Association between Lower Urinary Tract Symptoms and Sleep Quality of Patients with Depression
Abstract
1. Introduction
2. Materials and Methods
2.1. Instruments
2.2. Statistics
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Instruments
3.3. Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the International Continence Society. Neurourol. Urodyn. 2002, 21, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Irwin, D.E.; Milsom, I.; Hunskaar, S.; Reilly, K.; Kopp, Z.; Herschorn, S.; Coyne, K.; Kelleher, C.; Hampel, C.; Artibani, W.; et al. Population-Based Survey of Urinary Incontinence, Overactive Bladder, and Other Lower Urinary Tract Symptoms in Five Countries: Results of the EPIC Study. Eur. Urol. 2006, 50, 1306–1315. [Google Scholar] [CrossRef] [PubMed]
- Coyne, K.S.; Wein, A.J.; Tubaro, A.; Sexton, C.C.; Thompson, C.L.; Kopp, Z.S.; Aiyer, L.P. The burden of lower urinary tract symptoms: Evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009, 103, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Fantus, R.J.; Packiam, V.T.; Wang, C.H.; Erickson, B.A.; Helfand, B.T. The Relationship between Sleep Disorders and Lower Urinary Tract Symptoms: Results from the NHANES. J. Urol. 2018, 200, 161–166. [Google Scholar] [CrossRef]
- Branche, B.L.; Howard, L.E.; Moreira, D.M.; Roehrborn, C.; Castro-Santamaria, R.; Andriole, G.L.; Hopp, M.L.; Freedland, S.J. Sleep Problems are Associated with Development and Progression of Lower Urinary Tract Symptoms: Results from REDUCE. J. Urol. 2018, 199, 536–542. [Google Scholar] [CrossRef]
- Martin, S.A.; Appleton, S.L.; Adams, R.J.; Taylor, A.W.; Catcheside, P.G.; Vakulin, A.; McEvoy, R.D.; Antic, N.A.; Wittert, G.A. Nocturia, Other Lower Urinary Tract Symptoms and Sleep Dysfunction in a Community-Dwelling Cohort of Men. Urology 2016, 97, 219–226. [Google Scholar] [CrossRef]
- Helfand, B.T.; McVary, K.T.; Meleth, S.; Sharp, V.; Foster, H.; Naslund, M.; Williams, O.D. CAMUS Study Group The Relationship Between Lower Urinary Tract Symptom Severity and Sleep Disturbance in the CAMUS Trial. J. Urol. 2011, 185, 2223–2228. [Google Scholar] [CrossRef]
- Przydacz, M.; Skalski, M.; Golabek, T.; Sobański, J.A.; Klasa, K.; Świerkosz, A.; Dudek, D.; Chłosta, P. Nocturia has no impact on depression severity in patients suffering from depression but correlates with sleep quality. Psychiatr. Polska 2018, 52, 835–842. [Google Scholar] [CrossRef]
- Cakir, O.O.; McVary, K.T. LUTS and Sleep Disorders: Emerging Risk Factor. Curr. Urol. Rep. 2012, 13, 407–412. [Google Scholar] [CrossRef]
- Skalski, M.; Przydacz, M.; Sobański, J.; Cyranka, K.; Klasa, K.; Datka, W.; Gołąbek, T.; Chłosta, P.; Dudek, D. Coexistence of lower urinary tract symptoms (LUTS) with depressive symptoms in patients suffering from depressive disorders. Psychiatr. Polska 2019, 53, 939–953. [Google Scholar] [CrossRef]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The Association of Sleep and Pain: An Update and a Path Forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef]
- Sochal, M.; Małecka-Panas, E.; Gabryelska, A.; Talar-Wojnarowska, R.; Szmyd, B.; Krzywdzińska, M.; Białasiewicz, P. Determinants of Sleep Quality in Inflammatory Bowel Diseases. J. Clin. Med. 2020, 9, 2921. [Google Scholar] [CrossRef]
- Cremonini, F.; Camilleri, M.; Zinsmeister, A.R.; Herrick, L.M.; Beebe, T.; Talley, N.J. Sleep disturbances are linked to both upper and lower gastrointestinal symptoms in the general population. Neurogastroenterol. Motil. 2009, 21, 128–135. [Google Scholar] [CrossRef]
- Scovell, J.M.; Pastuszak, A.W.; Slawin, J.; Badal, J.; Link, R.E.; Lipshultz, L.I. Impaired Sleep Quality is Associated With More Significant Lower Urinary Tract Symptoms in Male Shift Workers. Urology 2017, 99, 197–202. [Google Scholar] [CrossRef]
- Siddiqui, N.Y.; Wiseman, J.B.; Cella, D.; Bradley, C.S.; Lai, H.H.; Helmuth, M.E.; Smith, A.R.; Griffith, J.W.; Amundsen, C.L.; Kenton, K.S.; et al. Mental Health, Sleep and Physical Function in Treatment Seeking Women with Urinary Incontinence. J. Urol. 2018, 200, 848–855. [Google Scholar] [CrossRef]
- Zimmerman, M.; Martinez, J.H.; Young, D.; Chelminski, I.; Dalrymple, K. Severity classification on the Hamilton depression rating scale. J. Affect. Disord. 2013, 150, 384–388. [Google Scholar] [CrossRef]
- Kerkhof, G.A.; Geuke, M.E.H.; Brouwer, A.; Rijsman, R.M.; Schimsheimer, R.J.; Van Kasteel, V. Holland Sleep Disorders Questionnaire: A new sleep disorders questionnaire based on the International Classification of Sleep Disorders-2. J. Sleep Res. 2013, 22, 104–107. [Google Scholar] [CrossRef]
- Rom, M.; Schatzl, G.; Swietek, N.; Rücklinger, E.; Kratzik, C. Lower urinary tract symptoms and depression. BJU Int. 2012, 110, E918–E921. [Google Scholar] [CrossRef]
- Kupelian, V.; Rosen, R.C.; Link, C.L.; McVary, K.T.; Aiyer, L.P.; Mollon, P.; Kaplan, S.A.; McKinlay, J.B. Association of Urological Symptoms and Chronic Illness in Men and Women: Contributions of Symptom Severity and Duration—Results From the BACH Survey. J. Urol. 2009, 181, 694–700. [Google Scholar] [CrossRef]
- Skalski, M.; Sobański, J.; Golabek, T.; Świerkosz, A.; Klasa, K.; Przydacz, M.; Rutkowski, K.; Dembińska, E.; Mielimąka, M.; Cyranka, K.; et al. Associations of selected lower urinary tract symptoms with biographical context in patients of a day hospital for neurotic disorders. Psychiatr. Polska 2016, 50, 1207–1234. [Google Scholar] [CrossRef]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef]
- Klovning, A.; Avery, K.; Sandvik, H.; Hunskaar, S. Comparison of two questionnaires for assessing the severity of urinary incontinence: The ICIQ-UI SF versus the incontinence severity index. Neurourol. Urodyn. 2009, 28, 411–415. [Google Scholar] [CrossRef]
- Park, J.S.; Ham, W.S.; Hong, C.H.; Chung, B.H.; Koo, K.C. The association of depression with lower urinary tract symptoms: Data from the National Health and Nutrition Examination Survey, 2005–2008. PeerJ 2019, 7, e7795. [Google Scholar] [CrossRef]
- Gee, B.; Orchard, F.; Clarke, E.; Joy, A.; Clarke, T.; Reynolds, S. The effect of non-pharmacological sleep interventions on depression symptoms: A meta-analysis of randomised controlled trials. Sleep Med. Rev. 2019, 43, 118–128. [Google Scholar] [CrossRef]
- Murphy, M.J.; Peterson, M.J. Sleep Disturbances in Depression. Sleep Med. Clin. 2015, 10, 17–23. [Google Scholar] [CrossRef]
- Cunningham, J.E.; Stamp, J.A.; Shapiro, C.M. Sleep and major depressive disorder: A review of non-pharmacological chronotherapeutic treatments for unipolar depression. Sleep Med. 2019, 61, 6–18. [Google Scholar] [CrossRef]
- Fang, H.; Tu, S.; Sheng, J.; Shao, A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J. Cell. Mol. Med. 2019, 23, 2324–2332. [Google Scholar] [CrossRef]
- Przydacz, M.; Golabek, T.; Sobanski, J.; Jaworska, K.; Skalski, M.; Swierkosz, A.; Dudek, P.; Sobieraj, D.; Dudek, D.; Chlosta, P. Perception of Lower Urinary Tract Symptoms by psychiatrists in mentally affected patients. Psychiatr. Pol. 2017, 51, 963–978. [Google Scholar] [CrossRef]
- Nortvedt, M.W.; Riise, T.; Sanne, B. Are men more depressed than women in Norway? Validity of the Hospital Anxiety and Depression Scale. J. Psychosom. Res. 2006, 60, 195–198. [Google Scholar] [CrossRef]
- Golabek, T.; Skalski, M.; Przydacz, M.; Świerkosz, A.; Siwek, M.; Golabek, K.; Stangel-Wójcikiewicz, K.; Dudek, D.; Chlosta, P. Lower urinary tract symptoms, nocturia and overactive bladder in patients with depression and anxiety. Psychiatr. Pol. 2015, 50, 1–14. [Google Scholar] [CrossRef]
- Wuerstle, M.C.; Eeden, S.K.V.D.; Poon, K.T.; Quinn, V.P.; Hollingsworth, J.M.; Loo, R.K.; Jacobsen, S.J.; Project, F.T.U.D.I.A. Contribution of Common Medications to Lower Urinary Tract Symptoms in Men. Arch. Intern. Med. 2011, 171, 1680–1682. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A. Genetic variation in cortico-amygdala serotonin function and risk for stress-related disease. Neurosci. Biobehav. Rev. 2008, 32, 1293–1314. [Google Scholar] [CrossRef] [PubMed]
- Laumann, E.O.; Kang, J.-H.; Glasser, D.B.; Rosen, R.C.; Carson, C.C. Lower Urinary Tract Symptoms are Associated With Depressive Symptoms in White, Black and Hispanic Men in the United States. J. Urol. 2008, 180, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.H.; Maletic, V.; Raison, C.L. Inflammation and Its Discontents: The Role of Cytokines in the Pathophysiology of Major Depression. Biol. Psychiatry 2009, 65, 732–741. [Google Scholar] [CrossRef]
- Fukunaga, A.; Kawaguchi, T.; Funada, S.; Yoshino, T.; Tabara, Y.; Matsuda, F.; Yoshimura, K.; Ogawa, O.; Negoro, H. Sleep Disturbance Worsens Lower Urinary Tract Symptoms: The Nagahama Study. J. Urol. 2019, 202, 354. [Google Scholar] [CrossRef]
- Marshall, S.D.; Raskolnikov, D.; Blanker, M.H.; Hashim, H.; Kupelian, V.; Tikkinen, K.A.; Yoshimura, K.; Drake, M.J.; Weiss, J.P. Nocturia: Current Levels of Evidence and Recommendations from the International Consultation on Male Lower Urinary Tract Symptoms. Urology 2015, 85, 1291–1299. [Google Scholar] [CrossRef]
- Tikkinen, K.A.; Johnson, T.M., II; Tammela, T.L.; Sintonen, H.; Haukka, J.; Huhtala, H.; Auvinen, A. Nocturia frequency, bother, and quality of life: How often is too often? A population-based study in Finland. Eur. Urol. 2010, 57, 488–496. [Google Scholar] [CrossRef]
| Specification | Total, N (%) |
|---|---|
| Number of included patients | 102 (100%) |
| Sex | |
| Male | 42 |
| Female | 60 |
| Education | |
| Primary | 3 |
| Secondary (including students) | 45 |
| Higher | 54 |
| Employment status | |
| Employed | 55 |
| Unemployed | 13 |
| Pensioners | 30 |
| Students | 4 |
| Relationship | |
| Stable relationship/marriage | 73 |
| Unstable relationship/marriage | 12 |
| Single | 17 |
| Drugs | Number of Patients |
|---|---|
| Antidepressants | |
| SNRIs | 47 |
| SSRIs | 46 |
| TCAs | 23 |
| NaSSAs | 21 |
| SARIs | 21 |
| Lithium | 14 |
| Others antidepressants | 10 |
| Anti-epileptics | |
| Valproate | 23 |
| Lamotrigine | 16 |
| Carbamazepine | 10 |
| Neuroleptics, first generation | |
| Phenothiazines | 35 |
| Thioxanthenes | 13 |
| Butyrophenones | 6 |
| Neuroleptics, second generation | |
| Quetiapine | 24 |
| Sulpiride | 16 |
| Olanzapine | 14 |
| Aripiprazole | 8 |
| Other neuroleptics | 6 |
| Anxiolytics | |
| Benzodiazepines | 33 |
| Hydroxyzine | 10 |
| Buspirone | 3 |
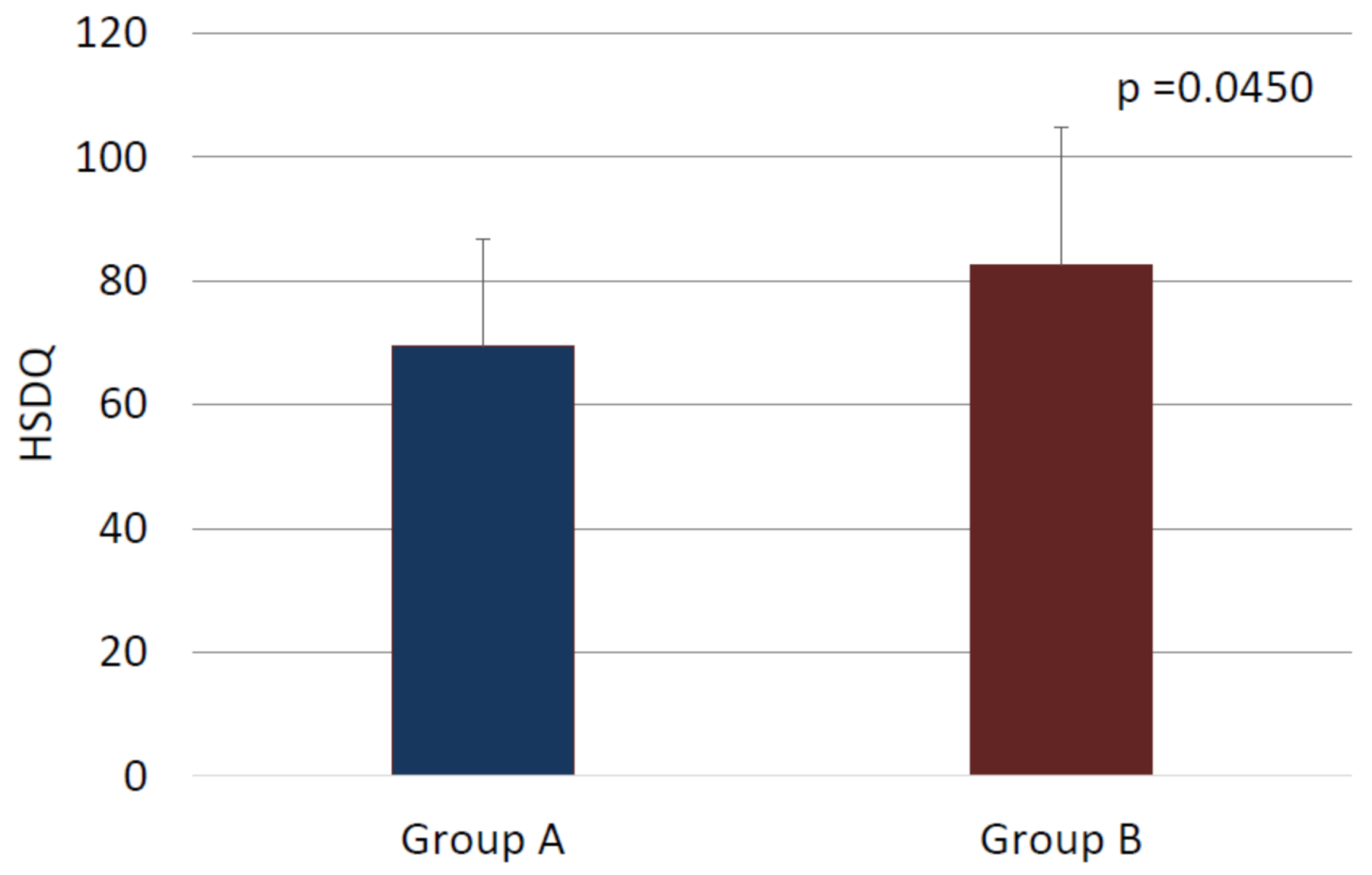
| Group A | Group B | p-Value | |
|---|---|---|---|
| HSDQ | 0.0450 1 | ||
| Mean (standard deviation) | 69.4 (17.4) | 82.5 (22.4) | |
| Range | 34.0–91.0 | 38.0–134.0 | |
| Median | 72.0 | 81.5 | |
| 95% confidence interval | [59.3;79.4] | [77.1;87.8] |
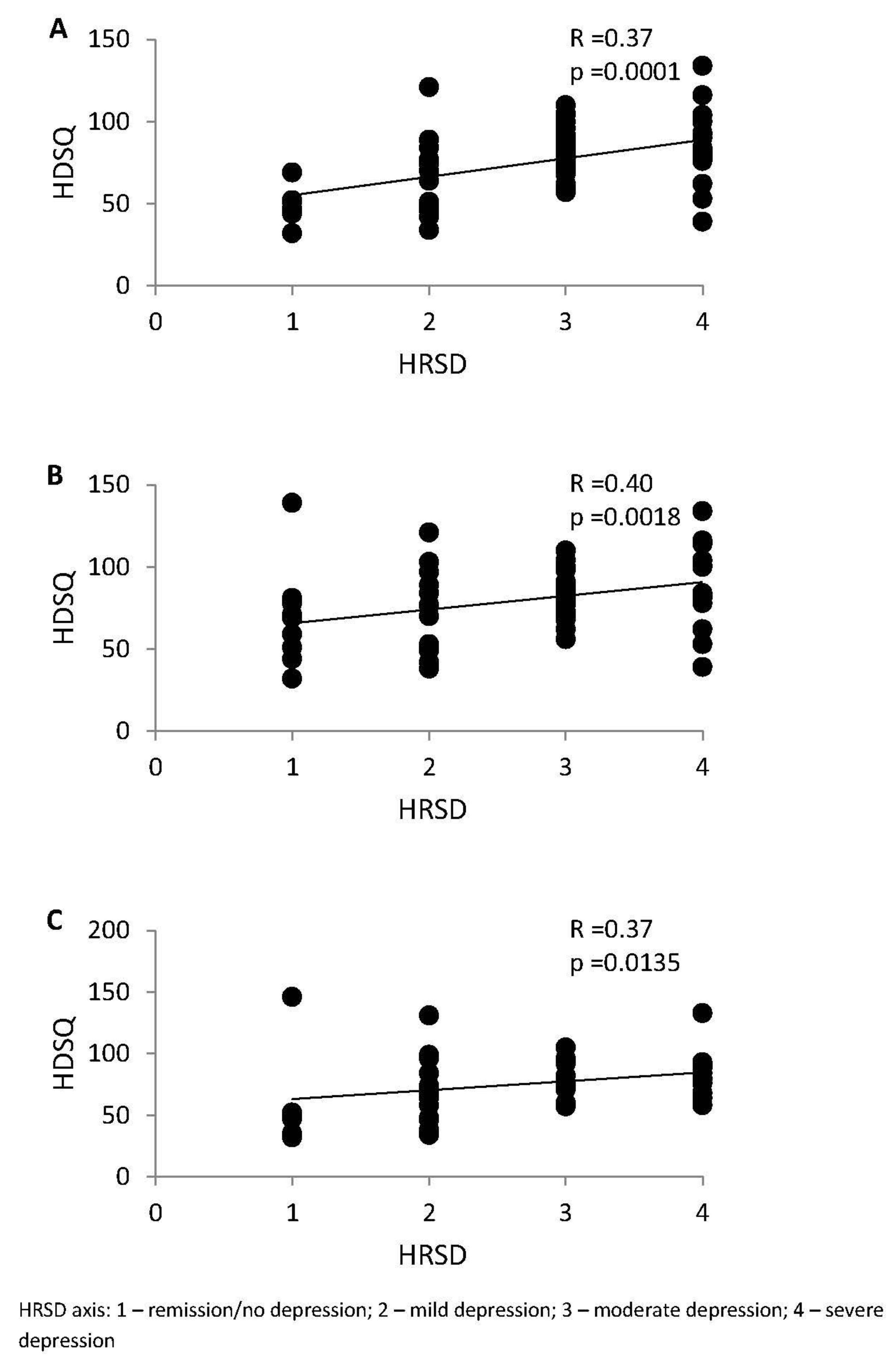
| Parameter | p-Value |
|---|---|
| HRSD | 0.0010 |
| Remission/no depression (0–7) | 0.0119 |
| Mild depression (8–16) | 0.2123 |
| Moderate depression (17–23) | 0.2780 |
| Severe depression (≥24) | 0.0193 |
| HRSD (0–16) | 0.0020 |
| HRSD (≥17) | 0.0020 |
| IPSS | 0.0001 |
| None (0) | 0.0291 |
| Mild LUTS (1–7) | 0.1659 |
| Moderate LUTS (8–19) | 0.1306 |
| Severe LUTS (20–35) | 0.0011 |
| ICIQ-UI SF | 0.0003 |
| Mild UI (1–5) | 0.0054 |
| Moderate UI (6–12) | 0.1030 |
| Severe UI (13–18) | 0.0043 |
| Very severe UI (19–21) | 0.2865 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Przydacz, M.; Skalski, M.; Sobanski, J.; Chlosta, M.; Raczynski, K.; Klasa, K.; Dudek, D.; Chlosta, P. Association between Lower Urinary Tract Symptoms and Sleep Quality of Patients with Depression. Medicina 2021, 57, 394. https://doi.org/10.3390/medicina57040394
Przydacz M, Skalski M, Sobanski J, Chlosta M, Raczynski K, Klasa K, Dudek D, Chlosta P. Association between Lower Urinary Tract Symptoms and Sleep Quality of Patients with Depression. Medicina. 2021; 57(4):394. https://doi.org/10.3390/medicina57040394
Chicago/Turabian StylePrzydacz, Mikolaj, Michal Skalski, Jerzy Sobanski, Marcin Chlosta, Karol Raczynski, Katarzyna Klasa, Dominika Dudek, and Piotr Chlosta. 2021. "Association between Lower Urinary Tract Symptoms and Sleep Quality of Patients with Depression" Medicina 57, no. 4: 394. https://doi.org/10.3390/medicina57040394
APA StylePrzydacz, M., Skalski, M., Sobanski, J., Chlosta, M., Raczynski, K., Klasa, K., Dudek, D., & Chlosta, P. (2021). Association between Lower Urinary Tract Symptoms and Sleep Quality of Patients with Depression. Medicina, 57(4), 394. https://doi.org/10.3390/medicina57040394






