A Systematic Review and Meta-Analysis of Ayurvedic Herbal Preparations for Hypercholesterolemia
Abstract
1. Introduction
1.1. Treatment Approaches
1.2. Ayurveda
1.3. Need for Study
2. Materials and Methods
2.1. Search Strategy
- The Cochrane Library, Cochrane Database of Systematic Reviews (CDSR), Cochrane Controlled Trials Register (CENTRAL), Database of Abstracts of Reviews of Effectiveness (DARE), Health Technology Assessment Database (HTA), MEDLINE, EMBASE, AMED (Allied and Complementary Medicine Database), World Health Organization (WHO) ICTRP (International Clinical Trials Registry Platform-http://apps.who.int/trialsearch/, accessed on 1 December 2020), ClinicalTrials.gov, EU Clinical Trials Register, and Europe PubMed Central. A MEDLINE (via Ovid platform) email alert service was continuously applied to identify newly published studies using the same search strategy as described for MEDLINE. If any additional relevant key words were detected during any of the electronic or other searches, the electronic search strategies were modified to incorporate these terms and document the changes.
- Clinical Trial Registry India, AYUSH research portal (Evidence Based Research Data of AYUSH Systems at Global Level, Department of AYUSH, Ministry of Health & Family Welfare, Government of India), Journal of Research in Ayurveda and Siddha, The Journal of Research & Education in Indian Medicine (JERIM), AYU (publication of Gujarat Ayurveda University, India), The International Journal for Ayurveda Research, Journal of Drug Research in Ayurveda, Journal of Ayurveda and Integrative Medicine, Ancient Science of Life, International Journal of Ayurveda and Pharma Research, A Bibliography of Indian Medicine (ABIM), Digital Helpline for Ayurveda Research Articles (DHARA), Indian Heart Journal.
- Other resources. Every effort was made to identify other potentially eligible trials or ancillary publications by searching the reference lists of retrieved included trials, systematic reviews, meta-analyses, and health technology assessment reports. In addition, study authors of included trials were contacted to identify any further studies that may have been missed.
- (a)
- Ayurvedic herbal preparations. These include extracts from mixtures of herbs, single herbs, Ayurvedic proprietary medicines, or a compound of herbs that are prescribed by an Ayurvedic practitioner. All the available interventions under this category, regardless of their mechanism of action, were included;
- (b)
- Ayurvedic herbal preparations in addition to standard care. Studies with Ayurvedic herbal medicines and conventional treatment for cholesterol (for example statins) as an intervention were also included as long as both the arms of the randomized trials received the conventional treatment.
2.1.1. Comparison Groups
- Placebo compared with (a) or (b);
- Usual care compared with (a) or (b);
- Non-pharmacological intervention (for example diet, exercise, or both);
- No intervention.
2.1.2. Outcomes
Primary Outcomes
- Total cholesterol levels;
- Adverse events;
- Major adverse cardiovascular events such as MI, stroke.
Secondary Outcomes
- Serum triglyceride levels;
- High-density lipoprotein (HDL) levels;
- Low-density lipoprotein (LDL) levels;
- Changes in body mass index (BMI) and body weight;
- Morbidity and or mortality;
- Health-related quality of life;
- Socioeconomic effects.
2.1.3. Assessment of Risk of Bias in Included Studies
- Random sequence generation (selection bias);
- Allocation concealment (selection bias);
- Blinding of participants and personnel (performance bias);
- Blinding of outcome assessment (detection bias);
- Incomplete outcome data (attrition bias).
2.1.4. Data Analyses
2.2. Subgroup Analysis and Investigation of Heterogeneity
- Age;
- Ethnicity;
- Geographical location;
- Diet pattern (Indian diet and Western diet, salt-restricted diet and salt-unrestricted diet, etc.)
2.3. Sensitivity Analysis
- Restricting the analysis to published studies;
- Restricting the analysis by considering risk of bias, as specified in Section 2.1.3 (Assessment of Risk of Bias in Included Studies);
- Restricting the analysis to very long or large studies to establish the extent to which they dominate the results;
- Restricting the analysis to studies using the following filters: diagnostic criteria, imputation, language of publication, source of funding (industry versus other), and country.
2.4. Including Non-Randomized Studies
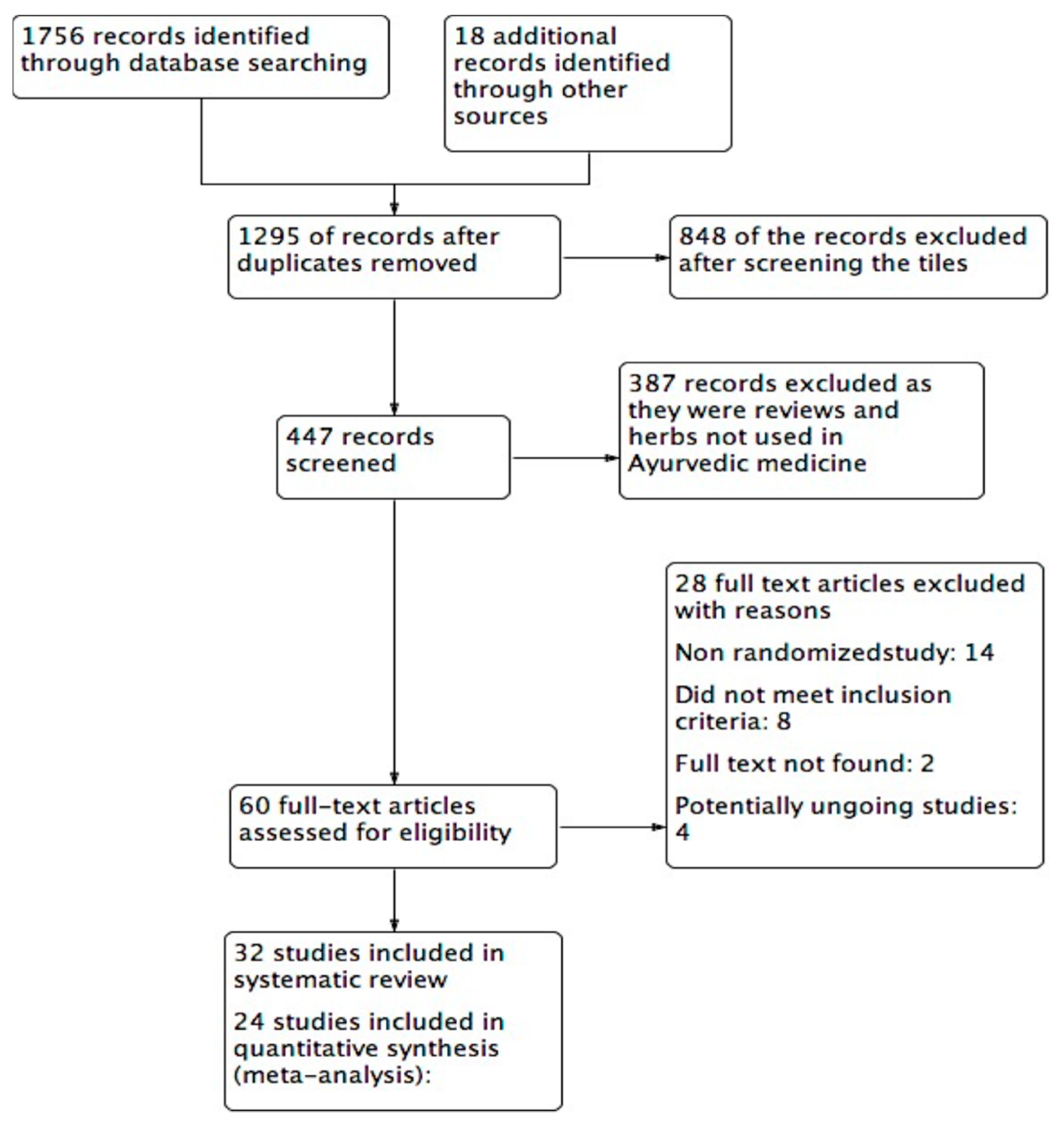
3. Results
3.1. Effects of Ayurvedic Herbs
3.1.1. Total Cholesterol (TC) (mg/dL)
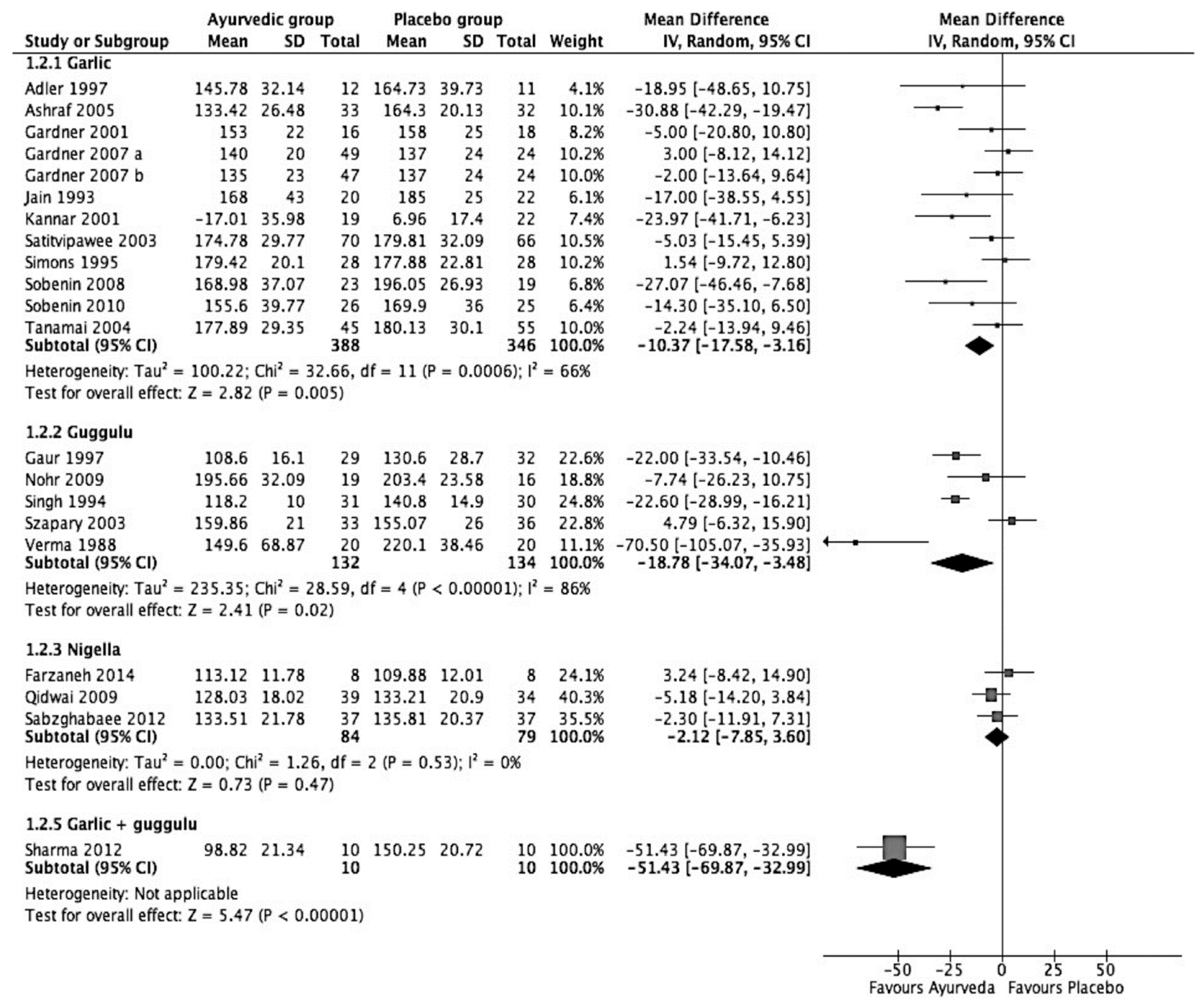
3.1.2. LDL Cholesterol (mg/dL)
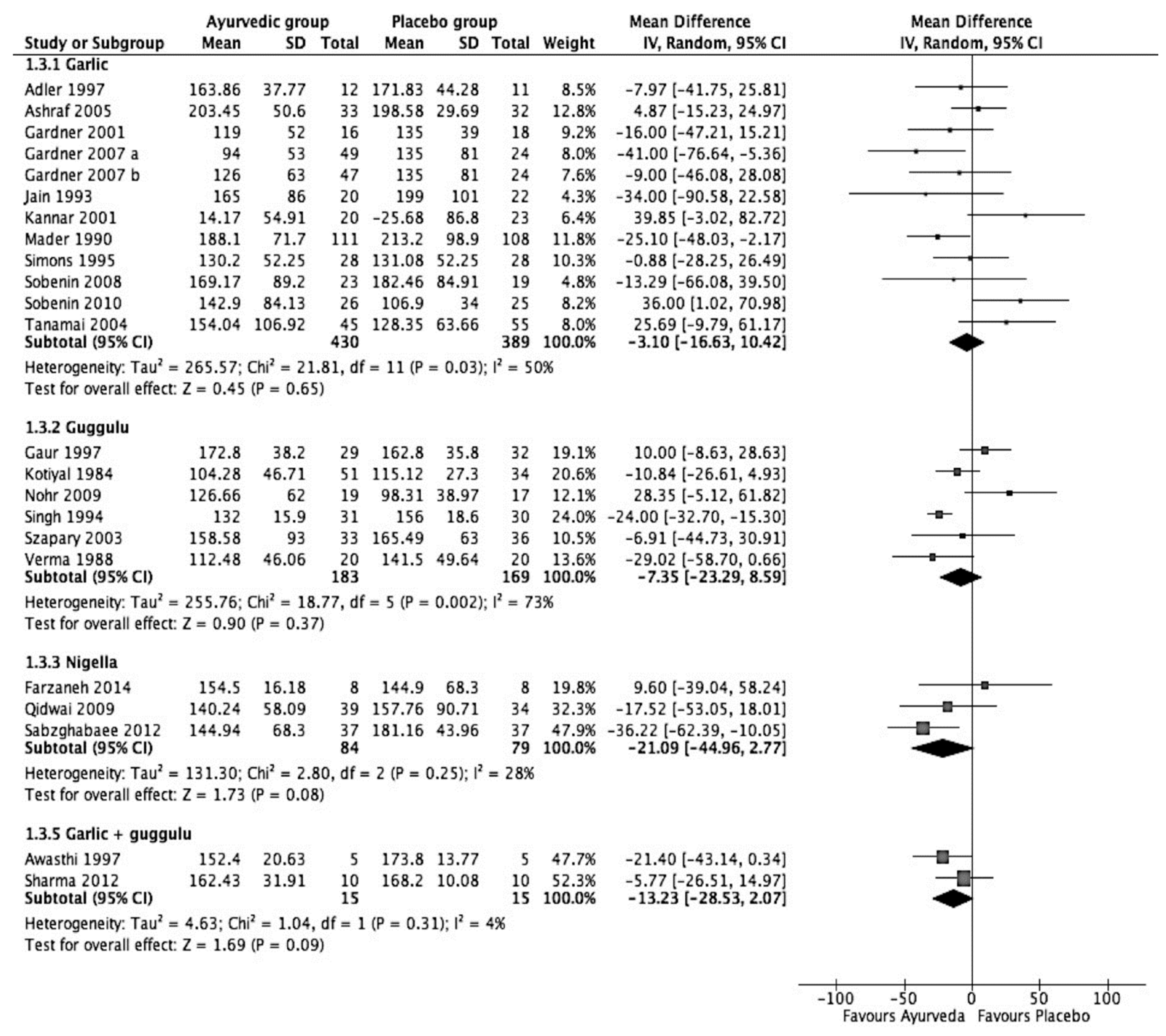
3.1.3. Triglycerides (mg/dL)
3.1.4. HDL (mg/dL)
4. Discussion
4.1. Commiphora Mukul (Guggulu)
4.1.1. Garlic
4.1.2. Nigella Sativa
4.1.3. Adverse Effects
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mendis, S.; Puska, P.; Norrving, B. Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol-United States, 1999–2002 and 2005–2008. MMWR 2011, 4, 109–114. [Google Scholar]
- Gupta, A.; Sehgal, V.; Mehan, S. Hyperlipidemia: An updated review. Int. J. Biopharm. Toxicol. Res. 2011, 1, 81–89. [Google Scholar]
- National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143. [Google Scholar] [CrossRef]
- The Lipid Research Clinics Coronary Primary Prevention Trial Results. JAMA 1984, 251, 351–364. [CrossRef] [PubMed]
- The Lipid Research Clinics Coronary Primary Prevention Trial Results. II. The Relationship of Reduction in Incidence of Coronary Heart Disease to Cholesterol Lowering. JAMA 1984, 251, 365–374. [CrossRef]
- Punekar, R.S.; Fox, K.M.; Richhariya, A.; Fisher, M.D.; Cziraky, M.; Gandra, S.R.; Toth, P.P. Burden of First and Recurrent Cardiovascular Events among Patients with Hyperlipidemia. Clin. Cardiol. 2015, 38, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Bahia, L.R.; Rosa, R.S.; Santos, R.D.; Araújo, D.V. Estimated costs of hospitalization due to coronary artery disease attributable to familial hypercholesterolemia in the Brazilian public health system. Arch. Endocrinol. Metab. 2018, 62, 303–308. [Google Scholar] [CrossRef]
- Soni, A. Top 10 Most Costly Conditions among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older, Med. Expend. Panel Surv. (2011) Statistical Brief #331). Available online: https://meps.ahrq.gov/data_files/publications/st331/stat331.shtml (accessed on 10 November 2020).
- Scirica, B.M.; Cannon, C.P. Treatment of Elevated Cholesterol. Circulation 2005, 111, 360–363. [Google Scholar] [CrossRef]
- Golomb, B.A.; Evans, M.A. Statin Adverse Effects. Am. J. Cardiovasc. Drugs 2008, 8, 373–418. [Google Scholar] [CrossRef]
- Chrysant, S.G. New onset diabetes mellitus induced by statins: Current evidence. Postgrad. Med. 2017, 129, 430–435. [Google Scholar] [CrossRef]
- Bove, M.; Cicero, A.F.; Borghi, C. Emerging drugs for the treatment of hypercholesterolemia. Expert Opin. Emerg. Drugs 2019, 24, 63–69. [Google Scholar] [CrossRef]
- Arnett, D.K.; Jacobs, D.R.; Luepker, R.V.; Blackburn, H.; Armstrong, C.; Claas, S.A. Twenty-Year Trends in Serum Cholesterol, Hypercholesterolemia, and Cholesterol Medication Use: The Minnesota Heart Survey. Circulation 2005, 112, 3884–3891. [Google Scholar] [CrossRef]
- Qidwai, W.; Jahan, F.; Nanji, K. Role of Complementary and Alternative Medicine in Controlling Dyslipidemia. Evid. Based Complement. Altern. Med. 2014, 2014, 1–2. [Google Scholar] [CrossRef]
- Singh, B.B.; Vinjamury, S.P.; Der-Martirosian, C.; Kubik, E.; Mishra, L.C.; Shepard, N.P.; Singh, V.J.; Meier, M.; Madhu, S.G. Ayurvedic and collateral herbal treatments for hyperlipidemia: A systematic review of randomized controlled trials and qua-si-experimental designs. Altern. Ther. Health Med. 2007, 13, 22–28. [Google Scholar]
- Patwardhan, B. Bridging Ayurveda with evidence-based scientific approaches in medicine. EPMA J. 2014, 5, 1–7. [Google Scholar] [CrossRef]
- Kessler, C.; Wischnewsky, M.; Michalsen, A.; Eisenmann, C.; Melzer, J. Ayurveda: Between Religion, Spirituality, and Medicine. Evid. Based Complement. Altern. Med. 2013, 2013, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Singhal, S.; Goyle, A.; Sharma, V.N. Antioxidant and hypocholesterolaemic effects of Terminalia arjuna tree-bark powder: A randomised placebo-controlled trial. J. Assoc. Physicians India 2001, 49, 231–235. [Google Scholar]
- Silagy, C.; Neil, A. Garlic as a Lipid Lowering Agent—A Meta-Analysis. J. R. Coll. Physicians Lond. 1994, 28, 39–45. [Google Scholar] [PubMed]
- Szapary, P.O.; Wolfe, M.L.; Bloedon, L.T.; Cucchiara, A.J.; DerMarderosian, A.H.; Cirigliano, M.D.; Rader, D.J. Guggulipid for the Treatment of Hypercholesterolemia. JAMA 2003, 290, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Qidwai, W.; Yeoh, P.N.; Inem, V.; Nanji, K.; Ashfaq, T. Role of Complementary and Alternative Medicine in Cardiovascular Diseases. Evid. Based Complement. Altern. Med. 2013, 2013, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, K. Promoting evidence-base for Ayurveda. J. Ayurveda Integr. Med. 2019. [Google Scholar] [CrossRef]
- Dwivedi, S. Terminalia arjuna Wight & Arn.—A useful drug for cardiovascular disorders. J. Ethnopharmacol. 2007, 114, 114–129. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Shafiq, N.; Negi, H.; Pandey, A.; Reddy, S.; Kaur, H.; Chadha, N.; Malhotra, S. Terminalia arjunain Chronic Stable Angina: Systematic Review and Meta-Analysis. Cardiol. Res. Pract. 2014, 2014, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ulbricht, C.; Basch, E.; Szapary, P.; Hammerness, P.; Axentsev, S.; Boon, H.; Kroll, D.; Garraway, L.; Vora, M.; Woods, J. Guggul for hyperlipidemia: A review by the Natural Standard Research Collaboration. Complement. Ther. Med. 2005, 13, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Ahmada, A.; Husainb, A.; Mujeebc, M.; Alam Khan, S.; Najmi, A.K.; Siddique, N.A.; Damanhouri, Z.A.; Anwarh, F. A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pac. J. Trop. Biomed. 2013, 3, 337–352. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Updated March 2011. The Cochrane Collaboration, 2001. Available online: www.cochrane-handbook.org (accessed on 1 December 2020).
- Gyawali, D.; Schneider, R.H.; Orme-Johnson, D.W.; Ramaratnam, S. Ayurvedic herbal preparations for hypercholesterolaemia. Cochrane Database Syst. Rev. 2016, 3. [Google Scholar] [CrossRef]
- Deeks, J.; Higgins, J. Statistical algorithms in Review Manager 5. Available online: https://training.cochrane.org/handbook/statistical-methods-revman5 (accessed on 20 May 2021).
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Sterne, J.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Wood, L.; Egger, M.; Gluud, L.L.; Schulz, K.F.; Jüni, P.; Altman, D.G.; Gluud, C.; Martin, R.M.; Wood, A.J.G.; Sterne, J.A.C. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: Meta-epidemiological study. BMJ 2008, 336, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G.; Spiegelhalter, D.J. A re-evaluation of random-effects meta-analysis. J. R. Stat. Soc. Ser. A 2009, 172, 137–159. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.D.; Higgins, J.P.T.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 342, d549. [Google Scholar] [CrossRef] [PubMed]
- Prakash, V.; Sehgal, V.; Bajaj, V.; Singh, H. To compare the effects of Terminalia Arjuna with Rosuvastatin on total cholesterol and low-density lipoprotein cholesterol. Int. J. Med. Dent. Sci. 2016, 5, 1056–1066. [Google Scholar] [CrossRef]
- Farzaneh, E.; Nia, F.R.; Mehrtash, M.; Mirmoeini, F.S.; Jalilvand, M. The effects of 8-week Nigella sativa supplementation and aerobic training on lipid profile and VO2 max in sedentary overweight females. Int. J. Prev. Med. 2014, 5, 210–216. [Google Scholar]
- Rathi, R.; Rathi, B.J. A clinical comparative study of rasonadi leha with hridrogadi churna in coronary artery disease. Punarnav 2013, 1, 44–54. [Google Scholar]
- Devra, D.K.; Mathur, K.C.; Agrawal, R.P.; Bhadu, I.; Goyal, S.; Agarwal, V. Effect of Tulsi (Ocimum sanctum Linn.) on clinical and biochemical parameters of metabolic syndrome. J. Nat. Remed. 2012, 12, 63–67. [Google Scholar]
- Huseini, H.F.; Kianbakht, S.; Hajiaghaee, R.; Dabaghian, F.H. Anti-hyperglycemic and anti-hypercholesterolemic effects of Aloe vera leaf gel in hyperlipidemic type 2 diabetic patients: A randomized double-blind placebo-controlled clinical trial. Planta Med. 2012, 78, 311–316. [Google Scholar] [CrossRef]
- Joseph, S.; Santhosh, D.; Udupa, A.L.; Gupta, S.; Ojeh, N.; Rathnakar, U.P.; Benegal, D.; Benegal, A.; Shubha, H.V.; Rao, S.P.; et al. Hypolipidemic Activity of Phyllanthus Emblica Linn (Amla) & Trigonella Foenum Graecum (Fenugreek) Combination In Hypercholesterolemic Subjects–A Prospective, Randomised, Parallel, Open-Label, Positive Controlled Study. Asian J. Bio. Pharma. Res. 2012, 2, 225–230. [Google Scholar]
- Sabzghabaee, A.M.; Dianatkhah, M.; Sarrafzadegan, N.; Asgary, S.; Ghannadi, A. Clinical evaluation of Nigella sativa seeds for the treatment of hyperlipidemia: A randomized, placebo controlled clinical trial. Med. Arch. 2012, 66, 198–200. [Google Scholar] [CrossRef]
- Sharma, A.K.; Sharma, S.M.; Sharma, S.P.; Sharma, A.K. Management of stable angina with lashunadi guggulu- an ayurvedic formulation. Ann. Ayurvedic. Med. 2012, 1, 15–21. [Google Scholar]
- Sobenin, I.A.; Pryanishnikov, V.V.; Kunnova, L.M.; Rabinovich, Y.A.; Martirosyan, D.M.; Orekhov, A.N. The effects of time-released garlic powder tablets on multifunctional cardiovascular risk in patients with coronary artery disease. Lipids Health Dis. 2010, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nohr, L.A.; Rasmussen, L.B.; Straand, J. Resin from the mukul myrrh tree, guggul, can it be used for treating hypercholesterolemia? A randomized, controlled study. Complement. Ther. Med. 2009, 17, 16–22. [Google Scholar] [CrossRef]
- Qidwai, W.; Bin Hamza, H.; Qureshi, R.; Gilani, A. Effectiveness, safety, and tolerability of powdered nigella sativa (kalonji) seed in capsules on serum lipid levels, blood sugar, blood pressure, and body weight in adults: Results of a randomized, double-blind controlled trial. J. Altern. Complement. Med. 2009, 15, 639–644. [Google Scholar] [CrossRef]
- Alizadeh-Navaei, R.; Roozbeh, F.; Saravi, M.; Pouramir, M.; Jalali, F.; Moghadamnia, A.A. Investigation of the effect of ginger on the lipid levels. A double blind controlled clinical trial. Saudi Med. J. 2008, 29, 1280–1284. [Google Scholar]
- Sobenin, I.A.; Andrianova, I.V.; Demidova, O.N.; Gorchakova, T.; Orekhov, A.N. Lipid-lowering effects of time-released garlic powder tablets in double-blinded placebo-controlled randomized study. J. Ather. Thromb. 2008, 15, 334–338. [Google Scholar] [CrossRef]
- Gardner, C.D.; Lawson, L.D.; Block, E.; Chatterjee, L.M.; Kiazand, A.; Balise, R.R.; Kraemer, H.C. Effect of raw garlic vs commercial garlic supplements on plasma lipid concentrations in adults with moderate hypercholesterolemia. Arch. Intern. Med. 2007, 167, 346–353. [Google Scholar] [CrossRef]
- Ashraf, R.; Aamir, K.; Shaikh, A.R.; Ahmed, T. Effects of garlic on dyslipidemia in patients with type 2 diabetes mellitus. J. Ayub. Med. Coll. Abbottabad. 2005, 17, 60–64. [Google Scholar]
- Tanamai, J.; Veeramanomai, S.; Indrakosas, N. The efficacy of cholesterol-lowering action and side effects of garlic enteric coated tablets in man. J. Med. Ass. Thailand 2004, 87, 1156–1161. [Google Scholar]
- Satitvipawee, P.; Suparp, J.; Podhipak, A.; Viwatwongkasem, C. Can garlic extract supplement lower blood pressure in hypercholesterolemic subjects? J. Public Health 2003, 33, 18–26. [Google Scholar]
- Double-Blind Comparative Clinical Trial of Abana and Simvastatin in Hyperlipidaemia. Available online: https://cdn.greensoft.mn/uploads/users/1977/files/tsakhurtumur%20sudalga/Abana%20sudalgaa.pdf (accessed on 28 May 2021).
- Kannar, D.; Wattanapenpaiboon, N.; Savige, G.S.; Wahlqvist, M.L. Hypocholesterolemic effect of an enteric-coated garlic supplement. J. Am. Coll. Nutr. 2001, 20, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Gardner, C.D.; Chatterjee, L.M.; Carlson, J.J. The effect of a garlic preparation on plasma lipid levels in moderately hypercholesterolemic adults. Atherosclerosis 2001, 154, 213–220. [Google Scholar] [CrossRef]
- Adler, A.J.; Holub, B.J. Effect of garlic and fish-oil supplementation on serum lipid and lipoprotein concentrations in hypercholesterolemic men. Am. J. Clin. Nutr. 1997, 65, 445–450. [Google Scholar] [CrossRef]
- Awasthi, A.; Kothari, K.; Sharma, R. Evaluation of the effect of the indigenous herbal drug lashunadi guggulu in management of chronic stable Angina. Aryavaidyan Xi 1997, 1, 20. [Google Scholar]
- Gaur, S.P.; Garg, R.K.; Kar, A.M. Gugulipid, a new hypolipidaemic agent, in patients of acute ischaemic stroke: Effect on clinical outcome, platelet function and serum lipids. Asia Pacif. J. Pharm. 1997, 12, 65–69. [Google Scholar]
- Singh, R.B.; Niaz, M.A.; Ghosh, S. Hypolipidemic and antioxidant effects of Commiphora mukul as an adjunct to dietary therapy in patients with hypercholesterolemia. Cardiovasc. Drugs. Ther. 1994, 8, 659–664. [Google Scholar] [CrossRef]
- Jain, A.K.; Vargas, R.; Gotzkowsky, S.; McMahon, F.G. Can garlic reduce levels of serum lipids? A controlled clinical study. Am. J. Med. 1993, 94, 632–635. [Google Scholar] [CrossRef]
- Tiwari, A.K.; Agrawal, A.; Gode, J.D.; Dubey, G.P. Perspective, randomised crossover study of propranolol and Abana in hypertensive patients: Effect on lipids and lipoproteins. Antiseptic. 1991, 88, 14. [Google Scholar]
- Mader, F.H. Treatment of hyperlipidaemia with garlic-powder tablets. Evidence from the German Association of General Practitioners’ multicentric placebo-controlled double-blind study. Arzneimittel-Forschung 1990, 40, 1111–1116. [Google Scholar]
- Nityanand, S.; Srivastava, J.S.; Asthana, O.P. Clinical trials with gugulipid. A new hypolipidaemic agent. J. Assoc. Physicians Ind. 1989, 37, 323–328. [Google Scholar]
- Verma, S.K.; Bordia, A. Effect of Commiphora mukul (gum guggulu) in patients of hyperlipidemia with special reference to HDL-cholesterol. Indian J. Med. Res. 1988, 87, 356–360. [Google Scholar]
- Kotiyal, J.P.; Singh, D.S.; Bisht, D.B. Gum guggulu (Commiphora mukul) fraction A in obesity—A double-blind clinical trial. J. Res. Ayur. Siddha. 1985, 6, 20–35. [Google Scholar]
- Kuppurajan, K.; Rajagopalan, S.S.; Rao, T.K.; Sitaraman, R. Effect of guggul (Commiphora mukul–Engl.) on serum lipids in obese, hypercholesterolemic and hyperlipemic cases. J. Assoc. Physicians India. 1978, 26, 367–373. [Google Scholar] [PubMed]
- Law, M.R.; Wald, N.J.; Thompson, S.G. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ 1994, 308, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Delahoy, P.J.; Magliano, D.J.; Webb, K.; Grobler, M.; Liew, D. The relationship between reduction in low-density lipoprotein cholesterol by statins and reduction in risk of cardiovascular outcomes: An updated meta-analysis. Clin. Ther. 2009, 31, 236–244. [Google Scholar] [CrossRef]
- Chunekar, K.C. Bhavprakash Nighantu of Bhavmisra; Chaukambha Orientalia: Varanasi, India, 2009. [Google Scholar]
- Urizar, N.L.; Moore, D.D. GUGULIPID: A Natural Cholesterol-Lowering Agent. Annu. Rev. Nutr. 2003, 23, 303–313. [Google Scholar] [CrossRef]
- Golomb, B.A. Misinterpretation of trial evidence on statin adverse effects may harm patients. Eur. J. Prev. Cardiol. 2015, 22, 492–493. [Google Scholar] [CrossRef]
- Ried, K.; Toben, C.; Fakler, P. Effect of garlic on serum lipids: An updated meta-analysis. Nutr. Rev. 2013, 71, 282–299. [Google Scholar] [CrossRef]
- Reinhart, K.M.; Talati, R.; White, C.M.; Coleman, C.I. The impact of garlic on lipid parameters: A systematic review and meta-analysis. Nutr. Res. Rev. 2009, 22, 39–48. [Google Scholar] [CrossRef]
- Stevinson, C.; Pittler, M.; Ernst, E. Garlic for treating hypercholesterolemia. ACC Curr. J. Rev. 2001, 10, 37. [Google Scholar] [CrossRef]
- Amagase, H.; Petesch, B.L.; Matsuura, H.; Kasuga, S.; Itakura, Y. Intake of garlic and its bioactive components. J. Nutr. 2001, 131, 955S–962S. [Google Scholar] [CrossRef]
- Shastri, K. Sushruta Samhita of Maharshi Sushruta Part I, 14th ed.; Chaukhamba Sanskrita Sansthana: Varanasi, India, 2001. [Google Scholar]
- Wang, H.-P.; Yang, J.; Qin, L.-Q.; Yang, X.-J. Effect of Garlic on Blood Pressure: A Meta-Analysis. J. Clin. Hypertens. 2015, 17, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Beccuti, G.; Simental-Mendía, L.E.; Nobili, V.; Bo, S. Nigella sativa (black seed) effects on plasma lipid concentrations in humans: A systematic review and meta-analysis of randomized placebo-controlled trials. Pharmacol. Res. 2016, 106, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Zeb, F.; Safdar, M.; Fatima, S.; Khan, S.; Alam, S.; Muhammad, M.; Syed, A.; Habib, F.; Shakoor, H. Supplementation of garlic and coriander seed powder: Impact on body mass index, lipid profile and blood pressure of hyperlipidemic patients. Pak. J. Pharm. Sci. 2018, 31, 1935–1941. [Google Scholar] [PubMed]
- Iskandar, I.; Harahap, Y.; Wijayanti, T.R.; Sandra, M.; Prasaja, B.; Cahyaningsih, P.; Rahayu, T. Efficacy and tolerability of a nutraceutical combination of red yeast rice, guggulipid, and chromium picolinate evaluated in a randomized, placebo-controlled, double-blind study. Complement. Ther. Med. 2020, 48, 102282. [Google Scholar] [CrossRef] [PubMed]
- Kuchewar, V.V. Efficacy and safety study of triphala in patients of dyslipidemia: A pilot project. Int. J. Res. Ayurveda Pharm. 2017, 8, 177–180. [Google Scholar] [CrossRef]
- Bhatt, J.; Hemavathi, K.G.; Gopa, B. A comparative clinical study of hypolipidemic efficacy of Amla (Emblica officinalis) with 3-hydroxy-3-methylglutaryl-coenzyme-A reductase inhibitor simvastatin. Indian J. Pharmacol. 2012, 44, 238–242. [Google Scholar] [CrossRef]
- Upadya, H.; Prabhu, S.; Prasad, A.; Subramanian, D.; Gupta, S.; Goel, A. A randomized, double blind, placebo controlled, multicenter clinical trial to assess the efficacy and safety of Emblica officinalis extract in patients with dyslipidemia. BMC Complement. Altern. Med. 2019, 19, 27. [Google Scholar] [CrossRef]


| Study ID | Intervention & Comparator | Duration of Intervention | Description of Participants | Trial Period | Country, Place | Setting | Ethnic Groups (%) |
|---|---|---|---|---|---|---|---|
| Prakash 2016 [38] | I: T. arjuna | 12 weeks | Age < 20 years, total cholesterol ≥ 200 mg/dL, LDL-C ≥ 130 mg/dL | - | India | Outpatient clinic of university hospital | - |
| C: Rosuvastatin | - | ||||||
| Farzaneh 2014 [39] | I: N. sativa | 8 weeks | Adult overweight females with sedentary lifestyle and total cholesterol > 200 mg/dL | - | Iran | University clinic | - |
| C: Placebo | - | ||||||
| Rathi 2013 [40] | I: Rasonadi leha + Hridroghar churna + Usual care | 3 months | Patients of post MI attending private hospital of Betul, Madhya Pradesh, India | - | India | Hospital | - |
| C: Usual care | - | ||||||
| Devra 2012 [41] | I: Tulsi extract | 3 months | Patients of metabolic syndrome | - | India | Hospital | |
| C: Placebo | |||||||
| Huseini 2012 [42] | I: Aloe | 2 months | Patients with type 2 diabetes and hyperlipidemia | - | Iran | Outpatient clinic | - |
| C: Placebo | - | ||||||
| Joseph 2012 [43] | I: Amla + Fenugreek | 12 weeks | Patients of hypercholesterolemia with total cholesterol > 220 mg/dL | - | - | Outpatient department of tertiary teaching hospital | - |
| C: Atorvastatin | - | ||||||
| Sabzghabaee 2012 [44] | I. N. sativa | 4 weeks | Patients with toral cholesterol > 200 mg/dL | July 2010–June 2011 | Iran | Outpatient clinics of University hospital | - |
| C: Placebp | - | ||||||
| Sharma 2012 [45] | I: Lashunadi guggulu | 45 days | Clinically diagnosed and confirmed patients of stable angina from out and in-patient departments of two hospitals of Jaipur, India | 2002–2004 | India | University hospital | - |
| C: Placebo | - | ||||||
| Sobenin 2010 [46] | I: Allicor | 12 months | Patients with documented CHD, 40–65 years age and s. cholesterol level > 200 mg/dL | - | Russia | Probably research center | - |
| C: Placebo | - | ||||||
| Nohr 2009 [47] | I: Guggulu formula | 12 (weeks) | Patients from Norwegian general practice who are not taking any prescriptions for hypercholesterolemia, CHD, DM | Feb–May 2003 | Oppland and Hedemark counties of Norway | General practice | Native Norwegians |
| C: Placebo | Native Norwegians | ||||||
| Qidwai 2009 [48] | I: N. sativa | 6 weeks | Patients with total cholesterol level > 180 to 250 mg/dL | Feb 2006–Jan 2007 | Pakistan | Outpatient clinics at university hospital | Pakistani |
| C: Placebo | Pakistani | ||||||
| Alizadeh-Navaei 2008 [49] | I: Ginger | 45 days | Patients of hyperlipidemia with cholesterol > 200 mg/dL or Triglyceride > 200 mg/dL | April 2004–May 2005 | Babol, Iran | Cardiac clinic | - |
| C: Placebo | - | ||||||
| Sobenin 2008 [50] | I: Allicor | 12 weeks | Men with mild hypercholesterolemia | - | Moscow, Russia | Research center | - |
| C: Placebo | - | ||||||
| Gardner 2007 a [51] | I: Raw Garlic | 6 months | Adults with LDL-C 130–190 mg/dL | Nov 2002–June 2005 | USA | University hospital clinic | White (73) Black (4) Asian (18) Hispanic (2) |
| C: Placebo | White (64) Asian (14) Hispanic (4) | ||||||
| Gardner 2007 b [51] | I: Garlic in tablets | 6 months | Adults with LDL-C 130–190 mg/dL | Nov 2002–June 2005 | USA | University hospital clinic | White (66) Black (4) Asian (21) Hispanic (6) |
| C: Placebo | White (64) Asian (14) Hispanic (4) | ||||||
| Ashraf 2005 [52] | I: Garlic | 12 weeks | Type 2 diabetes mellitus patients with newly diagnosed hyperlipidaemia | - | Karachi, Pakistan | University hospital | - |
| C: Placebo | - | ||||||
| Tanamai 2004 [53] | I: Garlic | 9 months | Hypercholesterolemia | - | Bangkok, Thailand | Hospital | Thai |
| C: Placebo | Thai | ||||||
| Satitvipawee 2003 [54] | I: Garlic | 12 weeks | Hypercholesterolemia | - | Thailand | Study center | - |
| C: Placebo | - | ||||||
| Szapary 2003 [21] | I: Guggulipid | 8 (weeks) | Ambulatory, community-dwelling, healthy adults with hypercholesterolaemia | March 2000–August 2001 | Philadelphia, Pa, metropolitan area | University hospital | White (85) |
| C: Placebo | White (75) | ||||||
| Venkataramaiah 2002 [55] | I: Abana | 8 weeks | Patients with total cholesterol > 200 mg/dL or triglycerides > 200 mg/dL | - | - | - | - |
| C: Simvastatin | - | ||||||
| Kannar 2001 [56] | I: Garlic | 12 weeks | Volunteers who failed to comply with previous lipid-lowering therapies | - | Victoria, Australia | University clinic | - |
| C: Placebo | - | ||||||
| Gardner 2001 [57] | I: Garlic | 12 weeks | General public and employees of Stanford University | June–October, 1997 | Stanford University, Palo Alto, CA | University hospital | - |
| C: Placebo | - | ||||||
| - | |||||||
| Adler 1997 [58] | I: Garlic | 12 weeks | Men with elevated T. cholesterol level > 5.2 mmol/L (200 mg/dL) | - | Guelph, Ontario, Canada | University hospital/clinic | - |
| C: Placebo | - | ||||||
| Awasthi 1997 [59] | I: Lashunadi guggulu | 2 months | Patients of chronic stbale angina from two hospitals in Jaipur | - | Jaipur, India | University hospital | - |
| C: Placebo | - | ||||||
| Gaur 1997 [60] | I: Gugulipid and usual care | 4/4 (weeks) | Patients of ischaemic stroke | - | India | - | - |
| C: Usual care | - | ||||||
| Singh 1994 [61] | I: Gugguluipid | 24 weeks | Patients with hypercholesterolaemia with s. cholesterol level > 200 mg/dL | - | India | - | White (70) Black (30) |
| C: Placebo | White (68) Black (32) | ||||||
| Jain 1993 [62] | I: Garlic | 12 weeks | Patients with s. total cholesterol level > 220 mg/dL | - | USA | Outptient clinic | - |
| C: Placebo | - | ||||||
| Tiwari 1991 [63] | I: Abana | 6 months | Diagnosed cases of hypertension and Angina pectoris | - | India | University hospital | - |
| C: Propanlol | - | ||||||
| Mader 1990 [64] | I: Garlic | 4 months | Patients of hyperlipidaemia from 30 different practices in Germany | - | Germany | General practice | - |
| C: Placebo | |||||||
| Nityanand 1989 [65] | I: Gugguluipid | 12 weeks | Patients with s. cholesterol levels > 220 mg/dL | - | India | - | |
| C: Clofibrate | - | ||||||
| Verma 1988 [66] | I: Guggulu | 16 weeks | Patients of hyperlipidaemia between age 40–60 years Type IIa or IIb of Frederichsons classification of hyperlipidemia | - | India | University hospital | - |
| C: Placebo | - | ||||||
| Kotiyal 1984 [67] | I: Guggulu | 12 weeks | Patients with features of obesity, 10% overweight for one’s height, age, and sex | - | India | Medical OPD of a hospital | - |
| C: Placebo | - | ||||||
| Kuppurajan 1978 [68] | I: Guggulu | 3 weeks | Patients with s. cholesterol > 300 mg/dL or total lipids > 750 mg/dL | - | India | - | - |
| C: Placebo | - |
| Study ID | Random Sequence Generation | Allocation Concealment | Blinding | Attrition Bias | Selective Outcome Reporting |
|---|---|---|---|---|---|
| Prakash 2016 | U | U | U | U | L |
| Farzaneh 2014 | U | U | L | H | L |
| Rathi 2013 | U | U | U | H | L |
| Devra 2012 | U | U | U | U | L |
| Huseini 2012 | L | L | L | L | L |
| Joseph 2012 | U | U | U | U | L |
| Sabzghabaee 2012 | U | L | U | U | L |
| Sharma 2012 | U | U | L | H | L |
| Sobenin 2010 | U | U | L | H | L |
| Nohr 2009 | L | L | L | H | L |
| Qidwai 2009 | U | U | L | H | L |
| Alizadeh-Navaei 2008 | U | U | L | U | L |
| Sobenin 2008 | U | U | L | U | L |
| Gardner 2007 | L | L | L | L | L |
| Ashraf 2005 | U | U | H | L | L |
| Tanamai 2004 | U | U | L | H | L |
| Satitvipawee 2003 | L | L | L | L | L |
| Szapary 2003 | L | L | L | L | L |
| Venkataramaiah 2002 | U | U | U | U | U |
| Kannar 2001 | U | U | L | L | L |
| Gardner 2001 | U | U | L | L | L |
| Adler 1997 | U | U | L | L | L |
| Awasthi 1997 | U | U | L | H | L |
| Gaur 1997 | U | U | U | H | L |
| Singh 1994 | U | U | L | H | L |
| Jain 1993 | U | U | H | L | L |
| Tiwari 1991 | U | U | L | H | L |
| Mader 1990 | L | L | L | L | L |
| Nityanand 1989 | U | U | L | H | L |
| Verma 1988 | U | U | L | U | L |
| Kotiyal 1984 | U | U | L | U | L |
| Kuppurajan 1978 | U | U | L | H | L |
| Outcome or Subgroup | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| 1.1 Total Cholesterol level | 24 | 1386 | Mean Difference (IV, Random, 95% CI) | |
| 1.1.1 Garlic | 11 | 813 | Mean Difference (IV, Random, 95% CI) | −12.45 (−18.68, −6.22) |
| 1.1.2 Guggulu | 8 | 380 | Mean Difference (IV, Random, 95% CI) | −16.78 (−30.96, −2.61) |
| 1.1.3 Nigella | 3 | 163 | Mean Difference (IV, Random, 95% CI) | −9.28 (−17.36, −1.19) |
| 1.1.5 Garlic + guggulu | 2 | 30 | Mean Difference (IV, Random, 95% CI) | −38.28 (−55.11, −21.44) |
| Outcome or Subgroup | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| 1.2 LDL-Cholesterol level | 21 | 1183 | Mean Difference (IV, Random, 95% CI) | |
| 1.2.1 Garlic | 12 | 734 | Mean Difference (IV, Random, 95% CI) | −10.37 (−17.58, −3.16) |
| 1.2.2 Guggulu | 5 | 266 | Mean Difference (IV, Random, 95% CI) | −18.78 (−34.07, −3.48) |
| 1.2.3 Nigella | 3 | 163 | Mean Difference (IV, Random, 95% CI) | −2.12 (−7.85, 3.60) |
| 1.2.5 Garlic + guggulu | 1 | 20 | Mean Difference (IV, Random, 95% CI) | −51.43 (−69.87, −32.99) |
| Outcome or Subgroup | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| 1.3 Triglycerides level | 23 | 1364 | Mean Difference (IV, Random, 95% CI) | |
| 1.3.1 Garlic | 12 | 819 | Mean Difference (IV, Random, 95% CI) | −3.10 (−16.63, 10.42) |
| 1.3.2 Guggulu | 6 | 352 | Mean Difference (IV, Random, 95% CI) | −7.35 (−23.29, 8.59) |
| 1.3.3 Nigella | 3 | 163 | Mean Difference (IV, Random, 95% CI) | −21.09 (−44.96, 2.77) |
| 1.3.5 Garlic + guggulu | 2 | 30 | Mean Difference (IV, Random, 95% CI) | −13.23 (−28.53, 2.07) |
| Outcome or Subgroup | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| 1.4 HDL-Cholesterol level | 21 | 1186 | Mean Difference (IV, Random, 95% CI) | |
| 1.4.1 Garlic | 12 | 736 | Mean Difference (IV, Random, 95% CI) | −2.91 (−9.19, 3.37) |
| 1.4.2 Guggulu | 5 | 267 | Mean Difference (IV, Random, 95% CI) | 2.19 (0.27, 4.12) |
| 1.4.3 Nigella | 3 | 163 | Mean Difference (IV, Random, 95% CI) | 1.92 (−1.62, 5.45) |
| 1.4.5 Garlic + guggulu | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 10.00 (5.87, 14.13) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyawali, D.; Vohra, R.; Orme-Johnson, D.; Ramaratnam, S.; Schneider, R.H. A Systematic Review and Meta-Analysis of Ayurvedic Herbal Preparations for Hypercholesterolemia. Medicina 2021, 57, 546. https://doi.org/10.3390/medicina57060546
Gyawali D, Vohra R, Orme-Johnson D, Ramaratnam S, Schneider RH. A Systematic Review and Meta-Analysis of Ayurvedic Herbal Preparations for Hypercholesterolemia. Medicina. 2021; 57(6):546. https://doi.org/10.3390/medicina57060546
Chicago/Turabian StyleGyawali, Dinesh, Rini Vohra, David Orme-Johnson, Sridharan Ramaratnam, and Robert H. Schneider. 2021. "A Systematic Review and Meta-Analysis of Ayurvedic Herbal Preparations for Hypercholesterolemia" Medicina 57, no. 6: 546. https://doi.org/10.3390/medicina57060546
APA StyleGyawali, D., Vohra, R., Orme-Johnson, D., Ramaratnam, S., & Schneider, R. H. (2021). A Systematic Review and Meta-Analysis of Ayurvedic Herbal Preparations for Hypercholesterolemia. Medicina, 57(6), 546. https://doi.org/10.3390/medicina57060546






