Development of a Rapid Diagnostic Kit for Congestive Heart Failure Using Recombinant NT-proBNP Antigen
Abstract
:1. Introduction
2. Materials and Methods
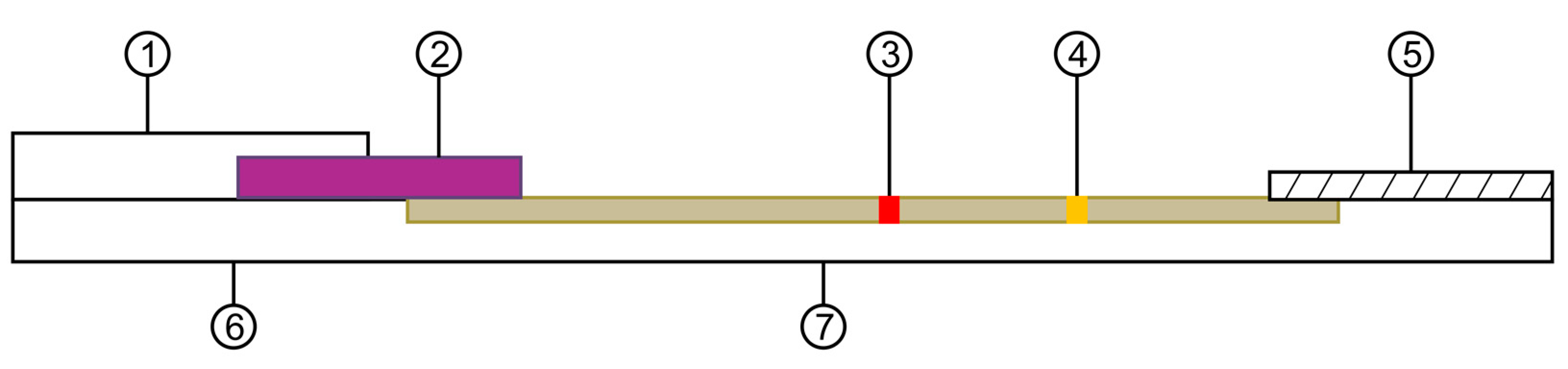
2.1. NT-proBNP Gene Synthesis and Cloning
2.2. Expression Vector Subcloning
2.3. Recombinant Protein Expression and Purification
2.4. Mouse Immunization and Cell Fusion
2.5. Hybridoma Screening
2.6. Monoclonal Cell Selection and Culture
2.7. Ascites Production and Mass Production of Monoclonal Antibodies
2.8. Purification of Monoclonal Antibodies
2.9. Preparation of Gold Nanoparticles and Antibody Conjugates
2.10. Rapid Diagnosis Kit Production and Components
2.11. Antigen-Antibody Reactivity Test
2.12. Statistical Analysis
3. Results
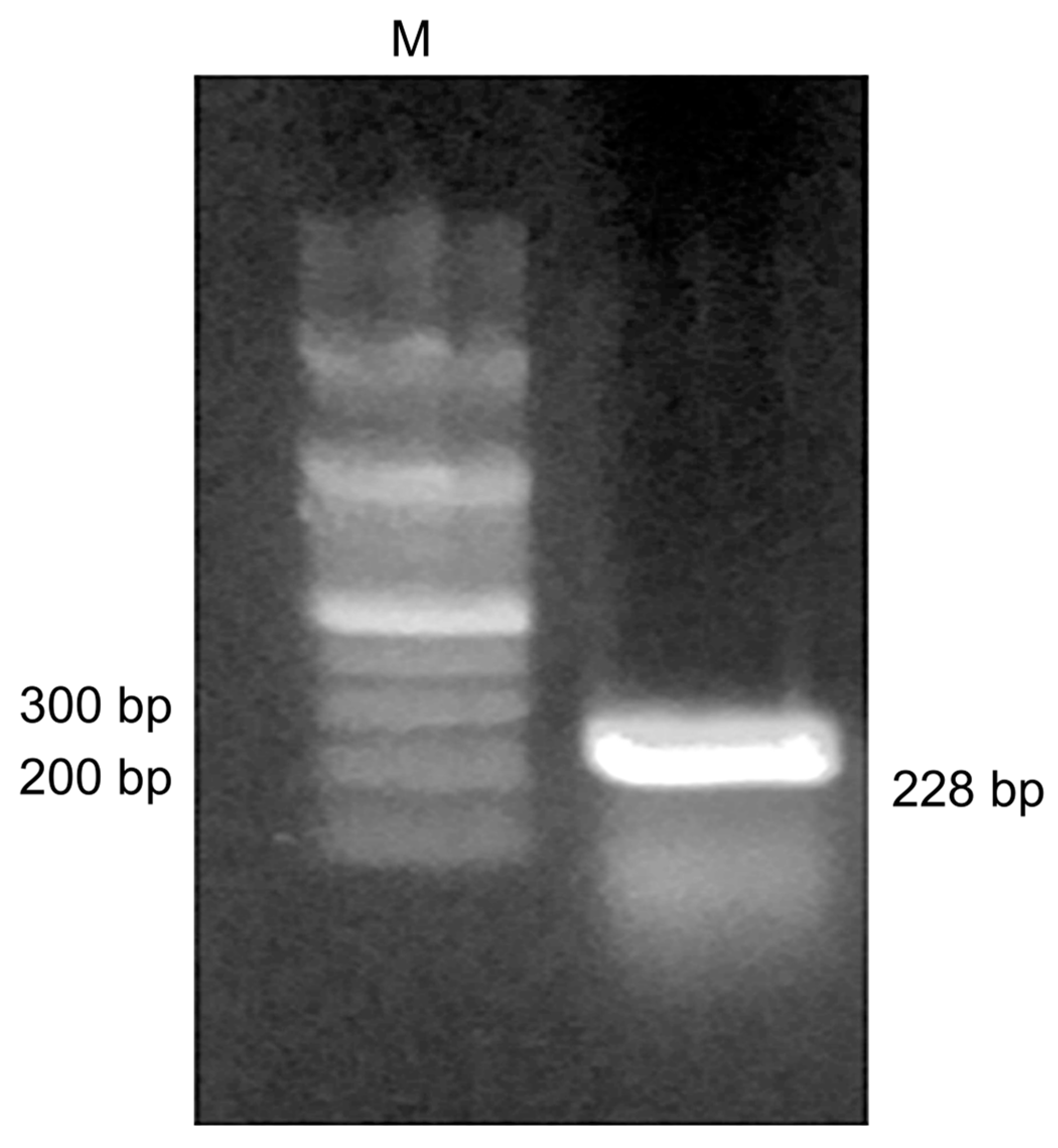
3.1. NT-proBNP Gene Synthesis and Cloning
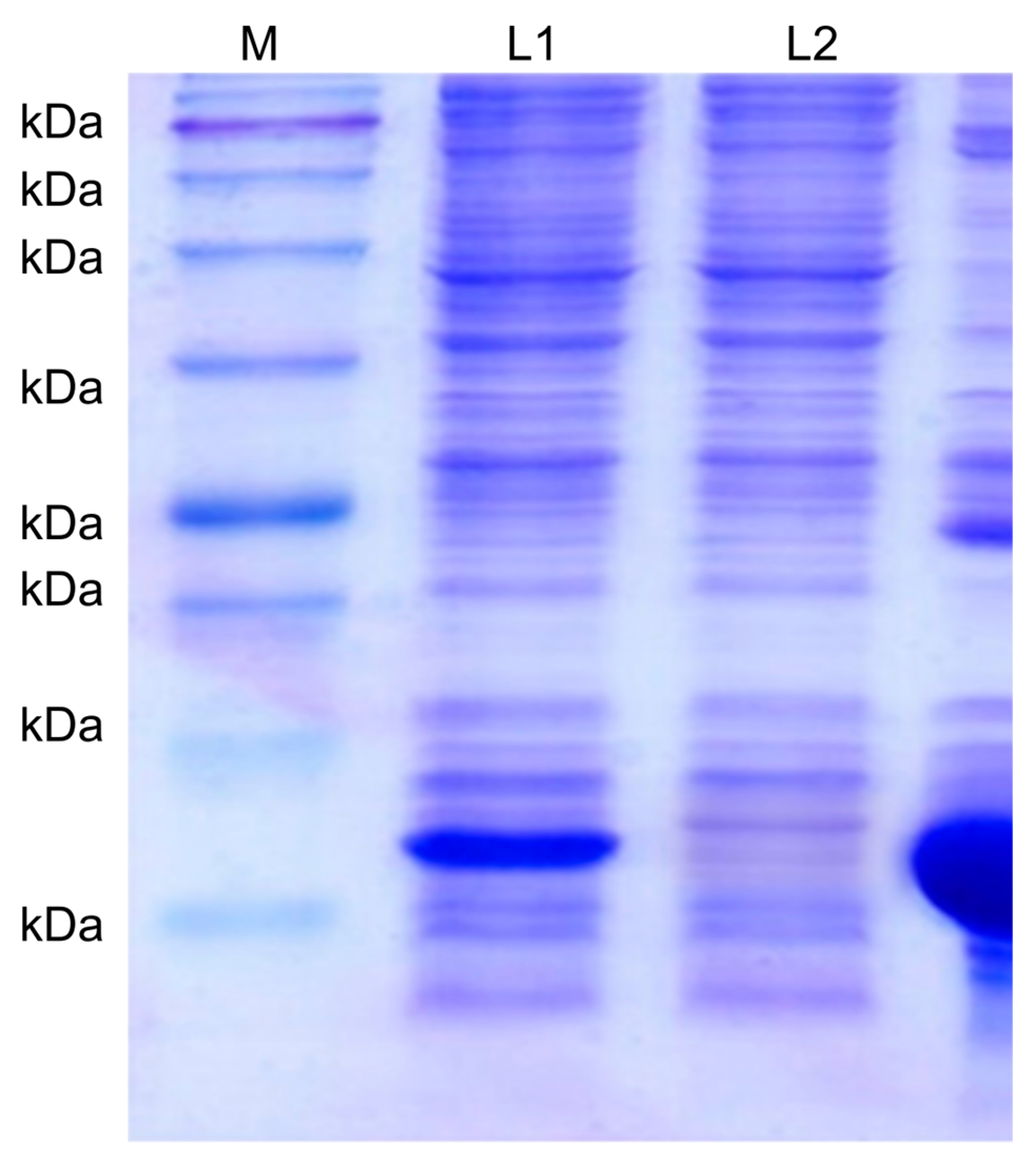
3.2. Recombinant Protein Expression and Purification
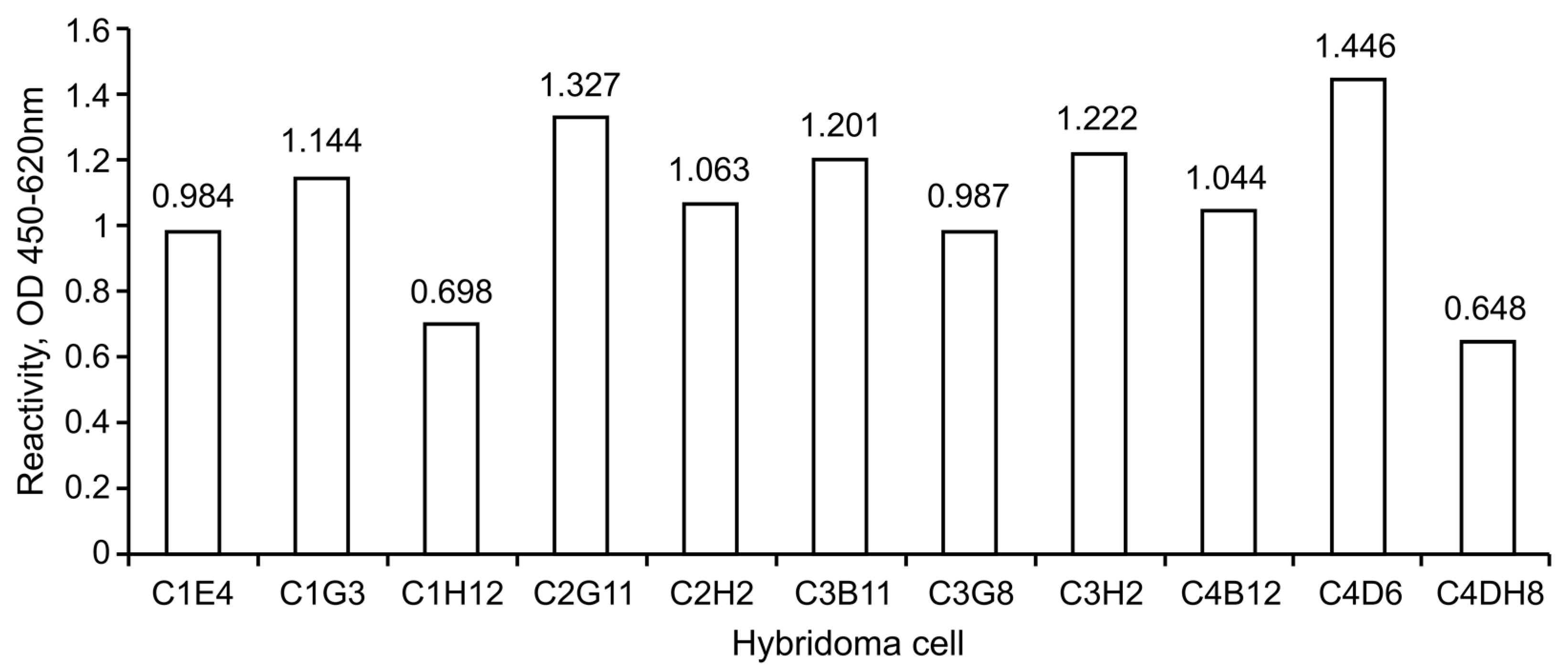
3.3. Immunization and Hybridoma Screening
3.4. Mass Production and Purification of Monoclonal Antibodies
3.5. Monoclonal Antibody Pair Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dunlay, S.M.; Shah, N.D.; Shi, Q.; Morlan, B.; VanHouten, H.; Long, K.H.; Roger, V.L. Lifetime Costs of Medical Care After Heart Failure Diagnosis. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 68–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, S.; Vasan, R.S. Advances in the Epidemiology of Heart Failure and Left Ventricular Remodeling. Circulation 2011, 124, e516–e519. [Google Scholar] [CrossRef] [Green Version]
- Sardu, C.; Marfella, R.; Santamaria, M.; Papini, S.; Parisi, Q.; Sacra, C.; Colaprete, D.; Paolisso, G.; Rizzo, M.R.; Barbieri, M. Stretch, Injury and Inflammation Markers Evaluation to Predict Clinical Outcomes After Implantable Cardioverter Defibrillator Therapy in Heart Failure Patients With Metabolic Syndrome. Front. Physiol. 2018, 9, 758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, C. NT-ProBNP: The Mechanism Behind the Marker. J. Card. Fail. 2005, 11, S81–S83. [Google Scholar] [CrossRef]
- Lu, Z.; Wang, B.; Wang, Y.; Qian, X.; Zheng, W.; Wei, M. Relationship between CCR and NT-proBNP in Chinese HF Patients, and Their Correlations with Severity of HF. BioMed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grewal, J.; McKelvie, R.; Lonn, E.; Tait, P.; Carlsson, J.; Gianni, M.; Jarnert, C.; Persson, H. BNP and NT-proBNP predict echocardiographic severity of diastolic dysfunction. Eur. J. Heart Fail. 2008, 10, 252–259. [Google Scholar] [CrossRef] [Green Version]
- Hall, C. Essential biochemistry and physiology of (NT-pro)BNP. Eur. J. Heart Fail. 2004, 6, 257–260. [Google Scholar] [CrossRef]
- Sarangadharan, I.; Huang, S.-W.; Kuo, W.-C.; Chen, P.-H.; Wang, Y.-L. Rapid detection of NT-proBNP from whole blood using FET based biosensors for homecare. Sens. Actuators B Chem. 2019, 285, 209–215. [Google Scholar] [CrossRef]
- Pfister, R.; Scholz, M.; Wielckens, K.; Erdmann, E.; Schneider, C. Use of NT-proBNP in routine testing and comparison to BNP. Eur. J. Heart Fail. 2004, 6, 289–293. [Google Scholar] [CrossRef] [Green Version]
- Salah, K.; Stienen, S.; Pinto, Y.M.; Eurlings, L.W.; Metra, M.; Bayes-Genis, A.; Verdiani, V.; Tijssen, J.G.P.; Kok, W.E. Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction. Heart 2019, 105, 1182–1189. [Google Scholar] [CrossRef] [Green Version]
- Sardu, C.; Paolisso, P.; Sacra, C.; Santamaria, M.; De Lucia, C.; Ruocco, A.; Mauro, C.; Paolisso, G.; Rizzo, M.R.; Barbieri, M.; et al. Cardiac resynchronization therapy with a defibrillator (CRTd) in failing heart patients with type 2 diabetes mellitus and treated by glucagon-like peptide 1 receptor agonists (GLP-1 RA) therapy vs. conventional hypoglycemic drugs: Arrhythmic burden, hospitalizations for heart failure, and CRTd responders rate. Cardiovasc. Diabetol. 2018, 17, 137. [Google Scholar] [CrossRef] [PubMed]
- Sardu, C.; Paolisso, P.; Ducceschi, V.; Santamaria, M.; Sacra, C.; Massetti, M.; Ruocco, A.; Marfella, R. Cardiac resynchronization therapy and its effects in patients with type 2 DIAbetes mellitus OPTimized in automatic vs. echo guided approach. Data from the DIA-OPTA investigators. Cardiovasc. Diabetol. 2020, 19. [Google Scholar] [CrossRef]
- Dębska-Kozłowska, A.; Książczyk, M.; Warchol, I.; Lubinski, A. Clinical Usefulness of N-terminal Prohormone of Brain Natriuretic Peptide and High Sensitivity Troponin T in Patients with Heart Failure Undergoing Cardiac Resynchronization Therapy. Curr. Pharm. Des. 2019, 25, 1671–1678. [Google Scholar] [CrossRef] [PubMed]
- Vasheghani-Farahani, A.; Sherafati, A. Usefulness of Biomarkers for Predicting Response to Cardiac Resynchronization Therapy. Curr. Cardiol. Rev. 2020, 16, 132–140. [Google Scholar] [CrossRef]
- San-Miguel, T.; Pérez-Bermúdez, P.; Gavidia, I. Production of soluble eukaryotic recombinant proteins in E. coli is favoured in early log-phase cultures induced at low temperature. SpringerPlus 2013, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bornhorst, J.A.; Falke, J.J. [16] Purification of proteins using polyhistidine affinity tags. Methods Enzymol. 2000, 326, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laemmli, U.K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 1970, 227, 680–685. [Google Scholar] [CrossRef]
- Gopal, D.J.; Iqbal, M.N.; Maisel, A. Updating the Role of Natriuretic Peptide Levels in Cardiovascular Disease. Postgrad. Med. 2011, 123, 102–113. [Google Scholar] [CrossRef]
- Anguita, M.; Montes, P.; Jordán, A.; Casares, G.; Gómez, I.; Recio, J.; Martínez, Á.; Zumalde, J.; Povar, J.; Ridocci, R.; et al. Utility of NT-proBNP for diagnosing heart failure in a heterogeneous population of patients with dyspnea. Spanish multicenter study. Rev. Esp. Cardiol. 2006, 59, 465–472. [Google Scholar] [CrossRef]
- Hobbs, F.D.R.; Davis, R.C.; Roalfe, A.K.; Hare, R.; Davies, M.K.; Kenkre, J.E. Reliability of N-terminal pro-brain natriuretic peptide assay in diagnosis of heart failure: Cohort study in representative and high risk community populations. BMJ 2002, 324, 1498. [Google Scholar] [CrossRef] [Green Version]
- Farnsworth, C.W.; Bailey, A.L.; Jaffe, A.S.; Scott, M.G. Diagnostic concordance between NT-proBNP and BNP for suspected heart failure. Clin. Biochem. 2018, 59, 50–55. [Google Scholar] [CrossRef]
- Masson, S.; Latini, R.; Anand, I.S.; Vago, T.; Angelici, L.; Barlera, S.; Missov, E.D.; Clerico, A.; Tognoni, G.; Cohn, J.N. Direct Comparison of B-Type Natriuretic Peptide (BNP) and Amino-Terminal proBNP in a Large Population of Patients with Chronic and Symptomatic Heart Failure: The Valsartan Heart Failure (Val-HeFT) Data. Clin. Chem. 2006, 52, 1528–1538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alawieh, H.; El Chemaly, T.; Alam, S.; Khraiche, M. Towards Point-of-Care Heart Failure Diagnostic Platforms: BNP and NT-proBNP Biosensors. Sensors 2019, 19, 5003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soleh, M.T.; Foo, J.Y.Y.; Bailey, U.-M.; Tan, N.Y.; Wan, Y.; Cooper-White, J.; Schulz, B.L.; Punyadeera, C. A rapid and cost-effective method of producing recombinant proBNP and NT-proBNP variants in Escherichia coli for immunoassay of heart failure. Biotechnol. Lett. 2014, 36, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Karisa, N.; Jeon, W.Y.; Lee, H.; Kim, Y.-C.; Ahn, J. High-level production of N-terminal pro-brain natriuretic peptide, as a calibrant of heart failure diagnosis, in Escherichia coli. Appl. Microbiol. Biotechnol. 2019, 103, 4779–4788. [Google Scholar] [CrossRef]
- Braunwald, E. Biomarkers in Heart Failure. N. Engl. J. Med. 2008, 358, 2148–2159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Usuku, H.; Nakayama, M.; Sumida, H.; Yamamuro, M.; Izumiya, Y.; Suzuki, S.; Kusuhara, K.; Ueno, H.; Sugiyama, S.; Yoshimura, M.; et al. Pump failure death and sudden cardiac death in patients with cardiac dysfunction: A search for prognostic predictive factors—A long-term follow-up study. J. Cardiol. 2010, 55, 55–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Gene | Amino Acid Sequence |
|---|---|
| NT-proBNP | 001-HPLGSPGSASDLETSGLQEQRNHLQGKLSE |
| 031-LQVEQTSLEPLQESPRPTGVWKSREVATEG | |
| 061-IRGHRKMVLYTLRAPR |
| Gene | Amino Acid Sequence | |
|---|---|---|
| NT-proBNP | Forward | 5′- AAG CTT CAC CCG CTG GGC AGC CCC-3′ |
| Reverse | 5′- CTC GAG TCG TGG TGC CCG CAG GGT-3′ | |
| Plate 1 | C1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| A | 0.422 | 0.472 | 0.303 | 0.353 | 0.3 | 0.411 | 0.289 | 0.338 | 0.335 | 0.258 | 0.292 | 0.398 | |
| B | 0.281 | 0.274 | 0.313 | 0.304 | 0.247 | 0.76 | 0.263 | 0.275 | 0.284 | 0.275 | 0.258 | 0.295 | |
| C | 0.288 | 0.233 | 0.72 | 0.263 | 0.249 | 0.3 | 0.287 | 0.259 | 0.267 | 0.287 | 0.261 | 0.283 | |
| D | 0.348 | 0.26 | 0.29 | 0.265 | 0.287 | 0.263 | 0.258 | 0.277 | 0.585 | 0.222 | 0.693 | 0.303 | |
| E | 0.31 | 0.254 | 0.684 | 1.043 | 0.265 | 0.289 | 0.279 | 0.479 | 0.232 | 0.242 | 0.237 | 0.308 | |
| F | 0.37 | 0.225 | 0.268 | 0.272 | 0.305 | 0.451 | 0.275 | 0.302 | 0.307 | 0.267 | 0.294 | 0.278 | |
| G | 0.355 | 0.276 | 1.197 | 0.334 | 0.325 | 0.231 | 0.251 | 0.287 | 0.292 | 0.253 | 0.274 | 0.308 | |
| H | 0.325 | 0.333 | 0.337 | 0.303 | 0.366 | 0.347 | 0.27 | 0.308 | 0.264 | 0.279 | 0.282 | 0.833 | |
| Plate 2 | C2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| A | 0.307 | 0.309 | 0.276 | 0.27 | 0.332 | 0.342 | 0.281 | 0.252 | 0.297 | 0.299 | 0.298 | 0.358 | |
| B | 0.281 | 0.25 | 0.282 | 0.269 | 0.28 | 0.303 | 0.288 | 0.302 | 0.267 | 0.241 | 0.239 | 0.315 | |
| C | 0.454 | 0.293 | 0.272 | 0.302 | 0.281 | 0.27 | 0.258 | 0.253 | 0.259 | 0.27 | 0.218 | 0.342 | |
| D | 0.304 | 0.26 | 0.289 | 0.317 | 0.313 | 0.28 | 0.32 | 0.321 | 0.288 | 0.253 | 0.253 | 0.275 | |
| E | 0.3 | 0.255 | 0.334 | 0.287 | 0.289 | 0.282 | 0.298 | 0.278 | 0.295 | 0.279 | 0.298 | 0.25 | |
| F | 0.254 | 0.249 | 0.275 | 0.439 | 0.263 | 0.288 | 0.46 | 0.279 | 0.34 | 0.259 | 0.252 | 0.278 | |
| G | 0.311 | 0.359 | 343 | 0.278 | 0.31 | 0.29 | 0.381 | 0.286 | 0.347 | 0.287 | 1.137 | 0.465 | |
| H | 0.411 | 0.984 | 0.295 | 0.272 | 0.287 | 0.284 | 0.289 | 0.525 | 0.341 | 0.254 | 0.313 | 0.317 | |
| Plate 3 | C3 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| A | 0.497 | 0.384 | 0.444 | 0.375 | 0.447 | 0.399 | 0.353 | 0.477 | 0.43 | 0.41 | 0.48 | 0.661 | |
| B | 0.364 | 0.371 | 0.356 | 0.364 | 0.368 | 0.312 | 0.339 | 0.378 | 0.369 | 0.385 | 0.934 | 0.41 | |
| C | 0.442 | 0.409 | 0.38 | 0.375 | 465 | 0.398 | 0.38 | 0.407 | 0.357 | 0.461 | 0.357 | 0.389 | |
| D | 0.427 | 0.353 | 0.404 | 0.382 | 0.403 | 0.404 | 0.455 | 0.388 | 0.383 | 0.392 | 0.364 | 0.367 | |
| E | 0.396 | 0.397 | 0.394 | 0.46 | 0.394 | 0.422 | 0.4 | 0.367 | 0.4 | 0.359 | 0.338 | 0.446 | |
| F | 0.418 | 0.352 | 0.401 | 0.422 | 0.379 | 0.408 | 0.4 | 0.436 | 0.385 | 0.33 | 0.319 | 0.406 | |
| G | 0.398 | 0.326 | 0.378 | 0.416 | 0.399 | 0.385 | 0.384 | 0.916 | 0.375 | 0.33 | 0.415 | 0.484 | |
| H | 0.348 | 1.027 | 0.296 | 0.247 | 0.28 | 0.297 | 0.275 | 0.306 | 0.248 | 0.264 | 0.293 | 0.242 | |
| Plate 4 | C4 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| A | 0.301 | 0.265 | 0.324 | 0.371 | 0.435 | 0.44 | 0.387 | 0.402 | 0.387 | 0.356 | 0.365 | 0.397 | |
| B | 0.442 | 0.38 | 0.416 | 0.328 | 0.538 | 0.406 | 0.377 | 0.361 | 0.348 | 0.384 | 0.364 | 0.912 | |
| C | 0.403 | 0.391 | 0.407 | 0.451 | 0.359 | 353 | 0.438 | 0.555 | 0.401 | 0.411 | 0.394 | 602 | |
| D | 0.584 | 0.389 | 0.423 | 0.354 | 0.386 | 1.339 | 0.42 | 0.375 | 0.497 | 0.375 | 0.377 | 356 | |
| E | 0.425 | 0.385 | 0.395 | 0.407 | 0.413 | 416 | 0.371 | 0.363 | 0.418 | 0.424 | 0.304 | 412 | |
| F | 0.433 | 0.387 | 0.423 | 0.4 | 0.449 | 0.371 | 0.361 | 0.343 | 0.372 | 0.349 | 0.346 | 377 | |
| G | 0.383 | 0.332 | 0.28 | 0.383 | 0.378 | 0.333 | 0.379 | 0.381 | 0.321 | 0.341 | 0.325 | 425 | |
| H | 0.373 | 0.315 | 0.373 | 0.37 | 0.403 | 0.364 | 0.385 | 0.843 | 0.406 | 0.359 | 0.322 | 406 |
| G/C | C1G3 | C2G11 | C2H2 | C3B11 | C3H2 | C4B12 | C4D6 |
|---|---|---|---|---|---|---|---|
| C1G3 | − | 1+ | 3+ | 3+ | 2+ | − | − |
| C2G11 | 1+ | − | − | 2+ | 1+ | 1+ | 1+ |
| C2H2 | − | − | − | 3+ | − | 2+ | 3+ |
| C3B11 | 2+ | 1+ | − | 3+ | − | 1+ | 2+ |
| C3H2 | 2+ | − | − | 2+ | − | 1+ | 1+ |
| C4B12 | − | 1+ | 3+ | 3+ | 2+ | − | − |
| C4D6 | − | 1+ | 2+ | 1+ | 1+ | − | − |
| Lane | Specimen | Concentration (ng/mL) | Sex | Age (Years) |
|---|---|---|---|---|
| (1) | Normal serum | - | - | - |
| (2) | Recombinant Antigen | 10 | - | - |
| (3) | Commercial Antigen | 10 | - | - |
| (4) | Patient’s serum ⓵ | 35 | Female | 59 |
| (5) | Patient’s serum ⓶ | 25 | Female | 93 |
| (6) | Patient’s serum ⓷ | 16 | Female | 86 |
| (7) | Patient’s serum ⓸ | 10 | Female | 91 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-K.; Choi, D.-O.; Kim, G.-Y. Development of a Rapid Diagnostic Kit for Congestive Heart Failure Using Recombinant NT-proBNP Antigen. Medicina 2021, 57, 751. https://doi.org/10.3390/medicina57080751
Lee Y-K, Choi D-O, Kim G-Y. Development of a Rapid Diagnostic Kit for Congestive Heart Failure Using Recombinant NT-proBNP Antigen. Medicina. 2021; 57(8):751. https://doi.org/10.3390/medicina57080751
Chicago/Turabian StyleLee, Young-Ki, Dong-Ok Choi, and Ga-Yeon Kim. 2021. "Development of a Rapid Diagnostic Kit for Congestive Heart Failure Using Recombinant NT-proBNP Antigen" Medicina 57, no. 8: 751. https://doi.org/10.3390/medicina57080751
APA StyleLee, Y.-K., Choi, D.-O., & Kim, G.-Y. (2021). Development of a Rapid Diagnostic Kit for Congestive Heart Failure Using Recombinant NT-proBNP Antigen. Medicina, 57(8), 751. https://doi.org/10.3390/medicina57080751







