 (70.1%) | 40 (81.6%) | 0.140 |
| TTE F-MR trace | 23 (26.4%) | 13 (26.5%) | 0.990 |
| TTE F-MR mild | 35 (40.2%) | 24 (48.9%) | 0.323 |
| TTE F-MR moderate | 3 (3.5%) | 2 (4.1%) | 0.851 |
| TTE F-MR severe | 0 (0.0%) | 1 (2.04%) | 0.181 |
| TTE F-MR moderate-severe | 3 (3.5%) | 3 (6.1%) | 0.466 |
| TEE F-MR any grade | 82 (94.3%) | 47 (95.9%) | 0.673 |
| TEE F-MR trace | 16 (18.4%) | 8 (16.3%) | 0.762 |
| TTE F-MR mild | 55 (63.2%) | 26 (53.0%) | 0.242 |
| TTE F-MR moderate | 11 (12.6%) | 11 (22.5%) | 0.136 |
| TTE F-MR severe | 0 (0%) | 2 (4.1%) | 0.058 |
| TTE F-MR moderate-severe | 11 (12.6%) | 13 (26.5%) | 0.041 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cichoń, M.; Wybraniec, M.; Mizia-Szubryt, M.; Mizia-Stec, K. Functional Mitral Regurgitation in Patients with Preserved Ejection Fraction Qualified for Pulmonary Vein Isolation: A Negative Prognostic Factor for Catheter Ablation Efficacy. Medicina 2021, 57, 798. https://doi.org/10.3390/medicina57080798
Cichoń M, Wybraniec M, Mizia-Szubryt M, Mizia-Stec K. Functional Mitral Regurgitation in Patients with Preserved Ejection Fraction Qualified for Pulmonary Vein Isolation: A Negative Prognostic Factor for Catheter Ablation Efficacy. Medicina. 2021; 57(8):798. https://doi.org/10.3390/medicina57080798
Chicago/Turabian StyleCichoń, Małgorzata, Maciej Wybraniec, Magdalena Mizia-Szubryt, and Katarzyna Mizia-Stec. 2021. "Functional Mitral Regurgitation in Patients with Preserved Ejection Fraction Qualified for Pulmonary Vein Isolation: A Negative Prognostic Factor for Catheter Ablation Efficacy" Medicina 57, no. 8: 798. https://doi.org/10.3390/medicina57080798
APA StyleCichoń, M., Wybraniec, M., Mizia-Szubryt, M., & Mizia-Stec, K. (2021). Functional Mitral Regurgitation in Patients with Preserved Ejection Fraction Qualified for Pulmonary Vein Isolation: A Negative Prognostic Factor for Catheter Ablation Efficacy. Medicina, 57(8), 798. https://doi.org/10.3390/medicina57080798






