3.1. Survey Question Responses
In total there were 23 responses received from EUROMENE members across 19 countries, namely: Austria, Belgium, Bulgaria, Denmark, Finland, France, Germany (3 responses), Greece, Ireland, Italy, Latvia, Netherlands, Norway, Poland, Romania, Serbia, Slovenia, Spain (3 responses), and the UK. With 20 member countries in EUROMENE, this represents a 95% country-level response rate. Where multiple responses were received from a country (namely Germany and Spain), we first examined the consistency of responses at a country level. Since there were some differences in responses for these countries for some questions, we chose to use data from all 23 responses in our analysis. Overall, however, our key results and findings do not alter significantly if we instead use a measure of the average response for these countries (results available on request).
In terms of the professional roles of respondents, 9 indicated that they were academics, 8 that they were medical consultants (e.g., neurology, internal medicine, infectious disease, psychology), 8 that they were GPs, 2 that they were retired, while 2 did not specify. Some respondents reported dual roles e.g., consultant and academic positions.
To start,
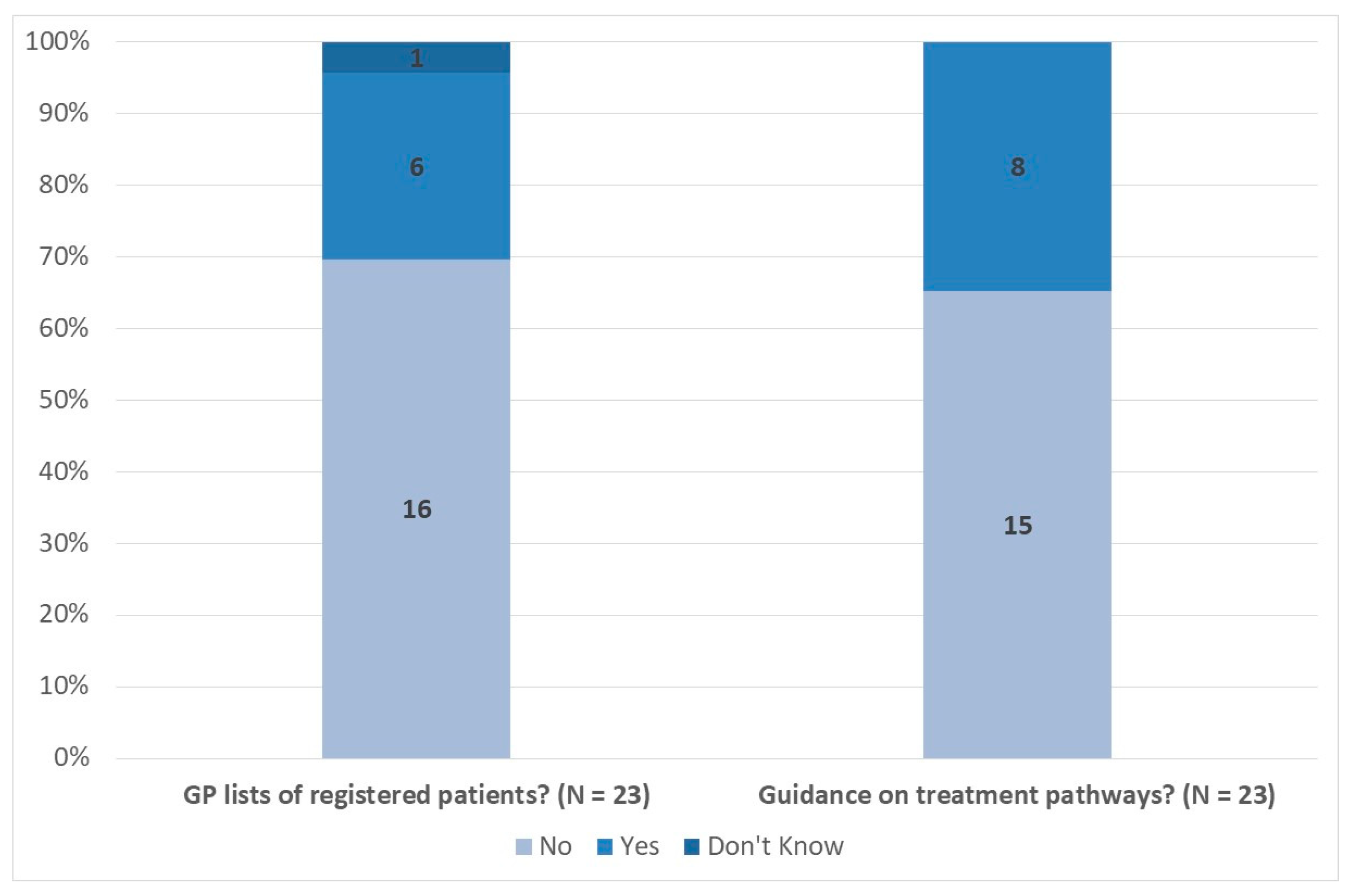
Figure 1 presents a summary of survey responses relating to the existence of GP patient lists and national guidance on treatment pathways. Overall 16 respondents (70%) reported there are no GP lists of registered patients in their country, while 15 (65%) reported no specific national guidance on treatment pathways.
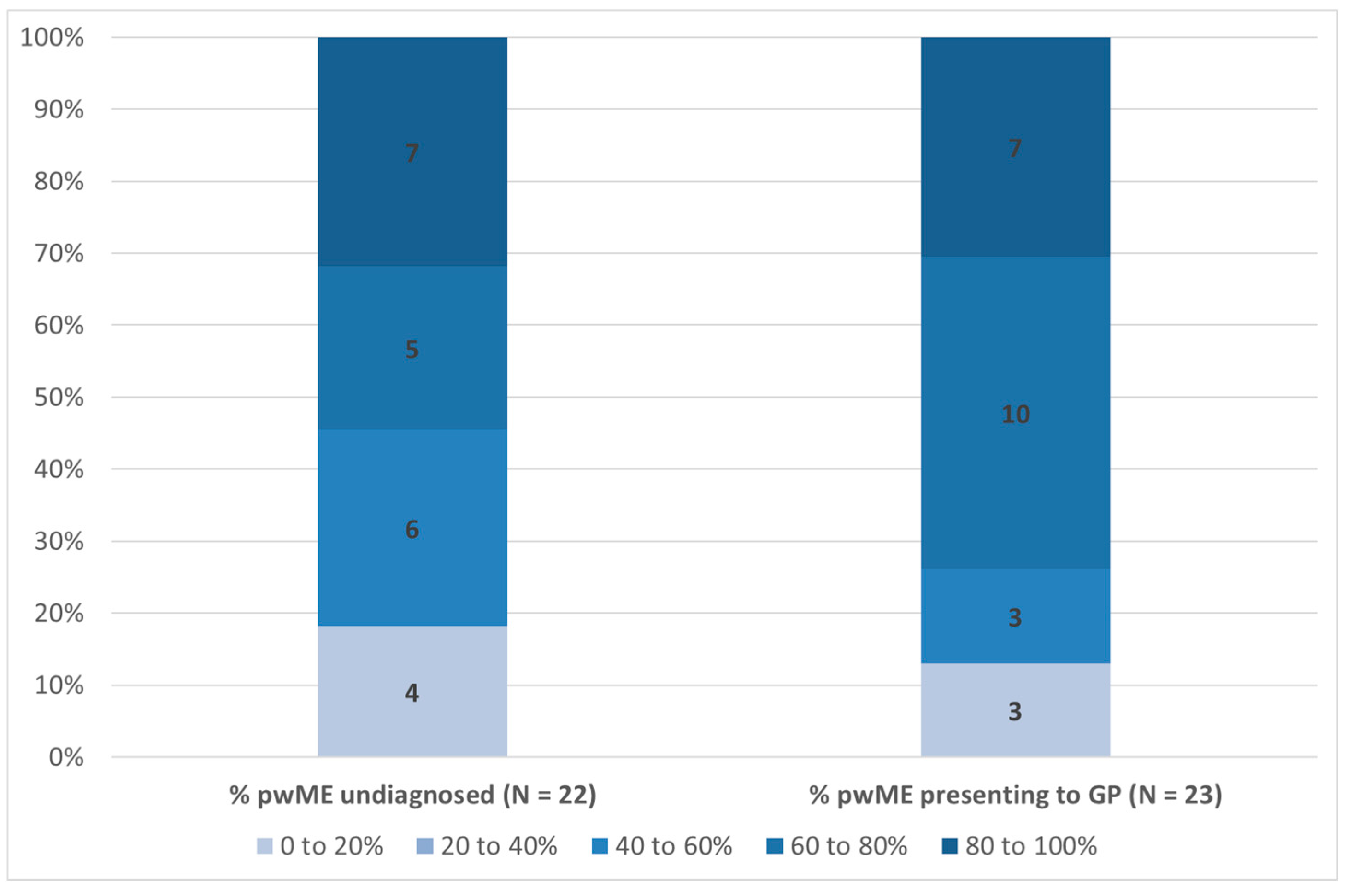
Figure 2 presents results relating to the percentage of people with ME/CFS that remain undiagnosed and the percentage that present to a GP. In relation to the former, there is considerable variation across respondents, with 4 respondents (18%) reporting between 0% and 20% remain undiagnosed, 6 (27%) that the proportion is 40–60%, 5 (23%) that it is 60% and 80%, and 7 (32%) that between 80% and 100% remain undiagnosed. It should be noted that one respondent did not answer this question. Taking a weighted average of all responses, and assuming a mid-point value for each option, gives an estimated average of 60% of people with ME/CFS remaining undiagnosed across our survey responses.
Figure 2 also includes responses relating to the percentage of people with ME/CFS that present to a GP. Here 3 respondents (13%) reported that 0–20% do so, 3 (13%) that it is 20–40%, 10 (44%) that it is 60–80%, and 7 (30%) reported that between 80% and 100% of people with ME/CFS present to a GP. The weighted average is 66%, implying the majority present to a GP.
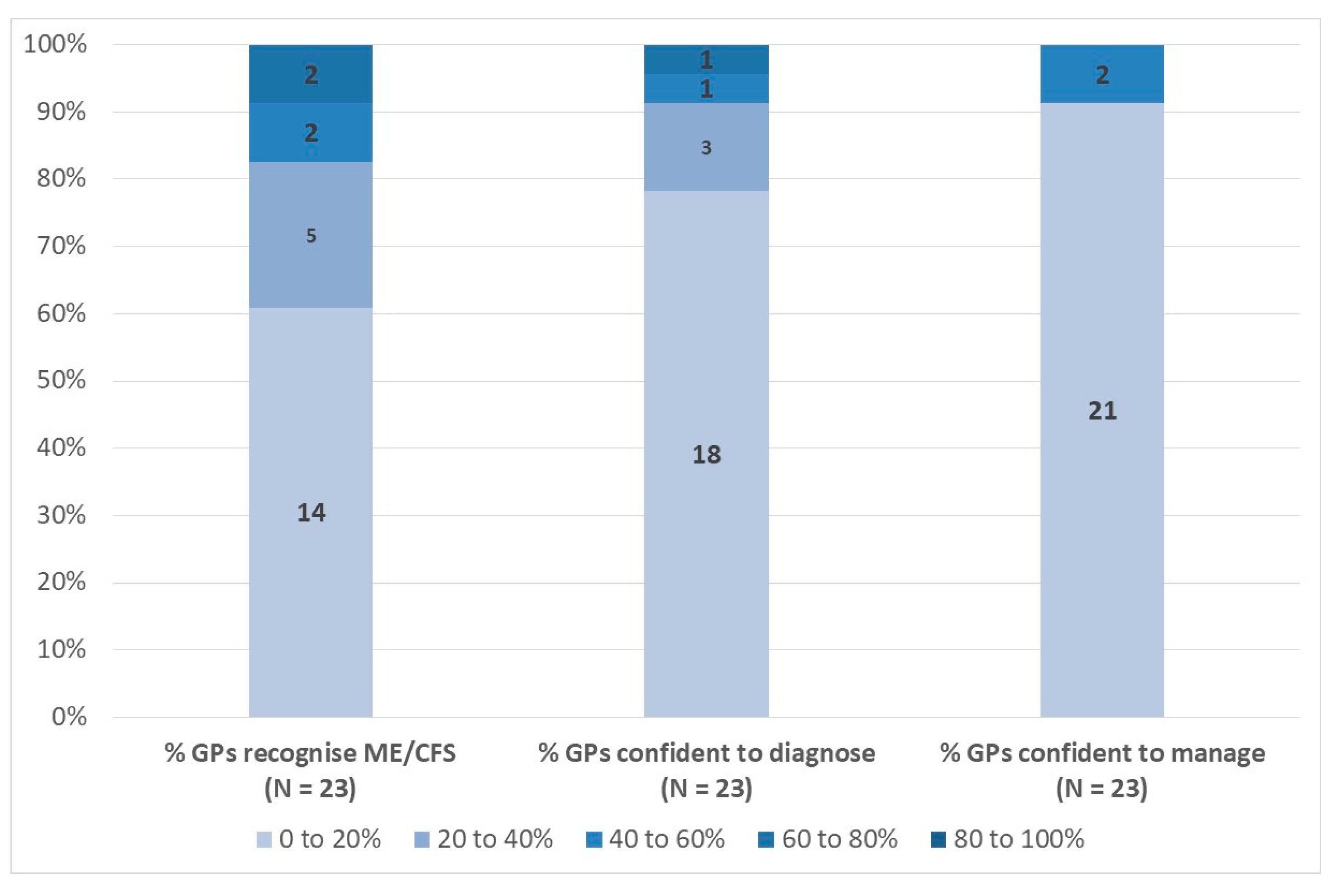
Responses to the questions relating to GP recognition, confidence in diagnosing, and confidence in managing ME/CFS are presented in
Figure 3. For GP recognition of the condition, 14 respondents (61%) chose the 0–20% option, while 5 (22%) reported 20–40%. Only a small number of respondents selected the other options and the weighted average estimate of the percentage of GPs recognising ME/CFS as a genuine clinical entity was 23%. Similar yet more pronounced patterns are evident for the diagnosis and management of ME/CFS. For example, 18 respondents (78%) reported that between 0% and 20% of GPs are confident of their ability to diagnose ME/CFS, with a weighted average of 17%. For management, 21 respondents (91%) reported that between 0% and 20% of GPs are confident of their ability to manage ME/CFS patients, with a weighted average of just 14%.
Figure 4 presents an overview of responses to the questions relating to the percentages of patients that are diagnosed by their GP, that are referred by their GP to specialist care, and that self-refer to specialist services. Overall, 14 respondents (61%) reported that between 0% and 20% of patients with ME/CFS who consult with their GP are in fact diagnosed by them, with 4 (18%) reporting the proportion to be 20–40% and 40–80%. The weighted average estimate from these respondents is 26%. There was more variation across responses to the question relating to GP referral to specialist care. For example, 5 respondents (23%) reported this to be 0–20% in their country, 5 (23%) that it is 20–40%, 3 (14%) that it is 40–60%, 7 (32%) that it is 60–80%, and 2 (9%) that 80–100% of patients that present to a GP are referred by the GP to specialist care. The weighted average response is 46%. Finally,
Figure 4 also shows the responses relating to self-referral to specialist services. Again there is quite a lot of variation across respondents for this question, possibly due to variability in how this question was interpreted by ME/CFS specialists versus other specialists, and the weighted average percentage of patients self-referring is an estimated 51%.
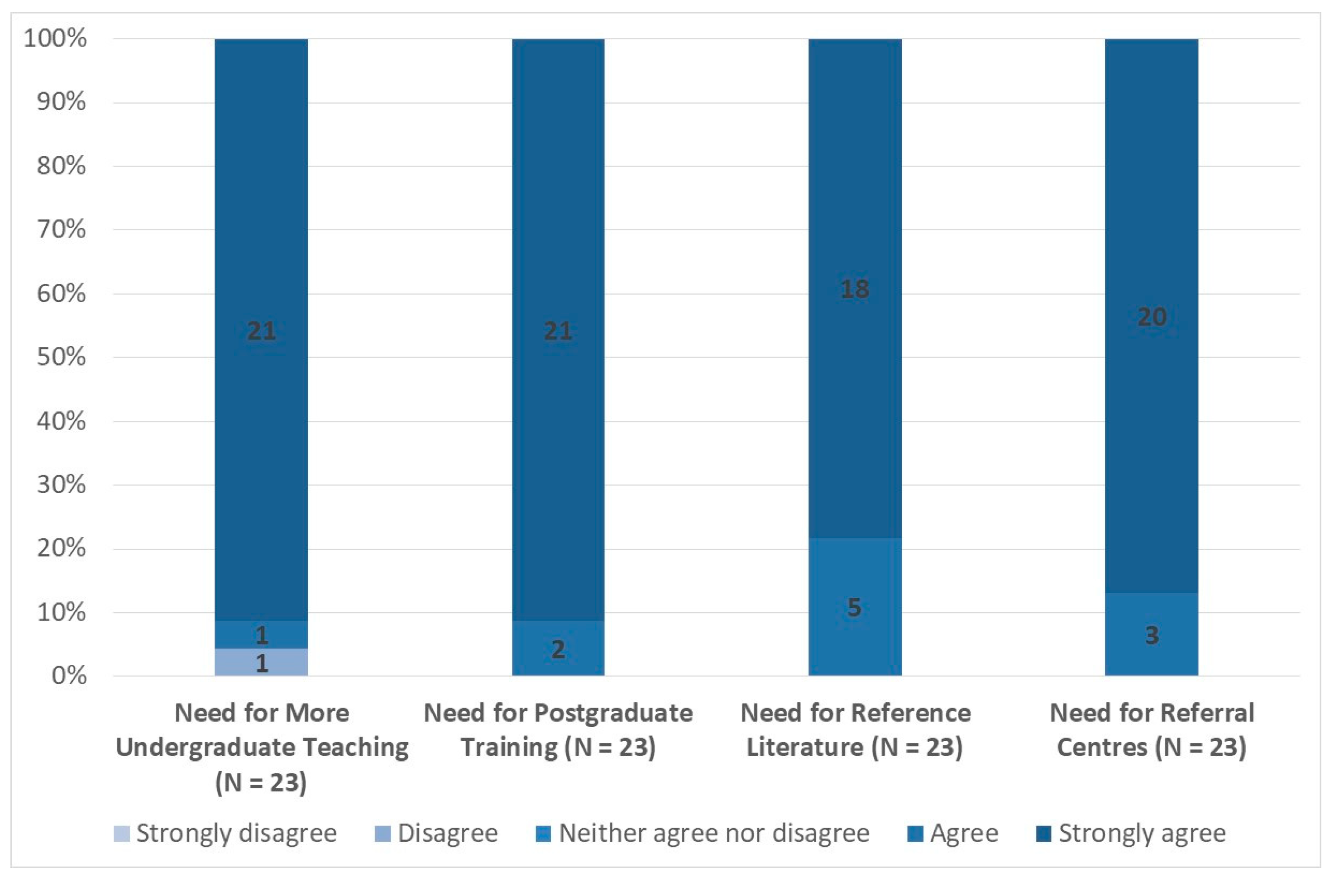
Responses to the questions relating to the needs for teaching, training, reference literature, and referral centres are presented in
Figure 5. Given the very high levels of consistency in responses across these responses, there is little need to discuss them in detail. Nonetheless, it is important to note that 21 respondents (91%) strongly agreed that there should be more teaching about ME/CFS in undergraduate medical curricula, while 21 respondents (91%) strongly agreed that postgraduate training about ME/CFS should be available for doctors and other healthcare professionals. For the latter question, the remaining survey respondents agreed with the statement. In addition, all respondents either strongly agreed or agreed that there is a need for succinct reference literature on ME/CFS for doctors and other healthcare professionals in primary care and that there is a need to ensure the existence of adequate secondary and tertiary referral centres for ME/CFS, from which primary care doctors could seek help and advice when necessary.
3.2. Analysis of Free Text Responses
3.2.1. Official Guidance on ME/CFS
Respondents were asked to indicate whether official guidance on ME/CFS for healthcare professionals existed in their countries. Their free text responses indicated that such guidance was available and accessible, or under development, in Belgium, Germany, Italy, the Netherlands, Norway, Slovenia, Spain, the United Kingdom, and Finland. In Ireland, while there were no guidelines, clinicians tended to follow the UK NICE guidelines. The responses are summarised below.
Belgium has guidelines on diagnosis and clinical pathways from the government’s illness insurance programme. In Germany, there is a guideline on fatigue in general, which also covers ME/CFS, but it is said to be quite superficial and to lack understanding of the disease, and is therefore unhelpful. In Italy, a document was published in 2014 on behalf of AGENAS (the National Agency for Regional Health Services), which is part of the Health Ministry. It promotes a multidisciplinary approach to ME/CFS, with advice on aetiology, physiopathology, clinical features, diagnosis, and treatment. Practice in the Netherlands was reported to be based on American guidance from 2015. This likely refers to guidance published by the Institute of Medicine (IOM), now the National Academy of Medicine (NAM), entitled “Beyond Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Redefining an Illness”, and summarised in a guide for healthcare providers [
6]. Norway published guidance in 2014, and this was revised in 2015. It covers interdisciplinary investigation, diagnosis, treatment, rehabilitation and care, in various care locations (outpatients, inpatients, rehabilitation institutions, and self-management programmes) [
7].
In Slovenia, EULAR recommendations for the management of fibromyalgia are followed [
8]. In Spain, the public health system published a guide in 2019, but this guide was withdrawn, and patient associations and doctors who treat patients with ME/CFS have requested a complete review. It is also suggested that AQUAS 2017 is followed. AQUAS (Aggregated Quality Assurance for Systems) is an EU supported project promoting a holistic approach to safety, security, and performance in system development, medicine being one of the priority areas [
9]. However, this appears rather remote from the diagnosis and management of patients with ME/CFS. In the United Kingdom, the NICE (National Institute for Health and Care Excellence) guidelines for ME/CFS are currently being revised [
10]. Finland has official guidance in preparation. While it includes little on treatment pathways, there will be confirmation that pacing has a role in management, and that graded exercise therapy (GET) and cognitive behaviour therapy (CBT) will not be considered as effective treatment, which is very much in line with the current UK draft guideline from NICE.
3.2.2. Specialist Care
Themes identified in the responses included the inadequacy of specialist care, the nature of the illness, specialties involved in care, multidisciplinary approaches, GP involvement, psychiatric involvement in care, the content of therapy, and the role of specialist centres. Emergent sub-themes regarding the nature of the illness included reporting of widespread disbelief in ME/CFS, as well as concern that it was regarded as a psychiatric, functional, or psychosomatic disease. On the content of therapy, emergent sub-themes were the use of CBT and GET, the involvement of rehabilitation institutions, and the role of laboratory investigations and psychological examination. A detailed examination of sub-themes is summarised below.
The central role of dedicated specialists was reported from Latvia and of specialised centres from Spain. There was one such dedicated specialist cluster in Latvia, and certain specific centres in Spain, with a role in diagnosis and management. Widespread disbelief in the existence of ME/CFS was reported as a factor limiting provision of specialist care in Greece. There was reported to be no specialist care available in Austria, Denmark, the Netherlands or Rumania, and little available in France, Germany, Ireland, or Poland. However, since specialist was not defined explicitly in the survey, it is possible that respondents may be referring to a lack of ME/CFS specialists, rather than saying that people with ME/CFS don’t have access to internal medicine and rehabilitation medicine specialists, neurologists, etc. Collaboration with GPs was seen as important in specialist care delivery in Belgium and Slovenia, but seen as problematic in Italy. In Ireland and the UK, GP referral is important as the gateway to specialist care, though this may be verging on non-existent or involve prolonged delays. The two specialist centres in Germany are involved in teaching GPs.
Psychiatric involvement in specialist care was widespread. ME/CFS was perceived to be seen as a functional or psychiatric disease in Austria and Finland, and in Belgium psychiatrists were involved in care. In Italy and the UK, multidisciplinary care involved psychiatrists and psychologists, and psychologists were also involved in care in Serbia. A variety of clinical specialties are involved in the specialist care of people with ME/CFS, though are few in number in most countries. Neurologists are most frequently mentioned, in France, Greece, Italy, Latvia, Slovenia, and Spain. In the UK, various specialties are involved, which would include neurology. Internal medicine specialists are mentioned as being involved in Belgium, France, Italy, Latvia, and Spain. In France and Italy, the involvement of immunologists was mentioned. In Italy and Latvia, the involvement of infectious disease specialists was mentioned. Physical medicine involvement was reported from Italy, rehabilitation medicine from Norway, exercise physiology from Poland, and rheumatology from Slovenia and Spain. There was little information volunteered regarding the content of therapy delivered in specialist care, though CBT and GET were reported from Belgium. The involvement of rehabilitation institutions was reported from Norway, and the role of laboratory investigations and psychological examination from Serbia. A multidisciplinary approach was reported as important in specialist care in Italy, Norway, Slovenia and the UK.
3.2.3. Increasing GP Knowledge and Understanding
Respondents were asked if they had any other suggestions as to possible ways to increase the knowledge and understanding of ME/CFS among primary care doctors and/or other healthcare professionals in primary care. Emergent themes from the responses were the inadequacy of current approaches, the need for top-down action to improve the situation, the importance of centres of excellence, the question of who needed training, the content of curricula, and communications strategies. The inadequacy of current approaches was reported from Austria, where it was stated that few healthcare professionals were involved in the care of people with ME/CFS and interest in the topic was largely down to chance. In Finland similarly, the approach was seen as inadequate because it reinforced the belief that ME/CFS was a functional disorder.
Suggested top-down approaches to improve the situation included the suggestion from Austria that such an approach was needed to establish specialist centres, while from the Netherlands there was seen to be a need for consensus and advice in order to establish such centres. From Germany, it was suggested that standard operating procedures were needed Europe-wide or even world-wide. A similar approach was suggested from Latvia through the development of clinical algorithms, while from Poland financial support for diagnosis and therapy was seen as a priority. In France also, the development of specialist centres was seen as a priority, and in Germany such a centre provided information and education for physicians and patients.
The need for education and training about ME/CFS in undergraduate curricula was raised in Greece, and for Belgium it was suggested that curricula should include the neurophysiology of chronic pain and fatigue. The question of who required training was addressed from Germany, and it was suggested that not only GPs but also neurologists, psychiatrists, cardiologists, endocrinologists, rheumatologists, oncologists, infectious disease specialists, and other specialists required training. Suggestions for possible communications strategies included video-talks, flyers in all general practice premises, health ‘passports’ with basic information on ME/CFS, local and national meetings involving patients’ associations, webinars, on-line short courses and Massive Open Online Courses (MOOCs), and information for the general public on overlapping syndromes like fibromyalgia.
3.2.4. Final Comments
Final comments were ventured from six countries. In Austria, the lack of a systematic plan for ME/CFS was stressed, as was the difficulty patients experienced in medical care and also as regards social insurance through dismissal of their illness. From Denmark it was pointed out that the history of ME/CFS could aid understanding of Covid and its sequelae. In Finland, it was felt that, despite current unhelpful attitudes and official opposition, the healthcare system was on the threshold of a change in attitudes, and patience, more research, and effective treatments were needed to bring this about. However, in Slovenia there was less optimism about the future. Finally, the French contribution was philosophical, quoting William 1st of Orange-Nassau: “Il n’est pas nécessaire d’espérer pour entreprendre, ni de réussir pour persévérer” (“It is not necessary to hope to embark on a course of action, nor to succeed in order to persevere”).