Exploring Unmet Needs from an Online Metastatic Breast Cancer Support Group: A Qualitative Study
Abstract
:1. Introduction
2. Material and Methods
3. Results
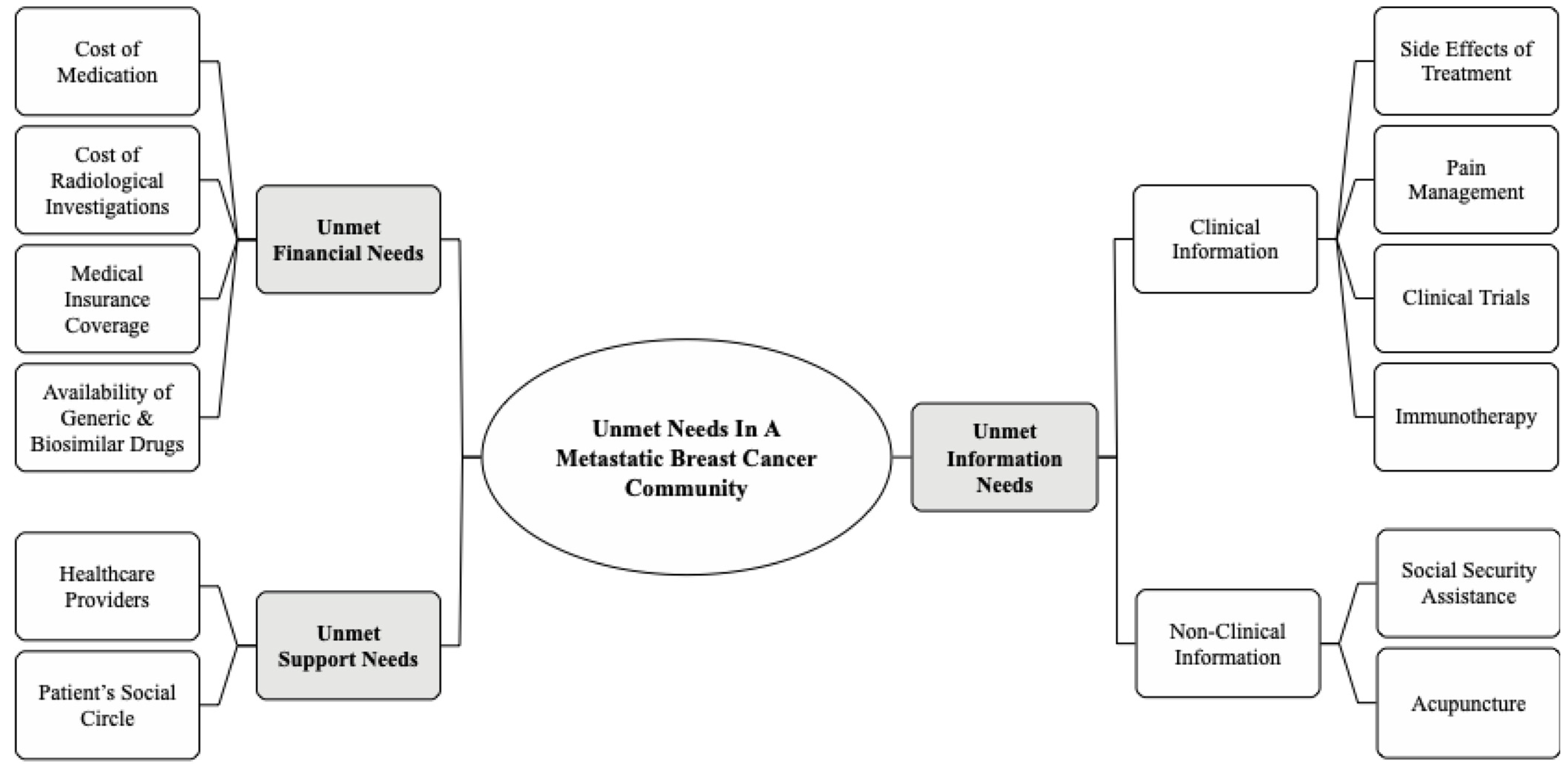
3.1. Unmet Information Needs
3.2. Unmet Financial Needs
3.3. Unmet Support Needs
4. Discussion
4.1. Implications in Clinical Practice
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Taib, N.A.; Yip, C.H.; Low, W.Y. A Grounded Explanation of Why Women Present with Advanced Breast Cancer. World J. Surg. 2014, 38, 1676–1684. [Google Scholar] [CrossRef]
- Saxena, N.; Hartman, M.; Bhoo-Pathy, N.; Lim, J.N.W.; Aw, T.-C.; Iau, P.; Taib, N.A.; Lee, S.-C.; Yip, C.-H.; Verkooijen, H.M. Breast Cancer in South East Asia: Comparison of Presentation and Outcome Between a Middle Income and a High Income Country. World J. Surg. 2012, 36, 2838–2846. [Google Scholar] [CrossRef]
- Cardoso, F.; Harbeck, N.; Mertz, S.; Fenech, D. Evolving psychosocial, emotional, functional, and support needs of women with advanced breast cancer: Results from the Count Us, Know Us, Join Us and Here & Now surveys. Breast 2016, 28, 5–12. [Google Scholar]
- Lewis, S.; Yee, J.; Kilbreath, S.; Willis, K. A qualitative study of women’s experiences of healthcare, treatment and support for metastatic breast cancer. Breast 2015, 24, 242–247. [Google Scholar] [CrossRef]
- Mosher, C.E.; Ms, C.J.; Dickler, M.; Norton, L.; Massie, M.J.; DuHamel, K. Living with Metastatic Breast Cancer: A Qualitative Analysis of Physical, Psychological, and Social Sequelae. Breast J. 2013, 19, 285–292. [Google Scholar] [CrossRef] [Green Version]
- El Saghir, N.S.; Adebamowo, C.A.; Anderson, B.O.; Carlson, R.W.; Bird, P.A.; Corbex, M.; Badwe, R.A.; Bushnaq, M.A.; Eniu, A.; Gralow, J.R.; et al. Breast cancer management in low resource countries (LRCs): Consensus statement from the Breast Health Global Initiative. Breast 2011, 20, S3–S11. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.-H.; Cazap, E.; Anderson, B.O.; Bright, K.L.; Caleffi, M.; Cardoso, F.; Elzawawy, A.M.; Harford, J.B.; Krygier, G.D.; Masood, S.; et al. Breast cancer management in middle-resource countries (MRCs): Consensus statement from the Breast Health Global Initiative. Breast 2011, 20, S12–S19. [Google Scholar] [CrossRef]
- Alaszewski, A. Risk communication: Identifying the importance of social context1. Health Risk Soc. 2005, 7, 101–105. [Google Scholar] [CrossRef]
- Bender, J.L.; Katz, J.; Ferris, L.E.; Jadad, A.R. What is the role of online support from the perspective of facilitators of face-to-face support groups? A multi-method study of the use of breast cancer online communities. Patient Educ. Couns. 2013, 93, 472–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parahoo, K.; Hueter, I.; Northouse, L. Online support groups for women with breast cancer. Cochrane Database Syst. Rev. 2015, 3, CD011652. [Google Scholar] [CrossRef]
- Vilhauer, R.P. Perceived Benefits of Online Support Groups for Women with Metastatic Breast Cancer. Women Health 2009, 49, 381–404. [Google Scholar] [CrossRef]
- Vilhauer, R.P.; McClintock, M.K.; Matthews, A.K. Online Support Groups for Women with Metastatic Breast Cancer: A Feasibility Pilot Study. J. Psychosoc. Oncol. 2010, 28, 560–586. [Google Scholar] [CrossRef]
- Wilson, E.K.A.; Dickson-Swift, V. Using Blogs as a Qualitative Health Research Tool: A Scoping Review. Int. J. Qual. Methods 2015, 14, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Bradshaw JTosnIM, G. (Ed.) Problems and Progress in Medical Care: Essays on Current Research; 7th series; Oxford University Press: London, UK, 1972; pp. 71–82. [Google Scholar]
- Social Security Organization: Invalidity Pension Scheme. Available online: https://www.perkeso.gov.my/index.php/en/social-security-protection-scheme/invalidity-scheme (accessed on 5 April 2020).
- Distelhorst, S.R.; Cleary, J.F.; Ganz, P.A.; Bese, N.; Camacho-Rodriguez, R.; Cardoso, F.; Ddungu, H.; Gralow, R.J.; Yip, C.-H.; Anderson, B.O. Optimisation of the continuum of supportive and palliative care for patients with breast cancer in low-income and middle-income countries: Executive summary of the Breast Health Global Initiative, 2014. Lancet Oncol. 2015, 16, e137–e147. [Google Scholar] [CrossRef]
- Clinical Practice Guidelines for Management of Breast Cancer 2nd edition 2010. Ministry of Health Malaysia. Available online: http://www.acadmed.org.my/index.cfm?&menuid=67#Cancer (accessed on 5 April 2020).
- Seah, D.; Lin, N.; Curley, C.; Winer, E.; Partridge, A. Informational needs and the quality of life of patients in their first year after metastatic breast cancer diagnosis. J. Community Support Oncol. 2014, 12, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M. Lessons Learned From the Metastatic Breast Cancer Community. Semin. Oncol. Nurs. 2010, 26, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Aranda, S.; Schofield, P.; Weih, L.; Yates, P.; Milne, D.; Faulkner, R.; Voudouris, N. Mapping the quality of life and unmet needs of urban women with metastatic breast cancer. Eur. J. Cancer Care Engl. 2005, 14, 211–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danesh, M.; Belkora, J.; Volz, S.; Rugo, H.S.; Danesh, M.; Belkora, J.; Volz, S.; Rugo, H.S. Informational Needs of Patients with Metastatic Breast Cancer: What Questions Do They Ask, and Are Physicians Answering Them? J. Cancer Educ. 2013, 29, 175–180. [Google Scholar] [CrossRef]
- Mellstedt, H.; Gaudernack, G.; Gerritsen, W.R.; Huber, C.; Melero, I.; Parmiani, G.; Scholl, S.; Thatcher, N.; Wagstaff, J.; Zielinski, C. Awareness and understanding of cancer immunotherapy in Europe. Hum. Vaccines Immunother. 2014, 10, 1828–1835. [Google Scholar] [CrossRef] [Green Version]
- Kong, Y.-C.; Wong, L.P.; Ng, C.; Taib, N.A.; Bhoo-Pathy, N.T.; Yusof, M.M.; Aziz, A.F.; Yehgambaram, P.; Ishak, W.Z.W.; Yip, C.; et al. Understanding the Financial Needs Following Diagnosis of Breast Cancer in a Setting with Universal Health Coverage. Oncologist 2020, 25, 497–504. [Google Scholar] [CrossRef] [Green Version]
- Group, A.S.; Kimman, M.; Jan, S.; Yip, C.H.; Thabrany, H.; Peters, S.A. Catastrophic health expenditure and 12-month mortality associated with cancer in Southeast Asia: Results from a longitudinal study in eight countries. BMC Med. 2015, 13, 190. [Google Scholar]
- Datuk, I.M.; Ghazali, R.J.D.M.; Manaf, N.H.A.; Abdullah, A.H.A.; Abu Bakar, A.; Salikin, F.; Umapathy, M.; Ali, R.; Bidin, N.; Ismail, W.I.W. Hospital waiting time: The forgotten premise of healthcare service delivery? Int. J. Health Care Qual. Assur. 2011, 24, 506–522. [Google Scholar] [CrossRef]
- Bhoo-Pathy, N.; Ng, C.-W.; Lim, G.C.-C.; Tamin, N.S.I.; Sullivan, R.; Bhoo-Pathy, N.T.; Abdullah, M.M.; Kimman, M.; Subramaniam, S.; Saad, M.; et al. Financial Toxicity After Cancer in a Setting With Universal Health Coverage: A Call for Urgent Action. J. Oncol. Pract. 2019, 15, e537–e546. [Google Scholar] [CrossRef] [PubMed]
- Lopes Gde, L. Cost comparison and economic implications of commonly used originator and generic chemotherapy drugs in India. Ann Oncol. 2013, 24 (Suppl. 5), v13–v16. [Google Scholar] [CrossRef] [PubMed]
- Beng, T.S.; Guan, N.C.; Jane, L.E.; Chin, L.E. Health Care Interactional Suffering in Palliative Care. Am. J. Hosp. Palliat. Med. 2014, 31, 307–314. [Google Scholar] [CrossRef]
- Thrift-Perry, M.; Cabanes, A.; Cardoso, F.; Hunt, K.M.; Cruz, T.A.; Faircloth, K. Global analysis of metastatic breast cancer policy gaps and advocacy efforts across the patient journey. Breast 2018, 41, 93–106. [Google Scholar] [CrossRef]
| Characteristics | No (%) | |
|---|---|---|
| Age, Years | 41–45 | 3 (13.6) |
| 46–50 | 10 (45.5) | |
| 51–55 | 5 (22.7) | |
| 56–60 | 4 (18.2) | |
| Marital Status | Married | 19 (86.4) |
| Single | 3 (13.6) | |
| Ethnicity | Chinese | 14 (63.6) |
| Malay | 5 (22.7) | |
| Indian | 3 (13.6) | |
| Duration of Metastases | <1 year | 1 (4.5) |
| 1–2 years | 10 (45.5) | |
| 3–5 years | 9 (40.9) | |
| 6–10 years | 2 (9.1) | |
| Initial Diagnosis (EBC) | Metastatic | 6 (27.3) |
| 1–5 years | 11 (50) | |
| 6–10 years | 3 (13.6) | |
| 11–15 years | 2 (9.1) | |
| Location of metastases | Bone only | 8 (36.4) |
| Viscera only | 10 (45.5) | |
| Bone and viscera | 4 (18.2) | |
| Chat Status | Remained | 16 (72.7) |
| Deceased | 4 (18.2) | |
| Left | 2 (9.1) | |
| Unmet Information Needs | |
|---|---|
| Side Effects of Treatment | Anybody having side effects with Eribulin? It works for me, but having tiredness and leg cramp. Now having bad numbness in fingers and toes. Praying for a miracle. (Patient 1) I’m frightened. Terribly frightened. Chemo treatment is suffering is it? I heard patients died during chemo. I’m terrified of nausea, and not having hair. In my whole life, I haven’t been sick, suddenly diagnosed with cancer. I’m scared and lonely. (Patient 16) |
| Pain Management | I am on Xgeva, calcium and vitamin D3 but I still feel pains/aches every day. I already did radiotherapy. What else can I do? Tramadol and Codeine helps but when taken too long, it made drowsy and non-functional. (Patient 12) |
| Clinical Trials | Can anyone share how to get into clinical trial in private hospitals? Need to change treatment soon cause I can’t afford it. (Patient 5) |
| Immunotherapy | What is the latest development for breast cancer therapy in the aspect of immunotherapy? Those offered by outside clinics, need to be wary as it’s not proven and very expensive. (Patient 18) |
| Acupuncture | Anyone did acupuncture to manage pain or side effects of cancer? My private doctor is usually against alternative treatment like acupuncture. (Patient 10) |
| Social Security Assistance | Anyone here applied for SOCSO? My application got rejected again. Any way I can apply? Most of us have had careers and we have contributed towards the economy. (Patient 22) |
| Types of Treatment | Dr … (private oncologist) said I can take this oral chemo, but oncologist at … (government hospital) said this should be 3rd line treatment for me...don’t know what to do. (Patient 9) |
| Unmet Financial Needs | |
|---|---|
| High Cost of Treatment | More than one of us (I have thought of it) are thinking of stopping treatment because we don’t want to use our family budget just to keep the cancer fighter alive. The drugs for us are usually on the very high end of the expenditure bracket especially from private hospitals. (Patient 4) |
| Cost of Radiological Investigations | I’ll need to do a CT scan and was wondering if anyone knows any private hospitals offering affordable and quality services? For public hospital, there will be a long wait list, or need to see medical officer first, go another day etc. - too stressful to do all the running around. (Patient 14) |
| Medical Insurance Coverage | I got the shock of my life when I found out my medical insurance coverage for critical illness is limited to RM30K per annum regardless for cancer or admission for fever. I think this is discrimination. (Patient 11) |
| Availability of Generic & Biosimilar Drugs | I hope cheaper generic drugs are accessible in the future. We need it to prevent monopoly & reduce costs so more of us can afford them. Hopefully, the generics are as good as the original and safe to use. Let’s hope we have all the options available. (Patient 5) |
| Unmet Support Needs | |
|---|---|
| Healthcare Providers | Don’t waste time checking with public hospitals. They are reluctant to treat MBC. I was told to take morphine & prepare to sit in a wheelchair. I was so traumatised that I cried, she (oncologist) was so sarcastic saying she will refer me to counselor because I’m scared of dying. Gave up on them. (Patient 3) Climbing up and down the stairs is definitely a challenge. I strongly recommend physiotherapy. Don’t wait for your oncologist to do it. The request for a nutritionist’s advice and physiotherapist should come from you. With our disease, we really need to be brave and upfront to some extent. Be your own advocate! (Patient 8) |
| Patient’s Family And Social Circle | Just feeling down as my friends are traveling here & there while I have to skimp to pay for my treatment. My hubby not so supportive so my friends send me to hospital. Sometimes I feel so down, I am now taking Lexapro to help me feel happier. But I do feel grateful for my friends who also helped me, especially cancer survivors. (Patient 13) I truly understand the fear, the chaotic schedule and at the same time managing the kids and household, not forgetting the politics of managing family members......extremely exhausting (Patient 15) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kadravello, A.; Tan, S.-B.; Ho, G.-F.; Kaur, R.; Yip, C.-H. Exploring Unmet Needs from an Online Metastatic Breast Cancer Support Group: A Qualitative Study. Medicina 2021, 57, 693. https://doi.org/10.3390/medicina57070693
Kadravello A, Tan S-B, Ho G-F, Kaur R, Yip C-H. Exploring Unmet Needs from an Online Metastatic Breast Cancer Support Group: A Qualitative Study. Medicina. 2021; 57(7):693. https://doi.org/10.3390/medicina57070693
Chicago/Turabian StyleKadravello, Aravinthan, Seng-Beng Tan, Gwo-Fuang Ho, Ranjit Kaur, and Cheng-Har Yip. 2021. "Exploring Unmet Needs from an Online Metastatic Breast Cancer Support Group: A Qualitative Study" Medicina 57, no. 7: 693. https://doi.org/10.3390/medicina57070693
APA StyleKadravello, A., Tan, S.-B., Ho, G.-F., Kaur, R., & Yip, C.-H. (2021). Exploring Unmet Needs from an Online Metastatic Breast Cancer Support Group: A Qualitative Study. Medicina, 57(7), 693. https://doi.org/10.3390/medicina57070693





