The E/e’ Ratio—Role in Risk Stratification of Acute Heart Failure with Preserved Ejection Fraction
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Study Endpoints and Groups Definition
2.5. In-Patient Assessment
2.6. Statistical Analysis
3. Results
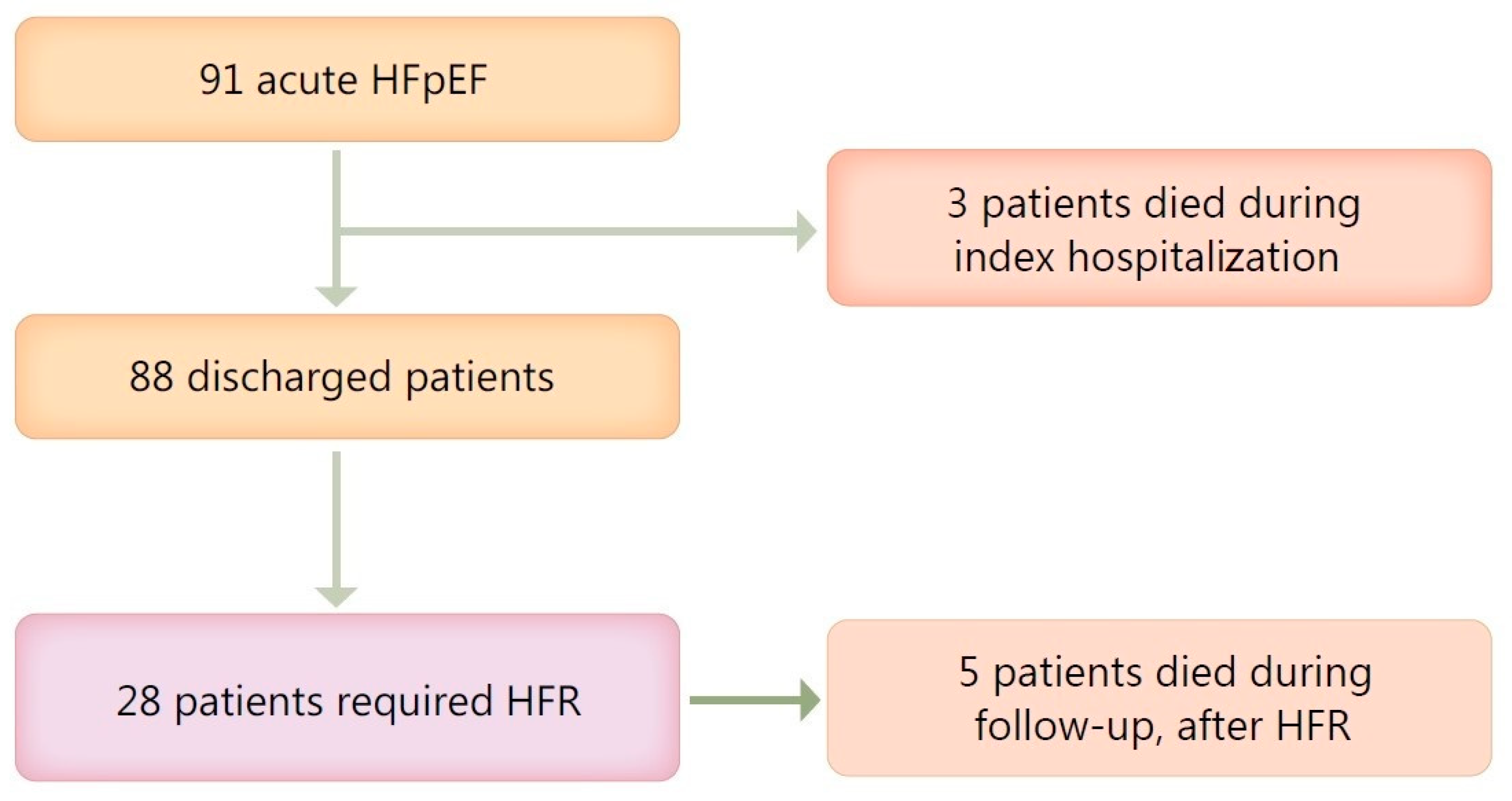
3.1. Patient Population
3.2. Baseline Characteristics
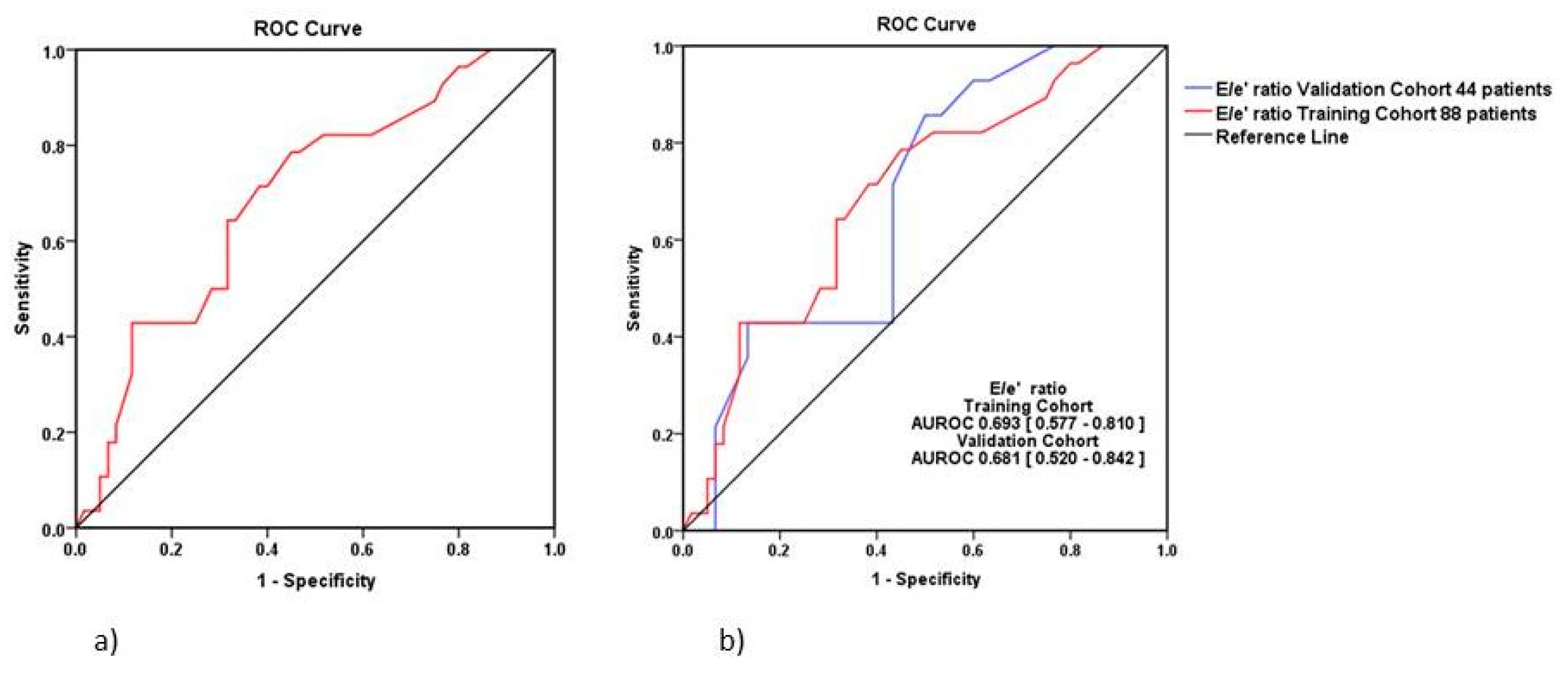
3.3. E/e’ Ratio—Independent Predictor for HFR Rehospitalization
3.4. Echocardiographic E/e’ Ratio Cut-Off for HFR
3.5. Clinical Outcomes
3.6. Echocardiography Parameters
3.7. The Risk for Heart Failure Rehospitalization and All-Cause Mortality
4. Discussion
4.1. The Rationale for the Study
4.2. Comparison to Similar Studies
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Cut-Off Value Selection | Maximize Sensitivity Associated Criterion < 8.9 | Maximize Specificity Associated Criterion > 27 | Youden’s Inde xAssociated Criterion > 13.8 | |||
|---|---|---|---|---|---|---|
| Training | Validation | Training | Validation | Training | Validation | |
| Sensitivity (%) | 100 (87.7–100) | 100 (76.8–100) | 0 (0–12.3) | 0 (0–23.2) | 78.57 (59–91.17) | 85.71 (57.2–98.2) |
| Specificity (%) | 13.33 (5.9–24.6) | 10 (2.1–26.5) | 100 (94–100) | 100 (88.4–100) | 55 (41.6.2–67.9) | 50 (31.3–68.7) |
| PPV (%) | 35 (32.8–37.3) | 34.1 (31.5–36.9) | - | - | 44.9 (36.7–53.4) | 44.4 (34.5–54.8) |
| NPV (%) | 100 | 100 | 68.2 | 68.2 | 84.6 (72.3–92.1) | 88.2 (66.4–96.6) |
| +LR | 1.15 (1–1.3) | 1.11 (1–1.3) | - | - | 1.75 (1.2–2.5) | 1.71 (1.1–2.6) |
| −LR | 0 | 0 | 1 | 1 | 0.39 (0.2–0.8) | 0.29 (0.08–1.1) |
| Univariate Analysis | E/e’ Ratio |
|---|---|
| Coefficient | 0.144 |
| Coefficient-Standard Error | 0.055 |
| Coefficient-Significance | 0.009 |
| Intercept | −2.92 |
| Intercept-Standard Error | 0.872 |
| Intercept-Significance | 0.001 |
| AUROC | 0.693 |
| Nagelkerke Pseudo-R² | 0.117 |
| Hosmer–Lemeshow p-value | 0.394 |
| AIC | 70.892 |
| BIC | 75.847 |
| Cut-off Value Selection | Maximize Sensitivity Criterion ≥ 0 | Maximize Specificity Criterion > 1 | Youden’s Index Associated Associated Criterion > 0 | |||
|---|---|---|---|---|---|---|
| Training | Validation | Training | Validation | Training | Validation | |
| Youden’s Index Associated-Value 0.335 | Youden’s Index Associated-Value 0.39 | |||||
| Sensitivity | 100 (87.7–100)% | 100 (76.8–100)% | 0 (0–12.3)% | 0 (0–23.2)% | 78.5 (59–91.7)% | 85.71 (57.2–98.2)% |
| Specificity | 0 (0–6)% | 0 (0–11.6)% | 100 (94–100)% | 100 (88.4–100)% | 55 (41.6- 67.9)% | 53.33 (34.3–71.7)% |
| PPV | 31.8% | 31.8% | - | - | 44.9 (36.7–53.4)% | 46.2 (35.6–57.1)% |
| NPV | - | - | 68.2% | 68.2% | 84.6 (72.3–92.1)% | 88.9 (68–96.8)% |
| +LR | 1 | 1 | - | - | 1.75 (1.32–2.5) | 1.84 (1.2–2.8) |
| −LR | - | - | 1 | 1 | 0.39 (0.2–0.8) | 0.27 (0.07–1) |
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Sharp, A.S.P.; Tapp, R.J.; Thom, S.A.M.G.; Francis, D.P.; Hughes, A.D.; Stanton, A.V.; Zambanini, A.; Brien, E.O.; Chaturvedi, N.; Lyons, S.; et al. Tissue Doppler E/e′ ratio is a powerful predictor of primary cardiac events in a hypertensive population: An ASCOT substudy. Eur. Heart J. 2010, 31, 747–752. [Google Scholar] [CrossRef]
- Mitter, S.S.; Shah, S.J.; Thomas, J.D. A Test in Context: E/A and E/e′ to Assess Diastolic Dysfunction and LV Filling Pressure. J. Am. Coll. Cardiol. 2017, 69, 1451–1464. [Google Scholar] [CrossRef]
- Lancellotti, P.; Galderisi, M.; Edvardsen, T.; Donal, E.; Goliasch, G.; Cardim, N.; Cardim, N.; Magne, J.; Laginha, S.; Hagendorff, A.; et al. Echo-Doppler estimation of left ventricular filling pressure: Results of themulticentre EACVI Euro-Filling study. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 961–968. [Google Scholar] [CrossRef]
- Owan, T.E.; Hodge, D.O.; Herges, R.M.; Jacobsen, S.J.; Roger, V.L.; Redfield, M.M. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N. Engl. J. Med. 2006, 355, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.P.; Donal, E.; Kraigher-Krainer, E.; Vasan, R.S. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2011, 13, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Massie, B.M.; Carson, P.E.; McMurray, J.J.; Komajda, M.; McKelvie, R.; Zile, M.R.; Anderson, S.; Donovan, M.; Iverson, E.; Staiger, C.; et al. Irbesartan in patients with heart failure and preserved ejection fraction. N. Engl. J. Med. 2008, 359, 2456–2467. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.G.F.; Tendera, M.; Adamus, J.; Freemantle, N.; Polonski, L.; Taylor, J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 2006, 27, 2338–2345. [Google Scholar] [CrossRef] [PubMed]
- Pitt, B.; Pfeffer, M.A.; Assmann, S.F.; Boineau, R.; Anand, I.S.; Claggett, B.; Clausell, N.; Desai, A.S.; Diaz, R.; Fleg, J.L.; et al. Spironolactone for Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2014, 370, 1383–1392. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin–Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef]
- Garg, R.; Gorlin, R.; Smith, T.; Yusuf, S. The Effect of Digoxin on Mortality and Morbidity in Patients with Heart Failure. N. Engl. J. Med. 1997, 336, 525–533. [Google Scholar]
- Pang, P.S.; Komajda, M.; Gheorghiade, M. The current and future management of acute heart failure syndromes. Eur. Heart J. 2010, 31, 784–793. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Vaduganathan, M.; Fonarow, G.C.; Bonow, R.O. Rehospitalization for heart failure: Problems and perspectives. J. Am. Coll. Cardiol. 2013, 61, 391–403. [Google Scholar] [CrossRef]
- Seferovic, P.M.; Ponikowski, P.; Anker, S.D.; Bauersachs, J.; Chioncel, O.; Cleland, J.G.F.; Boer, R.A.; Drexel, H.; Gal, T.B.; Hill, L.; et al. Clinical Practice Update on Heart Failure 2019: Pharmacotherapy, Procedures, Devices and Patient Management. An Expert Consensus Meeting Report of the Heart Failure Association of the European Society of Cardiology; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2019; pp. 1169–1186. [Google Scholar]
- McMurray, J.J.V.; Carson, P.E.; Komajda, M.; McKelvie, R.; Zile, M.R.; Ptaszynska, A.; Staiger, C.; Donovan, J.M.; Massie, B.M. Heart failure with preserved ejection fraction: Clinical characteristics of 4133 patients enrolled in the I-PRESERVE trial. Eur. J. Heart Fail. 2008, 10, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.S.; Lewis, E.F.; Li, R.; Solomon, S.D.; Assmann, S.F.; Boineau, R.; Clausell, N.; Diaz, R.; Fleg, J.L.; Gordeev, I.; et al. Rationale and design of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist Trial: A randomized, controlled study of spironolactone in patients with symptomatic heart failure and preserved ejection fraction. Am. Heart J. 2011, 162, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Little, W.C.; Oh, J.K. Echocardiographic evaluation of diastolic function can be used to guide clinical care. Circulation 2009, 120, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [PubMed]
- Pieske, B.; Butler, J.; Filippatos, G.; Lam, C.; Maggioni APietro Ponikowski, P.; Shah, S.; Solomon, S.; Kraigher-Krainer, E.; Samano, E.T.; Scalise, A.V.; et al. Rationale and design of the SOluble guanylate Cyclase stimulatoR in heArT failurE Studies (SOCRATES). Eur. J. Heart Fail. 2014, 16, 1026–1038. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.P.; Rienstra, M.; Tay, W.T.; Liu, L.C.Y.; Hummel, Y.M.; van der Meer, P.; de Boer, R.A.; Gelder, I.C.V.; Veldhuisen, D.J.V.; Voors, A.A.; et al. Atrial Fibrillation in Heart Failure with Preserved Ejection Fraction: Association With Exercise Capacity, Left Ventricular Filling Pressures, Natriuretic Peptides, and Left Atrial Volume. JACC Heart Fail. 2017, 5, 92–98. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association Declaration of Helsinki: Recommendations Guiding Physicians in Biomedical Research Involving Human Subjects. JAMA J. Am. Med. Assoc. 1997, 277, 925–926. [CrossRef]
- Lang, R.M.; Badano, L.P.; Victor, M.A.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. 2015, 16, 233–271. [Google Scholar]
- Chetrit, M.; Cremer, P.C.; Klein, A.L. Imaging of Diastolic Dysfunction in Community-Based Epidemiological Studies and Randomized Controlled Trials of HFpEF. JACC Cardiovasc. Imaging 2020, 13, 310–326. [Google Scholar] [CrossRef]
- Tromp, J.; Bamadhaj, S.; Cleland, J.G.F.; Angermann, C.E.; Dahlstrom, U.; Ouwerkerk, W.; Tay, W.T.; Dickstein, K.; Ertl, G.; Hassanein, M.; et al. Post-discharge prognosis of patients admitted to hospital for heart failure by world region, and national level of income and income disparity (REPORT-HF): A cohort study. Lancet Glob. Health 2020, 8, e411–e422. [Google Scholar] [CrossRef]
- Sambataro, G.; Giuffrè, M.; Sambataro, D.; Palermo, A.; Vignigni, G.; Cesareo, R.; Crimi, N.; Torrisi, S.E.; Vancheri, C.; Malatino, L.; et al. The Model for Early COvid-19 Recognition (MECOR) Score: A Proof-of-Concept for a Simple and Low-Cost Tool to Recognize a Possible Viral Etiology in Community-Acquired Pneumonia Patients during COVID-19 Outbreak. Diagnostics 2020, 10, 619. [Google Scholar] [CrossRef]
- Pieske, B.; Tschöpe, C.; De Boer, R.A.; Fraser, A.G.; Anker, S.D.; Donal, E.; Edelmann, F.; Fu, M.; Guazzi, M.; Lam, C.S.P.; et al. How to diagnose heart failure with preserved ejection fraction: The HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 2019, 40, 3297–3317. [Google Scholar] [CrossRef] [PubMed]
- Van Aelst, L.N.L.; Arrigo, M.; Placido, R.; Akiyama, E.; Girerd, N.; Zannad, F.; Manivet, P.; Rossignol, P.; Badoz, M.; Sadoune, M.; et al. Acutely decompensated heart failure with preserved and reduced ejection fraction present with comparable haemodynamic congestion. Eur. J. Heart Fail. 2018, 20, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Samman Tahhan, A.; Vaduganathan, M.; Greene, S.J.; Alrohaibani, A.; Anker, S.D.; Vardeny, O.; Fonarow, G.C.; Butler, J. Trends in prevalence of comorbidities in heart failure clinical trials. Eur. J. Heart Fail. 2020. [Google Scholar] [CrossRef]
- Beale, A.L.; Meyer, P.M.D.; Marwick, T.H.; Lam, C.S.P.; Kaye, D.M. Sex differences in cardiovascular pathophysiology why women are overrepresented in heart failure with preserved ejection fraction. Circulation 2018, 138, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Gori, M.; Lam, C.S.P.; Gupta, D.K.; Santos, A.B.S.; Cheng, S.; Shah, A.M.; Claggett, B.; Zile, M.R.; Kraigher-Krainer, E.; Pieske, B.; et al. Sex-specific cardiovascular structure and function in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2014, 16, 535–542. [Google Scholar] [CrossRef]
- Ho, J.E.; Gona, P.; Pencina, M.J.; Tu, J.V.; Austin, P.C.; Vasan, R.S.; Kannel, W.B.; D’Agostino, R.B.; Lee, D.S.; Levy, D. Discriminating clinical features of heart failure with preserved vs. reduced ejection fraction in the community. Eur. Heart J. 2012, 33, 1734–1741. [Google Scholar] [CrossRef]
- Owei, I.; Umekwe, N.; Wan, J.; Dagogo-Jack, S. Plasma lipid levels predict dysglycemia in a biracial cohort of nondiabetic subjects: Potential mechanisms. Exp. Biol. Med. 2016, 241, 1961–1967. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Dávila-Román, V.G.; Mann, D.L.; McNulty, S.; Semigran, M.J.; Lewis, G.D.; Fuentes, L.d.I.; Joseph, S.M.; Vader, J.; Hernandez, A.F.; et al. Cardiovascular phenotype in HFpEF patients with or without diabetes: A RELAX trial ancillary study. J. Am. Coll. Cardiol. 2014, 64, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Lahewala, S.; Hassan Virk, H.U.; Setareh-Shenas, S.; Patel, P.; Kumar, V.; Tripathi, B.; Shah, H.; Patel, V.; Gidwani, U.; et al. Etiologies, Trends, and Predictors of 30-Day Readmissions in Patients With Diastolic Heart Failure. Am. J. Cardiol. 2017, 120, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Habibi, J.; Aroor, A.R.; Sowers, J.R.; Jia, G.; Hayden, M.R.; Garro, M.; Barron, B.; Mayoux, E.; Rector, R.S.; Whaley-Connell, A.; et al. Sodium glucose transporter 2 (SGLT2) inhibition with empagliflozin improves cardiac diastolic function in a female rodent model of diabetes. Cardiovasc. Diabetol. 2017, 16, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Zile, M.R.; Gottdiener, J.S.; Hetzel, S.J.; McMurray, J.J.; Komajda, M.; McKelvie, R.; Baicu, C.F.; Massie, B.M.; Carson, P.E.; Investigators, I.P. Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation 2011, 124, 2491–2501. [Google Scholar] [CrossRef]
- Katz, D.H.; Beussink, L.; Sauer, A.J.; Freed, B.H.; Burke, M.A.; Shah, S.J. Prevalence, clinical characteristics, and outcomes associated with eccentric versus concentric left ventricular hypertrophy in heart failure with preserved ejection fraction. Am. J. Cardiol. 2013, 112, 1158–1164. [Google Scholar] [CrossRef]
- Shah, A.M.; Shah, S.J.; Anand, I.S.; Sweitzer, N.K.; O’Meara, E.; Heitner, J.F.; Sopko, G.; Li, G.; Assmann, S.F.; McKinlay, S.M.; et al. Cardiac structure and function in heart failure with preserved ejection fraction: Baseline findings from the echocardiographic study of the treatment of preserved cardiac function heart failure with an aldosterone antagonist trial. Circ. Heart Fail. 2014, 7, 104–115. [Google Scholar] [CrossRef]
- Carbone, S.; Lavie, C.J. Disparate effects of obesity on survival and hospitalizations in heart failure with preserved ejection fraction. Int. J. Obes. 2020, 44, 1543–1545. [Google Scholar] [CrossRef] [PubMed]
- Madamanchi, C.; Alhosaini, H.; Sumida, A.; Runge, M.S. Obesity and natriuretic peptides, BNP and NT-proBNP: Mechanisms and diagnostic implications for heart failure. Int. J. Cardiol. 2014, 176, 611–617. [Google Scholar] [CrossRef]
- Daniels, L.B.; Maisel, A.S. Natriuretic Peptides. J. Am. Coll. Cardiol. 2007, 50, 2357–2368. [Google Scholar] [CrossRef]
- Anjan, V.Y.; Loftus, T.M.; Burke, M.A.; Akhter, N.; Fonarow, G.C.; Gheorghiade, M.; Shah, G. Prevalence, clinical phenotype, and outcomes associated with normal B-type natriuretic peptide levels in heart failure with preserved ejection fraction. Am. J. Cardiol. 2012, 110, 870–876. [Google Scholar] [CrossRef]
- Kao, D.P.; Lewsey, J.D.; Anand, I.S.; Massie, B.M.; Zile, M.R.; Carson, P.E.; McKelvie, R.S.; Komajda, M.; McMurray, J.J.V.; Lindenfeld, J. Characterization of subgroups of heart failure patients with preserved ejection fraction with possible implications for prognosis and treatment response. Eur. J. Heart Fail. 2015, 17, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Abudiab, M.M.; Chebrolu, L.H.; Schutt, R.C.; Nagueh, S.F.; Zoghbi, W.A. Doppler Echocardiography for the Estimation of LV Filling Pressure in Patients with Mitral Annular Calcification. JACC Cardiovasc. Imaging 2017, 10, 1411–1420. [Google Scholar] [CrossRef]
- Donal, E.; Galli, E.; Fraser, A.G. Non-invasive estimation of left heart filling pressures: Another nail in the coffin for E/e’? Eur. J. Heart Fail. 2017, 19, 1661–1663. [Google Scholar] [CrossRef]
- Sharifov, O.F.; Schiros, C.G.; Aban, I.; Denney, T.S.; Gupta, H. Diagnostic accuracy of tissue Doppler index E/e’ for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: A systematic review and meta-analysis. J. Am. Heart Assoc. 2016, 5, e002530. [Google Scholar] [CrossRef]
- Hummel, Y.M.; Liu, L.C.Y.; Lam, C.S.P.; Fonseca-Munoz, D.F.; Damman, K.; Rienstra, M.; van der Meer, P.; Rosenkranz, S.; van Veldhuisen, D.J.; Voors, A.A.; et al. Echocardiographic estimation of left ventricular and pulmonary pressures in patients with heart failure and preserved ejection fraction: A study utilizing simultaneous echocardiography and invasive measurements. Eur. J. Heart Fail. 2017, 19, 1651–1660. [Google Scholar] [CrossRef]
- Donal, E.; Lund, L.H.; Oger, E.; Hage, C.; Persson, H.; Reynaud, A.; Ennezat, P.V.; Bauer, F.; Drouet, E.; Linde, C.; et al. New echocardiographic predictors of clinical outcome in patients presenting with heart failure and a preserved left ventricular ejection fraction: A subanalysis of the Ka (Karolinska) Ren (Rennes) Study. Eur. J. Heart Fail. 2015, 17, 680–688. [Google Scholar] [CrossRef]
- Holland, D.J.; Prasad, S.B.; Marwick, T.H. Prognostic implications of left ventricular filling pressure with exercise. Circ. Cardiovasc. Imaging 2010, 3, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, M.; Sakuragi, S.; Miyoshi, T.; Takayama, S.; Kawaguchi, T.; Kodera, N.; Akai, H.; Koide, Y.; Otsuka, H.; Wada, T.; et al. Fibrosis-4 index reflects right ventricular function and prognosis in heart failure with preserved ejection fraction. ESC Heart Fail. 2021. [Google Scholar] [CrossRef] [PubMed]
- Moreo, A.; Ambrosio, G.; De Chiara, B.; Pu, M.; Tran, T.; Mauri, F.; Raman, S.V. Influence of myocardial fibrosis on left ventricular diastolic function noninvasive assessment by cardiac magnetic resonance and echo. Circ. Cardiovasc. Imaging 2009, 2, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Müller-Brunotte, R.; Kahan, T.; López, B.; Edner, M.; González, A.; Díez, J.; Malmqvist, K. Myocardial fibrosis and diastolic dysfunction in patients with hypertension: Results from the Swedish Irbesartan Left Ventricular Hypertrophy Investigation versus Atenolol (SILVHIA). J. Hypertens. 2007, 25, 1958–1966. [Google Scholar] [CrossRef] [PubMed]
- Brilla, C.G.; Funck, R.C.; Rupp, H. Lisinopril-mediated regression of myocardial fibrosis in patients with hypertensive heart disease. Circulation 2000, 102, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- Drazner, M.H. The progression of hypertensive heart disease. Circulation 2011, 123, 327–334. [Google Scholar] [CrossRef]
- Blanco, R.; Ambrosio, G.; Belziti, C.; Lucas, L.; Arias, A.; D’Antonio, A.; Oberti, P.; Carluccio, E.; Pizarro, R. Prognostic value of NT-proBNP, and echocardiographic indices of diastolic function, in hospitalized patients with acute heart failure and preserved left ventricular ejection fraction. Int. J. Cardiol. 2020, 317, 111–120. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Zannad, F.; Sopko, G.; Klein, L.; Piña, I.L.; Konstam, M.A.; Massie, B.M.; Roland, E.; Targum, S.; Collins, S.P.; et al. Acute heart failure syndromes: Current state and framework for future research. Circulation 2005, 112, 3958–3968. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; De Luca, L.; Fonarow, G.C.; Filippatos, G.; Metra, M.; Francis, G.S. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am. J. Cardiol. 2005, 96, 11–17. [Google Scholar] [CrossRef]
- Voors, A.A.; Ouwerkerk, W.; Zannad, F.; van Veldhuisen, D.J.; Samani, N.J.; Ponikowski, P.; Ng, L.L.; Metra, M.; Maaten, J.M.T.; Lang, C.C.; et al. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur. J. Heart Fail. 2017, 19, 627–634. [Google Scholar] [CrossRef]
- Kasner, M.; Westermann, D.; Steendijk, P.; Gaub, R.; Wilkenshoff, U.; Weitmann, K.; Hoffmann, W.; Poller, W.; Schultheiss, H.P.; Pauschinger, M.; et al. Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: A comparative Doppler-conductance catheterization study. Circulation 2007, 116, 637–647. [Google Scholar] [CrossRef]
- Kasner, M.; Gaub, R.; Sinning, D.; Westermann, D.; Steendijk, P.; Hoffmann, W.; Schultheiss, H.P.; Tschöpe, C. Global strain rate imaging for the estimation of diastolic function in HFNEF compared with pressure-volume loop analysis. Eur. J. Echocardiogr. 2010, 11, 743–751. [Google Scholar] [CrossRef][Green Version]
- Dickinson, M.G.; Lam, C.S.; Rienstra, M.; Vonck, T.E.; Hummel, Y.M.; Voors, A.A.; Hoendermis, E.S. Atrial fibrillation modifies the association between pulmonary artery wedge pressure and left ventricular end-diastolic pressure. Eur. J. Heart Fail. 2017, 19, 1483–1490. [Google Scholar] [CrossRef]


| Characteristics | Value |
|---|---|
| Number (%) | 91 (100%) |
| Length of in-hospital stay, days, median (IQR) | 7.50 (5) |
| Age at diagnosis, yo, mean ± SD (95% CI) | 73.04 ± 10.61 (70.83–75.25) |
| Female gender, n (%) | 62 (68.1%) |
| Cardiovascular risk factors | |
| High blood pressure, n (%) | 91 (100%) |
| Diabetes mellitus, n (%) | 51 (56%) |
| Tobacco smoking (current or former), n (%) | 25 (27.5%) |
| Hypercholesterolemia, n (%) | 75 (82.4%) |
| BMI, mean ± SD (95% CI) | 32.13 ± 6.33 (30.81–33.45) |
| Previous medical history | |
| Medical history of CAD, n (%) | 21 (23.1%) |
| Medical history of MI, n (%) | 13 (14.3%) |
| Medical history of stroke, n (%) | 18 (19.8%) |
| History of Atrial fibrillation, n (%) | 63 (69.2%) |
| Medical history of lung disease, n (%) | 44(48.40%) |
| Medical history of sleep apnoea, n (%) | 12 (13.2%) |
| Assessment on admission | |
| Non-Invasive ventilation on admission, n (%) | 20 (22%) |
| Mechanical ventilation on admission, n (%) | 6 (6.6%) |
| Peripheral edema on admission, n (%) | 53 (58.20%) |
| SaO2 on admission, median (IQR) | 89 (6) |
| HR on admission, median (IQR) | 96 (55) |
| SBP, mm Hg, mean ± SD (95% CI) | 185.44 ± 34.77 (178.20–192.68) |
| Serum natremia, mmol/L, median (IQR) | 140 (5) |
| eGFR, mL/min/1.73sqm, mean ± SD (95% CI) | 66.52 ± 28.76 (60.53–72.51) |
| Hb, g/dL, mean ± SD (95% CI) | 11.97 ± 2.03 (11.55–12.39) |
| NTproBNP, ng/L, median (IQR) | 3074 (5241) |
| Characteristics | E/e’ Ratio < 13.80 | E/e’ Ratio > 13.80 | p-Value |
|---|---|---|---|
| Number (%) | 39 (44.30%) | 49 (55.70%) | |
| Age (yo) mean ± SD (95% CI) | 73.62 ± 9.95 (70.39–76.84) | 72.35 ± 11.36 (69.08–75.61) | 0.58 a |
| Male gender, n (%) | 12 (30.80%) | 17 (34.7%) | 0.69 ** |
| Smoking status, n (%) | 10 (25.60%) | 15 (30.60%) | 0.60 ** |
| Medical history of DM, n (%) | 15 (38.50%) | 33(67.3%) | 0.007 ** |
| Medical history of hypercholesterolemia, n (%) | 27 (69.20%) | 45 (91.8%) | 0.006 * |
| Medical history of CAD, n (%) | 6 (15.40%) | 15 (30.60%) | 0.096 * |
| Medical history of MI, n (%) | 3 (7.70%) | 10 (20.40%) | 0.095 * |
| Medical history of lung disease, n (%) | 20 (51.30%) | 22 (44.90%) | 0.55 * |
| Medical history of sleep apnoea, n (%) | 3 (7.70%) | 8 (16.30%) | 0.22 * |
| Pulmonary edema on admission, n (%) | 9 (23.70%) | 18 (37.50%) | 0.17 * |
| Peripheral edema on admission, n (%) | 23 (59%) | 29 (59.20%) | 0.98 * |
| BMI (kg/m²), mean ± SD (95% CI) | 31.13 ± 4.70 (29.61–32.66) | 32.73 ± 7.30 (30.63–34.83) | 0.21 * |
| SpO2 (%) on index admission, median (IQR) | 90 (5) | 87 (6) | 0.04 * |
| Heart rate (beats/min), mean ± SD (95% CI) | 109.36 ± 35.35 (97.90–120.82) | 104.73 ± 31.37 (95.72–113.75) | 0.64 a |
| SBP (mm Hg) on index admission, mean ± SD (95% CI) | 176.41 ± 30.02 (166.68–186.14) | 190.92 ± 37.27 (180.21–201.62) | 0.046 a |
| eGFR (mL/min/1.73 m²), mean ± SD (95% CI) | 72.74 ± 25.27 (64.55–80.94) | 61.38 ± 30.54 (52.61–70.16) | 0.06 a |
| Hb (g/dL) on index admission, mean ± SD (95% CI) | 12.36 ± 1.59 (11.84–12.88) | 11.70 ± 2.28 (11.04–12.35) | 0.11 a |
| NTproBNP (ng/L) on index admission, median (IQR) | 3800 (6323) | 2862 (5200) | 0.41 * |
| Left ventricle ejection fraction (%), mean ± SD (95% CI) | 55.87 ± 5.03 (54.24–57.50) | 55.86 ± 6.70 (53.93–57.78) | 0.99 a |
| LVEDD (mm), mean ± SD (95% CI) | 46.03 ± 5.15 (44.36–47.70) | 49.02 ± 5.47 (47.45–50.59) | 0.01 a |
| Left ventricle mass (g/m2), median (IQR) | 113 (26) | 130 (45.50) | 0.006 * |
| LVOT VTI (cm), median (IQR) | 16 (8) | 19.50 (5) | 0.012 * |
| TAPSE < 17mm, n (%) | 14 (35.90%) | 8 (16.30%) | 0.035 ** |
| Systolic PAP (mm Hg), mean ± SD (95% CI) | 40.46 ± 10.24 (37.14–43.78) | 41.10 ± 18.16 (35.88–46.31) | 0.83 a |
| DBP (mm Hg) on index admission, mean ± SD (95% CI) | 96.13 ± 15.41, (91.13–101.12) | 101.22 ± 20.06, (95.46–106.99) | 0.19 a |
| Systolic PAP > 35, n (%) | 30 (76.90%) | 28 (57.10%) | 0.052 ** |
| IVC diameter > 21 mm, n (%) | 20 (51.30%) | 19 (38.80%) | 0.24 ** |
| IVC collapse < 50%, n (%) | 16 (41%) | 18 (36.70%) | 0.68 ** |
| LAVi (mL/m²), mean ± SD (95% CI) | 50.41 ± 10.84 (46.90–53.92) | 52.03 ± 13.08 (48.27–55.79) | 0.53 a |
| Length of in-hospital stay (days), median (IQR) | 7 (6) | 8 (5) | 0.78 * |
| HFR at 6 months, n (%) | 6 (15.40%) | 22 (44.90%) | 0.003 ** |
| Time to first HFR (days), median (IQR) | 75 (104.75) | 30 (37.50) | 0.002 * |
| Number of rehospitalization/patient at 6 months, median (IQR) | 0 (1) | 1 (2) | 0.003 * |
| All-cause mortality at 6 months, n (%) | 2 (5.1%) | 3 (6.1%) | 0.84 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zamfirescu, M.-B.; Ghilencea, L.-N.; Popescu, M.-R.; Bejan, G.C.; Maher, S.M.; Popescu, A.-C.; Dorobanțu, M. The E/e’ Ratio—Role in Risk Stratification of Acute Heart Failure with Preserved Ejection Fraction. Medicina 2021, 57, 375. https://doi.org/10.3390/medicina57040375
Zamfirescu M-B, Ghilencea L-N, Popescu M-R, Bejan GC, Maher SM, Popescu A-C, Dorobanțu M. The E/e’ Ratio—Role in Risk Stratification of Acute Heart Failure with Preserved Ejection Fraction. Medicina. 2021; 57(4):375. https://doi.org/10.3390/medicina57040375
Chicago/Turabian StyleZamfirescu, Marilena-Brîndușa, Liviu-Nicolae Ghilencea, Mihaela-Roxana Popescu, Gabriel Cristian Bejan, Sean Martin Maher, Andreea-Catarina Popescu, and Maria Dorobanțu. 2021. "The E/e’ Ratio—Role in Risk Stratification of Acute Heart Failure with Preserved Ejection Fraction" Medicina 57, no. 4: 375. https://doi.org/10.3390/medicina57040375
APA StyleZamfirescu, M.-B., Ghilencea, L.-N., Popescu, M.-R., Bejan, G. C., Maher, S. M., Popescu, A.-C., & Dorobanțu, M. (2021). The E/e’ Ratio—Role in Risk Stratification of Acute Heart Failure with Preserved Ejection Fraction. Medicina, 57(4), 375. https://doi.org/10.3390/medicina57040375








